Abstract
Context:
Infectious mononucleosis is a disease primarily of adolescence and early adulthood. The risk of splenic injury and chronic fatigue make return-to-play decisions a challenge for the clinician caring for athletes with infectious mononucleosis.
Evidence Acquisition:
Data were obtained from the PubMed and MEDLINE databases through December 2012 by searching for epidemiology, diagnosis, clinical manifestations, management, and the role of the spleen in infectious mononucleosis.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
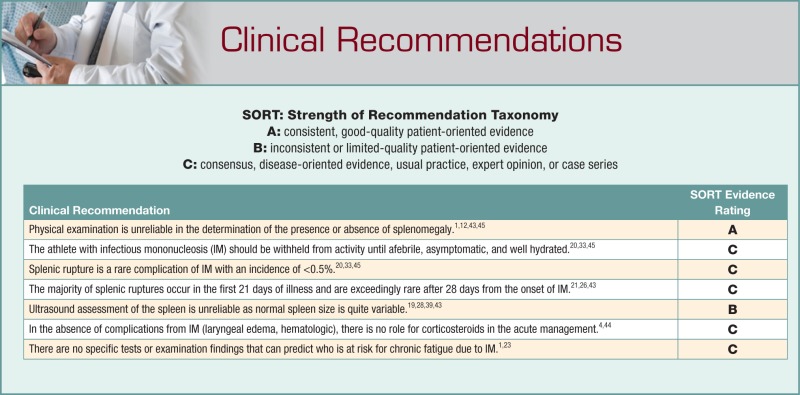
Infectious mononucleosis is commonly encountered in young athletes. Its disease pattern is variable and can affect multiple organ systems. Supportive care is the cornerstone, with little role for medications such as corticosteroids. Physical examination is unreliable for the spleen, and ultrasound imaging has limitations in its ability to guide return-to-play decisions. Exercise does not appear to place the young athlete at risk for chronic fatigue, but determining who is at risk for persistent symptoms is a challenge.
Conclusion:
Return-to-play decisions for the athlete with infectious mononucleosis need to be individualized because of the variable disease course and lack of evidence-based guidelines.
Keywords: mononucleosis, spleen imaging, splenomegaly, chronic fatigue
The question of when an athlete can return to play following contraction of infectious mononucleosis (IM) is complex because of the serious complication of splenic rupture.1,43 Splenic injury is rare but may occur spontaneously or with modest abdominal trauma.26,32 Protecting the athlete from splenic rupture should be at the forefront when making return-to-play decisions. The natural progression of splenic enlargement can be unpredictable, and splenic dimensions vary with body size and type so the role for ultrasonography is unclear. IM also carries the risk of persistent or chronic symptoms, most notably fatigue, as well as neurologic, hematologic, cardiac, and respiratory complications.1,14 The variable presentations and course of this disease pose a challenge for physicians, as evidence-based protocols for return to competition are lacking. Therefore, decisions regarding athletic participation should be made on an individual basis.
Epidemiology
Infectious mononucleosis is a self-limiting clinical syndrome typically caused by the Epstein-Barr virus (EBV).1,20 Epstein-Barr virus is a member of the herpes virus family that causes benign lymphoproliferative IM but has also been linked to Burkitt lymphoma, Hodgkin lymphoma, and nasopharyngeal carcinoma.42 Epstein-Barr virus exposure is common worldwide, with 90% to 95% displaying immunity by adulthood.6,20,30,34 Infection with EBV is often clinically silent in childhood but results in symptomatic illness during adolescence or adulthood.41 The incidence of IM in the United States is approximately 500 cases per 100,000 persons per year, with the highest incidence in the 15- to 24-year-old age group.7 The incidence is almost negligible by 35 years of age.1,20 Among college students, up to half may be initially seronegative, with 15% of that group eventually developing the disease.26,34 There is no sex predilection for IM.45 There is a higher incidence of IM in the white population in comparison with the African American population, believed to be due to earlier exposure to EBV resulting in subclinical manifestations.16
While moderate exercise can be beneficial to the immune system, the duration and intensity of exercise performed by the competitive athlete may impair immune function.14 This has been previously described by a “J curve,” where exercise can initially decrease the rate of illness but has a negative effect at more intense levels.14,19 There is no evidence supporting IM being more prevalent in the student-athlete population in comparison to nonathletes, but their higher incidence of trauma certainly places them at a higher risk for complications.34
Pathogenesis
Epstein-Barr virus, like other members of the herpes virus group, persists within the host in its latent form. The virus is transmitted via saliva, giving the virus the reputation of a “kissing disease,” and has an incubation period of 30 to 50 days.45 Epstein-Barr virus targets memory B lymphocytes and induces their proliferation. As a result, a cell-mediated immunity response produces a clonal expansion of T lymphocytes. The cytotoxic T lymphocytes release a multitude of cytokines that cause the classical IM symptoms. Additionally, the T-lymphocyte response produces lymphoid hyperplasia, a marked lymphocytosis, and atypical lymphocytes in a peripheral blood smear.26 Lytic infection of tonsillar crypt epithelial cells and B lymphocytes results in viral reproduction and shedding into saliva, which decreases exponentially over the first year of infection but will continue to persist for life.13
Clinical Manifestations
The history and physical examination are pertinent for making the correct diagnosis. The long incubation period makes it difficult to determine the source or onset of IM, yet there is a classic 3- to 5-day prodromal period consisting of malaise, fatigue, and anorexia. Symptoms then progress into the classic “triad” of IM—pharyngitis, fever, and lymphadenopathy. At times, the presentation of IM is much more atypical and can affect many different organ systems. Fatigue and pharyngitis are the most debilitating symptoms and often present as the chief complaint. The posterior cervical lymph nodes are more commonly involved in IM, with axillary and inguinal lymphadenopathy less likely to occur. Often, the signs of IM may be subtle, with the athlete presenting with nothing more than fatigue, lack of energy, or diminished performance. Other features of IM may include posterior palatine petechiae, jaundice, exudative pharyngitis, rash, and splenomegaly.14,29,34
Posterior palatine petechiae occur in about one third of cases and are highly suggestive of IM.8 This feature distinguishes an acute EBV infection from other causative agents, such as acute herpes simplex virus infection, HIV infection, or streptococcal infection, that could be included in the differential diagnosis.47
Jaundice is rare, occurring in less than 10% to 15% of patients.27 However, approximately 90% of patients have mildly elevated liver enzymes facilitating in the diagnosis of IM.36
Exudative pharyngitis and concomitant tonsillar enlargement can cause obstruction of the airway, leading to devastating consequences.14,20 The exudation has been described as white, gray, or green and even necrotic in appearance. The enlargement of the tonsil is due to lymphoid hyperplasia and pharyngeal inflammation. Often mistaken for streptococcal pharyngitis, the clinician must be vigilant for clues of IM such as fatigue, the appropriate age group, or posterior cervical lymphadenopathy.26 Positive testing for streptococcal pharyngitis does not completely exclude IM, since simultaneous infection may be seen in up to 30%.29
A rash is seen in about 10% to 40% of patients. The rash is transient and generalized with maculopapular, petechial, or urticarial features (Figure 1). This is more commonly seen in a patient who has been treated with penicillin in an effort to eradicate a presumed group A Streptococcus infection. This is almost pathognomonic for IM. Other antibiotic classes have been implicated, but the penicillins are the most widely reported to produce this effect.13,14
Figure 1.

Rash presenting with infectious mononucleosis.5
Splenomegaly in IM occurs as a result of lymphocytic infiltration enlarging the spleen beyond protection from the rib cage and creating an organ that is susceptible to rupture either spontaneously or traumatically.26,32 This infiltration may also alter splenic architecture, resulting in a more susceptible structure.32,43 The ability to determine the presence of splenomegaly by physical examination is unreliable, with 1 study showing as little as 17% of cases being identified on physical examination.1,12,43,45 Ultrasonography is the imaging modality of choice.1,43 Linear measurements are used since measuring spleen volume is technically difficult. Additionally, normative data are lacking as studies have shown that “average” spleen size can be variable, so this tool has limitations as far as its usefulness in predicting a safe return to play.19,28,39,43
Since baseline spleen size measurements on competitive athletes are impractical, serial ultrasound measurements may be employed to determine the course of splenomegaly in IM. A study of 19 patients with IM found normal spleen measurements in 84% at 1 month after diagnosis and 100% at 2 months. In this series, there were no serial or baseline measurements, leaving the possibility that the “normal” results may still have been abnormal for that individual.32 In a study where baseline spleen measurements were obtained in a large cohort of athletes, those with IM underwent serial ultrasonography. Peak splenic enlargement was typically seen within 2 weeks but, in some, extended to 3.5 weeks. For the majority, splenomegaly resolved in 4 to 6 weeks.18
The long incubation period and variable nature of the disease can make the task of identifying onset of illness a challenge. The acute phase of IM can resolve as quickly as 7 days, but usually takes between 2 and 3 weeks from the onset of symptoms.14,45 This is followed by a recovery period that may take up to 2 to 3 months.1,14,26 IM is typically self-limiting, but an acute EBV infection is a risk factor for chronic fatigue, with symptoms lasting in excess of 6 months.1,23
Diagnosis
The diagnosis of IM can be made through history and physical examination as well as atypical laboratory findings (Table 1).1,20,33 The differential diagnosis includes group A streptococcal infection, influenza virus, herpes virus, cytomegalovirus, toxoplasmosis, acute HIV infection, and many more bacterial and viral pathogens.1,43 Diagnostic criteria for IM (Hoagland criteria) include greater than 50% lymphocytes and at least 10% atypical lymphocytes with fever, pharyngitis, adenoapthy, and a positive serologic test.17 The presence of atypical lymphocytes has a sensitivity of 75% and a specificity of 92%.9 Other laboratory findings that could be suggestive of IM include transient neutropenia, thrombocytopenia, and elevated liver transaminases.27,45 Anemia is considered a feature of complicated IM and is indicative of autoimmune hemolytic anemia, splenic rupture, aplastic anemia, and even disseminated intravascular coagulation.24
Table 1.
| Test | Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value |
|---|---|---|---|---|
| Heterophile antibody—latex agglutination test | 87 | 91 | 52 | 2 |
| Heterophile antibody—solid phase immunoassay | 83 | 97 | 75 | 2 |
| Atypical lymphocytes ≥10% | 75 | 92 | 51 | 3 |
| Atypical lymphocytes ≥50% | 66.3 | 84.5 | 31 | 4 |
| VCA IgM and IgG | 97 | 94 | 64 | 0.5 |
| PCR for EBV DNA | 80 | 94 | 95 | 79 |
VCA, viral capsid antigen; IgM, immunoglobulin M; IgG, immunoglobulin G; PCR, polymerase chain reaction; EBV, Epstein-Barr virus.
Heterophile antibodies are a characteristic feature of IM.9,17,33 Epstein-Barr virus stimulates the development of immunoglobulin M (IgM) antibodies directed against viral antigens.9,17 These antibodies then cross-react with antigens found on sheep and horse red cells. Rapid (monospot) tests for these heterophile antibodies are used to screen patients for IM. About 85% to 90% of patients with confirmed IM will demonstrate a positive heterophile test by week 3 of illness.17,27 Therefore, the first few weeks of illness may result in a negative heterophile test whereby the false-negative rate can be as high as 25% in the first week and repeated testing is required at a later date.32 A definitive diagnosis can be made for IM with more sensitive tests that detect viral capsid antigens for IgM and IgG antibodies.24,33 The negative likelihood ratio for detecting viral capsid antigens is 0.03 in comparison with the negative likelihood ratio for the heterophile antibody test, which is 0.14 to 0.18. Viral capsid antigen testing is useful for patients who initially had a negative heterophile antibody test.2,10 Epstein-Barr virus is the causative agent in 90% of cases of IM, but other viruses rarely produce a “mono syndrome.”11 The most common agents are cytomegalovirus and toxoplasmosis. The illness would have the features of IM, but EBV testing would be negative.11
Management and Prevention
There is no specific treatment for IM. Supportive therapy is the mainstay of care, which includes adequate rest, hydration, and analgesics.14,20,33 Over-the-counter pain medication, such as anti-inflammatories, is generally sufficient to manage the myalgias and pharyngitis. Acetaminophen is appropriate but used judiciously because of potential liver complications, as IM frequently causes elevation in liver function tests.15 Aspirin should be avoided because of bleeding risks and an association of IM with Reye syndrome in children.14,33 There is no role for antivirals or antibiotics.14,15,20,34 Despite the fatigue, there is no role for strict bed rest. For patients with a quick recovery of symptoms, a return to light exercise in as little as 2 weeks from the onset of illness may provide a benefit. Close follow-up is recommended to ensure resolution of all symptoms as the athlete may risk progression to more chronic symptoms, specifically fatigue.20,46
The role of corticosteroids in the treatment of IM is of interest but there is insufficient evidence to recommend their use in uncomplicated IM. There does not appear to be any improvement in duration of symptoms or progression to chronic symptoms.4,44 In spite of this, a significant number of patients are given corticosteroids for symptom control in the absence of the complications of IM.41 There is general consensus that corticosteroids do have a role when there is airway obstruction as a result of laryngeal edema.4,33,41 Other severe complications of IM warranting corticosteroid treatment include hepatitis, myocarditis, or hematologic abnormalities.4,33,41 Risks and benefits must be weighed, as the adverse effects of corticosteroids in IM may include infection or even femoral head necrosis.4,14,20,41
Transmission is by close contact via saliva, so isolation is not necessary. Common sense precautions such as hand washing and not sharing water bottles are typically adequate. Unfortunately, the long incubation period can confound efforts to prevent infecting others.17,34 Current advances are being made to develop an EBV vaccine. In a phase 2 trial, vaccine recipients were less likely to have symptoms of IM during primary EBV infection compared with those who were not vaccinated.38 However, the recipients were not protected against acquiring EBV.38
Return-to-Play Considerations
There is general consensus that the athlete must be asymptomatic with resolution of symptoms such as fever, fatigue, and pharyngitis before they initiate any return to activity.20,31,33 The majority of those with IM will not feel well enough to pursue activity during the first weeks of illness, which makes clinical decisions easier. They ought to be afebrile and well hydrated.31,33,45 Any concern for oropharyngeal issues or airway compromise would clearly prohibit any sports participation.14,20,34,45 Although their level of conditioning would be expected to decline, the athlete should have full resolution of fatigue or risk prolonged symptoms.1,34 Resolution of laboratory abnormalities (eg, elevated white blood cell counts, abnormal liver function tests) do not play a role in assisting return-to-play decisions.34 It is difficult to predict who is at risk for prolonged symptoms, but competitive athletes may actually be at a lower level of risk for chronic fatigue.1,3,34 Nonetheless, the athlete should “feel good” before considering return to play.1,3,34
For those athletes who do have “early” resolution of symptoms, there is little consensus on the optimal time for return to activity. Keeping in mind that the highest risk for splenic injury is during the first 21 days of illness, it has not been shown that early return to light activity causes deleterious effects.21,26,43 The athlete should engage in very light activity at first (walking), with a gradual progression to light aerobic activity.33,36,45 Although it may take 2 to 3 months for the athlete to fully recover from IM, it appears they can initiate activity well before.1,34,43,46
The return to activities that place the spleen at risk for injury is a confounding matter. At this time, recommendations vary, and there is a lack of evidence-based protocols.33,45 The concern is the athlete participating in any activity that increases intra-abdominal pressure and contact sports that would place the chest or abdomen at risk for trauma.33,45 In ultrasound studies, peak spleen size is typically noted within the first 2 weeks of illness, but may extend to 3.5 weeks.18 The majority of spleen injuries occur within the first 21 days of illness and are exceedingly rare at >28 days.21,26,43 Fortunately, splenic rupture is rare, occurring in <0.5% of those with IM, but its consequences can be severe.20,34,43
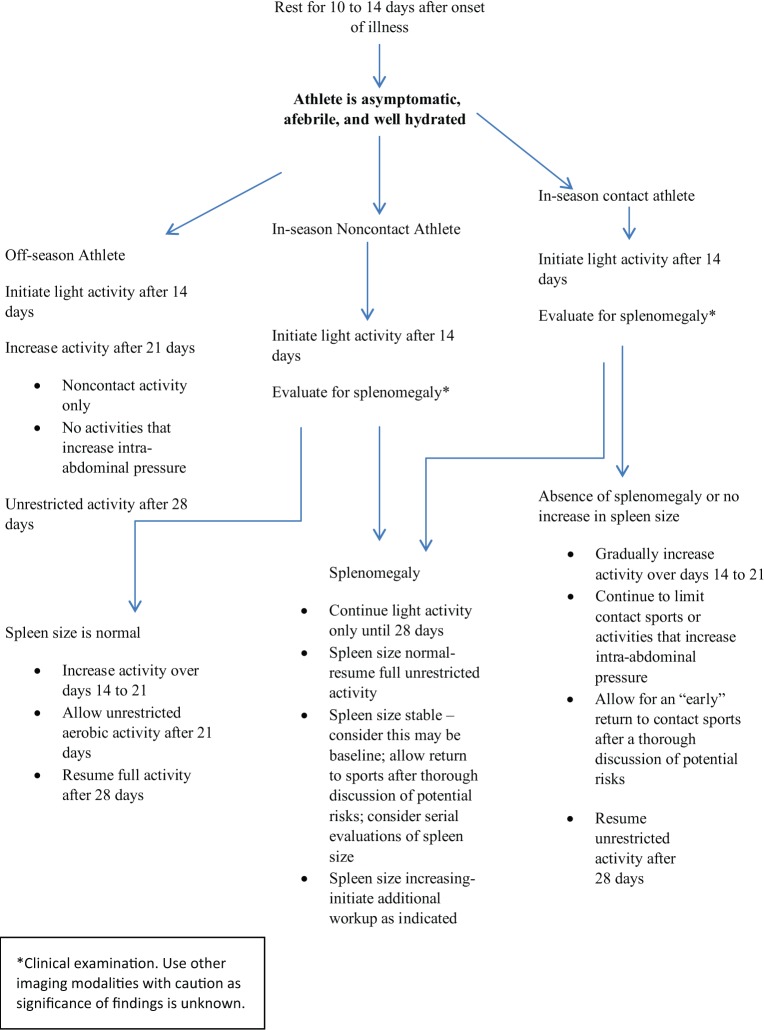
Most recommendations support that the athlete with IM should rest for 3 weeks and then begin resumption of light activity.1,20,25,34 Keeping in mind there is so much individual variability to this disease and the exact date of onset is often difficult to establish, return-to-play recommendations should be individualized. Ultrasonography may play a role in return-to-play decisions, but the variability in baseline spleen size can limit its utility.19,28,39,43 Additional factors include the nature of the activity or sport (contact vs noncontact) and the season in which the illness occurs (competitive season vs off-season). Any return to competition must include a detailed explanation of the risk of splenic injury, since full recovery may take months (Figure 2).
Figure 2.
Return-to-play recommendations for infectious mononucleosis (IM). Level of evidence, 4.7,9,24,28,32,35,40,41
There have been some novel attempts made to protect the spleen from contact for collision sports with a flak jacket22 or a customized protective brace for a college basketball season.37
Conclusion
Counseling the athlete with IM remains a challenge. The disease has a long latency period, the onset of illness may be difficult to identify, and the disease course is variable. There is no specific physical examination finding, laboratory test, or imaging modality that provides a definitive answer. To minimize complications of IM, return-to-play decisions must be individualized.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. Auwaerter PG. Infectious mononucleosis: return to play. Clin Sports Med. 2004;23:485-497 [DOI] [PubMed] [Google Scholar]
- 2. Bruu AL, Hjetland R, Holter E, et al. Evaluation of 12 commercial tests for detection of Epstein-Barr virus-specific and heterophile antibodies. Clin Diagn Lab Immunol. 2000;7:451-456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Candy B, Chalder T, Cleare AJ, et al. Predictors of fatigue following the onset of infectious mononucleosis. Psychol Med. 2003;33:847-855 [DOI] [PubMed] [Google Scholar]
- 4. Candy B, Hotopf M. Steroids for symptom control in infectious mononucleosis. Cochrane Database Syst Rev. 2006;(3):CD004402. [DOI] [PubMed] [Google Scholar]
- 5. Chan KH, Ng MH, Seto WH, Peiris JS. Epstein-Barr virus (EBV) DNA in sera of patients with primary EBV infection. J Clin Microbiol. 2001;39:4152-4154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chetham MM, Roberts KB. Infectious mononucleosis in adolescents. Pediatr Ann. 1991;20:206-213 [DOI] [PubMed] [Google Scholar]
- 7. Crawford DH, Macsween KF, Higgins CD, et al. A cohort study among university students: identification of risk factors for Epstein-Barr virus seroconversion and infectious mononucleosis. Clin Infect Dis. 2006;43:276-282 [DOI] [PubMed] [Google Scholar]
- 8. Dunnet WN. Infectious mononucleosis. Br Med J. 1963;1:1187-1191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ebell MH. Epstein-Barr virus infectious mononucleosis. Am Fam Physician. 2004;70:1279-1287 [PubMed] [Google Scholar]
- 10. Elgh F, Linderholm M. Evaluation of six commercially available kits using purified heterophile antigen for the rapid diagnosis of infectious mononucleosis compared with Epstein-Barr virus-specific serology. Clin Diagn Virol. 1996;7:17-21 [DOI] [PubMed] [Google Scholar]
- 11. Evans AS. Infectious mononucleosis and related syndromes. Am J Med Sci. 1978;276:325-339 [DOI] [PubMed] [Google Scholar]
- 12. Grover SA, Barkum AN, Sackett DL. The rational clinical examination: does this patient have splenomegaly? JAMA. 1993;270:2218-2221 [PubMed] [Google Scholar]
- 13. Hadito V, Shapiro M, Greenough TC, Sullivan JL, Luzuriaga K, Thurley-Lawson DA. On the dynamics of acute EBV infection and the pathogenesis of infectious mononucleosis. Blood. 2008;111:1420-1427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Harris MD. Infectious disease in athletes. Curr Sports Med Rep. 2011;10:84-89 [DOI] [PubMed] [Google Scholar]
- 15. Haverkos HW, Amsel Z. Adverse virus-drug interactions. Rev Infect Dis. 1991;13:697-704 [DOI] [PubMed] [Google Scholar]
- 16. Heath CW, Jr, Brodsky AL, Potolsky AI. Infectious mononucleosis in a general population. Am J Epidemiol. 1972;95:46-52 [DOI] [PubMed] [Google Scholar]
- 17. Hoagland RJ. Infectious mononucleosis. Primary Care. 1975;2:295-307 [PubMed] [Google Scholar]
- 18. Hosey RG, Kriss V, Uhl TL, DiFiori J, Hecht S, Wen DY. Ultrasonographic evaluation of splenic enlargement in patients with acute infectious mononucleosis. Br J Sports Med. 2008;42:974-977 [DOI] [PubMed] [Google Scholar]
- 19. Hosey RG, Mattacola CG, Kriss V, Armsey T, Quarles JD, Jagger J. Ultrasound assessment of spleen size in college athletes. Br J Sports Med. 2006;40:251-254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hosey RG, Rodenberg RE. Infectious disease and the college athlete. Clin Sports Med. 2007;26:449-471 [DOI] [PubMed] [Google Scholar]
- 21. Johnson MA, Cooperberg PL, Boisvert J, Stoller JL, Winrob H. Spontaneous splenic rupture in infectious mononucleosis. AJR Am J Roentgenol. 1981;136:111-114 [DOI] [PubMed] [Google Scholar]
- 22. Jong MD, Bytomski J. Idiopathic splenomegaly and return to play—men’s soccer. Med Sci Sports Exerc. 2005;37(suppl):279-280 [Google Scholar]
- 23. Katz BZ, Yukiko S, Mears CJ, Binns HJ, Taylor R. Chronic fatigue syndrome after infectious mononucleosis in adolescents. Pediatrics. 2009;124:189-193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Luzuraiaga K, Sullivan JL. Infectious mononucleosis. N Engl J Med. 2010;362:1993-2000 [DOI] [PubMed] [Google Scholar]
- 25. MacKnight JM. Infectious mononucleosis: ensuring a safe return to sport. Phys Sportsmed. 2002;30:27-41 [DOI] [PubMed] [Google Scholar]
- 26. Maki DG, Reich RM. Infectious mononucleosis in the athlete: diagnosis, complications, and management. Am J Sports Med. 1982;10:162-173 [DOI] [PubMed] [Google Scholar]
- 27. Mason WR, Jr, Adams EK. Infectious mononucleosis: an analysis of 100 cases with particular attention to diagnosis, liver function tests and treatment of selected cases with prednisone. Am J Med Sci. 1958;236:447-506 [PubMed] [Google Scholar]
- 28. McCorkle R, Thomas B. Normative spleen size in tall healthy athletes: implications for safe return to contact sports after infectious mononucleosis. Clin J Sport Med. 2010;20:413-415 [DOI] [PubMed] [Google Scholar]
- 29. Neiman DC. Is infection risk linked to exercise workload? Med Sci Sports Exerc. 2000;32(7 suppl):S406-S411 [DOI] [PubMed] [Google Scholar]
- 30. Niederman JC, Evans AS, Subrahamanyan L, McCollum RW. Prevalence, incidence and persistence of Epstein-Barr virus antibody in young adults. N Engl J Med. 1970;282:361-365 [DOI] [PubMed] [Google Scholar]
- 31. Noffsinger J. Physical activity considerations in children and adolescents with viral infections. Pediatr Ann. 1996;25:585-589 [DOI] [PubMed] [Google Scholar]
- 32. O’Connor TE, Skinner LJ, Kiely P, Fenton JE. Return to contact sports following infectious mononucleosis: the role of serial ultrasonography. ENT J. 2011;90:E21-E24 [DOI] [PubMed] [Google Scholar]
- 33. Putukian M, O’Connor FG, Stricker PR, et al. Mononucleosis and athletic participation: an evidence-based subject review. Clin J Sport Med. 2008;18:309-315 [DOI] [PubMed] [Google Scholar]
- 34. Rea TD, Russo JE, Katon W, Ashley RL, Buchwald DS. Prospective study of the natural history of infectious mononucleosis caused by Epstein-Barr virus. J Am Board Fam Pract. 2001;14:234-242 [PubMed] [Google Scholar]
- 35. Rush MC, Simon MW. Occurrence of Epstein-Barr virus illness in children diagnosed with group A streptococcal pharyngitis. Clin Pediatr (Phila). 2003;42:417-420 [DOI] [PubMed] [Google Scholar]
- 36. Schuler JG, Filtzer H. Spontaneous splenic rupture: the role of nonoperative management. Arch Surg. 1995;130:662-665 [DOI] [PubMed] [Google Scholar]
- 37. Shah N, Richards D. Facilitating sport participation with a customized spleen guard: a case of a basketball player with splenomegaly. Clin J Sport Med. 2008;18:92-95 [DOI] [PubMed] [Google Scholar]
- 38. Sokal EM, Hoppenbrouwers K, Vandermeulen C, et al. Recombinant gp350 vaccine for infectious mononucleosis: a phase 2, randomized, double-blind, placebo-controlled trial to evaluate the safety, immunogenicity, and efficacy of an Epstein-Barr virus vaccine in healthy young adults. J Infect Dis. 2007;196:1749-1753 [DOI] [PubMed] [Google Scholar]
- 39. Spielman AL, DeLong DM, Kliewer MA. Sonographic evaluation of spleen size in tall healthy athletes. AJR Am J Roentgenol. 2005;184:45-49 [DOI] [PubMed] [Google Scholar]
- 40. Tamir D, Benderly A, Levy J, Ben-Porath E, Vonsover A. Infectious mononucleosis and Epstein-Barr virus in childhood. Pediatrics. 1974;53:330-335 [PubMed] [Google Scholar]
- 41. Thompson SK, Doerr TD, Hengerer AS. Infectious mononucleosis and corticosteroids: management practices and outcomes. Otolaryngol Head Neck Surg. 2005;131:900-904 [DOI] [PubMed] [Google Scholar]
- 42. Thorley-Lawson DA, Gross A. Persistence of the Epstein-Barr virus and the origins of associated lymphomas. N Engl J Med. 2004;350:1328-1337 [DOI] [PubMed] [Google Scholar]
- 43. Turner J, Gard M. Splenomegaly and sports. Curr Sports Med Rep. 2008;7:113-116 [DOI] [PubMed] [Google Scholar]
- 44. Tynell E, Aurelius E, Brandell A. Acyclovir and prednisolone treatment of acute infectious mononucleosis: a multicenter, double-blind, placebo-controlled study. J Infect Dis. 1996;174:324-331 [DOI] [PubMed] [Google Scholar]
- 45. Waninger KN, Harcke HT. Determination of safe return to play for athletes recovering from infectious mononucleosis: a review of the literature. Clin J Sport Med. 2005;15:410-416 [DOI] [PubMed] [Google Scholar]
- 46. Welch MJ, Wheeler L. Aerobic capacity after contracting infectious mononucleosis. Orthop Sports Phys Ther. 1986;8:199-202 [DOI] [PubMed] [Google Scholar]
- 47. Yoda K, Sata T, Kurata T, Aramaki H. Oropharyngotonsillitis associated with nonprimary Epstein-Barr virus infection. Arch Otolaryngol Head Neck Surg. 2000;126:185-193 [DOI] [PubMed] [Google Scholar]