Abstract
Previous research has found a deleterious impact of stigma on the mental health of children affected by HIV/AIDS. Little is known about the longitudinal relationship of stigma and children’s mental health. This study explores the longitudinal reciprocal effects of depressive symptoms and stigma, specifically enacted stigma and perceived stigma, among children affected by HIV/AIDS aged 6 to 12. Longitudinal data were collected from 272 children orphaned by AIDS and 249 children of HIV-positive parents in rural China. Cross-lagged panel analysis was conducted in the study. Results showed that the autoregressive effects were stable for depressive symptoms, perceived stigma and enacted stigma suggesting the substantially stable individual differences over time. The cross-lagged effects indicated a vicious circle among the three variables in an order of enacted stigma→depressive symptom→perceived stigma→enacted stigma. The possibility of employing equal constraints on cross-lagged paths suggested that the cross-lagged effects were repeatable over time. The dynamic interplay of enacted stigma, perceived stigma and depressive symptoms suggests the need of a multilevel intervention in stigma reduction programming to promote mental health of children affected by HIV/AIDS.
Keywords: Children, HIV/AIDS, Enacted stigma, Perceived stigma, Depressive symptoms, Cross-lagged, Longitudinal
Introduction
As of 2011, 17.3 million children under the age of 18 have lost one or both parents to AIDS and millions more have been living with parents who are infected by HIV [1]. These children face numerous challenges – one of which is stigma. A limited number of cross-sectional studies have found the destructive effect of HIV-related stigma on the mental health of children affected by parental HIV/AIDS [2]. A longitudinal investigation would help to reveal the dynamic relationship between stigma and children’s mental health over time, and to better inform intervention development and dissemination. The present study used a three-wave data to examine the potential vicious circle of depressive symptoms and stigma, specifically perceived stigma and enacted stigma, among children affected by parental HIV/AIDS in rural China.
Social stigma was defined as a devalued identity that discredits a person in society [3, 4]. Individuals being associated with a health condition (e.g., psychiatric disorders), a social group (e.g., ethnic minority), or some life conditions (e.g., poverty) are often believed to possess some attribute that is devalued in a specific cultural context [3]. HIV stigma is socially shared knowledge about the devalued status of people living with HIV/AIDS (PLWHA) [5]. It manifests in stereotyping, discrediting, discounting, prejudice and discrimination directed at PLWHA [6–8]. It involves physical rejection derived from fear of infection by the HIV virus and moral judgment on behaviors such as drug use, commercial sex, and homosexual behaviors, which are perceived to be associated with HIV infection [9–11]. Numerous studies have demonstrated that stigma was one of the major risk factors that compromise PLWHA’s medical adherence and treatment and psychological well-being. According to a meta-analytical synthesis, stigma was significantly associated with various mental health indicators (e.g., depressive symptoms, anxiety, perceived stress, quality of life, and loneliness) with medium [12] to large effect sizes [13].
The deleterious impact of stigma does not stop at HIV/AIDS patients but also extends to their family members, including their uninfected children [8]. A study in Haiti reported that 32.4% caregivers felt that children affected by parental HIV were discriminated by others [14]. A few number of studies have consistently shown that stigma was an important risk factor associated with mental health outcomes among children affected by parental HIV [14–17]. A South African study found that the proportion of AIDS-orphaned adolescents who fell in the clinical range for an internalizing problem (anxiety, depressive symptoms, or posttraumatic stress) was nearly 3 times higher when orphans experienced HIV stigma [18]. Similarly, it was found that stigma was associated with children’s internalizing problems (depressive symptoms, loneliness), school adjustment (school interest, peer relationship, rule compliance, anxiety), social adjustment (self-esteem, future expectation, hopefulness and sense of control over future) in China [16, 19, 20]. Also, stigma was shown to mediate the relationships between AIDS orphanhood and long-term mental health problems [17].
Social stigma may be experienced by an individual in three forms: enacted stigma (overt behaviors), perceived stigma (awareness of stereotype), and internalized stigma (personal value) [7, 21]. Enacted stigma refers to overt acts of discrimination and humiliation directed at a person because of his or her stigmatized status, which captures the interpersonal aspect of stigma. By contrast, perceived stigma and internalized stigma captures the intrapersonal aspect of stigma. Perceived stigma refers to the subjective awareness of social stigma. Internalized stigma, also known as self-stigma, describes the process that an individual accepting society’s negative evaluation and incorporating it into personal value and sense of self [5]. Although experiencing either forms of HIV stigma has an important and negative consequence on individual’s mental health, various stigma components may contribute uniquely to different mental health problems. Perceived stigma may lead to the fear of stigmatization, anxiety in struggling whether to disclose, and distress in managing the treatment privately [5, 22]. These psychological burdens further delay the access to health care, weaken treatment adherence, discourage HIV disclosure and support seeking, therefore result in severe consequences for the control of the HIV pandemic [11, 23–27]. Experiencing enacted stigma may directly increase risk for psychological distress among PLWHA and their family members [27]. Internalizing stigma may directly devalue the self-esteem and the self-concept of PLWHA and their family members [28, 29]. It may also prevent them from seeking social support and needed resources, in turn causing psychological distress [29]. Limited evidence was available regarding the interrelationships of the three forms of stigma and their effects on psychosocial well-being. Based on research with other stigmatized groups (e.g., epilepsy patients), one study in India hypothesized that perceived stigma mediated the relationship between enacted stigma and psychological distress [5]. Another study in Thailand suggested that internalized stigma mediated the relationship between perceived stigma and depressive symptoms [28].
In China, an estimated 260,000 children lost one or both parents to AIDS and most of them are living in rural area in central China [30–32]. The nature of the epidemic in central provinces in China and its origins in commercial blood collection have produced a variety of challenges for children from HIV-affected families [31]. Due to the unhygienic blood collection in the late 1980s and early 1990s, the onset of the HIV epidemic was very rapid, with suddenly many people becoming sick and dying over a short period. It is devastating towards children because the epidemic took lives of people of a particular age; that of being the bread earners of the family and caregiver for children [31]. Recent studies in China showed that children from HIV-affected families demonstrated poorer physical health and psychological health than children from HIV-free families in the same community [30, 33, 34]. Perceived stigma and enacted stigma were reported as robust predictors to internalizing and externalizing problems not only among children affected by HIV/AIDS, but also among children of HIV-free family in the same community which was hardly hit by high HIV epidemic [20].
Limited data were available regarding the impact of different forms of stigma on children’s mental health in a longitudinal perspective and in resource limited settings. To study the interrelationships among perceived stigma, enacted stigma and children’s depressive symptoms, we propose a conceptual model (Figure 1). Based on the existing literature, we hypothesize that perceived stigma predicts depressive symptoms, which in turn reinforces perceived stigma. We also hypothesize that enacted stigma increases perceived stigma, which in turn reflects the continuous existence of enacted stigma. Regarding the effects of enacted stigma on depressive symptoms, we hypothesize that enacted stigma predicts depressive symptoms but not vice versa. In addition, we will explore whether perceived stigma and enacted stigma similarly affect the changes in children’s depressive symptoms over time.
Figure 1.
The hypothesized conceptual model
Method
Participants
The participants of this study include 272 children orphaned by AIDS (children who lost one or both their parents to HIV/AIDS [32]) and 249 children living with HIV-positive parent(s). The children were participants in a larger research project on the psychological adjustment of children affected by HIV. Participants were recruited from two rural counties in central China during 2006–2010 where many residents (mostly farmers) were infected with HIV through unhygienic blood collection. Both counties had the highest prevalence of HIV-infection in the province. The participants in the current study were mainly recruited from five administrative villages, which have the highest number of HIV-related death or confirmed HIV-infection according to the local surveillance data. The larger research project enrolled a total 1625 children and adolescents aged 6–18 years [34]. This study focuses on a subgroup of younger children (6–12 years old), who were in their developmental stage of childhood. It has been found that younger children may suffer more from parental illness and death compared to older children [35]. By focusing on this age cohort, we can provide data to inform the intervention design for this vulnerable group of children. Children were assessed annually over three years (i.e., three time points). Approximately, 7.5% participants dropped out from both second and third waves. As shown in Table 1, there were no significant differences between the dropped participants and the retained ones on either the demographic characteristics or the main study variables at the baseline. Missing values of study variables across waves were ranged from 1% to 5%. The majority (over 98%) of the participants were of Han ethnicity, the predominant ethnic group in China. Children with HIV infection were eligible to participate, although no HIV testing was conducted in the current study. According to the knowledge of the local community members with whom we worked with, the number of children with HIV infection was estimated to be very small.
Table 1.
Demographic profile of participants
| T1 | T2 | T3 | Retained at either T2 or T3 | Dropped at both T2 & T3 | |
|---|---|---|---|---|---|
| N (%) T0 | 521 (100%) | 471 (90.4%) | 428 (82.1%) | 482 (92.5%) | 39 (7.5%) |
| Care arrangement | |||||
| Orphanage | 89 (17.1%) | 81 (17.2%) | 76 (17.8%) | 83 (93.3%) | 6 (6.7%) |
| Family | 432 (82.9%) | 390 (82.8%) | 352 (82.2%) | 399 (92.4%) | 33 (7.6%) |
| Primary caregivers | |||||
| Father | 276 (64.6%) | 262 (67.2%) | 228 (64.8%) | 256 (65.0%) | 20 (60.6%) |
| Mother | 291 (68.1%) | 272 (69.7%) | 238 (67.6%) | 269 (8.3%) | 22 (66.7%) |
| Paternal grandparents | 174 (40.7%) | 153 (39.2%) | 142 (40.3%) | 162 (41.1%) | 12 (36.4%) |
| Maternal grandparents | 28 (6.6%) | 24 (6.2%) | 18 (5.1%) | 26 (6.6%) | 2 (6.1%) |
| Paternal relatives | 19 (4.4%) | 18 (3.3%) | 18 (5.1%) | 17 (4.3%) | 2 (6.1%) |
| Maternal relatives | 13 (3.0%) | 13 (3.3%) | 7 (2.0%) | 11 (2.8%) | 2 (6.1%) |
| Age | 10.69 (1.28) | 11.66 (1.28) | 12.61 (1.28) | 10.67 (1.28) | 10.97 (1.25) |
| Gender | |||||
| Boys | 275 (52.8%) | 247 (52.4%) | 214 (50%) | 252 (52.3%) | 23 (59.0%) |
| Girls | 246 (47.2%) | 224 (47.6%) | 214 (50%) | 230 (47.7%) | 16 (41.0%) |
| Awareness of parental HIV | |||||
| No | 117 (22.5%) | 63 (13.4%) | 18 (4.2%) | 107 (22.2%) | 10 (25.6%) |
| Yes | 361 (69.3%) | 399 (84.7%) | 377 (88.1%) | 336 (69.7%) | 25 (64.1%) |
| Not reported | 43 (8.3%) | 9 (1.9%) | 33 (7.7%) | 39 (8.1%) | 4 (10.3%) |
| Parental death | |||||
| No | 249 (47.8%) | 194 (41.2%) | 144 (33.6%) | 230 (47.7%) | 19 (48.7%) |
| Yes | 272 (52.2%) | 277 (58.8%) | 251 (58.6%) | 252 (52.3%) | 20(51.3%) |
| Not reported | 0 (0%) | 0 (0%) | 33 (7.7%) | 0 (0%) | 0 (0%) |
Note. The calculations in the last two columns were based on the data at T1.
Procedures
Approximately, 17.1% children were recruited from government-funded orphanages and 82.9% children were from family and kinship care settings. For those who were recruited from family care settings, we worked with the village leaders to generate lists of families caring for orphans and families with a confirmed diagnosis of parental HIV/AIDS and approached the families on the lists to randomly recruit one child per family to participate in the study. Because of the implementation of the Chinese’ government’s AIDS relief policy (e.g., free schooling for children affected by HIV/AIDS) in our study site, most of the school-age children (93%) were attending school. Therefore, data collection mainly took place at local schools. The interviewers administrated the survey in Mandarin to children individually or in a small group. For children with limited literacy, interviewers read questions to them and children gave responses. The entire assessment took about 75–90 minutes depending on the reading ability of the child. Children were offered a 10–15 minutes break after every 30 minutes during the survey. Each child received a gift at completion of the survey as a token of appreciation. The research protocol, including consenting procedure, was approved by the Institutional Review Boards at both Wayne State University in the US and Beijing Normal University in China.
Measures
Demographic characteristics of individual and family were reported by children, including age, sex, ethnicity, care arrangement, awareness of parental HIV infection, and parental death.
Depressive symptoms were measured with the Center for Epidemiological Studies Depression Scale for Children (CES-DC), which has been validated in Chinese child population [36, 37]. The scale consists of 20 items. Example items are “I had trouble keeping my mind on what I was doing” and “I felt depressed”. CES-DC asks children to respond to how often the affect or symptom occurred in the past week. To obtain the most reliable measurement, we deleted 5 items which had item-total correlations less than .30 in any of the three waves. The Cronbach alphas of the remaining 15 items were .88, .89 and .89 for the three waves, respectively.
Perceived stigma was assessed by the 10-item scale, Stigma Against Children Affected by AIDS [16]. Three items measured social exclusion against children affected by HIV (e.g., “people think children of PLWHA should leave their villages”). Four items measured purposive avoidance (e.g., “people do not want their children to play with children of PLWHA”). Three items measured perception that children affected by HIV are inferior to children of HIV-free families (e.g., “people think children of PLWHA are unclean”). The response options ranged from “strongly disagree” to “strongly agree”. The Cronbach alphas of the scale were .86, .91 and .94 for the three waves, respectively.
Enacted stigma was measured with a 12-item scale, in which children were asked to report whether they had experienced some stigmatized actions after parental illness. Sample items included: “being called bad names”, “being teased or picked on by other kids”, “relatives stopped visiting us when parents got sick or died”. The response options ranged from “never happened” to “always happened”. The scale along with other scales in the assessment inventory was pilot tested prior to actual field data collection and the scale demonstrated good content validity. The Cronbach alphas of the 12-item scale were .88, .84 and .87 for the three waves, respectively.
Data Analysis
Preliminary data analyses were performed using SPSS 11.0. Cross-lagged path models were tested using Mplus Version 5.1 [38]. To efficiently handle the missing data, we used full information maximum likelihood estimation. All models were controlled for child gender, child age, care arrangement (i.e., orphanage or family care), awareness of parental HIV infection, and parental death. The first step in the analyses was testing a basic stability model (Figure 2), in which we only estimated the autoregressive effects of depressive symptoms, perceived stigma, and enacted stigma. Within-wave residuals were allowed to be correlated. In the second step, we tested our hypothesized model (Figure 1). A sequence of path models were tested separately, each adding unidirectional cross-lagged paths separately: 1) perceived stigma→ depressive symptoms; 2) depressive symptoms → perceived stigma; 3) enacted stigma → depressive symptoms; 4) perceived stigma → enacted stigma; and 5) enacted stigma → perceived stigma. These models were to investigate whether these cross-lagged paths significantly improved the overall fit of the basic model. Paths were not included in the further model testing if they did not improve the model fit in comparison with the basic model. Finally, we examined the potential repeatability of cross-lagged effects over time and the within-wave residual correlations to determine the most parsimonious model that best represented the data. Several goodness-of-fit indices were applied to evaluate the fit of the models: chi-square, p-value, Comparative Fit Index (CFI), and Root Mean Square Error of Approximation (RMSEA). Non-significant chi-square is favorable. For the CFI, values greater than .90 indicate an acceptable fit of the model to the data, whereas the values of the RMSEA should be less than .08 for an acceptable fit [39]. Chi-square difference tests were used to compare the fit of different nested models.
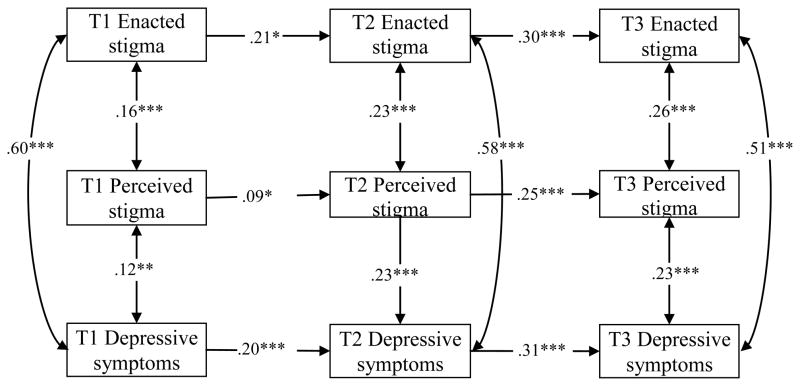
Figure 2.
Basic model with standardized path estimates (Model 1)
* p < .05, *** p < .001.
Results
Descriptive Statistics
Table 1 presents the demographic characteristics of participants at Time 1 (T1), Time 2 (T2), and Time 3 (T3). The difference of demographic profiles between participants retained at either T2 or T3 and participants dropped at both T2 and T3 were also presented. As shown in Table 1, 52.8% of the participants were boys and 47.2% were girls at T1. The average age of children at T1 was 10.69 years (SD = 1.28). Boys were slightly older than girls (10.81 vs. 10.57; p = .03). About seventy percent of children were aware of parental HIV infection at T1 and the awareness level increased about 8% by T3. The percentage of parental death was 52.2% at T1, 58.8% at T2, and 58.6% at T3. Preliminary analyses data (not shown in the table) were performed to explore whether these demographic characteristics were correlated with the main study variables. Awareness of parental HIV at T1 was significantly correlated with depressive symptoms at T2 (r = .10). Parental death were correlated with depressive symptoms at T1 (r = .09). Child’s age significantly and negatively correlated with depressive symptoms at T1 (r = −.20) and at T2 (r = −.09), with perceived stigma at T1 (r = −.21) and T2 (r = −.10), and with enacted stigma at T1 (r = −.21). Some gender differences were found in depressive symptoms at T3 (p <.05, Cohen’s d = .24), with girls scoring higher than boys. Differences by care arrangement were found in depressive symptoms at T2 (p < .01, Cohen’s d = .21), perceived stigma at T1 (p < .001, Cohen’s d = .41), and enacted stigma at T1 (p < .05, Cohen’s d = 26), with children living in orphanages scoring higher on those measures than those in family care settings. Depressive symptoms decreased over time (F[1.83, 756.27] = 103.27, p <. 001). Similarly, perceived stigma decreased over time (F[2, 826] = 86.70, p <. 001) and enacted stigma decreased over time (F[1.68, 669.85] =111.40, p <. 001). Table 2 presents the intercorrelations among the main study variables. Almost all the intercorrelations were significant. The within-wave correlations between enacted stigma and depressive symptoms were stronger (. 57 to .61) than those between perceived stigma and depressive symptoms (.17 to .28).
Table 2.
Correlation coefficients and descriptive statistics for study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1 Depressive symptoms | ||||||||||
| 2. T2 Depressive symptoms | .28 *** | |||||||||
| 3. T3 Depressive symptoms | .16 *** | .36 *** | ||||||||
| 4. T1 Perceived stigma | .17 *** | .19 *** | .12** | |||||||
| 5. T2 Perceived stigma | .13 ** | .26 *** | .14** | .16 *** | ||||||
| 6. T3 Perceived stigma | .03 | .20 *** | .28*** | .15 ** | .28 *** | |||||
| 7. T1 Enacted stigma | .61 *** | .24 *** | .21*** | .20 *** | .14 ** | .04 | ||||
| 8. T2 Enacted stigma | .25 *** | .61 *** | .31*** | .25 *** | .29 *** | .16 | ** | .29 *** | ||
| 9. T3 Enacted stigma | .13 ** | .28 *** | .57*** | .17 *** | .18 *** | .29 | *** | .21 *** | .37 *** | |
| Mean | .74 | .44 | .35 | 2.24 | 1.82 | 1.69 | 1.73 | 1.34 | 1.23 | |
| SD | .56 | .46 | .41 | .75 | .75 | .76 | .73 | .49 | .39 | |
| Range | .00–3.00 | .00–2.87 | .00–2.33 | 1.00–4.00 | 1.00–5.00 | 1.00–4.80 | 1.00–5.00 | 1.00–4.10 | 1.00–3.91 | |
p < .01
p < .001
Path Analysis
Table 3 presents the goodness-of-fit indices and model comparison tests of each tested model. The basic model with autoregressive paths and within-wave correlated residuals (Model 1) was tested first. The model fit the data well. All autoregressive effects were statistically significant (see Figure 2). This indicates that a significant portion of individual differences remained stable over time for depressive symptoms, perceived stigma, and enacted stigma. We then tested whether adding the hypothesized cross-lagged paths among the three study variables improved model fit of the basic model. Model 3 to Model 5 significantly improved the model fit of Model 1. However, Model 2 and Model 6 did not improve the model fit of Model 1. Adding paths (perceived stigma→depressive symptoms) or the paths (enacted stigma→perceived stigma) did not improve the model fit of the basic model. Therefore, we did not include these paths in the subsequent model testing. Model 7, including all the significant cross-lagged paths, autoregressive paths, and within-wave correlated residuals, were tested. The model fit the data very well and it substantially improved the fit indices of the basic model.
Table 3.
Model comparison of cross-lagged path analysis
| Model fit indices | Model comparison test | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| χ2 | df | p | CFI | RMSEA | Δχ2 | Δdf | ||
| Model 1: Basic model | 110.21 | 57 | <.001 | .95 | .04 | |||
| Model 2: Basic + perceived stigma→depressive symptoms | 110.01 | 55 | <.001 | .94 | .04 | 2 vs. 1 | .20 | 2 |
| Model 3: Basic + depressive symptoms→perceived stigma | 102.69 | 55 | <.001 | .95 | .04 | 3 vs. 1 | 7.52* | 2 |
| Model 4: Basic + enacted stigma→depressive symptoms | 94.89 | 55 | <.001 | .96 | .04 | 4 vs. 1 | 15.32*** | 2 |
| Model 5: Basic + perceived stigma→enacted stigma | 94.41 | 55 | <.001 | .96 | .04 | 5 vs. 1 | 15.8*** | 2 |
| Model 6: Basic + enacted stigma→perceived stigma | 106.21 | 55 | <.001 | .95 | .04 | 6 vs. 1 | 4.00 | 2 |
| Model 7: Basic + significant cross-lagged paths | 71.01 | 51 | .03 | .98 | .03 | 7 vs.1 | 39.20*** | 6 |
| Model 8: Final parsimonious model with possible equal constrains | 76.27 | 56 | 0.04 | .98 | .03 | 8 vs. 7 | 5.26 | 5 |
p < .05
p < .001
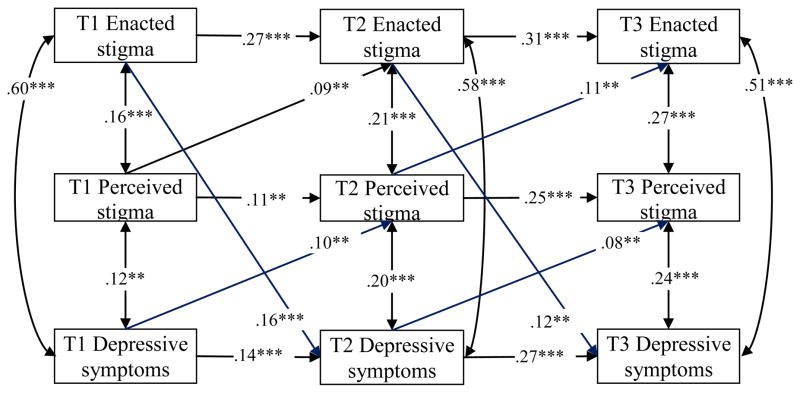
Furthermore, we examined whether it was possible to fix the within-wave correlated residuals and the cross-lagged paths to determine the repeatability of cross-lagged effects over time. The following paths could be constrained to be equal across waves: depressive symptoms→perceived stigma (Δχ2(1) =.59, p = .44), enacted stigma→depressive symptoms (Δχ2(1) = 1.29, p = .26), and perceived stigma→enacted stigma (Δχ2(1) = 2.83, p =.09). It was also possible to constrain the within-wave correlated residuals to be equal of perceived stigma and depressive symptoms (Δχ2(1) =.25, p = .62), and of perceived stigma and enacted stigma (Δχ2(1) =.79, p = .37), across waves. The equal constraint of the within-wave correlated residuals of depressive symptoms and enacted stigma across waves significantly altered the model fit (Δχ2(1) = 14.62, p < .001), therefore we did not include the constraint in the final model. The final parsimonious model (Model 8) with aforementioned five possible equal constraints were not significantly different with Model 7 (Δχ2(5) = 5.26, p = .38). Thereby, we chose Model 8 as the best fitting model. The standardized path coefficients of this final model are presented in Figure 3. Note that although unstandardized coefficients were constrained to be equal, the standardized coefficients can still slightly differ from each other. The results suggested that there was considerable stability of significant cross-lagged effects over time.
Figure 3.
Final model (model 8) with crossed lagged effects.
Note.** p < .01, *** p < .001. The cross-lagged paths were constrained to be equal across waves. The within-waves correlated residuals were constrained to be equal across waves of depressive symptoms and perceived stigma, and of perceived stigma and enacted stigma
The indirect effect test of the cross-lagged paths was also performed. Results showed that T1 perceived stigma predicted T3 depressive symptoms indirectly through T2 enacted stigma (p < .01), T1 enacted stigma predicted T3 perceived stigma indirectly through T2 depressive symptoms (p < .05); T1 depressive symptoms predicted T3 enacted stigma indirectly through T2 perceived stigma (p < .05). These results revealed a vicious circle among the three variables in a specific direction, enacted stigma→depressive stigma→perceived stigma→enacted stigma.
Discussion
This study tested a cross-lagged model to depict the reciprocal effects of enacted stigma, perceived stigma and depressive symptoms among children affected by parental HIV/AIDS in an HIV epicenter of rural China. Autoregressive effects were stable over time for depressive symptoms, perceived stigma and enacted stigma, suggesting the substantially stable individual differences over time. Cross-lagged effects indicated a vicious circle among the three variables in a specific direction enacted stigma→depressive stigma→perceived stigma→enacted stigma. The possibility of employing equal constraints on cross-lagged paths suggested the cross-lagged effects are repeatable over time. The current study extends the existing literature by demonstrating that perceived stigma and enacted stigma affect children’s well-being in different pathways. Importantly, the current findings offer the first evidence that the link between depressive symptoms and various forms of stigma is longitudinal and bidirectional.
Our data indicated that enacted stigma directly predicted later depressive symptoms with a stable degree and aggravated the negative effect of perceived stigma on later depressive symptoms. Our findings are consistent with the previous cross-sectional findings among children affected by HIV/AIDS [18] and among children with other health and social adversities, such as mental illness [40], physical disabilities [41], and poverty [10]. The potential mediating effect of enacted stigma between perceived stigma and depressive symptoms suggest the important role of enacted stigma in psychological distress. Children experienced more discriminatory, isolated and threatened actions from others are expected to demonstrate more depressive symptoms. The feelings of shame or embarrassment caused by enacted stigma might inhibit a child’s psychological adjustment by maintaining a focus on negative aspects of living with HIV-positive parents.
The results also showed that depressive symptoms predicted perceived stigma, which predicted enacted stigma over time. This finding enriches our knowledge about the relationship between stigma and depressive symptoms. Most of the previous studies, if not all, assumed that the negative effect of stigma on depressive symptoms was unidirectional. No previous study explored the potential effect of depressive symptoms on perceived stigma and enacted stigma. According to social ecology theory [42], individuals actively interact with their environmental system in the life span. An individual is never a passive recipient of experiences in the living system, but someone who helps to construct or modify the living system. It is very possible that children with a higher depressive level are more sensitive to society’s negative attitude against HIV-affected families, which may reflect children’s experience of actual stigmatized behaviors towards them or their families over time.
Besides the longitudinal and bidirectional relation among perceived stigma, enacted stigma and depressive symptoms, the within-wave residuals correlations were significant. In accordance with the previous findings [18, 20], perceived stigma and enacted stigma were positively associated with depressive symptoms. However, the initial correlation between enacted stigma and depressive symptoms was stronger than that between perceived stigma and depressive symptoms and these correlations were stable over time. These findings suggest that an increase in stigma, either perceived or enacted, is related to an increase in depressive symptoms.
The current findings elucidating longitudinal and bidirectional relationship among enacted stigma, perceived stigma and depressive symptoms suggest the needs for multilevel interventions in stigma reduction efforts. The different patterns of perceived stigma and enacted stigma in their direction and magnitude of prediction lend support for stigma reduction strategies in various levels of children’s social ecological system. Although the actual stigmatizing actions against children affected by HIV/AIDS appeared to predict depressive symptoms in a proximate manner, perceived stigma also predict depressive symptoms indirectly through enacted stigma, when the latter was presented in children’s life. Future mental health promotion efforts need to emphasize the interplay of enacted stigma, perceived stigma and depressive symptoms, rather than to focus on only one factor or one pathway. Intervention programs aimed at stigma reduction may have potentials to alleviate the negative impact of parental HIV on children’s well-being in both the individual level and the community level to disrupt the vicious circle.
Existing efforts in reducing HIV stigma at a community level, in general, have focused on stigma directed at HIV positive adults and children, and limited studies to date have evaluated the impact of stigma reduction strategies on children affected by parental HIV/AIDS [9]. More rigorous program evaluation is needed in terms of capacity to reduce community stigma and to increase the well-being of HIV-affected families, not only PLHWA but also their family members including children. Meanwhile, intervention efforts may also emphasize the promotion of child resilience in the context of parental death and HIV stigma [17]. A wealth of literature with children in various adversities has suggested substantial individual variation in mental health outcomes, with some children demonstrating amazing resilience even when exposed to chronic or severe stress [43]. Interventions among children or families exposed to HIV stigma can focus on building up individual’s resilience in coping with stigma-related adversities. By integrating modifiable factors that could buffer the impact of stigma-related adversities into intervention programming, we can facilitate individual’s ability to cope with stigma and even thrive in the exposure of stigma-related stress.
The current study has several limitations. First, the study sample may not be representative of children affected by HIV/AIDS in other settings because the HIV epidemic in our research site was primarily due to unhygienic blood collection. Second, the current study did not include internalized stigma to examine the interaction among the three aspects of stigma. We anticipate that internalized stigma might exert negative effect, interactively with perceived stigma and enacted stigma, on children’s psychosocial well-being. The scales measuring perceived stigma and enacted stigma also need to be further validated among other populations. Third, awareness of parental HIV and parental death were reported by children themselves. There might be some inaccuracy in reporting due to various reasons (e.g., stigma, disclosure). Future studies may employ multiple sources of data (e.g., caregiver) to improve the accuracy of the data. Finally, the current study did not control for some variables that might potentially be associated with depressive symptoms and HIV stigma, such as family SES, health status of child, children’s HIV status, children’s awareness and knowledge of HIV transmission.
Despite these limitations, to the best of our knowledge, the present study is among the first efforts to examine the longitudinal relationship among perceived stigma, enacted stigma and depressive symptoms among children affected by HIV/AIDS. The findings underscore the importance to consider different aspects of stigma in affecting children’s psychosocial well-being in future research. The results also imply needs to reduce or mitigate the negative effect of stigma at both individual level and school/community level and to promote mental health of children in the context of parental HIV/AIDS.
Acknowledgments
This study reported in this article was supported by NIH Research Grant from the National Institute of Mental health (R01MH76488) and the National Institute of Nursing Research (R01NR13466). The authors wish to thank Joanne Zwemer for help in preparing the manuscript.
Footnotes
The content of the article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental health and the National Institute of Nursing Research.
References
- 1.UNICEF. Statistics by Area/HIV/AIDS. 2013 [cited 2013 Jan 15, 2013]; Available from: http://www.childinfo.org/hiv_aids_global_trends.html.
- 2.Chi P, Li X. Impact of Parental HIV/AIDS on Children’s Psychological Well-Being: A Systematic Review of Global Literature. AIDS Behav. 2012 doi: 10.1007/s10461-012-0290-2. Epub 09/13/2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crocker J, Major B, Steele R. Social stigma. In: Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social psychology. New York: McGraw Hill; 1998. pp. 504–33. [Google Scholar]
- 4.Goffman E. Stigma: Notes on the management of spoiled identity. New York: Simon & Schuster Inc; 1963. [Google Scholar]
- 5.Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, Wrubel J, et al. HIV-related stigma: Adapting a theoretical framework for use in India. Soc Sci Med. 2008;67(8):1225–35. doi: 10.1016/j.socscimed.2008.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991–1999. Am J Public Health. 2002;92(3):371–7. doi: 10.2105/ajph.92.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herek GM, Gillis JR, Cogan JC. Internalized stigma among sexual minority adults: Insights from a social psychological perspective. J Couns Psychol. 2009;56(1):32. [Google Scholar]
- 8.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Soc Sci Med. 2003;57(1):13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 9.Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: What have we learned? AIDS Educ Prev. 2003;15(1):49–69. doi: 10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- 10.Campbell C, Skovdal M, Mupambireyi Z, Madanhire C, Robertson L, Nyamukapa CA, et al. Can AIDS stigma be reduced to poverty stigma? Exploring Zimbabwean children’s representations of poverty and AIDS. Child Care Health Dev. 2011 doi: 10.1111/j.1365-2214.2011.01311.x. Epub 2011/10/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gausset Q, Mogensen HO, Yameogo WME, Berthé A, Konaté B. The ambivalence of stigma and the double-edged sword of HIV/AIDS intervention in Burkina Faso. Soc Sci Med. 2012;74(7):1037–44. doi: 10.1016/j.socscimed.2011.11.044. [DOI] [PubMed] [Google Scholar]
- 12.Logie C, Gadalla T. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care. 2009;21(6):742–53. doi: 10.1080/09540120802511877. [DOI] [PubMed] [Google Scholar]
- 13.Mak WWS, Poon CYM, Pun LYK, Cheung SF. Meta-analysis of stigma and mental health. Soc Sci Med. 2007;65(2):245–61. doi: 10.1016/j.socscimed.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 14.Surkan PJ, Mukherjee JS, Williams DR, Eustache E, Louis E, Jean-Paul T, et al. Perceived discrimination and stigma toward children affected by HIV/AIDS and their HIV-positive caregivers in central Haiti. AIDS Care. 2010;22(7):803–15. doi: 10.1080/09540120903443392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nyamukapa CA, Gregson S, Wambe M, Mushore P, Lopman B, Mupambireyi Z, et al. Causes and consequences of psychological distress among orphans in eastern Zimbabwe. AIDS Care. 2010;22(8):988–96. doi: 10.1080/09540121003615061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao J, Li X, Fang X, Hong Y, Zhao G, Lin X, et al. Stigma Against Children Affected by AIDS (SACAA): Psychometric evaluation of a brief measurement scale. AIDS Behav. 2010;14(6):1302–12. doi: 10.1007/s10461-009-9629-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boyes ME, Cluver LD. Relationships Among HIV/AIDS Orphanhood, Stigma, and Symptoms of Anxiety and Depression in South African Youth A Longitudinal Investigation Using a Path Analysis Framework. Clin Psychol Sci. 2013;1(3):323–30. [Google Scholar]
- 18.Cluver LD, Orkin M. Cumulative risk and AIDS-orphanhood: Interactions of stigma, bullying and poverty on child mental health in South Africa. Soc Sci Med. 2009;69(8):1186–93. doi: 10.1016/j.socscimed.2009.07.033. [DOI] [PubMed] [Google Scholar]
- 19.Lin X, Zhao G, Li X, Stanton B, Zhang L, Hong Y, et al. Perceived HIV stigma among children in a high HIV-prevalence area in central China: Beyond the parental HIV-related illness and death. AIDS Care. 2010;22(5):545–55. doi: 10.1080/09540120903253999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao G, Li X, Zhao J, Zhang L, Stanton B. Relative importance of various measures of HIV-related stigma in predicting psychological outcomes among children affected by HIV. Community Ment Health J. 2012;48(3):275–83. doi: 10.1007/s10597-011-9424-7. Epub 2011/06/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scambler G. Epilepsy. London: Routledge; 1989. [Google Scholar]
- 22.Liamputtong P, Haritavorn N, Kiatying-Angsulee N. HIV and AIDS, stigma and AIDS support groups: Perspectives from women living with HIV and AIDS in central Thailand. Soc Sci Med. 2009;69(6):862–8. doi: 10.1016/j.socscimed.2009.05.040. [DOI] [PubMed] [Google Scholar]
- 23.Letteney S, LaPorte HH. Deconstructing stigma: perceptions of HIV-seropositive mothers and their disclosure to children. Soc Work Health Care. 2004;38(3):105–23. doi: 10.1300/J010v38n03_06. [DOI] [PubMed] [Google Scholar]
- 24.Maman S, Abler L, Parker L, Lane T, Chirowodza A, Ntogwisangu J, et al. A comparison of HIV stigma and discrimination in five international sites: The influence of care and treatment resources in high prevalence settings. Soc Sci Med. 2009;68(12):2271–8. doi: 10.1016/j.socscimed.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith R, Rossetto K, Peterson BL. A meta-analysis of disclosure of one’s HIV-positive status, stigma and social support. AIDS Care. 2008;20(10):1266–75. doi: 10.1080/09540120801926977. [DOI] [PubMed] [Google Scholar]
- 26.Uys L, Chirwa M, Kohi T, Greeff M, Naidoo J, Makoae L, et al. Evaluation of a health setting-based stigma intervention in five African countries. AIDS Patient Care and STDS. 2009;23(12):1059–66. doi: 10.1089/apc.2009.0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whetten K, Ostermann J, Whetten RA, Pence BW, O’Donnell K, Messer LC, et al. A comparison of the wellbeing of orphans and abandoned children Ages 6–12 in institutional and community-based care settings in 5 less wealthy nations. Plos One. 2009;4(12):e8169. doi: 10.1371/journal.pone.0008169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li L, Lee SJ, Thammawijaya P, Jiraphongsa C, Rotheram-Borus MJ. Stigma, social support, and depression among people living with HIV in Thailand. AIDS Care. 2009;21(8):1007–13. doi: 10.1080/09540120802614358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64(9):1823–31. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.He Z, Ji C. Nutritional status, psychological well-being and the quality of life of AIDS orphans in rural Henan Province, China. Trop Med Int Health. 2007;12(10):1180–90. doi: 10.1111/j.1365-3156.2007.01900.x. [DOI] [PubMed] [Google Scholar]
- 31.West A, Wedgwood K. Children affected by AIDS, orphans and impact mitigation in China. In: Kaufman J, Kleinman A, Saich T, editors. AIDS and social policy in China. Cambridge, MA: Harvard University Asia Center; 2006. pp. 243–64. [Google Scholar]
- 32.UNAIDS, UNICEF, USAID. Children on the brink 2004: A joint report of new orphan, estimates and a framework for Action. New York: 2004. [Google Scholar]
- 33.Xu T, Yan Z, Duan S, Wang C, Rou K, Wu Z. Psychosocial well-being of children in HIV/AIDS-affected families in southwest China: A qualitative study. J Child Fam Stud. 2009;18(1):21–30. [Google Scholar]
- 34.Li X, Barnett D, Fang X, Lin X, Zhao G, Zhao J, et al. Lifetime incidence of traumatic events and mental health among children affected by HIV/AIDS in rural China. J Clin Child Adolesc Psychol. 2009;38(5):731–44. doi: 10.1080/15374410903103601. [DOI] [PubMed] [Google Scholar]
- 35.Dowdney L. Annotation: Childhood bereavement following parental death. J Child Psychol Psychiatry. 2000;41(7):819–30. [PubMed] [Google Scholar]
- 36.Fendrich M, Wessiman MM, Warner V. Screening for depressive disorder in children and adolescents: Validating the Center for Epidemiologic Studies Depression Scale for Children. Am J Epidemiol. 1990;131(3):538–51. doi: 10.1093/oxfordjournals.aje.a115529. [DOI] [PubMed] [Google Scholar]
- 37.Wang X. Rating Scales for Mental Health (Chinese Journal of Mental Health Supplement) Beijing: Chinese Association of Mental Health; 1993. [Google Scholar]
- 38.Muthén LK, Muthén BO. Mplus user’s guide. 5. Los angeles, CA: Author; 2007. [Google Scholar]
- 39.Quintana SM, Maxwell SE. Implications of recent developments in structural equation modeling for counseling psychology. Couns Psychol. 1999;27(4):485–527. [Google Scholar]
- 40.Mukolo A, Heflinger CA, Wallston KA. The stigma of childhood mental disorders: A conceptual framework. J Am Acad Child Adolesc Psychiatry. 2010;49(2):92–103. doi: 10.1097/00004583-201002000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Green SE. The impact of stigma on maternal attitudes toward placement of children with disabilities in residential care facilities. Soc Sci Med. 2004;59(4):799–812. doi: 10.1016/j.socscimed.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 42.Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge, Mass: Harvard University Press; 1979. [Google Scholar]
- 43.Ungar M, Ghazinour M, Richter J. Annual Research Review: What is resilience within the social ecology of human development? J Child Psychol Psychiatry. 2013;54(4):348–66. doi: 10.1111/jcpp.12025. [DOI] [PubMed] [Google Scholar]