Abstract
Background:
The in-line lunge of the Functional Movement Screen (FMS) evaluates lateral stability, balance, and movement asymmetries. Athletes who score poorly on the in-line lunge should avoid activities requiring power or speed until scores are improved, yet relationships between the in-line lunge scores and other measures of balance, power, and speed are unknown.
Hypothesis:
(1) Lunge scores will correlate with center of pressure (COP), maximum jump height (MJH), and 36.6-meter sprint time and (2) there will be no differences between limbs on lunge scores, MJH, or COP.
Study Design:
Descriptive laboratory study.
Level of Evidence:
Level 3.
Methods:
Thirty-seven healthy, active participants completed the first 3 tasks of the FMS (eg, deep squat, hurdle step, in-line lunge), unilateral drop jumps, and 36.6-meter sprints. A 3-dimensional motion analysis system captured MJH. Force platforms measured COP excursion. A laser timing system measured 36.6-m sprint time. Statistical analyses were used to determine whether a relationship existed between lunge scores and COP, MJH, and 36.6-m speed (Spearman rho tests) and whether differences existed between limbs in lunge scores (Wilcoxon signed-rank test), MJH, and COP (paired t tests).
Results:
Lunge scores were not significantly correlated with COP, MJH, or 36.6-m sprint time. Lunge scores, COP excursion, and MJH were not statistically different between limbs.
Conclusion:
Performance on the FMS in-line lunge was not related to balance, power, or speed. Healthy participants were symmetrical in lunging measures and MJH.
Clinical Relevance:
Scores on the FMS in-line lunge should not be attributed to power, speed, or balance performance without further examination. However, assessing limb symmetry appears to be clinically relevant.
Keywords: screening, symmetry, unilateral, limb dominance
Superior athletic performance is typically attributed to athletes who possess greater power, speed, and balance,28 and limb asymmetries appear to increase risk of injury.15,32,33,39 The Functional Movement Screen (FMS) uses standardized movement patterns to clinically assess movement quality in active individuals.2,3,6-8,11,12,21,23,31 The FMS forecasts risk of injury and identifies specific exercises and activities to avoid until the required movement competency is achieved.9 Higher scores on the FMS are anecdotally linked to better athletic performance, and poorer scores are addressed to decrease risk of injury.7-9
The FMS is composed of 7 tests: the deep squat, hurdle step, in-line lunge, shoulder mobility, active straight-leg raise, trunk stability push up, and rotary stability.7,8 Each test is scored on a 0 to 3 scale, with 3 being the best score, and scores of all tests are then summed for a total score.7,8 Poor scores are thought to increase risk of injury, thus certain activities should be avoided until the limited movement pattern is addressed.9 However, there is inconsistency in interpreting FMS results, as both high and low scores have predicted increased risk for injury in active male and female individuals.2,6 Furthermore, total FMS score is not a meaningful predictor of sprinting, jumping, and agility measures,31 and limited evidence exists to inform whether specific scores on the 7 tasks are associated with athletic performance.4,29
Grading guidelines state that if an athlete scores asymmetrically or is graded a 1 on the in-line lunge, then speed and agility training is inappropriate until the faulty in-line lunge pattern is corrected.9 Yet the relationships between FMS in-line lunge scores and performance measures remain unclear.5,29 Testing whether in-line lunge scores are related to known measures of power (unilateral maximum jump height [MJH]) and speed (36.6-m sprint)10,18-20,25,38 are warranted to support these guidelines. Since balance (center of pressure [COP] during the in-line lunge) and movement asymmetries are associated with increased risk of injury,15,32,33,39 the association between balance and in-line lunge scores and scoring the in-line lunge to quantify asymmetrical movement patterns is also warranted.
The purpose of this research was to understand the FMS in-line lunge’s relationship to unilateral jump height, 36.6-m sprint time, and COP excursion in the medial-lateral direction during the in-line lunge. We hypothesized that (1) lunge scores will correlate with MJH, 36.6-m sprint time, and COP excursion while lunging and (2) there will be no difference between the dominant and nondominant limb in scores on the FMS in-line lunge, MJH during the unilateral drop jump, and COP during the in-line lunge.
Methods
A descriptive study design was used to evaluate limb symmetry during lunging and unilateral drop jumps and to determine whether relationships between FMS in-line lunge score, power, speed, and balance existed. The study took place at the University of New England’s Human Performance Laboratory located at Orthopaedic Associates Performance Center, Saco, Maine, USA.
Participants
Because of a lack of information in the current literature, to power our study, we chose to use the Cohen method with a moderate d, an α of 0.05, and a β of 0.8 to estimate our sample size.34 Thirty-three participants were estimated, and we received funding to compensate 37 participants to account for potential attrition via outliers and/or unusable data. Outliers were defined a priori as greater than 3 standard deviations from the mean.
Thirty-seven participants were recruited using posted fliers at the University of New England (UNE) and e-mails to the UNE community (Portland and Biddeford campuses). We included healthy men and women, aged 18 to 40 years, who met the fitness guidelines set forth by the American College of Sports Medicine, defined as follows: (1) performed moderate-intensity aerobic physical activity for a minimum of 30 minutes 5 days per week or vigorous activity for a minimum of 20 minutes 3 days per week or (2) performed activities that maintain or increase muscular strength and endurance a minimum of 2 days each week.37 Participants were excluded if they had a history of or current musculoskeletal pathology that restricted normal movement capabilities, which included but were not limited to the following: spine/hip/knee/ankle surgeries; hip/knee osteoarthritis; shoulder impingement or upper extremity issues restricting internal and external range of motion necessary to reach the dorsum of the hand to the lumbar spine and palmar aspect of the hand to the back of the head, respectively (this motion is required to hold a dowel while performing the in-line lunge assessment); knee joint effusion; and/or any complaints of pain during lunging or jumping. There were no exclusion criteria based on lower extremity range of motion.
Data Collection
The subject was asked to perform the first 3 tests of the FMS protocol, then unilateral drop jump landings, and finally, the 36.6-m sprints. To establish limb preference, participants were asked, “If you were to stand with feet parallel and hip width apart, arms by sides, and eyes fixed straight ahead, which leg would you use to kick a ball, pick up a marble, and trace shapes with your foot if the objects for manipulation were placed midway between both limbs?” A laterality quotient was used to determine limb dominance by subtracting the frequency of left limb responses from right limb responses and then dividing by the total number of tasks. A negative number corresponded with the right limb and a positive number with the left. A laterality quotient using similar criteria based on the same 3 tasks demonstrated high reliability in determining footedness.36
Once limb dominance was determined, a random number generator was used to determine which limb would be forward first when performing the lunge. To keep in agreement with the FMS protocol, no warm-up or practice trials were allowed, and the forward limb was the limb of interest.7,8 Participants completed 3 repetitions of the first 3 tasks of the FMS in a predetermined order per the FMS protocol: deep squat, hurdle step, and in-line lunge.7 The FMS kit was used for the deep squat and hurdle step tasks, and the in-line lunge platform was not used. Instead, the laboratory floor was prepared with a 6-inch-wide strip marked with tape on the force plate to replicate the platform used by the FMS kit. The participant’s tibia length was measured, from the ground to the top center of the tibial tuberosity, to determine the distance between feet when lunging.7 Lunge scores were based on FMS grading criteria7 (Table 1 and Figure 1).
Table 1.
Functional Movement Screen in-line scoring criteria
| Functional Movement Screen Score | |||
|---|---|---|---|
| 3 | 2 | 1 | 0 |
| • Dowel contacts remain with lumbar spine extension | • Dowel contacts do not remain with lumbar spine extension | • Loss of balance is noted | • The athlete will receive a score of zero if pain is associated with any portion of this test; a medical professional should perform a thorough evaluation of the painful area |
| • No torso movement is noted | • Movement is noted in torso | ||
| • Dowel and feet remain in sagittal plane | • Dowel and feet do not remain in sagittal plane | ||
| • Knee touches board behind heel of front foot | • Knee does not touch behind heel of front foot | ||
Figure 1.
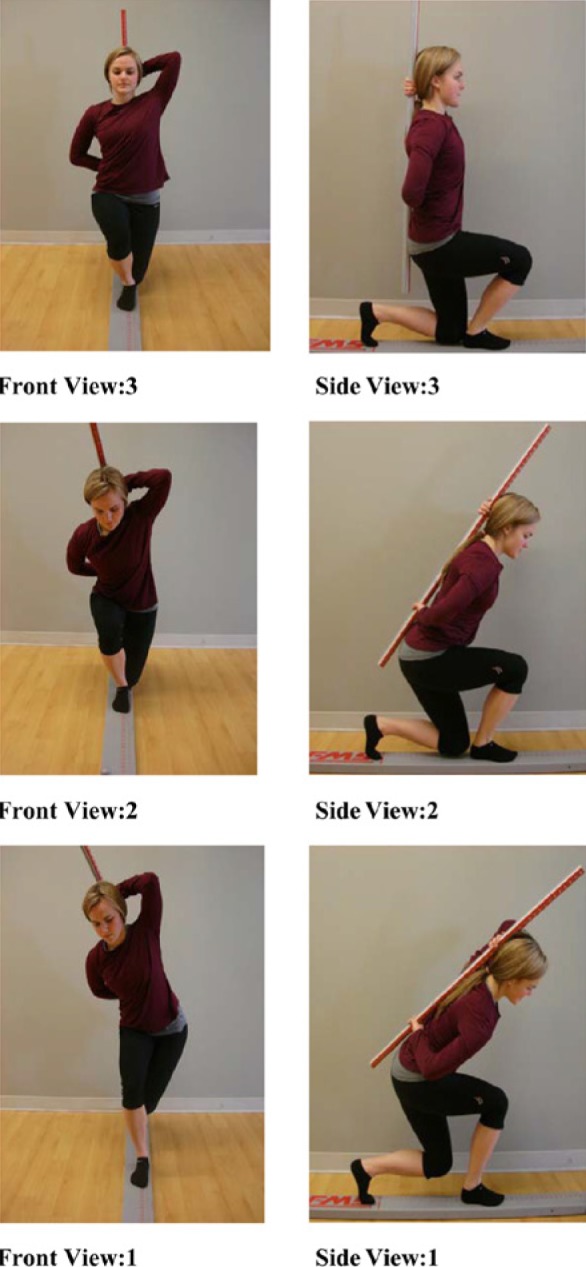
Functional Movement Screen in-line scoring criteria outline.
All in-line lunge scores were determined by the same investigator who was familiar with the FMS in-line lunge protocol and scoring criteria. Reliability of FMS scoring between novice and expert raters has been shown to be moderate to excellent, with intrasession interrater reliability measuring 0.98 on total FMS scoring33 and 89.8% agreement in scoring on the in-line lunge between novice and expert raters.27 Three trials were attempted, with the highest rating used for analysis. Additionally, the COP excursion in the medial-lateral direction that corresponded with the best in-line lunge score for each limb was used for analysis.20
After lunging, participants performed 3 unilateral drop jumps off a 30.48-cm (12-inch) plyometric box for both the dominant and nondominant limb.1 Participants were given 2 practice trials for each limb followed by 3 measured trials. A 45- to 60-second rest period between each jump was given to minimize the effects of fatigue. Participants were asked to stand on the plyometric box with the nonjumping leg (which was randomized) then lean forward to fall from the box. Instructions were to immediately jump up as high as possible on landing with time on the ground kept to a minimum. A total of 3 jumps were measured, and the best of the 3 trials was used for analysis.
After completion of the drop jump landing tasks, participants were asked to sprint. Sprint trials were measured using a laser timer system (Brower Timing Systems, Draper, Utah). Participants were allowed 1 practice 36.6-m sprint as a warm up where they selected their starting position and thumb placement on the starting pad. Participants were instructed to stand behind a start line on an indoor rubber track. From the start point, participants began in a 3-point stance, started to sprint when desired, and sprinted 36.6 m. A total of 3 trials were measured, and the best of the 3 trials was used for the analysis.
Data Management and Analysis
Lunge and drop jump trials were performed on 2 force plates (AMTI, Watertown, Massachusetts) set at 2400 Hz covered by a Super X indoor rubber track surface (All Sports Enterprises, Exton, Pennsylvania). Jump height was measured with a single marker attached to the pelvis over the sacrum. A standing calibration was used to attain baseline height for the pelvic marker. Lunge COP excursion (maximal distance moved) was normalized to foot width,18,19 with markers on the first and fifth metatarsal heads used to define foot width. Kinematic data were collected at 240 Hz using 8 Oqus Series-3 cameras (Qualisys, Gothenburg, Sweden).
Visual 3D was used to apply a Butterworth filter with a cutoff of 12 Hz for jump trials32 and 6 Hz for lunge trials for kinematic data and a Butterworth filter with cutoff of 20 Hz for analog data, as determined by a fast Fourier transformation.
Statistical Analysis
Statistics software was used to calculate demographic data and to perform the analyses (SPSS Statistics 20, IBM Corporation, Armonk, New York). A Wilcoxon signed-rank test was used to determine whether scores on the in-line lunge differed between dominant and nondominant limbs. Paired t tests were used to compare the dominant and nondominant limb’s COP during the FMS in-line lunge and maximum jump height. A Spearman rho test was used to determine relationships between FMS in-line lunge scores and COP excursion during the FMS in-line lunge, unilateral drop jump maximum height, and 36.6-m sprint times.
Results
Descriptive statistics were calculated for age, weight, height, body mass index, sex, and limb dominance (Table 2). Frequency counts of the FMS in-line lunge scores were obtained for the dominant and nondominant limb (Table 3). FMS in-line lunge scores were not statistically significantly correlated with any athletic performance measures (eg, COP excursion, MJH, or sprint time) (Table 4). No significant differences between limbs were found for FMS in-line lunge scores, COP excursions, or MJH during the unilateral drop jump (Table 5).
Table 2.
Subject demographics
| Mean (SD) | Range | |
|---|---|---|
| Age, y | 25.1 (3.7) | 21-40 |
| Mass, kg | 72.0 (15.9) | 51.8-129.6 |
| Height, m | 1.7 (0.1) | 1.59-1.90 |
| BMI, kg/m2 | 24.5 (3.9) | 19.55-38.7 |
| Sex | 17 men; 20 women | |
| Limb dominance | 30 right; 7 left | |
SD, standard deviation; BMI, body mass index.
Table 3.
Frequency count of Functional Movement Screen (FMS) in-line lunge score
| Dominant Limb | Nondominant Limb | |
|---|---|---|
| FMS score 3 | 18 | 18 |
| FMS score 2 | 15 | 13 |
| FMS score 1 | 4 | 6 |
| N | 37 | 37 |
Table 4.
Relationships between Functional Movement Screen ranking and performance measures
| Dominant Lunge | Nondominant Lunge | |
|---|---|---|
| COP | ||
| Correlation coefficient | 0.081 | −0.293 |
| P value | 0.64 | 0.08 |
| N | 37 | 37 |
| MJH | ||
| Correlation coefficient | 0.101 | −0.036 |
| P value | 0.55 | 0.83 |
| N | 37 | 37 |
| 36.6-meter sprint | ||
| Correlation coefficient | −0.136 | −0.219 |
| P value | 0.42 | 0.19 |
| N | 37 | 37 |
COP, center of pressure excursion in the medial-lateral direction; MJH, maximum jump height.
Table 5.
Limb differences
| Dominant Limb, Mean (SD) | Nondominant Limb, Mean (SD) | 95% CI | P Value | |
|---|---|---|---|---|
| FMS in-line lunge scores | 2.38 (0.681) | 2.32 (0.747) | −0.121 to 0.229 | 0.527a |
| COP (% foot width) | 31.5 (9.60) | 34.6 (10.3) | −6.9 to 0.7 | 0.110b |
| MJH (m) | 0.278 (0.059) | 0.271 (0.056) | −0.004 to 0.017 | 0.201b |
FMS, Functional Movement Screen; SD, standard deviation; CI, confidence interval; COP, center of pressure; MJH, maximum jump height.
P value for the Wilcoxon matched-pair signed-rank test.
P value for the paired-samples t test.
Discussion
Better performance on the FMS in-line lunge was not related to better balance while lunging (smaller COP excursion), greater power generation (MJH), or faster speed (lower 36.6-m sprint time), as hypothesized. However, no significant differences were found between limbs while lunging (scores or COP measures) or jumping. The implication that those with lower scores should not perform power/speed movements until the scores on the in-line lunge improve7 was not supported by our findings. Thus, using the in-line lunge grading criteria to assess limb asymmetries may be clinically meaningful, whereas relating poor lunge performance with readiness to work on parameters of power, speed, and balance is not recommended.
Though supporters of the FMS suggest that mobility and stability gained by working on the lunge movement pattern will enhance body awareness and motor learning and lead to better power and speed,7,9 lunge scores do not relate well to these performance measures. Other researchers found a relationship between the lunge score and the T-run agility test for the left limb only, but lunge scores were not related to the backward medicine ball throw or the single leg squat test.29 Additionally, no significant correlations were found between the total FMS score and vertical jump height as well as the 10-m and 20-m sprint time.31 Furthermore, scores on the in-line lunge do not relate to balance measures in the medial-lateral direction.
Others reported no significant relationship between FMS in-line lunge scores and standing balance measured by COP standard deviation in the medial-lateral and anterior-posterior directions, COP velocity, and COP area.6 Since dynamic tests of balance have more utility in evaluating athletic balance than static balance measures,19 we investigated COP measures during the in-line lunge task itself. Given that a tandem stance increases stress on the postural-control system in the frontal plane30 and the in-line lunge assumes an exaggerated tandem stance, we hypothesized that a relationship would exist between lunge scores and maximum medial-lateral excursion of COP. Additionally, since frontal plane movement lowers the score on the lunge, a larger total COP excursion in the medial-lateral direction was expected for lower scores. However, a lack of empirical evidence relating FMS in-line lunge to static standing balance or balance during the in-line lunge task itself questions the assumption that performance on the FMS in-line lunge is associated with balance performance.
Our findings indicate that healthy participants scored highly on the FMS in-line lunge for both limbs and moved symmetrically. Participants’ in-line lunge scores were distributed across the 1, 2, and 3 score ranges (see Table 3), yet scores were predominantly 3 (skewness: −0.647 for the dominant limb and −0.621 for the nondominant limb). The in-line lunge is one of the most consistent and highest graded tests of the FMS, with the majority of young, active male and female individuals scoring either a 2 or 3.13,35 Both active individuals and elite athletes score symmetrically during the in-line lunge, maximal jumping, and static and dynamic balance tests.14,16,17,21,22,24,26 Based on our results and in conjunction with previous research across the spectrum of elite athletes and nonathletes, it appears that healthy individuals tend to have equal side-to-side postural control of their limbs during static and dynamic tasks including the FMS in-line lunge and symmetrical unilateral jump heights.
Limitations
Our results are generalizable to healthy, physically active 18- to 40-year-old subjects. The majority of our participants scored high (2 or 3) on the FMS in-line lunge, which may have limited our ability to make meaningful correlations. Additionally, we were interested in medial-lateral sway during the FMS in-line lunge, and subsequent research using additional postural control variables would provide a more comprehensive investigation of the relationship between balance measures and in-line lunge performance.
Conclusion
The FMS in-line lunge scores were not found to be related to power, speed, or balance performance measures. The results suggest that scoring of the FMS in-line lunge may not be sensitive enough to effectively differentiate variables that could affect performance, such as center of pressure measures in the medial-lateral direction, a 36.6-m sprint, or unilateral drop jump. Healthy subjects were symmetrical when lunging and performing maximal jump height during the unilateral drop jump. Scores on the FMS in-line lunge should not be attributed to a subject’s balance during the in-line lunge task or infer performance ability in tasks requiring lower extremity power or speed; however, lunge scores may still have clinical utility in identifying abnormal and asymmetrical movement as part of a thorough examination.
Acknowledgments
We acknowledge the Department of Physical Therapy’s grant funding, which was used for subject honorariums for this study. We also to thank Stanley Skolfield, ATC, CSCS, the OA Performance Center/Parisi Speed School Manager, for allowing us to use their FMS kit during this study.
Footnotes
The following author declared potential conflicts of interest: Erin Hartigan received a grant and consulting fees or honorarium from UNE.
References
- 1. Baechle TE. Essentials of Strength Training and Conditioning. Champaign, IL: Human Kinetics; 2008 [Google Scholar]
- 2. Ben Kazman J, Galecki J, Lisman P, Deuster PA, O’Connor FG. Factor structure of the Functional Movement Screen in Marine officer candidates [published online August 5, 2013]. J Strength Cond Res. 10.1519/JSC.0b013e3182a6dd83 [DOI] [PubMed] [Google Scholar]
- 3. Bodden JG, Needham RA, Chockalingam N. The effect of an intervention program on Functional Movement Screen test scores in mixed martial arts athletes [published online July 15, 2013]. J Strength Cond Res. 10.1519/JSC.0b013e3182a480bf [DOI] [PubMed] [Google Scholar]
- 4. Butler RJ, Plisky PJ, Southers C, Scoma C, Kiesel KB. Biomechanical analysis of the different classifications of the Functional Movement Screen deep squat test. Sports Biomech. 2010;9:270-279 [DOI] [PubMed] [Google Scholar]
- 5. Chapman RF, Laymon AS, Arnold T. Functional movement scores and longitudinal performance outcomes in elite track and field athletes [published online April 23, 2013]. Int J Sports Physiol Perform. [DOI] [PubMed] [Google Scholar]
- 6. Chorba RS, Chorba DJ, Bouillon LE, Overmyer CA, Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. N Am J Sports Phys Ther. 2010;5:47-54 [PMC free article] [PubMed] [Google Scholar]
- 7. Cook G, Burton L, Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function—part 1. N Am J Sports Phys Ther. 2006;1:62-72 [PMC free article] [PubMed] [Google Scholar]
- 8. Cook G, Burton L, Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function—part 2. N Am J Sports Phys Ther. 2006;1:132-139 [PMC free article] [PubMed] [Google Scholar]
- 9. Cook G, Burton L, Kiesel K, Rose G, Bryant M. Movement—Functional Movement Systems: Screening, Assessment and Corrective Strategies. Santa Cruz, CA: On Target; 2010 [Google Scholar]
- 10. Cronin JB, Hansen KT. Strength and power predictors of sports speed. J Strength Cond Res. 2005;19:349-357 [DOI] [PubMed] [Google Scholar]
- 11. Duncan MJ, Stanley M. Functional movement is negatively associated with weight status and positively associated with physical activity in British primary school children. J Obes. 2012;2012:697563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Duncan MJ, Stanley M, Leddington Wright S. The association between functional movement and overweight and obesity in British primary school children. BMC Sports Sci Med Rehabil. 2013;5:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Frost DM, Beach TA, Callaghan JP, McGill SM. Using the Functional Movement Screen to evaluate the effectiveness of training. J Strength Cond Res. 2012;26:1620-1630 [DOI] [PubMed] [Google Scholar]
- 14. Golomer E, Fery YA. Unilateral jump behavior in young professional female ballet dancers. Int J Neurosci. 2001;110:1-7 [DOI] [PubMed] [Google Scholar]
- 15. Gribble PA, Hertel J, Plisky P. Using the star excursion balance test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47:339-357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hewit JK, Cronin JB, Hume PA. Asymmetry in multi-directional jumping tasks. Phys Ther Sport. 2012;13:238-242 [DOI] [PubMed] [Google Scholar]
- 17. Hoffman M, Schrader J, Applegate T, Koceja D. Unilateral postural control of the functionally dominant and nondominant extremities of healthy subjects. J Athl Train. 1998;33:319-322 [PMC free article] [PubMed] [Google Scholar]
- 18. Hrysomallis C. Balance ability and athletic performance. Sports Med. 2011;41:221-232 [DOI] [PubMed] [Google Scholar]
- 19. Hrysomallis C. Relationship between balance ability, training and sports injury risk. Sports Med. 2007;37:547-556 [DOI] [PubMed] [Google Scholar]
- 20. Hrysomallis C, McLaughlin P, Goodman C. Balance and injury in elite Australian footballers. Int J Sports Med. 2007;28:844-847 [DOI] [PubMed] [Google Scholar]
- 21. Kiesel K, Plisky P, Butler R. Functional movement test scores improve following a standardized off-season intervention program in professional football players. Scand J Med Sci Sports. 2011;21:287-292 [DOI] [PubMed] [Google Scholar]
- 22. Lin WH, Liu YF, Hsieh CC, Lee AJ. Ankle eversion to inversion strength ratio and static balance control in the dominant and non-dominant limbs of young adults. J Sci Med Sport. 2009;12:42-49 [DOI] [PubMed] [Google Scholar]
- 23. Lisman P, O’Connor FG, Deuster PA, Knapik JJ. Functional Movement Screen and aerobic fitness predict injuries in military training. Med Sci Sports Exerc. 2013;45:636-643 [DOI] [PubMed] [Google Scholar]
- 24. Marchetti PH, Hartigan EH, Duarte M. Comparison of the postural control performance of collegiate basketball players and nonathletes. Athl Train Sports Health Care. 2012;4:251-256 [Google Scholar]
- 25. Marchetti PH, Orselli MI, Duarte M. The effects of uni- and bilateral fatigue on postural and power tasks. J Appl Biomech. 2013;29:44-48 [DOI] [PubMed] [Google Scholar]
- 26. McElveen MT, Riemann BL, Davies GJ. Bilateral comparison of propulsion mechanics during single-leg vertical jumping. J Strength Cond Res. 2010;24:375-381 [DOI] [PubMed] [Google Scholar]
- 27. Minick KI, Kiesel KB, Burton L, Taylor A, Plisky P, Butler RJ. Interrater reliability of the functional movement screen. J Strength Cond Res. 2010;24:479-486 [DOI] [PubMed] [Google Scholar]
- 28. Noyes FR, Barber Westin SD. Anterior cruciate ligament injury prevention training in female athletes: a systematic review of injury reduction and results of athletic performance tests. Sports Health. 2012;4:36-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Okada T, Huxel KC, Nesser TW. Relationship between core stability, functional movement, and performance. J Strength Cond Res. 2011;25:252-261 [DOI] [PubMed] [Google Scholar]
- 30. Palmieri R, Ingersoll CD, Stone MB. Center-of-pressure parameters used in the assessment of postural control. J Sports Rehabil. 2002;11:51-66 [Google Scholar]
- 31. Parchmann CJ, McBride JM. Relationship between functional movement screen and athletic performance. J Strength Cond Res. 2011;25:3378-3384 [DOI] [PubMed] [Google Scholar]
- 32. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968-1978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36:911-919 [DOI] [PubMed] [Google Scholar]
- 34. Portney LG WM. Foundations of Clinical Research Applications to Practice. New Jersey: Alexander JL; 2009 [Google Scholar]
- 35. Schneiders AG, Davidsson A, Horman E, Sullivan SJ. Functional movement screen normative values in a young, active population. Int J Sports Phys Ther. 2011;6:75-82 [PMC free article] [PubMed] [Google Scholar]
- 36. Schneiders AG, Sullivan SJ, O’Malley KJ, Clarke SV, Knappstein SA, Taylor LJ. A valid and reliable clinical determination of footedness. PM R. 2010;2:835-841 [DOI] [PubMed] [Google Scholar]
- 37. Thompson W. American College of Sports Medicine’s Guidelines for Excerise Testing and Prescription. 8th Lippincott Williams and Wilkins; 2010 [Google Scholar]
- 38. Waldron M, Worsfold P, Twist C, Lamb K. Concurrent validity and test-retest reliability of a global positioning system (GPS) and timing gates to assess sprint performance variables. J Sports Sci. 2011;29:1613-1619 [DOI] [PubMed] [Google Scholar]
- 39. Zifchock RA, Davis I, Hamill J. Kinetic asymmetry in female runners with and without retrospective tibial stress fractures. J Biomech. 2006;39:2792-2797 [DOI] [PubMed] [Google Scholar]


