Abstract
Background
This paper presents two replications of a heuristic model for measuring environment in studies of gene-environment interplay in the etiology of young adult problem behaviors.
Methods
Data were drawn from two longitudinal, U.S. studies of the etiology of substance use and related behaviors: the Raising Healthy Children study (RHC; N = 1,040, 47% female) and the Minnesota Twin Family Study (MTFS; N = 1,512, 50% female). RHC included a Pacific Northwest, school-based, community sample. MTFS included twins identified from state birth records in Minnesota. Both studies included commensurate measures of general family environment and family substance-specific environments in adolescence (RHC ages 10–18; MTFS age 18), as well as young adult nicotine dependence, alcohol and illicit drug use disorders, HIV sexual risk behavior, and antisocial behavior (RHC ages 24, 25; MTFS age 25).
Results
Results from the two samples were highly consistent and largely supported the heuristic model proposed by Bailey et al. (2011). Adolescent general family environment, family smoking environment, and family drinking environment predicted shared variance in problem behaviors in young adulthood. Family smoking environment predicted unique variance in young adult nicotine dependence. Family drinking environment did not appear to predict unique variance in young adult alcohol use disorder.
Conclusions
Organizing environmental predictors and outcomes into general and substance-specific measures provides a useful way forward in modeling complex environments and phenotypes. Results suggest that programs aimed at preventing young adult problem behaviors should target general family environment and family smoking and drinking environments in adolescence.
Keywords: replication, problem behavior, nicotine dependence, alcohol misuse, measuring environment for GxE
1. INTRODUCTION
Tobacco dependence and alcohol use disorders carry serious health and social consequences with significant personal and economic costs. Tobacco and alcohol problems often co-occur with each other (Hawkins et al., 2002; Hughes et al., 2000; Jackson et al., 2005) and with other problem behaviors, particularly criminal or antisocial behaviors (Krueger et al., 2002; McGue et al., 2006), illicit drug use (Bailey et al., 2006; Tsuang et al., 2001; Young et al., 2006), and risky sexual behavior (Bailey et al., 2011; Iacono et al., 1999; Kanh et al., 2012). Research suggests that the development of tobacco and alcohol dependence and comorbid problems is influenced by both environmental and genetic factors (Kreek et al., 2005; Rutter et al., 2006), including environmental and genetic main effects, gene-environment interactions (GxE), and gene-environment correlations (rGE). Understanding the etiology of adult tobacco and alcohol misuse requires measuring and defining these phenotypes and modeling a complex array of interacting genetic and environmental risk and protective factors.
To reduce the complexity of analyses of gene-environment interplay in understanding problem behavior, some authors suggest simplifying strategies for measuring environment. One common strategy is to pick a single, powerful environmental exposure, like childhood abuse (Moffitt et al., 2006). A second strategy involves combining multiple environmental pathogens into an index of environmental risk (Blomeyer et al., 2006). Strengths of these methods include their parsimony in measuring environment and, given well-chosen environmental exposures, their likelihood of identifying GxE if it is present. These methods, however, do not reflect the state of knowledge about the complex, multidimensional nature of environmental influences on problem behavior. Nor do they provide clear implications for treatment or prevention.
1.1. Model to be replicated
Bailey et al. (2011) presented an alternative model for simplifying complex, multidimensional measures of the environment for studies of gene-environment interplay in the etiology of problem behavior. They advocated using a general versus substance-specific framework to conceptualize substance use phenotypes and environmental predictors. Using latent variable modeling, they partitioned variance in nicotine dependence (ND), alcohol use disorder (AUD), and illicit drug use disorder (IDUD) symptom counts; crime; and HIV sexual risk behavior (SRB) into shared and substance-specific, or unique residual, variance. Similarly, latent variables organized environmental risk in adolescence into positive general family environment (e.g., good family management, strong bonding) and substance-specific family environment (e.g., parent and sibling use, parent attitudes) factors. This framework allowed the simultaneous examination of processes related to co-occurring problem behaviors and processes uniquely related to a particular substance or behavior. It also allowed the distillation of multiple measures of complex environments into a small number of simplified yet multidimensional measures.
Bailey et al. (2011) found support for the proposed framework using data from the Seattle Social Development Project (SSDP; Hawkins et al., 2005, 2008). Specifically, good general adolescent family environment and general problem behavior in young adulthood (age 24) were negatively related. Adolescent family smoking and drinking environments predicted unique variance in young adult ND and AUD, respectively. Neither substance-specific family environment measure was related to unique variance in the other young adult problem behaviors. An extension of this model to problem behavior among SSDP participants at age 33 largely replicated the pattern of findings (Epstein et al., 2013). Although supported in both studies, the model may have been sample dependent.
1.2. A “test and replicate” model of collaboration
Reproducibility of findings is a foundation of scientific inquiry, but concerns abound regarding publication bias and the lack of systematic replication of findings in psychology and other social sciences (Bakker et al., 2012; Makel et al., 2012; Pashler and Wagenmakers, 2012). Many argue that, to address these issues, more authors should attempt to replicate new findings using well-powered studies (Bakker et al., 2012). In general, the suggested strategies for replication have focused on and are most clearly applicable to cross-sectional or short-term, pre-post experimental designs. Long-term longitudinal and etiological studies are extremely difficult to replicate closely, given their scale and complexity.
For those who wish to examine genetic as well as environmental influences on substance use using longitudinal data, options for replication are limited. In 2011, our two research groups, the Social Development Research Group at the University of Washington, and the Minnesota Center for Twin and Family Research at the University of Minnesota, began a collaborative investigation of gene-environment interplay in the etiology of substance use and general problem behavior using several datasets available at the two sites. Our collaborative model involves a test and replicate strategy, where predictive models are developed and tested in one sample, and then replicated in the remaining samples.
This paper presents two replications, in independent samples, of the Bailey et al. (2011) conceptual model of general and substance-specific environmental influences. Data are drawn from the Raising Healthy Children study (RHC) and the Minnesota Twin Family Study (MTFS).
2. METHOD
2.1. Participants
2.1.1. RHC
RHC is a longitudinal study of students attending 10 public schools in a suburban Pacific Northwest U.S. school district. It is a study of the etiology of positive and problem behaviors with a randomized test of a preventive intervention nested within it (see Brown et al., 2005; Haggerty et al., 2006 for a detailed overview). It was designed as a replication and extension of the SSDP study. The sample includes 1,040 individuals (76% of those eligible; 47% female) who were age 5 (younger cohort) or 6 (older cohort) in 1993. Annual data collection was conducted in the spring through 2011, when participants were age 24/25. The sample was 75% White, 7% Asian or Pacific Islander, 4% African American, 2% Native American, and 12% mixed race; 9% of participants were Hispanic/Latino(a). Unlike MTFS, which is a twin study (see below), RHC did not target twins or siblings. Thus, the majority of youth were unrelated; however, the sample did include 102 siblings (full, half, step siblings; see section 2.4 Analysis).
Retention rates ranged from 85% to 94% in the years from which age 10–18 family environment data were drawn. A total of 923 individuals (89% of the original sample) participated in 2010 (younger cohort age 23, older cohort age 24) and 917 (88%) participated in 2011, the years from which outcome data were drawn. Retention was not related to gender, age, or race. Participants in the intervention group (89% versus 93% of controls) or in the older cohort (86% versus 97% in the younger cohort) were less likely to be retained in young adulthood.
2.1.2. MTFS
MTFS is a study of the development and etiology of substance use and related behaviors (see Iacono et al., 1999 for a detailed overview). Twins born in the state of Minnesota between 1977 and 1984 and their parents were recruited to participate the year the twins turned 11 years old. Families were identified using birth certificates, which are publicly available in Minnesota. Approximately 90% of twin families were successfully located and contacted to determine study eligibility. Eligible participants lived within a day’s drive of the lab. Exclusion criteria included any mental or physical handicap and adoption of the twins by nonrelatives (determined by a prescreen telephone interview with one parent, usually the mother). About 84% of eligible families agreed to participate. Most twins (95%) were Caucasian (2% Native American, 1% Asian/Pacific Islander, < 1% Black, Hispanic/Latino(a), Other/Mixed), matching the region from which they were sampled in the relevant birth years (Iacono et al., 1999). Out of 756 pairs of twins, 270 were dizygotic (DZ) and 486 were monozygotic (MZ). All twin pairs were same sex.
A total of 1,512 participants completed the first assessment (756 sets of twins 49.7% male; M age = 11.7, SD = .43). Retention was 87% and 88%, respectively, at the two interviews from which the present data were drawn: the second follow-up (FU2; M age = 18.2, SD = .70) and the fourth follow-up (FU4; M age = 25.3, SD = .74). Attrition was not related to child sex or race/ethnicity, except males were less likely than females to participate at FU4.
2.2 Procedures
2.2.1. RHC
Study procedures were approved by the University of Washington Institutional Review Board. Parents gave written permission for their minor child to participate and minor children assented each year. Parents and young adults over age 18 gave consent at each survey time point. Through 2006 (younger cohort age 19, older cohort age 20), surveys were administered in person. Questions about sexual behavior were self-administered. After 2006, about two thirds of the sample completed the survey over the Internet and one third was interviewed in person. A randomized trial of this multimode survey administration indicated no differences in rates of reported sexual activity or risk behavior by survey mode (McMorris et al., 2009).
2.2.2. MTFS
Procedures were approved by the University of Minnesota Institutional Review Board. Twins and their parents provided written consent to participate at each assessment; parents provided written permission for children under the age of 18. A variety of measures were completed at each time point, including diagnostic interviews, self-report surveys, and computerized assessments. If twins could not be scheduled for an in-person follow-up visit (21% at FU2, 16% at FU4), they were interviewed by phone and completed all assessments.
2.3 Measures
Online supplementary materials1 describe items used, scale reliabilities, ages of administration, and correspondence with the Bailey et al. (2011) study measures. Some items differed across studies; however, congeneric measures of key constructs were available. Family environment measures in RHC were assessed yearly when target youth were ages 10 to 18 and averaged across adolescence. In MTFS, family environment measures were obtained when twins were age 18.
2.3.1. General family environment
Indicators of general family environment included bonding to family members, management, conflict, and positive involvement. In RHC, these constructs were reported by youth. In MTFS, relevant items were administered to the twins and drawn from the Parent Environment Questionnaire (PEQ; Elkins et al., 1997) and the Family Adaptability and Cohesion Evaluation Scales (FACES III; Olson et al., 1985). Child ratings of mother and father from the PEQ were averaged.
2.3.2. Family drinking environment
Indicators of family drinking environment in RHC included parent drinking attitudes, parent and sibling drinking, and involvement of the youth in family member drinking (e.g., getting or opening a drink for a family member). Family drinking environment measures were parent reported except for sibling drinking, which was reported by the target youth. In MTFS, measures of family drinking environment included self-reported co-twin and parent drinking and were assessed using the Substance Abuse Module (SAM; Robins et al., 1987), an expanded version of the CIDI (Robins et al., 1988). Items measuring parent attitudes about drinking were not available; however an item indexing perceived pressure to drink from the co-twin was included in the measure of sibling drinking. Maternal and paternal alcohol use was averaged.
2.3.3. Family smoking environment
Parent smoking, sibling smoking, and involvement of youth in family member smoking (getting or lighting cigarettes for family members) were indicators of family smoking environment in RHC. One parent per family reported their own and their partner’s smoking and any involvement of the target child in family member smoking. Sibling smoking was reported by target youth. MTFS measures of self-reported co-twin and parent smoking were obtained using the SAM (Robins et al., 1987). An item indexing perceived pressure to smoke from the co-twin was included in the sibling smoking measure. Maternal and paternal reports of smoking were averaged.
2.3.4. Problem behaviors at age 24/25
In both studies, problem behaviors included ND, AUD, and IDUD DSM-IV symptom counts (American Psychiatric Association, 1994); antisocial behavior; and HIV SRB. In RHC, ND symptoms were measured using the Diagnostic Interview Schedule (Robins et al., 1981; 1989) in 2011 when the younger cohort was age 24 and the older cohort was age 25. All other problem behaviors were measured at age 24 for both cohorts. AUD and IDUD symptom counts were measured using the World Health Organization International Composite Diagnostic Interview (CIDI; World Health Organization, 1990). HIV SRB measures assessed having three or more sex partners in the past year, using condoms inconsistently with the last three sexual partners, being involved in prostitution, and having used alcohol or other drugs before having sex half of the time or more often. Scores represented a count of the number of sex risk behaviors reported (possible range 0–4). Antisocial behavior was operationalized as past-year involvement in crime, and was measured by self-report of engagement in a series of minor delinquency, property crime, drug crime, and violent crime acts in the past year. The number of crimes reported was summed.
In MTFS, ND, AUD, and IDUD symptoms were assessed using a modified version of the SAM (Robins et al., 1987). Antisocial behavior was operationalized as DSM-IV Antisocial Personality Disorder Criterion A (AAB) symptoms, and was assessed using a version of the Structured Clinical Interview for Personality Disorders (Spitzer et al., 1987) modified to cover DSM-IV symptoms. Structured diagnostic interviews were conducted by trained clinical interviewers. The measures of HIV SRB assessed past-year engagement in SRB under the influence of drugs and alcohol and number of sexual partners (casual and committed, lifetime and last 12 months). These two measures (sex under the influence and number of lifetime sexual partners) were standardized and summed to create a single measure of risky sex.
Both studies used community samples. As would be expected, few respondents in either study reported high numbers of ND, AUD, or IDUD symptoms or criminal/antisocial behaviors. For example, only 5% to 13% of RHC participants and 1% to 5% of MTFS participants reported more than four symptoms for any of the DSM-IV disorders measured. For this reason and to mirror procedures used in Bailey et al. (2011), all symptom counts were capped at four.
2.3.5. Control variables
Control variables included child sex, race/ethnicity, and socioeconomic status (SES) for the family of origin. The RHC race/ethnicity measure combined parent reports, school records, and repeated self-reports; the MTFS race/ethnicity measure was a summation of repeated self-reports. Family of origin SES was measured in RHC by parent-reported eligibility for the National School Lunch/School Breakfast program between grades 5–7 and in MTFS by a composite of parent reports of mother’s and father’s education level, highest occupational prestige rating, and income.
2.4. Analysis
Correlation coefficients and structural equation models were estimated using Mplus version 6 (MTFS) and 7 (RHC; Muthén and Muthén, 1998–2011). Categorical variables were specified as such for both types of analysis. We used the Weighted Least Squares Means Variances (WLSMV) estimator and Theta parameterization, which allows for the estimation of residuals for categorical variables (Muthén and Muthén, 1998–2011). Full Information Maximum Likelihood estimation was used to minimize bias due to missing data. In RHC, the DIFFTEST option and multiple-group modeling were used to check the appropriateness of pooling treatment and control groups and older and younger cohorts for analysis. We found no differences in model parameters between treatment and control groups or between younger and older cohorts; all RHC participants were pooled for analysis. The analyses presented here included the 102 RHC siblings. Supplementary analyses including only one child per family (not shown) tested for differences due to sibling nesting within family. Patterns of significance were identical and parameter estimates were highly similar; most differed slightly at the second or third decimal place. Analyses of MTFS data accounted for clustering of twins within families using the COMPLEX specification.
3. RESULTS
Descriptive information and correlations are presented in Table 1 (RHC) and Table 2 (MTFS). In RHC, 35% of participants reported at least one ND symptom, 48% reported at least one AUD symptom, 39% reported at least one IDUD symptom, 19% reported at least one criminal activity, and 58% reported at least one SRB in young adulthood. In MTFS, 36% of participants reported at least one ND symptom, 35% reported at least one AUD symptom, 18% reported at least one IDUD symptom, and 57% reported at least one AAB symptom.
Table 1.
Correlations and descriptive statistics for variables in RHC.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Fam management | - | |||||||||||||||
| 2. Fam conflict | −.65* | - | ||||||||||||||
| 3. Involvement | .73* | −.54* | - | |||||||||||||
| 4. Bonding | .73* | −.60* | −.72* | - | ||||||||||||
| 5. Sib Smoking | −.20* | .16* | −.19* | −.19* | - | |||||||||||
| 6. Par Smoking | −.07* | .13* | −.17* | −.15* | .23* | - | ||||||||||
| 7. Involvement in par smoking | −.03 | .05* | −.06* | −.03 | .16* | −.28* | - | |||||||||
| 8. Sib drinking | −.25* | .19* | −.22* | −.19* | .73* | .16* | .05 | - | ||||||||
| 9. Par drinking | −.06 | .10* | −.06 | −.07* | .11* | .27* | .09* | .15* | - | |||||||
| 10. Pro drink attitudes | −.07* | .11* | −.07* | −.07* | .04 | .22* | .17* | .06 | .46* | - | ||||||
| 11. Involvement in par drinking | −.03 | .06* | .00 | −.01 | −.00 | .06 | .41* | −.00 | .30* | .22* | - | |||||
| 12. Risky sex | −.10* | .09* | −.08 | −.07 | .05 | .02 | .02 | .10* | .02 | .02 | .03 | - | ||||
| 13. Crime | −.18* | .24* | −.21* | −.17* | .13* | .14* | .15* | .19* | .11* | .05 | .08* | .33* | - | |||
| 14. ND symptoms | −.17* | .26* | −.21* | −.19* | .27* | .23* | .10* | .22* | .10* | .07 | .06 | .10* | .42* | - | ||
| 15. AUD symptoms | −.17* | .15* | −.16* | −.16* | .19* | .08 | .00 | .19* | .11* | .13* | .02 | .28* | .46* | .36* | - | |
| 16. IDUD symptoms | −.27* | .30* | −.28* | −.26* | .24* | −17* | .07 | .27* | .17* | .11* | .06 | .16* | .57* | .64* | .45* | - |
| M | 3.29 | 2.06 | 2.82 | 3.01 | .21 | .03 | 1.10 | .22 | .01 | 1.71 | 1.15 | .70 | .30 | .88 | 1.21 | 1.06 |
| SD | .37 | .48 | .50 | .46 | .30 | .60 | .25 | .27 | .50 | .44 | .26 | .70 | .76 | 1.36 | 1.52 | 1.55 |
p < .05
NOTE: Fam = family, Sib = sibling, Par = parent, ND = nicotine dependence, AUD = alcohol use disorder, IDUD = illicit drug use disorder.
Table 2.
Correlations and descriptive statistics for variables in MTFS.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Fam management | -- | ||||||||||||
| 2. Fam conflict | −.55* | -- | |||||||||||
| 3. Involvement | .43* | −.38* | -- | ||||||||||
| 4. Bonding | .70* | −.63* | .48* | -- | |||||||||
| 5. Co-twin smoking | −.19* | .12* | −.20* | −.08* | -- | ||||||||
| 6. Par smoking | −.10* | .04 | −.08 | .00 | .23* | -- | |||||||
| 7. Co-twin drinking | −.18* | .12* | −.13* | −.06 | .59* | .09* | -- | ||||||
| 8. Par drinking | −.03 | −.01 | .01 | .06 | .14* | .31* | .21* | -- | |||||
| 9. Risky sex | −.16* | .24* | −.11* | −.15* | .21* | .05 | .30* | .11* | -- | ||||
| 10. AAB symptoms | −.20* | .20* | −.11* | −.16* | .27* | .14* | .33* | .13* | .50* | -- | |||
| 11. ND Symptoms | −.20* | .20* | −.14* | −.08* | .48* | .23* | .35* | .13* | .32* | .48* | -- | ||
| 12. AUD symptoms | −.16* | .22* | −.13* | −.13* | .23* | .05 | .30* | .14* | .49* | .67* | .46* | -- | |
| 13. IDUD symptoms | −.11* | .17* | −.02 | −.08 | .25* | .15* | .27* | .07 | .41* | .66* | .49* | .56* | -- |
| M | .00 | −.00 | −.00 | .00 | .01 | .06 | .06 | −.04 | .05 | .82 | .88 | .75 | .45 |
| SD | .68 | .74 | .68 | .75 | 2.43 | 3.47 | 3.23 | 4.24 | 1.70 | .92 | 1.35 | 1.26 | 1.11 |
p < .05
NOTE: Fam = family, Par = parent, AAB = Adult Antisocial Behavior, ND = nicotine dependence, AUD = alcohol use disorder, IDUD = illicit drug use disorder.
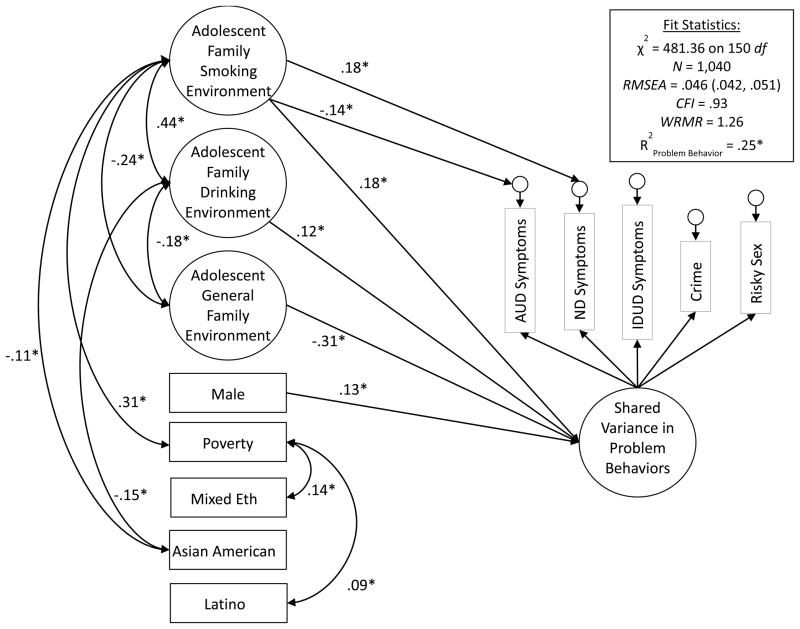
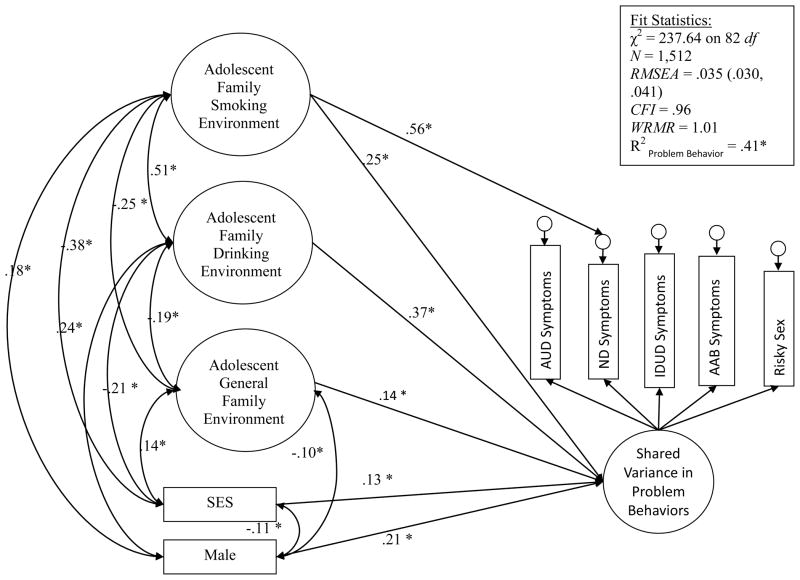
Structural equation models testing the fit of the heuristic model in each sample showed acceptable fit [RHC: χ2 = 481.36 on 150 df, RMSEA = .046 (90% Confidence Interval = .042, .051), CFI = .93, WRMR = 1.26; MTFS: χ2 = 237.64 on 82 df, RMSEA = .035 (90% Confidence Interval = .030, .041), CFI = .96; WRMR = 1.01]. Table 3 (RHC) and Table 4 (MTFS) display factor loadings and standard errors for each latent factor in the two samples. All indicators loaded significantly on their respective factor in both studies.
Table 3.
Factor loadings for latent variables in RHC.
| Standardized Estimate (SE) | |
|---|---|
| Family general environment | |
| Family management | .86 (.02)* |
| Conflict | −.75 (.02)* |
| Involvement | .82 (.02)* |
| Bonding | .82 (.02)* |
| Family drinking environment | |
| Pro drinking attitudes | .58 (.04)* |
| Parent drinking | .73 (.04)* |
| Sibling drinking | .33 (.04)* |
| Involvement in parent drinking | .37 (.02)* |
| Family smoking environment | |
| Parent smoking | .72 (.04)* |
| Sibling smoking | .47 (.05)* |
| Involvement in parent smoking | .36 (.02)* |
| Shared variance in problem behaviors | |
| Alcohol use disorder symptoms | .62 (.05)* |
| Nicotine dependence symptoms | .66 (.05)* |
| Illicit drug use disorder symptoms | .86 (.04)* |
| Crime | .69 (.04)* |
| Sex risk behavior | .28 (.04)* |
p < .05
Table 4.
Factor loadings for latent variables in MTFS.
| Standardized Estimate (SE) | |
|---|---|
| Family general environment | |
| Family management | .82 (.02)* |
| Conflict | −.73 (.02)* |
| Involvement | .56 (.03)* |
| Bonding | .79 (.02)* |
| Family drinking environment | |
| Parent drinking | .31 (.05)* |
| Co-twin drinking | .70 (.05)* |
| Family smoking environment | |
| Parent smoking | .27 (.05)* |
| Co-twin smoking | .77 (.08)* |
| Shared variance in problem behaviors | |
| Alcohol use disorder symptoms | .80 (.04)* |
| Nicotine dependence symptoms | .32 (.05)* |
| Illicit drug use disorder symptoms | .73 (.03)* |
| Adult antisocial behavior | .86 (.02)* |
| Sex risk behavior | .61 (.02)* |
p < .05
NOTE: SE = Standard Error
Figure 1 (RHC) and Figure 2 (MTFS) show the significant structural paths in the two samples, respectively. In both samples, adolescent general family environment, family smoking environment, and family drinking environment were all significantly related to the shared variance among young adult problem behaviors. Additionally, family smoking environment predicted unique variance in young adult ND symptoms in both samples. In the RHC sample, there was a significant, negative association between adolescent family smoking environment and unique variance in AUD symptoms at age 24; however, we believe this to be a suppressor effect given the positive zero-order correlation coefficients linking family smoking variables and young adult AUD symptoms (see Table 1). In the MTFS sample, there was no substance-specific association between family drinking or smoking and the unique variance in AUD symptoms. In both RHC and MFTS, family drinking and smoking environments were positively related to each other, and both were negatively related to general family environment. Males in both studies reported higher levels of general problem behavior in young adulthood. Neither study suggested associations between race/ethnicity and young adult problem behavior. SES was unrelated to young adult problem behavior among RHC youth, but those from higher SES backgrounds in MTFS reported more adult problem behavior. The positive SES/problem behavior link was interpreted as suppressor effect; SES was negatively related to problem behavior indicators at the zero order.
Figure 1.
Structural equation modeling results for RHC sample: standardized coefficients. Nonsignificant paths are not shown for readability. ND = nicotine dependence, AUD = alcohol use disorder, IDUD = illicit drug use disorder.
Figure 2.
Structural equation modeling results for MTFS sample: standardized coefficients. Nonsignificant paths are not shown for readability. Co-twin smoking and drinking were correlated, as were parent smoking and drinking; these paths were omitted to improve readability of the figure. ND = nicotine dependence, AUD = alcohol use disorder, IDUD = illicit drug use disorder, AAB = adult antisocial behavior.
In the RHC sample, the model explained 25% of the variance in the general problem behavior factor, 50% of the variance in nicotine dependence symptoms, and 36% of the variance in AUD symptoms (all p’s < .001). In the MTFS sample, the model explained 41% of the variance in the general problem behavior factor, 57% of the variance in ND symptoms, and 61% of the variance in AUD symptoms (all p’s < .001). Unstandardized estimates for both RHC and MTFS are available in online supplementary materials2.
4. DISCUSSION
This study aimed to replicate the heuristic model and findings from Bailey et al. (2011) in samples from RHC and MTFS, two independent, well-powered, longitudinal studies. There was strong consistency between the RHC and MTFS results that largely showed support for the methodological approach of partitioning environmental influence and phenotype into general and drug-specific components. In fact, patterns of significance in the RHC and MTFS samples were identical, with the exception of two likely suppressor effects, one inversely linking family smoking environment and unique variance in AUD symptoms in RHC and one linking higher SES with increased young adult problem behavior in MTFS.
As in the Bailey et al. (2011) paper, indicators of adolescent general family environment, family smoking environment, family drinking environment, and young adult general problem behavior formed usable latent factors. The general family environment to general problem behavior link found in the original study was replicated in both samples. Taken together with the Bailey et al. (2011) and Epstein et al. (2013) studies, the current results suggest that the quality of the general family environment in adolescence is predictive of a range of problem behaviors in adulthood and constitutes an important target for preventive interventions. These results are consistent with a large body of literature that underscores the importance of positive adolescent family environment in preventing young adult problem behaviors (e.g., Bailey et al., 2006; Chassin et al., 1998; Epstein et al., 2013) and support the use of the general/specific modeling framework for future gene-environment interplay studies.
Adolescent family smoking environment was consistently related to unique variance in adult ND in both samples studied here and in the SSDP data (Bailey et al., 2011; Epstein et al., 2013). Other researchers also have found substance-specific links between family smoking environment and smoking among young adults (Chassin et al., 1998; Keyes et al., 2008). This emerging pattern of results suggests an important and unique role of family smoking environments in young adult ND. Preventive interventions aimed at reducing young adult smoking need to target the smoking behavior and attitudes of family members during childhood and adolescence (see also Stone et al., 2012). General family environment, however, also contributed indirectly to adult ND in both samples, suggesting that smoking prevention efforts also should target general family characteristics like monitoring, bonding, conflict, and involvement.
Neither this study nor Epstein et al. (2013) found a link between family drinking environment and unique variance in AUD symptoms, as was reported by Bailey et al. (2011). Notably, the alcohol environment to unique alcohol variance link was small in the original study (standardized estimate = .11, p = .04). In the two studies reported here, it appears that family drinking environment may operate indirectly on young adult AUD via its link to general problem behavior. This finding goes against some prior literature that suggests alcohol-specific heritability (Kendler et al., 2003; Hicks et al., 2004), but is consistent with studies demonstrating heritability or intergenerational transmission of a general tendency toward antisocial behavior, of which alcohol use is a part (Bailey et al., 2006; McGue et al., 2006; Dick et al., 2010). More research is needed to determine whether adolescent family drinking environment contributes to unique variance in young adult AUD that is not shared with other problem behaviors and to understand the association between family drinking environment and young adult problem behavior.
RHC and MTFS data showed associations between family smoking and drinking environments and young adult general problem behavior that were not found in Bailey et al. (2011) or Epstein et al. (2013). Sample differences between the prior studies and the studies reported here likely explain this difference in findings. The SSDP sample was largely urban, sampled respondents from a mix of high-risk and lower risk neighborhoods, and was racially/ethnically diverse, including nearly 50% non-White participants. In contrast, both samples used here were mostly White (75% in RHC, 95% in MTFS), less urban, and not oversampled for high-risk individuals. In these lower risk samples, family smoking and drinking may have been more indicative of deviance, and therefore more closely tied to young adult general problem behavior than in the higher risk sample used in the first two studies. Future replication attempts should test the generalizability of findings with respect to race/ethnicity, urban/suburban location, neighborhood risk, and socioeconomic status.
Study strengths include the longitudinal data, the relatively large samples, and the congeneric measures across studies. Some limitations should be considered when drawing conclusions from the current findings. The samples used here are geographically restricted (although not to the same region), which may limit generalizability. Exact replication of long-term, longitudinal studies is extremely difficult; the replications reported here are conceptual rather than exact. Some authors have argued that exact replications are to be preferred, and that replications should be independent, not including authors of the original study(ies) (Makel et al., 2012). We enthusiastically encourage further replications of the proposed heuristic model. Although both studies were longitudinal, the current procedures did not investigate potential changes in the roles of family general, smoking, and drinking environments across adolescent development.
Understanding the etiology of adult problem behavior requires measuring and defining complex phenotypes and modeling a broad array of interacting genetic and environmental risk and protective factors. The proposed simplifying model offers several advantages for those studying GxE and rGE in problem behavior. It yields a small number of parsimonious measures of environment that reflect current knowledge about the multidimensional nature of environmental influence and have clear implications for treatment and prevention. Although it has yet to be tested with molecular genetic data, we believe the model will facilitate the inclusion of stronger and more sophisticated measures of environment in GxE studies.
Supplementary Material
Acknowledgments
We gratefully acknowledge the staff and participants of the Raising Healthy Children study and the Minnesota Twin and Family Study, as well as Tanya Williams for editing this manuscript.
Funding
This research was supported by Grants DA024411, DA008093, DA009679, and DA05147 from the National Institute on Drug Abuse and Grant AA09367 from the National Institute on Alcohol Abuse and Alcoholism. Dr. Samek was also supported by Grant MH017069 from the National Institute of Mental Health.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
See Supplementary Table 1, by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
See Supplementary Tables 2 and 3 by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Contributors
All authors were involved in study conceptualization. Drs. Samek, Hicks, and Bailey conducted the statistical analyses with consultation from the other authors. Drs. Samek and Bailey conducted literature searches, summarized prior work, and wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of interest
Dr. Catalano serves on the board of Channing Bete Company, which owns portions of the Raising Healthy Children intervention mentioned here. All other authors declare that they have no conflict of interest.
Portions of the present findings were reported at the annual meeting of the Society for Prevention Research, San Francisco, CA, May 28–31, 2013.
The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Bailey JA, Hill KG, Meacham MC, Young SE, Hawkins JD. Strategies for characterizing complex phenotypes and environments: general and specific family environmental predictors of young adult tobacco dependence, alcohol use disorder, and co-occurring problems. Drug Alcohol Depend. 2011;118:444–451. doi: 10.1016/j.drugalcdep.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey JA, Hill KG, Oesterle S, Hawkins JD. Linking substance use and problem behavior across three generations. J Abnorm Child Psychol. 2006;34:273–292. doi: 10.1007/s10802-006-9033-z. [DOI] [PubMed] [Google Scholar]
- Bakker M, van Dijk A, Wicherts JM. The rules of the game called psychological science. Perspect Psychol Sci. 2012;7:543–554. doi: 10.1177/1745691612459060. [DOI] [PubMed] [Google Scholar]
- Blomeyer D, Treutlein J, Esser G, Schmidt MH, Schumann G, Laucht M. Interaction between CRHR1 gene and stressful life events predicts adolescent heavy alcohol use. Biol Psychiatry. 2006;63:146–151. doi: 10.1016/j.biopsych.2007.04.026. [DOI] [PubMed] [Google Scholar]
- Brown EC, Catalano RF, Fleming CB, Haggerty KP, Abbott RD. Adolescent substance use outcomes in the Raising Healthy Children project: a two-part latent growth curve analysis. J Consult Clin Psychol. 2005;73:699–710. doi: 10.1037/0022-006X.73.4.699. [DOI] [PubMed] [Google Scholar]
- Chassin L, Presson CC, Todd M, Rose JS, Sherman SJ. Maternal socialization of adolescent smoking: the intergenerational transmission of parenting and smoking. Dev Psychol. 1998;34:1189–1201. doi: 10.1037//0012-1649.34.6.1189. [DOI] [PubMed] [Google Scholar]
- Dick DM, Meyers J, Aliev F, Nurnberger J, Jr, Kramer J, Kuperman S, Porjesz B, Tischfield J, Edenberg HJ, Foroud T, Schuckit M, Goate A, Hesselbrock V, Bierut LJ. Evidence for genes on chromosome 2 contributing to alcohol dependence with conduct disorder and suicide attempts. Am J Med Genet. 2010;153B:1179–1188. doi: 10.1002/ajmg.b.31089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkins IJ, McGue M, Iacono WG. Genetic and environmental influences on parent-son relationships: evidence for increasing genetic influence during adolescence. Dev Psychol. 1997;33:351–363. doi: 10.1037//0012-1649.33.2.351. [DOI] [PubMed] [Google Scholar]
- Epstein M, Hill KG, Bailey JA, Hawkins JD. The effect of general and drug-specific family environments on comorbid and drug-specific problem behavior: a longitudinal examination. Dev Psychol. 2013;49:1151–1164. doi: 10.1037/a0029309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haggerty KP, Fleming CB, Catalano RF, Harachi TW, Abbott RD. Raising healthy children: examining the impact of promoting healthy driving behavior within a social development intervention. Prev Sci. 2006;7:257–267. doi: 10.1007/s11121-006-0033-6. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Hill KG, Guo J, Battin-Pearson SR. Substance use norms and transitions in substance use: implications for the gateway hypothesis. In: Kandel DB, editor. Stages and Pathways of Drug Involvement. Examining the Gateway Hypothesis. Cambridge University Press; New York: 2002. pp. 42–64. [Google Scholar]
- Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Promoting positive adult functioning through social development intervention in childhood: long-term effects from the Seattle Social Development Project. Arch Pediatr Adolesc Med. 2005;159:25–31. doi: 10.1001/archpedi.159.1.25. [DOI] [PubMed] [Google Scholar]
- Hawkins JD, Kosterman R, Catalano RF, Hill KG, Abbott RD. Effects of social development intervention in childhood fifteen years later. Arch Pediatr Adolesc Med. 2008;162:1133–1141. doi: 10.1001/archpedi.162.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks BM, Krueger RF, Iacono WG, McGue M, Patrick CJ. Family transmission and heritability of externalizing disorders: a twin-family study. Arch Gen Psychiatry. 2004;61:922–928. doi: 10.1001/archpsyc.61.9.922. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Rose GL, Callas PW. Nicotine is more reinforcing in smokers with a past history of alcoholism than in smokers without this history. Alcohol Clin Exp Res. 2000;24:1633–1638. [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-use disorders: findings from the Minnesota Twin Family Study. Dev Psychopathol. 1999;11:869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Schulenberg JE. Conjoint developmental trajectories of young adult alcohol and tobacco use. J Abnorm Psychol. 2005;114:612–626. doi: 10.1037/0021-843X.114.4.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanh MR, Berger AT, Wells BE, Cleland CM. Longitudinal associations between adolescent alcohol use and adulthood sexual risk behavior and sexually transmitted infection in the United States: assessment of differences by race. Am J Public Health. 2012;102:867–876. doi: 10.2105/AJPH.2011.300373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Keyes M, Legrand LN, Iacono WG, McGue M. Parent smoking and adolescent problem behavior: an adoption study of general and specific effects. Am J Psychiatry. 2008;165:1338–1344. doi: 10.1176/appi.ajp.2008.08010125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreek MJ, Nielsen DA, Butelman ER, LaForge KS. Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Nat Neurosci. 2005;8:1450–1457. doi: 10.1038/nn1583. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J Abnorm Psychol. 2002;111:411–24. [PubMed] [Google Scholar]
- Makel MC, Plucker JA, Hegarty B. Replications in psychology research: how often do they really occur? Perspect Psychol Sci. 2012;7:537–542. doi: 10.1177/1745691612460688. [DOI] [PubMed] [Google Scholar]
- McGue M, Iacono WG, Krueger R. The association of early adolescent problem behavior and adult psychopathology: a multivariate behavioral genetic perspective. Behav Genet. 2006;36:591–602. doi: 10.1007/s10519-006-9061-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMorris BJ, Petrie RS, Catalano RF, Fleming CB, Haggerty KP, Abbott RD. Use of web and in-person survey modes to gather data from young adults on sex and drug use: an evaluation of cost, time, and survey error based on a randomized mixed-mode design. Eval Rev. 2009;33:138–158. doi: 10.1177/0193841X08326463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Rutter M. Measured gene-environment interactions in psychopathology: concepts, research strategies, and implications for research, intervention, and public understanding of genetics. Perspect Psychol Sci. 2006;1:5–27. doi: 10.1111/j.1745-6916.2006.00002.x. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Muthén & Muthén; Los Angeles: 1998–2011. [Google Scholar]
- Olson DH, Portner J, Lavee Y. Family Adaptability and Cohesion Scale. 3. University of Minnesota; St. Paul: 1985. (FACES-III) [Google Scholar]
- Pashler H, Wagenmakers EJ. Editors’ introduction to the special section on replicability in psychological science: a crisis of confidence? Perspect Psychol Sci. 2012;7:528–530. doi: 10.1177/1745691612465253. [DOI] [PubMed] [Google Scholar]
- Robins LN, Babor T, Cottler L. Composite International Diagnostic Interview: Expanded Substance Abuse Module. Washington University School of Medicine; St. Louis, MO: 1987. [Google Scholar]
- Robins LN, Cottler L, Goldring E. The Diagnostic Interview Schedule Version III-R. Washington University School of Medicine; St. Louis, MO: 1989. [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Williams JBW, Spitzer RL. NIMH Diagnostic Interview Schedule: Version III (May 1981) National Institute of Mental Health; Rockville, MD: 1981. [Google Scholar]
- Robins LN, Wing J, Wittchen HU, Helzer JE, Babor T, Burke J, Famer A, Jablenski A, Pickens R, Reiger DA, Sartorious N, Towle LH. The Composite International Diagnostic Interview: an epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry. 1988;45:1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- Rutter M, Moffitt TE, Caspi A. Gene-environment interplay and psychopathology: multiple varieties but real effects. J Child Psychol Psychiatry. 2006;47:226–261. doi: 10.1111/j.1469-7610.2005.01557.x. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M. Structured Clinical Interview for DSM-III-R (SCID) New York State Psychiatric Institute, Biometrics Research; New York: 1987. [Google Scholar]
- Stone AL, Becker LG, Huber AM, Catalano RF. Risk and protective factors of substance use and problem use in emerging adulthood. Addict Behav. 2012;37:747–775. doi: 10.1016/j.addbeh.2012.02.014. [DOI] [PubMed] [Google Scholar]
- Tsuang MT, Bar JL, Harley RM, Lyons MJ. The Harvard Twin Study of Substance Abuse: what we have learned. Harv Rev Psychiatry. 2001;9:267–279. [PubMed] [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview, Version 1.0. World Health Organization; Geneva: 1990. [Google Scholar]
- Young SE, Rhee SH, Stallings MC, Corley RP, Hewitt JK. Genetic and environmental vulnerabilities underlying adolescent substance use and problem use: general or specific? Behav Genet. 2006;36:603–615. doi: 10.1007/s10519-006-9066-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.