Abstract
Context:
Sport-related spleen and liver injuries pose a challenge for the physician. Although rare, these injuries can have serious and even life-threatening outcomes if not accurately diagnosed and managed in a timely fashion. Currently, there are no evidence-based guidelines on duration and intensity of restricted activity and return to play after spleen and liver injury. In addition, there is controversy on follow-up imaging after injury.
Evidence Acquisition:
PubMed was searched using the terms splenic or spleen and trauma and hepatic or liver and trauma from 1980 to 2013. The citations from sentinel papers were also reviewed.
Study Design:
Clinical review.
Level of Evidence:
Level 3.
Results:
Ultrasound is ideal in the unstable athlete. Nonoperative management of blunt splenic and hepatic injuries is recommended for hemodynamically stable patients regardless of injury grade, patient age, or presence of associated injuries. Follow-up imaging is not routinely recommended unless clinically indicated. Athletes may engage in light activity for the first 3 months after injury and then gradual return to unrestricted activity as tolerated. High-level athletes may choose splenectomy or serial imaging for faster return to play.
Conclusion:
Intravenous contrast-enhanced computed tomography is the diagnostic imaging modality of choice in stable athletes with blunt abdominal trauma.
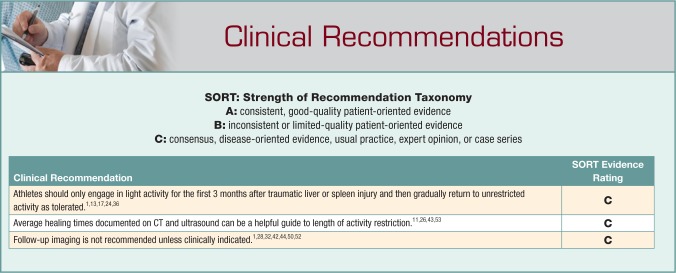
Strength-of-Recommendation Taxonomy:
C.
Keywords: guideline, return to play, spleen and liver injury
Abdominal injuries are rare in sports. However, unrecognized, they can be serious and even life threatening. Up to 10% of all abdominal injuries result from sport-related trauma.5,55 The spleen and liver are the 2 most commonly injured organs in blunt abdominal trauma, with splenic injuries leading the way.10,15,51 Injuries to the abdomen can occur in almost any sport but are more common in contact or collision sports. Injury to the spleen and the liver have occurred from tackling in football,34,39,51 checking in hockey,46 landing on a ball in rugby,38 a blow to the abdomen from a boogie board6 or lacrosse ball,18 and even in downhill skiing and snowboarding.4 Delayed splenic rupture 3 weeks after being crosschecked during an amateur hockey game has occurred.14 Therefore, return-to-play decisions after injury remain controversial.
Sideline Evaluation
Signs and symptoms of spleen and liver injuries can be very subtle, making it challenging for physicians to differentiate benign from life-threatening injuries. It is therefore crucial to have a high index of suspicion in any athlete complaining of abdominal pain or discomfort, particularly in those who have sustained trauma. Athletes may complain of pain radiating to the left or the right shoulder due to free intraperitoneal blood irritating the diaphragm (Kehr sign).35 Ecchymosis in the periumbilical region (Cullen sign)41 and the lateral abdominal wall (Gray Turner sign)41 are suggestive of hemoperitoneum, which may cause diffuse abdominal pain, rebound tenderness, and guarding.35,41 Bowel sounds may be lost; however, these are often late findings. Cardiovascular signs may be an earlier manifestation of hemorrhage from an injured intra-abdominal organ. Tachycardia must be distinguished from the physiological elevation associated with activity. Pulse volume can weaken and become “thready.”9 Diminished blood pressure signifies hypovolemia but is also unfortunately a late sign after significant blood loss has occurred. Body movement, for example, walking or running, may precipitate pain,9 and the lower ribs should be assessed for fracture. However, physical exam can be very unreliable as signs of injury may be delayed, making frequent serial assessments imperative.35,41 Of athletes with significant abdominal trauma, 50% have a negative initial exam, so reexamination can be crucial. Moreover, 20% of patients with an acute hemoperitoneum have an initial benign abdominal exam.25
The spleen is the most frequently injured organ and leading cause of death in sport-related abdominal trauma.41 Injury is typically caused by a direct blow to the left upper quadrant of the abdomen or left lower chest wall but has also occurred in open slope falls in snowsports.16 Injury to the spleen is classically described as left upper quadrant pain and tenderness to palpation. There may be tenderness over the ribs overlying the spleen. The athlete may also complain of pain radiating to the left or the right shoulder.41 Although not as common as splenic injuries, sport-related hepatic trauma can also have adverse outcomes. Liver injuries are caused by direct blows and deceleration mechanisms41 and usually occur after a blow to the right upper quadrant of the abdomen or the right lower chest. The ribs overlying the liver may also be tender.9
Review of symptoms and past medical history are also important in revealing predisposing factors for spleen and liver injuries.19 Infectious mononucleosis, malaria, hematologic disorders, and pregnancy can cause splenic enlargement and capsule thinning, making it more fragile.35
Abdominal wall injury often produces transient localized pain and dyspnea that get better when the underlying muscle spasm resolves. Injury to the underlying organs leads to persistent or worsening symptoms.41 If a physician suspects intra-abdominal injury, prompt transport to a nearby trauma center should be arranged. Definitive treatment should not be delayed by performing time-consuming measures in the field.9,41 Further description of sideline management of abdominal trauma may be obtained from the First Aid in Rugby online course,23 provided by the International Rugby Board, or equivalent field-side training manuals.
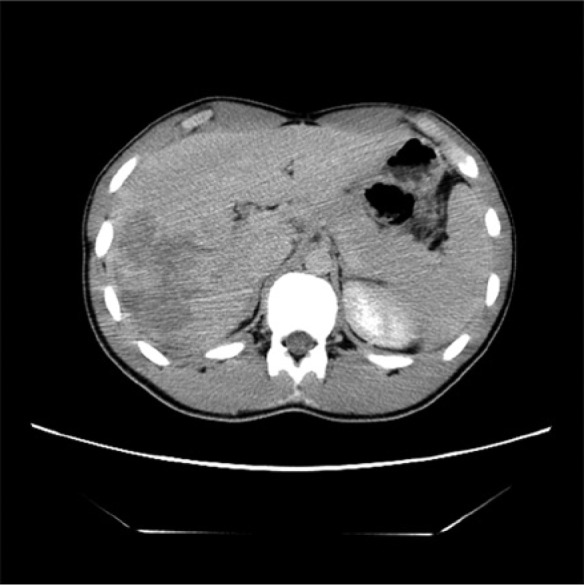
Diagnostic Imaging
Commuted tomography (CT) remains the gold standard in evaluating blunt abdominal trauma in hemodynamically stable patients3,19,40,45 and is the imaging modality of choice for diagnosing spleen and liver injuries (Figure 1).41 It has replaced ultrasonography in stable patients because it is more sensitive, provides accurate anatomic details, and allows for injury grading. Intravenous contrast-enhanced CT gives the most detailed information about organ injury (Figure 2)54 and is considered the optimal standard to diagnose splenic and hepatic injuries.12,56
Figure 1.
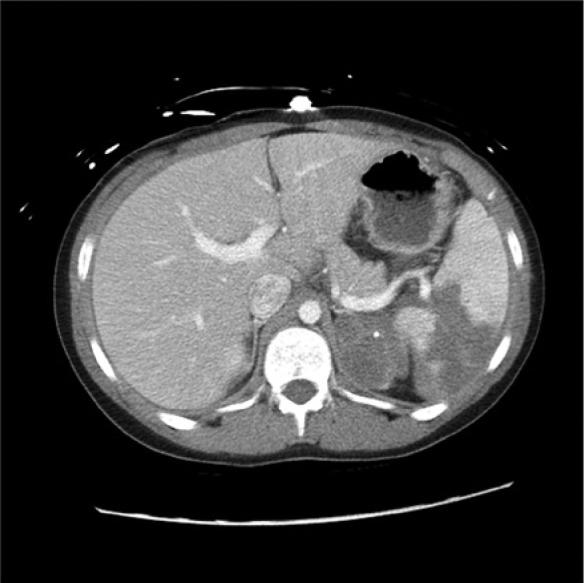
Computed tomography scan revealing a grade IV splenic laceration and moderate hemoperitoneum in a 14-year-old male kneed in the left upper quadrant of the abdomen during soccer.
Figure 2.
Computed tomography scan identifying a grade V splenic laceration with 50% hypoattenuation in a 14-year-old male who was kicked in the left flank during football. (a) Axial view and (b) coronal view.
The most widely used grading system for blunt splenic injury is the American Association for the Surgery of Trauma organ injury scale. Splenic injuries are graded on CT from I to V based on hematoma or laceration location, percentage of spleen involved, and hilar vasculature involvement (Figure 3).29 The recently developed Baltimore CT grading system for splenic injury integrates vascular injury into the score and supports clinical decision making, especially the need for angiography and embolization or surgery.31 Liver injuries are graded from I to VI on CT,29,33 with severity ranging from minor capsular tear without parenchymal injury to extensive disruption of both lobes (Figures 4-7).41
Figure 3.

Computed tomography scan demonstrating large hemoperitoneum (small arrow) and a grade IV-V splenic laceration with devascularization of the anterior aspect of the spleen (large arrow) in a 17-year-old male who sustained a left upper quadrant abdominal injury during ice hockey.
Figure 4.

Computed tomography scan revealing a large area of decreased attenuation in the liver, consistent with a grade V laceration in a 13-year-old female who fell while skiing. (a) Axial view and (b) coronal view.
Figure 5.
Computed tomography scan showing a grade IV liver laceration in a 15-year-old male who was run over by multiple dirt bikes in a race.
Figure 6.

Computed tomography scan identifying a grade III-IV splenic laceration and a grade I liver laceration in a 14-year-old male who struck his abdomen against his BMX bike handle bars.
Figure 7.

Computed tomography scan identifying a grade III hepatic laceration in a 17-year-old female complaining of right upper quadrant pain after being tackled in rugby. (a) Axial view and (b) coronal view.
Ultrasonography has a role in the diagnosis of abdominal trauma. It is operator dependent and less sensitive than CT, but it is an ideal choice in the hemodynamically unstable patient.2,20 Studies have shown a sensitivity of approximately 85% and a specificity of 99% in detecting intra-abdominal injuries.20 Although ultrasound can visualize free intraperitoneal fluid, it is poor at grading the injury and identifying the injured organ.54 Conditions identified on ultrasound in stable patients will eventually require CT to identify the injury and to guide management.54
Management
The current management practice for blunt spleen and liver injuries is selective operative and nonoperative treatment.22,47,48 The 2012 Eastern Association for the Surgery of Trauma (EAST) guidelines for the management of blunt splenic injury suggest nonoperative management (NOM) for the hemodynamically stable patient regardless of injury grade, patient age, or presence of associated injuries.48 The overall morbidity and mortality are very low. NOM should be considered in a setting where close monitoring and an operating room for urgent laparotomy are available. NOM may fail in patients aged 40 years or older, with splenic injury grade III or higher, and with an injury severity score of 25 or higher.30 Angiography with embolization continues to be an adjunctive therapy in NOM, along with repeat imaging based on changes in clinical status.48 Hemodynamically unstable patients or those with diffuse peritonitis should undergo immediate exploratory laparotomy.48 The 2012 EAST guidelines for the management of blunt hepatic injury are identical to those for blunt splenic injuries with adjunct interventions and include angiography, endoscopic retrograde cholangio pancreatography, endoscopy, and laparoscopy.47 Blunt trauma patients with concomitant splenic and hepatic injuries have a higher failure rate with NOM, requiring close monitoring.27
Return-To-Play Guidelines
There is a lack of consensus on recommendations for resuming full activity after blunt splenic and hepatic injuries.13,15,17,21,37,51 Controversy stems from an inability to accurately predict delayed complications and the time needed for full recovery.
Splenic Injury
Recommendations for resuming unrestricted activity after splenic injury vary from 3 weeks to greater than 6 months for severe injury.13,15,17,21,37,51 Clinical judgment is often the key determinant for EAST members making return-to-activity decisions.13 For mild splenic injuries, most restricted all activity for 2 weeks, allowing full activity by 6 weeks.13 Restrictions were stricter for severe injuries (grade III-V).13
Two professional hockey players with grade III spleen injury were managed conservatively with serial CTs until radiographic and clinical findings suggested complete healing.46 They returned to full-contact hockey within 2 months without any complications.46 Athletes who choose splenectomy often return to activity much sooner.51 Athletes with splenic injury have returned to unrestricted activity 3 weeks after splenectomy.37,51
Radiographic healing time is directly proportional to splenic injury grade.26 In the study by Lynch et al,26 CT-documented injury was identified by ultrasound for all patients, and patients returned to full activity with no long-term complications after ultrasound demonstrated healing (Table 1).
Table 1.
Mean time to ultrasound healing (weeks) by grade of splenic injury26
| Grade of Injury | Mean Time to Ultrasound Healing (Weeks) |
|---|---|
| I | 3.1 |
| II | 8.2 |
| III | 12.1 |
| IV | 20.7 |
Computed tomographic healing of splenic injury has occurred in 84% of patients at 2.5 months, regardless of initial severity.43
Delayed splenic rupture is the primary argument for follow-up imaging.19 Radiographic healing may lag physiologic healing.51 Therefore, routine follow-up abdominal CTs for blunt splenic injury are not necessary to allow patients to resume their normal activities after an appropriate time of restricted activity.1,42,44,52 Most recommend a 3-month period of activity restriction,1,35 with the first 3 weeks after discharge comprising light activity at home.17
Management and return-to-play decisions should be individualized. Athletes should be asymptomatic and back to baseline fitness before returning to unrestricted activity. Repeat imaging should be considered for unresolved or worsening symptoms. Referring to average healing times documented on CT can be a helpful guide to length of activity restriction. Serial CTs may be considered for high-level athletes on a case-by-case basis. However, the radiation exposure from multiple CTs should be considered.46 Ultrasound may be a less potentially harmful option when considering repeat imaging, especially if a CT-documented injury was identified on ultrasound. Elective splenectomy for high-level athletes to return to play sooner should not be the norm, as it is not without its consequences such as an increased risk of sepsis, particularly from encapsulated organisms such as pneumococcus.35 Postsplenectomy vaccination with pneumococcal and meningococcal vaccines is recommended.8
Liver Injury
The literature on activity restriction and return to play after liver injury is scarce. Healing of a simple liver laceration and subcapsular hematoma occurs in 2 to 4 months, whereas complex injuries require up to 6 months.24 The healing time for hepatic lacerations is different from subcapsular hematomas (Table 2).53
Table 2.
Healing time by grade and type of liver injury53
| Grade of Liver Injury | Type of Liver Injury | Healing Time (Days) |
|---|---|---|
| I | Hematoma | 6 |
| II | Hematoma | 16 |
| II | Laceration | 29 |
| III | Laceration | 34 |
| III | Hematoma | 108 |
| IV | Laceration | 78 |
Some recommend return to unrestricted activity only after a normal CT, usually 3 to 6 months after injury.7,49 Although CT documentation of resolution was once standard of care, follow-up CT is no longer recommended unless clinically indicated.1,28,32,44,50
Basic principles should be used to guide return-to-play decisions. In addition to return to baseline, the athlete should not compete until anatomic and functional healing occurs. Normalization of liver enzymes may be indicators of functional healing.34,41 Anatomic healing times documented by CT may also help guide return-to-play decisions. Just as with splenic injury, serial CTs with conservative management for high-level athletes can be considered with the knowledge of an increased risk of radiation.
Conclusion
Although abdominal injuries are uncommon in sports, frequent assessments are necessary to determine an athlete’s status, especially the need for immediate intervention and transport to the hospital.41 Intravenous contrast-enhanced CT is the diagnostic imaging modality of choice in stable athletes presenting with blunt abdominal trauma.3,19,40,41,45 Ultrasound is ideal in the unstable athlete.2,20 NOM for hemodynamically stable patients continues to be the norm.47,48 There is no consensus on the duration and intensity of restricted activity after spleen and liver injury.13,15,17,21,37,51 Athletes may engage in light activity for the first 3 months after injury and then gradually return to unrestricted activity as tolerated.13,17,41 Follow-up imaging is not routinely recommended unless clinically indicated.1,28,32,44,50 High-level athletes may choose splenectomy or serial imaging to return to play faster; however, the risks and benefits of these measures need to be considered.46,51
Footnotes
The following author declared potential conflicts of interest: Hamish A. Kerr, MD, is the Team Physician at Siena College.
References
- 1. Allins A, Ho T, Nguyen TH, Cohen M, Waxman K, Hiatt JR. Limited value of routine follow-up CT scans in nonoperative management of blunt liver and splenic injuries. Am Surg. 1996;62:883-886 [PubMed] [Google Scholar]
- 2. Amaral JF. Thoracoabdominal injuries in the athlete. Clin Sports Med. 1997;16:739-753 [DOI] [PubMed] [Google Scholar]
- 3. Amoroso TA. Evaluation of the patient with blunt abdominal trauma: an evidence based approach. Emerg Med Clin North Am. 1999;17:63-65 [DOI] [PubMed] [Google Scholar]
- 4. Arisawa F, Kogure K, Tsuzuki Y, et al. Snowboarding splenic injury: four case reports. Injury. 2002;33:173-177 [DOI] [PubMed] [Google Scholar]
- 5. Berqvist D, Hedelin H, Karlsson G, et al. Abdominal trauma during thirty years: analysis of a large case series. Injury. 1981;13:93-99 [DOI] [PubMed] [Google Scholar]
- 6. Choo KL, Hansen JB, Bailey DM. Beware the boogie board: blunt abdominal trauma from bodyboarding. Med J Aust. 2002;176:326-327 [DOI] [PubMed] [Google Scholar]
- 7. Cywes S, Rode H, Millar AJ. Blunt liver trauma in children: nonoperative management. J Pediatr Surg. 1985;20:14-18 [DOI] [PubMed] [Google Scholar]
- 8. Di Sabatino A, Carsetti R, Corazza GR. Post-splenectomy and hyposplenic states. Lancet. 2011;378:86-97 [DOI] [PubMed] [Google Scholar]
- 9. Diamond DL. Sports-related abdominal trauma. Clin Sports Med. 1989;8:91-99 [PubMed] [Google Scholar]
- 10. El-Osta H. Delayed splenic rupture: myth or reality? Ann Intern Med. 2009;150:224-225 [DOI] [PubMed] [Google Scholar]
- 11. Emery KH, Babcock DS, Borgman AS, Garcia VF. Splenic injury diagnosed with CT: US follow-up and healing rate in children and adolescents. Radiology. 1999;212:515-518 [DOI] [PubMed] [Google Scholar]
- 12. Fang JF, Wong YC, Lin BC, Hsu YP, Chen MF. The CT risk factors for the need of operative treatment in initially hemodynamically stable patients after blunt hepatic trauma. J Trauma. 2006;61:547-554 [DOI] [PubMed] [Google Scholar]
- 13. Fata P, Robinson L, Fakhry SM. A survey of EAST member practices in blunt splenic injury: a description of current trends and opportunities for improvement. J Trauma. 2005;59:836-842 [DOI] [PubMed] [Google Scholar]
- 14. Flik K, Callahan LR. Delayed splenic rupture in an amateur hockey player. Clin Sport Med. 1998;8:309-310 [DOI] [PubMed] [Google Scholar]
- 15. Gaines BA. Intra-abdominal solid organ injury in children: diagnosis and treatment. J Trauma. 2009;67:135-138 [DOI] [PubMed] [Google Scholar]
- 16. Gammons M, Boynton M, Russell J, Wilkens K. On-mountain coverage of competitive skiing and snowboarding events. Curr Sports Med Rep. 2011;10:140-146 [DOI] [PubMed] [Google Scholar]
- 17. Gandhi RR, Keller MS, Schwab CW, Stafford PW. Pediatric splenic injury: pathway to play? J Pediatr Surg. 1999;34:55-59 [DOI] [PubMed] [Google Scholar]
- 18. Gangemi JJ, Binns OA, Young JS. Splenic injury after athletic trauma: a case report of splenic rupture induced by a lacrosse ball. J Trauma. 1999;46:736-737 [DOI] [PubMed] [Google Scholar]
- 19. Gannon EH, Howard T. Splenic injuries in athletes: a review. Curr Sports Med Rep. 2010;9:111-114 [DOI] [PubMed] [Google Scholar]
- 20. Hoffman R, Nerlich M, Muggia-Sullam M, et al. Blunt abdominal trauma in cases of multiple trauma evaluated by ultrasonography: a prospective analysis of 291 patients. J Trauma. 1992;32:452-458 [DOI] [PubMed] [Google Scholar]
- 21. Huebner S, Reed MH. Analysis of the value of imaging as part of the follow-up of splenic injury in children. Pediatr Radiol. 2001;31:852-855 [DOI] [PubMed] [Google Scholar]
- 22. Hurtuk M, Reed RL, 2nd, Esposito TJ, Davis KA, Luchette FA. Trauma surgeons practice what they preach: the NTDB story on solid organ injury management. J Trauma. 2006;61:243-255 [DOI] [PubMed] [Google Scholar]
- 23. International Rugby Board. First Aid in Rugby. Player welfare. http://www.irbplayerwelfare.com/?documentid=module&module=9. Accessed March 2, 2013
- 24. Karp MP, Cooney DR, Pros GA, et al. The nonoperative management of pediatric hepatic trauma. J Pediatr Surg. 1983;18:512-518 [DOI] [PubMed] [Google Scholar]
- 25. Kerr HA, Curtis C, d’Hemecourt PA. Thoracoabdominal injuries. In: Micheli LJ, Powell L. (eds). The Adolescent Athlete: A Practical Approach. New York, NY: Springer Science & Business Media; 2007:141-164 [Google Scholar]
- 26. Lynch JM, Meza MP, Newman B, Gardner MJ, Albanese CT. Computed tomography grade of splenic injury is predictive of the time required for radiographic healing. J Pediatr Surg. 1997;32:1093-1096 [DOI] [PubMed] [Google Scholar]
- 27. Malhotra AK, Latifi R, Fabian TC, et al. Multiplicity of solid organ injury: influence on management and outcomes after blunt abdominal trauma. J Trauma. 2003;54:925-929 [DOI] [PubMed] [Google Scholar]
- 28. Meredith JW, Young JS, Bowling J, et al. Nonoperative management of blunt hepatic trauma: the exception to the rule? J Trauma. 1994;36:529-535 [DOI] [PubMed] [Google Scholar]
- 29. Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). J Trauma. 1995;38:323-324 [DOI] [PubMed] [Google Scholar]
- 30. Olthof DC, Joosse P, van der Vlies CH, de Haan RJ, Goslings JC. Prognostic factors for failure of nonoperative management in adults with blunt splenic injury: a systematic review. J Trauma Acute Care Surg. 2013;74:546-557 [DOI] [PubMed] [Google Scholar]
- 31. Olthof DC, van der Vlies CH, Scheerder MJ, et al. Reliability of injury grading systems for patients with blunt splenic trauma. Injury. 2014;45:146-150 [DOI] [PubMed] [Google Scholar]
- 32. Pachter HL, Knudson MM, Esrig B, et al. The status of nonoperative management of blunt hepatic injuries in 1995: a multicenter experience with 404 patients. J Trauma. 1996;40:31-38 [DOI] [PubMed] [Google Scholar]
- 33. Parks RW, Chrysos E, Diamond T. Management of liver trauma. Br J Surg. 1999;86:1121-1135 [DOI] [PubMed] [Google Scholar]
- 34. Parmelee-Peters K, Moeller JL. Liver trauma in a high school football player. Curr Sports Med Rep. 2004;3:95-99 [DOI] [PubMed] [Google Scholar]
- 35. Peitzman AB, Ford HR, Harbrecht BG, et al. Injury to the spleen. Curr Prob Surg. 2001;38:921-1008 [DOI] [PubMed] [Google Scholar]
- 36. Pranikoff T, Hirschl RB, Schlesinger AE, Polley TZ, Coran AG. Resolution of splenic injury after nonoperative management. J Pediatr Surg. 1994;29:1366-1369 [DOI] [PubMed] [Google Scholar]
- 37. Pucci E, Brody F, Zemon H, et al. Laparoscopic splenectomy for delayed splenic rupture after embolization. J Trauma. 2007;63:687-690 [DOI] [PubMed] [Google Scholar]
- 38. Quinlan JF, McCarthy CJ, McGlone B, Magee DJ. High grade splenic rupture in an elite Rugby Union player. J Sports Med Phys Fitness. 2010;50:68-71 [PubMed] [Google Scholar]
- 39. Ray R, Lemire JE. Liver laceration in an intercollegiate football player. J Athl Train. 1995;30:324-326 [PMC free article] [PubMed] [Google Scholar]
- 40. Richardson MC, Hollman AS, Davis CF. Comparison of computed tomography and ultrasonographic imaging in the assessment of blunt abdominal trauma in children. Br J Surg. 1997;84:1144-1146 [PubMed] [Google Scholar]
- 41. Rifat SF, Gilvydis RP. Blunt abdominal trauma in sports. Curr Sports Med Rep. 2003;2:93-97 [DOI] [PubMed] [Google Scholar]
- 42. Rovin JD, Alford BA, McIlhenny TJ, Burns RC, Rodgers BM, McGahren ED. Follow-up abdominal computed tomography after splenic trauma in children may not be necessary. Am Surg. 2001;67:127-130 [PubMed] [Google Scholar]
- 43. Savage SA, Zarzaur BL, Magnotti LJ, et al. The evolution of blunt splenic injury: resolution and progression. J Trauma. 2008;64:1085-1092 [DOI] [PubMed] [Google Scholar]
- 44. Sharma OP, Oswanski MF, Singer D. Role of repeat computerized tomography in nonoperative management of solid organ trauma. Am Surg. 2005;71:244-249 [PubMed] [Google Scholar]
- 45. Shuman WP. CT of blunt abdominal trauma in adults. Radiology. 1997;205:297-306 [DOI] [PubMed] [Google Scholar]
- 46. Silvis ML, Plakke MJ, Tice JG, Black KP. Splenic lacerations and return to play: case report of 2 professional hockey players. Sports Health. 2012;4:232-235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Stassen NA, Bhullar I, Cheng JD, et al. ; Eastern Association for the Surgery of Trauma. Nonoperative management of blunt hepatic injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(suppl 4):S288-S293 [DOI] [PubMed] [Google Scholar]
- 48. Stassen NA, Bhullar I, Cheng JD, et al. ; Eastern Association for the Surgery of Trauma. Selective nonoperative management of blunt splenic injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(suppl 4):S294-S300 [DOI] [PubMed] [Google Scholar]
- 49. Stricker PR, Hardin BH, Puffer JC. An unusual presentation of liver laceration in a 13-yr-old football player. Med Sci Sports Exerc. 1993;25:667-672 [PubMed] [Google Scholar]
- 50. Stylianos S. Evidence-based guidelines for resource utilization in children with isolated spleen or liver injury. The APSA Trauma Committee. J Pediatr Surg. 2000;35:164-167 [DOI] [PubMed] [Google Scholar]
- 51. Terrell TR, Lundquist B. Management of splenic rupture and return-to-play decisions in a college football player. Clin Sport Med. 2002;12:400-402 [DOI] [PubMed] [Google Scholar]
- 52. Thaemert BC, Cogbill TH, Lambert PJ. Nonoperative management of splenic injury: are follow-up computed tomographic scans of any value? J Trauma. 1997;43:748-751 [DOI] [PubMed] [Google Scholar]
- 53. Tiberio GA, Portolani N, Coniglio A, et al. Evaluation of the healing time of non-operatively managed liver injuries. Hepatogastroenterology. 2008;55:1010-1012 [PubMed] [Google Scholar]
- 54. Walter KD. Radiographic evaluation of the patient with sport-related abdominal trauma. Curr Sports Med Rep. 2007;6:115-119 [DOI] [PubMed] [Google Scholar]
- 55. Wan J, Corvino TF, Greenfield SP, et al. The incidence of recreational genitourinary and abdominal injuries in the western New York pediatric population. J Urol. 2003;170:1525-1527 [DOI] [PubMed] [Google Scholar]
- 56. Willmann JK, Roos JE, Platz A, et al. Multidetector CT: detection of active hemorrhage in patients with blunt abdominal trauma. AJR Am J Roentgenol. 2002;179:437-444 [DOI] [PubMed] [Google Scholar]