Abstract
Objective
Sexually transmitted diseases (STDs) are a significant public health concern. Numerous internalizing and externalizing psychiatric disorders have been found to be related to STD risk. However, to date, no studies have examined several psychiatric disorders simultaneously to account for STD risk. Given that psychiatric disorders often co-occur and can be explained by a limited number of latent dimensions of psychopathology, it is important to examine whether the relationship between STDs and psychiatric disorders is best explained by broad dimensions of psychopathology.
Methods
The current study examined the associations between a range of Axis I and II psychiatric disorders at baseline and rates of STDs at a three-year follow up in a large, nationally representative sample of adults in the United States (n = 34,434). A confirmatory factor analysis (CFA) was conducted to fit three factors, two internalizing and one externalizing. Structural equation modeling (SEM) was used to assess the relationships between and among the factors and STD status and to test for mediation.
Results
In bivariate analyses, most Axis I and II disorders were associated with STD diagnosis at Wave 2, whereas the results of the structural model showed that only the externalizing factor was significantly associated with STD diagnosis at Wave 2. Further, the externalizing factor mediated the relationship between one of the internalizing factors and STD diagnosis.
Conclusion
Findings suggest the unique contribution of externalizing psychopathology to STD risk and the importance of examining latent dimensions of disorders when understanding this relationship between psychiatric disorders and STDs.
Keywords: externalizing, internalizing, sexually transmitted disease, latent factors, structural model
Introduction
Sexually transmitted diseases (STDs) are a significant public health and societal concern. When not detected or treated early, STDs (e.g., HPV, chlamydia, gonorrhea) have the potential to cause serious health problems (e.g., cervical cancer, chronic pelvic pain, ectopic pregnancy [1]). STDs can also increase an individual’s susceptibility for HIV infection [2]. Although both men and women are significantly affected by STDs, women tend to face more serious long-term health consequences, including reproductive health problems and infertility; it is estimated that undiagnosed STDs contribute to infertility for approximately 24,000 women annually [2]. In addition to potentially serious health consequences for those infected, STDs also present a significant burden to the health care system, with direct medical costs for STDs estimated to exceed $16 billion in the United States alone [1].
Individuals with psychiatric disorders are at high risk for STDs [3-8]. This has been found for a range of internalizing and externalizing disorders, including mood disorders [9-11], anxiety disorders [9,11], substance use disorders [9,12,13], and antisocial personality disorder (ASPD; 14). However, the literature in this area has been constrained by several limitations.
First, the majority of studies have narrowly focused on individual psychiatric disorders, rather than examining several psychiatric disorders simultaneously. Given that previous research has shown psychiatric disorders often co-occur and that their pattern of co-occurrence is well explained by a limited number of latent variables representing broad dimensions of psychopathology [15-17], it is important to examine the relationship between STDs and psychiatric disorders taking into account these latent factors. Furthermore, it is important to determine whether the relationship between psychiatric disorders and STDs is best explained by these broad dimensions of psychopathology or by the individual disorders.
Prior work examining the relationship between psychiatric disorders and STD risk also has been constrained by the use of treatment-seeking samples (e.g., 9,11,14), samples with restricted age ranges (e.g., younger populations; 10,12,13,18) and geographical areas (e.g.,19), or sample sizes with limited statistical power or that may not generalize to the larger U.S. population (e.g., 11,14). Finally, most work in this area, particularly among adult populations, has used cross-sectional designs (e.g., 9–11,13,14). It has been suggested that future research in this domain incorporate larger sample sizes, longitudinal designs, and models that include a range of Axis I and II psychiatric disorders simultaneously [3].
As such, the primary objective of the current study was to examine the associations between a broad range of Axis I and II psychiatric disorders and rates of STDs. We sought to build on prior work in this area by using a large, nationally representative sample in the U.S. and assessed psychiatric disorders and STDs over a 3-year period. To take into account broader dimensions of psychiatric disorders, we tested whether the identified associations could be explained by three latent factors identified in previous research [17] or were specific for each psychiatric disorder, and whether these associations were mediated by one or more latent factors.
Method
Participants and Procedure
The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) target population consisted of civilian, non-institutionalized adult individuals over 18 years of age residing in households and group quarters. The survey included individuals residing the continental U.S., District of Columbia, Alaska, and Hawaii. African Americans, Hispanics, and individuals aged 18 to 24 years of age were oversampled, and data were adjusted to reflect design characteristics of the NESARC survey and to account for oversampling and non-response. Face-to-face interviews were conducted by lay interviewers with extensive training and supervision [20, 21].In total, 43,093 respondents were interviewed in Wave 1 from 2001 to 2002.
The Wave 2 interview was conducted approximately three years later (mean interval: 36.6 months). Of respondents that continue to be eligible at Wave 2, the response rate was 86.7%, resulting in 34,653 completed interviews at Wave 2. Sample weights were also developed to adjust for Wave 2 non-response [21]. Participants in the current study were 34,434 respondents who participated in both Waves 1 and 2 of interviews and completed the STD assessment. Participants were 47.9% male, 71% White, mean age of 45.06 (S.E. = 0.17), mean education years 13.80 (SE = 0.05), mean individual income of $30,120 (S.E. = 0.53), 63.1% married, 16.4% widowed/separated/divorced, and 20.5% never married. At Wave 2, 0.54% had an STD in the past year (n = 194), and 99.46% did not have an STD in the past year (n = 34,240). Individuals (n = 219) who had missing data for the STD assessment at Wave 2 were not included in this study. All procedures contributing to this work were in accordance with the Declaration of Helsinki for experiments involving humans.
Assessment of DSM-IV Axis I and II disorders at Wave 1
The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV (AUDADIS-IV; 22) Wave 1 version was used to assess DSM-IV Axis I and II disorders. The AUDADIS-IV is a structured diagnostic interview designed for lay professional interviewers to measure substance use and mental disorders in large-scale surveys. Computer algorithms were used to diagnose all DSM-IV Axis I and II disorders at Wave 1. Axis I diagnoses included substance use disorders (alcohol use disorder, drug use disorder, and nicotine dependence), mood disorders (major depressive disorder, dysthymic disorder, and bipolar disorder), anxiety disorders (panic disorder, social anxiety disorder, specific phobia, and generalized anxiety disorder), and pathological gambling. For all Axis I disorders, diagnoses were made in the past 12 months prior to Wave 1. All diagnoses reported were “primary” such that they exclude disorders characterized as “substance-induced” or due to a general medical condition, and they all met the clinical significance criterion. Axis II disorders were assessed on a lifetime basis and required long-term patterns of social and occupational impairment [23]. Further, at least one symptom reported had to cause distress or social or occupational dysfunction. The AUDADIS-IV Wave 1 version included assessment of avoidant, dependent, obsessive-compulsive, paranoid, schizoid, histrionic, and antisocial personality disorders. Test-retest reliability and validity of the AUDADIS-IV measures of the DSM-IV disorders are adequate and have been reported in detail elsewhere; overall reliability is good for MDD (k = 0.65-0.73), good to excellent for SUDs (k = 0.70-0.84), and fair to good for other mood and anxiety disorders (k = 0.65-0.73) and personality disorders (k = 0.40-0.67) [20,21,23,24].
Assessment of STD incidence at Wave 2
Rates of STD in the past 12-months was determined if the respondent indicated that they had an STD (e.g., gonorrhea, syphilis, chlamydia) diagnosed and confirmed by a health professional in the 12 months prior to participation in the Wave 2 interview. This item was assessed separately from HIV status and asks specifically “In the last 12 months, did you have any other sexually transmitted diseases or venereal diseases [excluding HIV] like gonorrhea, syphilis, chlamydia, or herpes?”
Statistical Analyses
We first examined the bivariate relationships between Wave 1 psychiatric disorders and Wave 2 STD status adjusting for relevant sociodemographic characteristics that have been previously shown to be associated with STD risk, such as age [25], gender [26], race/ethnicity [27], education level [28], income [29], and marital status [30]. Weighted percentages and means were computed to derive past year prevalence of Axis I disorders and lifetime presence of select Axis II disorders at Wave 1 and STD status (yes/no) at Wave 2. A set of bivariate analyses yielded adjusted odds ratios (AORs) and 95% confidence intervals (CIs) indicating measures of association between Wave 1 diagnostic characteristics and STD status at Wave 2.
Next, we used confirmatory factor analysis (CFA) to identify latent factors underlying the individual psychiatric disorders assessed at Wave 1. This was done to more parsimoniously predict STD risk with disorder clusters by taking into account shared variance across disorders. We tested a three-factor model with two internalizing dimensions and one externalizing, which was based upon a previously tested three-factor model in this sample [17]. To determine model fit, we examined goodness-of-fit measures such as the comparative fit index (CFI), the Tucker-Lewis index (TLI), and the root mean squared error of approximation (RMSEA). CFI and TLI values greater than 0.95 and values of RMSEA less than 0.06 are commonly used to indicate good model fit [31].
Finally, we examined the relationship between the latent factors of the psychiatric disorders at Wave 1 and STD status at Wave 2. Structural equation modeling was used to regress STD status on the latent factors of psychiatric disorders identified in the CFA, adjusting for the demographic characteristics listed above. Initially an SEM was fit without specifying any causal relationships among the latent factors but simply allowing them to be mutually correlated. Standardized estimates of the relationship between STD status and each latent factor indicate how many standard deviations higher (or lower) the mean of the latent variable underlying the binary outcome is expected to be for each increase in an additional unit of that latent factor while controlling for the other factors and covariates. Modification indices (i.e. chi-square tests with 1 d.f.) were examined to test if any residuals associated with specific disorders are correlated with the STD outcome. If a residual association is found to be significant, this would indicate a particular disorder is associated with STD above and beyond the association induced by the latent variable. In an attempt to further explicate the relationships among the latent factors and how they combine to influence STD, we tested a second SEM that assumed the externalizing factor was a mediator of the effects of the internalizing factors on STD. Indirect effects (i.e. mediation effect) were estimated using the product rule and tested using standard delta method approaches. All analyses were conducted in Mplus, which takes into account the NESARC sampling weights and design effects in all analyses, including a parameter as well as standard error estimation and model fit calculations.
Results
Bivariate analyses between Wave 1 psychiatric disorders and Wave 2 STD status
Table 1 shows bivariate analyses between Wave 1 psychiatric disorders and Wave 2 STD status. After adjusting for sociodemographic characteristics listed above, past year alcohol use disorder (AUD), nicotine dependence, major depressive disorder (MDD), bipolar disorder, and panic disorder were associated with a greater likelihood of having an STD diagnosis at Wave 2. All Axis II disorders, with the exception of dependent personality disorder, were also associated with higher rates of STDs at Wave 2.
Table I.
Bivariate analysis between psychiatric disorders at Wave 1 and STD status at Wave 2 past year adjusting for relevant demographic characteristics.
| Disorders at Wave 1 | With STD at Wave 2 (N=194, 0.54%) |
Without STD at Wave 2 (N=34240, 99.46%) |
Adjusted Odds Ratios |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| n | % | S.E . |
Row % |
S.E . |
n | % | S.E. | Row % |
S.E. | AO R |
95% CI | ||
| Axis I disorders | |||||||||||||
|
| |||||||||||||
| Alcohol use disorder |
3 8 |
26.0 1 |
5.2 3 |
1.71 | 0.4 3 |
2644 | 8.18 | 0.2 5 |
98.2 9 |
0.43 | 2.9 8 |
1.6 7 |
5.3 1 |
| Drug use disorder | 9 | 4.14 | 1.5 1 |
1.17 | 0.4 4 |
599 | 1.92 | 0.1 0 |
98.8 3 |
0.44 | 1.3 0 |
0.5 9 |
2.8 7 |
| Nicotine dependence |
4 1 |
27.0 1 |
5.0 3 |
1.18 | 0.2 8 |
3961 | 12.36 | 0.3 8 |
98.8 2 |
0.28 | 2.1 0 |
1.3 3 |
3.3 3 |
| Major depressive disorder |
2 5 |
13.5 6 |
3.0 9 |
1.41 | 0.3 4 |
1891 | 5.18 | 0.1 6 |
98.5 9 |
0.34 | 2.0 5 |
1.1 9 |
3.5 4 |
| Bipolar disorder | 1 7 |
9.18 | 2.6 8 |
1.88 | 0.5 7 |
934 | 2.62 | 0.1 2 |
98.1 2 |
0.57 | 2.3 6 |
1.2 3 |
4.5 3 |
| Dysthymic disorder | 4 | 3.74 | 1.9 7 |
1.65 | 0.8 9 |
473 | 1.22 | 0.0 7 |
98.3 5 |
0.89 | 2.6 1 |
0.8 7 |
7.7 9 |
| Panic disorder | 1 3 |
7.46 | 2.5 9 |
1.92 | 0.6 8 |
755 | 2.09 | 0.1 0 |
98.0 8 |
0.68 | 2.8 4 |
1.2 8 |
6.2 9 |
| Social anxiety disorder |
9 | 5.95 | 2.6 0 |
1.14 | 0.5 4 |
976 | 2.82 | 0.1 3 |
98.8 6 |
0.54 | 1.7 9 |
0.7 2 |
4.4 5 |
| Specific phobia | 1 9 |
12.0 2 |
3.2 2 |
0.91 | 0.2 8 |
2547 | 7.14 | 0.2 7 |
99.0 9 |
0.28 | 1.4 3 |
0.7 7 |
2.6 4 |
| Generalized anxiety disorder |
1 1 |
5.39 | 2.1 4 |
1.43 | 0.5 7 |
731 | 2.03 | 0.1 0 |
98.5 7 |
0.57 | 2.0 9 |
0.9 0 |
4.8 4 |
| Pathological gambling |
1 | 0.64 | 0.6 3 |
2.20 | 2.1 9 |
63 | 0.15 | 0.0 2 |
97.8 0 |
2.19 | 3.5 4 |
0.4 5 |
27. 51 |
|
| |||||||||||||
| Axis II disorders | |||||||||||||
|
| |||||||||||||
| Avoidant PD | 1 0 |
7.68 | 3.0 3 |
1.80 | 0.7 7 |
807 | 2.30 | 0.1 2 |
98.2 0 |
0.77 | 2.5 2 |
1.0 8 |
5.8 7 |
| Dependent PD | 3 | 1.33 | 0.8 5 |
1.70 | 1.0 8 |
142 | 0.42 | 0.0 5 |
98.3 0 |
1.08 | 1.9 8 |
0.5 2 |
7.5 8 |
| Obsessive compulsive PD |
3 1 |
17.1 8 |
3.7 1 |
1.16 | 0.2 9 |
2710 | 8.03 | 0.2 3 |
98.8 4 |
0.29 | 2.1 8 |
1.2 9 |
3.6 7 |
| Paranoid PD | 2 3 |
11.4 0 |
3.1 6 |
1.43 | 0.4 6 |
1657 | 4.29 | 0.1 6 |
98.5 7 |
0.46 | 2.0 9 |
1.1 4 |
3.8 5 |
| Schizoid PD | 1 3 |
7.54 | 2.2 4 |
1.33 | 0.4 2 |
1127 | 3.05 | 0.1 3 |
98.6 7 |
0.42 | 2.2 3 |
1.1 5 |
4.3 2 |
| Histrionic PD | 1 3 |
5.66 | 1.7 7 |
1.72 | 0.5 5 |
632 | 1.77 | 0.0 9 |
98.2 8 |
0.55 | 2.1 1 |
1.0 4 |
4.2 6 |
| Antisocial PD | 1 9 |
12.5 3 |
3.3 6 |
1.88 | 0.5 8 |
1128 | 3.58 | 0.1 6 |
98.1 2 |
0.58 | 3.3 2 |
1.8 2 |
6.0 6 |
Note: All Axis I disorders were past year diagnoses; PD = Personality disorder. Percentages are weighted to reflect prevalence in U.S. population. Adjusted odds ratios are adjusted for demographic characteristics adjusted for in SEM model (age, gender, race/ethnicity, education, income, marital status).
Confirmatory Factor Analysis (CFA)
We fitted a CFA to account for known patterns of co-occurrence across disorders (Table 2). We fit three factors, two internalizing and one externalizing based upon the three-factor model previously tested in this sample [17]. Factor 1, the externalizing factor, included past year AUD, DUD, nicotine dependence, pathological gambling, and antisocial personality disorder. Factor 2, one of the internalizing factors included bipolar disorder, panic disorder, social anxiety disorder, specific phobia, and the remaining personality disorders (avoidant personality disorder, depressive personality disorder, obsessive compulsive personality disorder, paranoid personality disorder, schizoid personality disorder, and histrionic personality disorder). Factor 3, the second internalizing factor included MDD, DD, and GAD. This model provided good fit (RMSEA = 0.014, CFI = 0.962, TLI = 0.956), which is consistent with previously published empirical support for this model [17]. Factor 1 (externalizing) had a correlation with Factor 2 of 0.62, Factors 1 and 3 had a correlation of 0.44, and Factors 2 and 3 had a correlation of 0.67.
Table II.
CFA for Wave 1 past year psychiatric disorders
| MODEL | 3-Factor Model | |||
|---|---|---|---|---|
|
| ||||
| CFI | 0.962 | |||
| TLI | 0.956 | |||
| RMSEA | 0.014 | |||
|
| ||||
| Prevalence | Item (Standardized Result) | Factor 1 | Factor 2 | Factor 3 |
|
| ||||
| 0.083 | Alcohol use disorder | 0.573 | - | - |
| 0.019 | Drug use disorder | 0.783 | - | |
| 0.124 | Nicotine dependence | 0.669 | - | |
| 0.052 | Major depressive disorder | - | 0.716 | |
| 0.027 | Bipolar disorder | - | 0.734 | - |
| 0.012 | Dysthymic disorder | - | 0.781 | |
| 0.021 | Panic disorder | - | 0.649 | - |
| 0.028 | Social anxiety disorder | - | 0.712 | - |
| 0.072 | Specific phobia | - | 0.555 | - |
| 0.020 | Generalized anxiety disorder | - | 0.930 | |
| 0.002 | Pathological gambling | 0.539 | - | |
| 0.023 | Avoidant PD | - | 0.828 | - |
| 0.004 | Dependent PD | - | 0.843 | - |
| 0.081 | Obsessive compulsive PD | - | 0.666 | - |
| 0.043 | Paranoid PD | - | 0.848 | - |
| 0.031 | Schizoid PD | - | 0.733 | - |
| 0.018 | Histrionic PD | - | 0.725 | - |
| 0.036 | Antisocial PD | 0.774 | - | |
Note: PD = Personality disorder
Structural Equation Models
In Table 3, we present the results of the initial structural equation model used to test the association between STDs and psychiatric disorders, taking into account the latent dimensions of psychiatric disorders and relevant demographic characteristics. In this model, no specific causal relationships are assumed between any of the three latent dimensions hence they are all mutually controlling for one another. The standardized estimates of the direct relationship between the three factors of psychiatric disorders at Wave 1 and STD status at Wave 2 indicate that, after adjusting for other covariates and each other, only the externalizing factor had a significant direct effect on greater likelihood of having an STD at Wave 2. Moreover, there were no direct effects from any specific disorder to STD as assessed by finding no modification indices significant between residuals for disorders and STD. Being older and male (vs. female) decreased the probability of STD, whereas being divorced/separated/ widowed (vs. married) increased the likelihood of STD.
Table III.
Prediction of STD Status at Wave 2 from Factor Scores at Wave 1 adjusting for demographic characteristics
| MODEL | 3-factor model | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Fact or 1 |
Fact or 2 |
Fact or 3 |
Male | Whit e |
Age | Education years |
Inco me |
Widow/Sep arated/ Divorced |
Sin gle |
||
| 0.0 05 |
STD on (STD standardized result) |
0.24
1 |
- 0.00 5 |
0.06 8 |
-
0.19 6 |
0.14 9 |
-
0.01 9 |
0.016 | - 0.00 1 |
0.332 | 0.0 98 |
| p-value | 0.00 2 |
0.96 4 |
0.51 7 |
0.00 1 |
0.06 3 |
<0. 001 |
0.235 | 0.55 8 |
<0.001 | 0.2 51 |
|
Note: There is no item with modification index greater or equal to 10 to predict STD in addition.
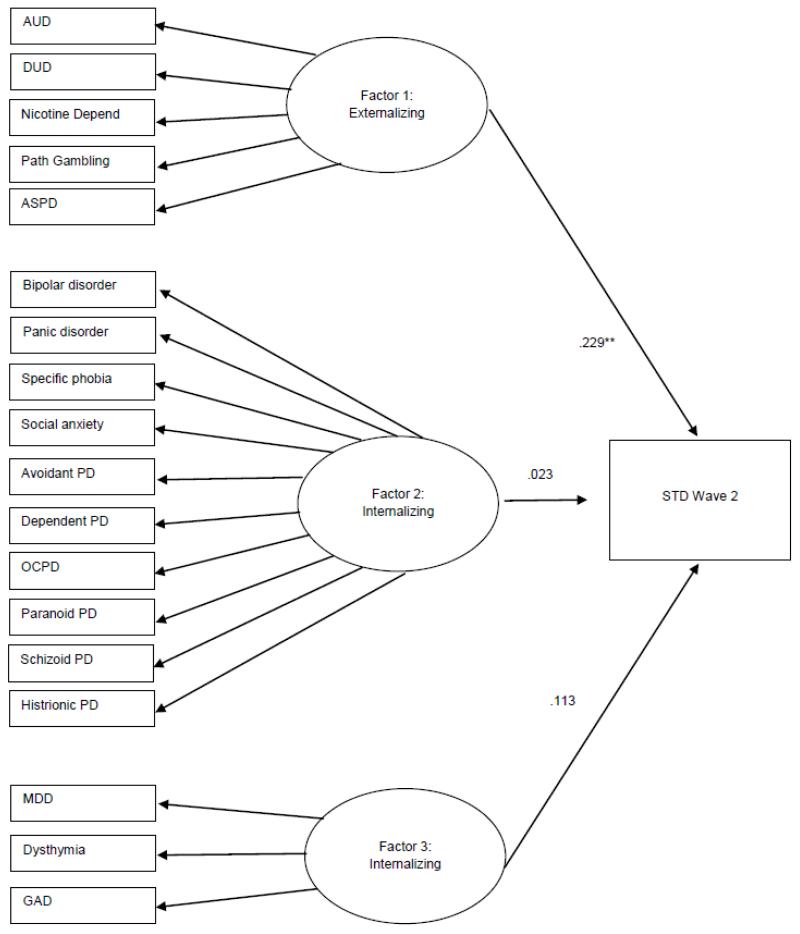
To test the robustness of our results, we also tested the same SEM without any demographic covariates included. The results remained consistent such that only the direct relationship between the externalizing factor and STD was statistically significant. See Figure 1 for these results and a visual depiction of the model.
Figure 1.
Results of SEM model testing the association between latent dimensions of psychiatric disorders and STDs without covariates.
Note: ** p = .004; all other p values > 0.1
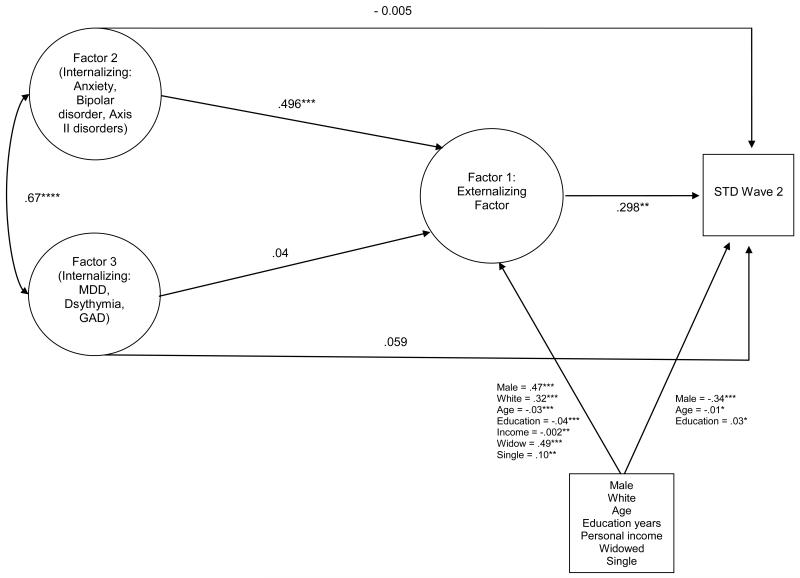
Because the internalizing and externalizing factors are moderate to highly correlated with one another, we additionally tested the possibility that the effects of the internalizing factors on STD may, in fact, be mediated by their influence on the externalizing factor. That is, we set out to test if either internalizing factor has an indirect effect on STD through its effect on externalizing. Figure 2 depicts the results from the SEM model testing the mediating role of Factor 1, the externalizing factor, in relation to the association between both internalizing factors (Factors 2 and 3) and STD status. Findings demonstrate the role of Factor 1 in mediating the relationship between Factor 2 (underlying anxiety disorders, bipolar disorder, and Axis II disorders) and STD but not the relationship between Factor 3 (the internalizing factor made up of MDD, dysthymia, and GAD) and STD. There was a significant indirect relationship between Factor 2 and STD through the externalizing Factor 1 (β = 0.15; p = 0.003). The other internalizing factor, Factor 3, did not show a significant indirect effect on STD through the externalizing Factor 1 (β = .01; p = .31). The relationship between Factor 3 and Factor 1 also was non-significant (p = .30). There were several significant effects of covariates on Factor 1 and STD status (See Figure 2).
Figure 2.
Results of SEM model testing mediating role of Factor 1 (Externalizing Factor).
Note: **** p < .0001; *** p < .001; ** p < .01; * p < .05.
Conclusion
To our knowledge, the current study is the first to empirically test the relationship between the latent structure of psychiatric disorders and STDs among a nationally-representative sample of adults followed prospectively over time. The latent model of past year psychiatric disorders used is consistent with previous research in this area, which has documented that typically two to three correlated factors fit common psychiatric disorders among adults, including a single externalizing factor and a variable number of internalizing factors [15,16,32,33]. The latent model in this study is one of few models to date that have included a range of both Axis I and II disorders, and as such there may be some differences in the number of factors identified depending on which disorders have been included across studies, yet consistently a clear externalizing dimension and at least one internalizing dimension emerges [34, 35].
Findings in the bivariate analyses confirm prior research that many psychiatric disorders increase risk for STD (e.g., 9, 14). Although these findings shed light on the individual relationships between specific psychiatric disorders and STDs, without accounting for the shared variance between these disorders and the potential mediating effects of broader dimensions of psychopathology, their relative impact on STDs is unclear. When more clearly assessing relative impact, only the externalizing dimension remained significantly associated with STD status after accounting for other comorbid disorders through both structural models.
The findings from the SEM model suggest that the relationship between select anxiety, mood, and personality disorders and STD status is mediated by their co-occurrence with externalizing disorders. That some internalizing disorders may be related to STD status at least in part due to their co-occurrence with externalizing disorders is consistent with previous findings from the adolescent literature (e.g., 36). Our findings are in accord with research that has pointed to the role of externalizing symptoms (e.g., substance use) in mediating the relationship between psychological distress and STD risk behaviors among youth [37]. To date there has been a much greater focus on the role of internalizing disorders in relation to STD risk among adolescents and young adults as opposed to adult populations, and to our knowledge existing research has not tested whether externalizing symptoms account for the relationship between internalizing disorders and STD risk among adults. These findings also suggest that depressive disorders and GAD alone may not confer risk for STD and their association with STD is due to the confounding effects of their co-occurrence with externalizing disorders. This may help clarify the mixed findings identified previously in the literature regarding the relationship between depressive symptoms [38] and generalized anxiety [11] with STD, such that these relationships may only be apparent when externalizing symptomatology co-occurs.
The current study highlights the role externalizing disorders may play in the relationship between psychiatric disorders and STDs. Disorders that load on the externalizing factor appear to share disinhibition, or impulsivity, as a common characteristic; thus, a propensity towards impulsivity may lead to specific difficulties inhibiting desires to engage in sexually risky behaviors [39]. Additionally, intoxication from substance use may decrease the likelihood of practicing safer sex behaviors. This is consistent with research pointing to sensation seeking, a disinhibition-based trait characterized by the tendency to pursue novelty and arousing experiences, accounting for this relationship between substance use and risky sexual behavior [40]. Our findings are in line with modern conceptualizations that emphasize the role of broad underlying dimensions, rather than individual disorders, as the key constructs to understand psychopathology and its relationships with other medical disorders [15,41].
The results of the current study may also inform clinical practice. Given that externalizing disorders are associated with increased STD risk, prevention interventions may benefit from integrating traditional sexual risk reduction techniques with empirically-supported treatments for emotion regulation, impulsivity, or substance dependence [42,43]. Traditional behavioral STD/HIV prevention interventions typically yield significant, yet modest effects [44,45]. It has been hypothesized that one limitation of these approaches is that they fail to address the psychosocial context in which much of elevated sexual risk behaviors occur, and data indicate that psychosocial problems moderate the degree in which traditional prevention interventions are effective, in that psychological distress can interfere with the uptake of these interventions [46]. Integrating evidence-based interventions for co-occurring psychiatric disorders may enhance the efficacy of traditional STD prevention efforts, for instance combining information, motivation, and behavioral skills training with explicit treatment of the psychosocial problems that place individuals at risk for engaging in sexual risk behaviors [7,45]; providing psychoeducation alone without treating co-occurring symptomatology may not be sufficient to affect change in sexual risk behavior among individuals with psychiatric symptoms [5]. Combining interventions to address constructs that may underlie much of externalizing pathology, such as emotional dysregulation (e.g, 47) impulsivity (e.g. 48), or substance dependence (e.g., 49) with sexual risk reduction may be an effective approach to addressing the interplay between externalizing psychopathology and STD prevention [6]. Additionally, it may be important to integrate sexual risk reduction interventions into substance abuse treatment, particularly for substance abusing individuals who may not perceive themselves at high risk for STDs, and thus may be more likely to seek substance abuse treatment than STD/HIV prevention programs.
Despite the novel findings, the current study is not without limitations. Although we collected data on psychiatric disorders in Wave 1 and STDs in Wave 2, causality cannot be inferred. Additionally, although an extensive list of Axis I and II disorders are included in the diagnostic assessment of the NESARC, this list is not all-inclusive. Some disorders that may also affect STD risk, such as psychotic disorders [3], were not included in the standardized assessment and not included in the current study.
Finally, to limit respondents’ burden, STDs were assessed using a single item that did not distinguish between specific types of STDs; this is an important distinction for future replications of this work. STD assessment also was based on self-report of diagnosis and confirmation of diagnosis by a health professional, rather than verification with testing reports or medical records. However, use of a single question and self-report of STDs should be biased in the direction of underreporting and thus towards the null [50]. Thus, our results are likely to be robust.
Indeed in our sample, 0.54% reported having an STD at Wave 2 (n = 194), a low rate which is likely conservative for a few reasons. This rate likely excludes individuals with asymptomatic STDs in the past year, as well as those without access to health care for testing and confirmation of diagnosis. Additionally, our sample was largely middle-aged, which may also reflect the lower rates of STDs than may have been expected, given that adolescents and young adults account for approximately half of all new STDs in the U.S. each year [51].
In summary, this is the first study to use latent variable techniques to examine the relationship between psychiatric disorders and STD risk. After accounting for co-occurrence of disorders, externalizing psychopathology was uniquely related to increased likelihood of acquiring STDs among a nationally-representative sample of U.S. adults and mediated the relationship between select internalizing disorders and STD risk. Addressing mechanisms underlying externalizing psychopathology (e.g., impulsivity, sensation seeking) and the development of integrated interventions that address sexual risk behaviors in the context of co-occurring externalizing pathology may be fruitful areas for future research.
Acknowledgements
The National Epidemiologic Survey on Alcohol and Related Conditions was sponsored by the National Institute on Alcohol Abuse and Alcoholism with supplemental support from the National Institute on Drug Abuse. Dr. Blanco’s work on this manuscript was supported by NIH grants DA019606, DA023973, MH076051 and MH082773 and the New York State Psychiatric Institute. Dr. Magidson’s work on this manuscript was supported by NIH grants R36DA034513 and T32MH093310. Dr. Blashill was supported by K23MH096647.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
The authors have no competing interests to report.
References
- [1].Centers for Disease Control and Prevention (CDC) Incidence, Prevalence, and Cost of Sexually Transmitted Infections in the United States. 2013 Available from http://www.cdc.gov/std/stats/STI-Estimates-Fact-Sheet-Feb-2013.pdf.
- [2].CDC STD Trends in the United States. 2011 National Data for Chlamydia, Gonorrhea, and Syphilis. 2011 Available from http://www.cdc.gov/std/stats11/trends-2011.pdf.
- [3].Otto-Salaj LL, Stevenson LY. Influence of psychiatric diagnoses and symptoms on HIV risk behavior in adults with serious mental illness. AIDS Read. 2001;11:197–204. 206–8. [PubMed] [Google Scholar]
- [4].Carey MP, Carey KB, Weinhardt LS, Gordon CM. Behavioral risk for HIV infection among adults with a severe and persistent mental illness: patterns and psychological antecedents. Community Ment Health J. 1997;33:133–42. doi: 10.1023/a:1022423417304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].McKinnon K, Cournos F, Sugden R, Guido JR, Herman R. The relative contributions of psychiatric symptoms and AIDS knowledge to HIV risk behaviors among people with severe mental illness. J Clin Psychiatry. 1996;57:506–13. doi: 10.4088/jcp.v57n1101. [DOI] [PubMed] [Google Scholar]
- [6].Brown LK, Danovsky MB, Lourie KJ, DiClemente RJ, Ponton LE. Adolescents with psychiatric disorders and the risk of HIV. J Am Acad Child Adolesc Psychiatry. 1997;36:1609–17. doi: 10.1016/S0890-8567(09)66573-4. [DOI] [PubMed] [Google Scholar]
- [7].Carey MP, Carey KB, Kalichman SC. Risk for human immunodeficiency virus (HIV) infection among persons with severe mental illnesses. Clin Psychol Rev. 1997;17:271–91. doi: 10.1016/s0272-7358(97)00019-6. [DOI] [PubMed] [Google Scholar]
- [8].Davidson S, Judd F, Jolley D, Hocking B, Thompson S, Hyland B. Risk factors for HIV/AIDS and hepatitis C among the chronic mentally ill. Aust N Z J Psychiatry. 2001;35:203–9. doi: 10.1046/j.1440-1614.2001.00867.x. [DOI] [PubMed] [Google Scholar]
- [9].Carey MP, Carey KB, Maisto SA, Schroder KEE, Vanable PA, Gordon CM. HIV risk behavior among psychiatric outpatients: association with psychiatric disorder, substance use disorder, and gender. J Nerv Ment Dis. 2004;192:289–96. doi: 10.1097/01.nmd.0000120888.45094.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ramrakha S, Caspi A, Dickson N, Moffitt TE, Paul C. Psychiatric disorders and risky sexual behaviour in young adulthood: cross sectional study in birth cohort. BMJ. 2000;321:263–6. doi: 10.1136/bmj.321.7256.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Shoptaw S, Peck J, Reback CJ, Rotheram-Fuller E. Psychiatric and substance dependence comorbidities, sexually transmitted diseases, and risk behaviors among methamphetamine-dependent gay and bisexual men seeking outpatient drug abuse treatment. J Psychoactive Drugs. 2003;35(Suppl 1):161–8. doi: 10.1080/02791072.2003.10400511. [DOI] [PubMed] [Google Scholar]
- [12].Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, Washburn JJ. Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatr Serv. 2005;56:823–8. doi: 10.1176/appi.ps.56.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Cavazos-Rehg PA, Spitznagel EL, Bucholz KK, Norberg K, Reich W, Nurnberger J, Jr, et al. The relationship between alcohol problems and dependence, conduct problems and diagnosis, and number of sex partners in a sample of young adults. Alcohol Clin Exp Res. 2007;31:2046–52. doi: 10.1111/j.1530-0277.2007.00537.x. [DOI] [PubMed] [Google Scholar]
- [14].Erbelding EJ, Hutton HE, Zenilman JM, Hunt WP, Lyketsos CG. The prevalence of psychiatric disorders in sexually transmitted disease clinic patients and their association with sexually transmitted disease risk. Sex Transm Dis. 2004;31:8–12. doi: 10.1097/01.OLQ.0000105326.57324.6F. [DOI] [PubMed] [Google Scholar]
- [15].Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56:921–6. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- [16].Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–37. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- [17].Blanco C, Krueger RF, Hasin DS, Liu S-M, Wang S, Kerridge BT, et al. Mapping common psychiatric disorders: structure and predictive validity in the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry. 2013;70:199–208. doi: 10.1001/jamapsychiatry.2013.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Elkington KS, Teplin LA, Mericle AA, Welty LJ, Romero EG, Abram KM. HIV/sexually transmitted infection risk behaviors in delinquent youth with psychiatric disorders: a longitudinal study. J Am Acad Child Adolesc Psychiatry. 2008;47:901–11. doi: 10.1097/CHI.0b013e318179962b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].O’Leary A, Broadwell SD, Yao P, Hasin D. Major depression, alcohol and drug use disorders do not appear to account for the sexually transmitted disease and HIV epidemics in the southern United States. Sex Transm Dis. 2006;33:S70–77. doi: 10.1097/01.olq.0000204840.90020.88. [DOI] [PubMed] [Google Scholar]
- [20].Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:807–16. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- [21].Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14:1051–66. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Grant B, Dawson D, Hasin D. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 2001. [Google Scholar]
- [23].Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Stinson FS, Dawson DA, Goldstein RB, Chou SP, Huang B, Smith SM, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV narcissistic personality disorder: results from the wave 2 national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2008;69:1033–45. doi: 10.4088/jcp.v69n0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].CDC STD Health Equity - Rates by Age. 2011 Available from http://www.cdc.gov/std/health-disparities/age.htm.
- [26].CDC Health Equity - Rates by Gender. 2011 Available from http://www.cdc.gov/std/health-disparities/gender.htm.
- [27].CDC STD Health Equity - Rates by Race or Ethnicity. 2011 Available from http://www.cdc.gov/std/health-disparities/race.htm.
- [28].Hampton MC, Halkitis PN, Storholm ED, Kupprat SA, Siconolfi DE, Jones D, et al. Sexual risk taking in relation to sexual identification, age, and education in a diverse sample of African American men who have sex with men (MSM) in New York City. AIDS Behav. 2013;17:931–8. doi: 10.1007/s10461-012-0139-8. [DOI] [PubMed] [Google Scholar]
- [29].Ickovics JR, Beren SE, Grigorenko EL, Morrill AC, Druley JA, Rodin J. Pathways of risk: Race, social class, stress, and coping as factors predicting heterosexual risk behaviors for HIV among women. AIDS Behav. 2002;6:339–50. [Google Scholar]
- [30].Wayment HA, Wyatt GE, Tucker MB, Romero GJ, Carmona JV, Newcomb M, et al. Predictors of risky and precautionary sexual behaviors among single and married white women. J Appl Soc Psychol. 2003;33:791–816. [Google Scholar]
- [31].Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. 1999;6:1–55. [Google Scholar]
- [32].Vollebergh WA, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Arch Gen Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- [33].Kendler KS, Aggen SH, Knudsen GP, Røysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. Am J Psychiatry. 2011;168:29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Arch Gen Psychiatry. 2011;68:1003–11. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- [35].Røysamb E, Kendler KS, Tambs K, Orstavik RE, Neale MC, Aggen SH, et al. The joint structure of DSM-IV Axis I and Axis II disorders. J Abnorm Psychol. 2011;120:198–209. doi: 10.1037/a0021660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Brown LK, Hadley W, Stewart A, Lescano C, Whiteley L, Donenberg G, et al. Psychiatric disorders and sexual risk among adolescents in mental health treatment. J Consult Clin Psychol. 2010;78:590–7. doi: 10.1037/a0019632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Elkington KS, Bauermeister JA, Zimmerman MA. Psychological distress, substance use, and HIV/STI risk behaviors among youth. J Youth Adolesc. 2010;39:514–27. doi: 10.1007/s10964-010-9524-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychol. 2001;20:291–299. doi: 10.1037//0278-6133.20.4.291. [DOI] [PubMed] [Google Scholar]
- [39].Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E. Understanding AIDS-risk behavior among adolescents in psychiatric care: links to psychopathology and peer relationships. J Am Acad Child Adolesc Psychiatry. 2001;40:642–53. doi: 10.1097/00004583-200106000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Kalichman SC, Heckman T, Kelly JA. Sensation seeking as an explanation for the association between substance use and HIV-related risky sexual behavior. Arch Sex Behav. 1996;25:141–54. doi: 10.1007/BF02437933. [DOI] [PubMed] [Google Scholar]
- [41].Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–51. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- [42].O’Cleirigh C, Safren S. Breaking the mold or business as usual? Meeting the challenges of HIV prevention in people with serious mental illness and substance use disorders. Clin Psychol Sci Pract. 2007;14:34–8. [Google Scholar]
- [43].Walkup J, Blank MB, Gonzalez JS, Safren S, Schwartz R, Brown L, et al. The impact of mental health and substance abuse factors on HIV prevention and treatment. J Acquir Immune Defic Syndr. 2008;47(Suppl 1):S15–19. doi: 10.1097/QAI.0b013e3181605b26. [DOI] [PubMed] [Google Scholar]
- [44].Herbst JH, Sherba RT, Crepaz N, Deluca JB, Zohrabyan L, Stall RD, et al. A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. J Acquir Immune Defic Syndr. 2005;39:228–41. [PubMed] [Google Scholar]
- [45].Noar SM. Behavioral interventions to reduce HIV-related sexual risk behavior: review and synthesis of meta-analytic evidence. AIDS Behav. 2008;12:335–53. doi: 10.1007/s10461-007-9313-9. [DOI] [PubMed] [Google Scholar]
- [46].Mimiaga MJ, Noonan E, Donnell D, Safren SA, Koenen KC, Gortmaker S, et al. Childhood sexual abuse is highly associated with HIV risk-taking behavior and infection among MSM in the EXPLORE Study. J Acquir Immune Defic Syndr. 2009;51:340–8. doi: 10.1097/QAI.0b013e3181a24b38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Barlow DH, Ellard KK, Fairholme TJ, Boisseau CL, Ehrenreich May JT, Allen LB. Unified protocol for the transdiagnostic treatment of emotional disorders: Workbook 2011. Oxford University Press; USA: [Google Scholar]
- [48].Stratton KJ. Mindfulness-based approaches to impulsive behaviors. New Sch Psychol Bull. 2009:4. [Google Scholar]
- [49].McHugh RK, Hearon BA, Otto MW. Cognitive-Behavioral Therapy for Substance Use Disorders. Psychiatr Clin North Am. 2010;33:511–25. doi: 10.1016/j.psc.2010.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Clark LR, Brasseux C, Richmond D, Getson P, D’Angelo LJ. Are adolescents accurate in self-report of frequencies of sexually transmitted diseases and pregnancies? J Adolesc Health Off Publ Soc Adolesc Med. 1997;21:91–6. doi: 10.1016/s1054-139x(97)00042-6. [DOI] [PubMed] [Google Scholar]
- [51].Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MCB, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40:187–93. doi: 10.1097/OLQ.0b013e318286bb53. [DOI] [PubMed] [Google Scholar]