Abstract
Background
A closed pleural biopsy is commonly performed for diagnosing patients exhibiting pleural effusion if prior thoracentesis is not diagnostic. However, the diagnostic yield of such biopsies is unsatisfactory. Instead, a thoracoscopic pleural biopsy is more useful and less painful.
Methods
We compared the diagnostic yield of needle thoracoscopic pleural biopsy performed under local anesthesia with that of closed pleural biopsy. Sixty-seven patients with pleural effusion were randomized into groups A and B. Group A patients were subjected to closed pleural biopsies, and group B patients were subjected to pleural biopsies performed using needle thoracoscopy under local anesthesia.
Results
The diagnostic yields and complication rates of the two groups were compared. The diagnostic yield was 55.6% in group A and 93.5% in group B (p<0.05). Procedure-related complications developed in seven group A patients but not in any group B patients. Of the seven complications, five were pneumothorax and two were vasovagal syncope.
Conclusion
Needle thoracoscopic pleural biopsy under local anesthesia is a simple and safe procedure that has a high diagnostic yield. This procedure is recommended as a useful diagnostic modality if prior thoracentesis is non-diagnostic.
Keywords: Biopsy; Pleural disease; Pleural effusion; Tumor, malignant; Video-assisted thoracic surgery (VATS)
INTRODUCTION
If thoracentesis is not diagnostic for a patient with pleural effusion, it is important to perform tissue diagnosis for ensuring adequate treatment. Currently, blind closed pleural biopsy is usually conducted for this purpose because the procedure is simple and can be performed readily under local anesthesia. However, the diagnostic yield of this procedure is low. A retrospective study of 414 patients with malignant pleural effusion revealed that closed pleural biopsies were of diagnostic utility in only 7.1% of the patients [1]. It is known that performing video-assisted thoracoscopic surgery (VATS) on pleural effusion increases the diagnostic yield, even when both thoracentesis and closed pleural biopsy (both conducted prior) are non-diagnostic [2,3]. In recent times, the diagnostic yield afforded by VATS in this context has approached 100% [4]. Thus, even as early as 1997, the American Thoracic Society recommended that thoracoscopy should be used for evaluating lung cancer prior to treatment if two prior cytological examinations of pleural effusion in patients with suspected malignancies have been negative [5]. Although conventional thoracoscopy using a tube having a diameter of 5 to 10 mm affords high diagnostic accuracy, patients are vulnerable to the risks associated with general anesthesia. Conventional thoracoscopy performed under local anesthesia is poorly accepted by patients because of the pain and discomfort associated with the passage of relatively large instruments through narrow intercostal spaces. However, the use of a 2-mm-diameter instrument in a technique called needle thoracoscopy reduces the procedure-related discomfort, trauma, and the torque exerted on narrow intercostal spaces upon the introduction of the instrument into the pleural cavity. To evaluate the utility of performing this procedure under local anesthesia for diagnosing pleural effusion, we prospectively compared its diagnostic yield with that of closed pleural biopsy.
METHODS
Sixty-seven patients underwent pleural biopsies over an 18-month period. The criterion for patient inclusion was that their pleural effusion remained undiagnosed after thoracentesis. Patients were randomized into two groups. Group A contained 36 patients with hydrothorax who underwent closed pleural biopsies. Group B contained 31 patients with hydrothorax who underwent pleural biopsies via needle thoracoscopy under local anesthesia. A pre-procedural workup included chest radiography, chest computed tomography (CT), thoracentesis for pleural fluid analysis, a bacteriological study, and cytological evaluation (Fig. 1). In group A patients, closed pleural biopsies were performed aseptically using Abrams biopsy needles after administering local anesthesia (via infiltration of 5 to 10 mL of 1% [w/v] lidocaine) at the bedside. Oxygen was provided continuously via a facial mask, and pulse oximetry, electrocardiogram (ECG), and blood pressure monitoring were conducted throughout the procedure. A pleural biopsy was considered adequate if at least three specimens containing pleural tissue were obtained. Chest radiography was performed immediately after each procedure for identifying any iatrogenic pneumothorax. Group B patients were subjected to video-assisted thoracoscopic pleural biopsy in a fully equipped operating room, under local anesthesia, and by using a thoracoscope and biopsy forceps, each having a diameter of 2 mm (Auto Suture, Norwalk, CT, USA), introduced via a trocar of the same diameter (Miniport; Auto Suture). Oxygen was provided continuously via a facial mask, and pulse oximetry, ECG, and blood pressure monitoring were conducted throughout the procedure. The procedure was usually performed with the patient in the lateral decubitus position, but the supine or semi-lateral decubitus positions were occasionally employed. Local anesthesia was administered via the infiltration of 1% (w/v) lidocaine (range, 10 to 15 mL) at the site of the thoracoscopic port's placement. The entry point was selected according to the location of the fluid and the biopsy site. A small skin incision was usually made along the anterior-to-mid-axillary line between the fourth and the seventh intercostal space. The 2-mm-diameter port was inserted through this incision, and the pleural fluid was aspirated. The needle thoracoscope was introduced through the same port. If the lung was over-inflated, CO2 was infused through a port having a diameter of 2 mm. A second skin incision was made, and a 2-mm-diameter port was inserted in it for carrying the small biopsy forceps. Biopsy was rather easy to perform because we could directly visualize the parietal and visceral pleura (Fig. 2). After biopsy, hemostasis was established, and a chest drain was placed through the 2-mm port.
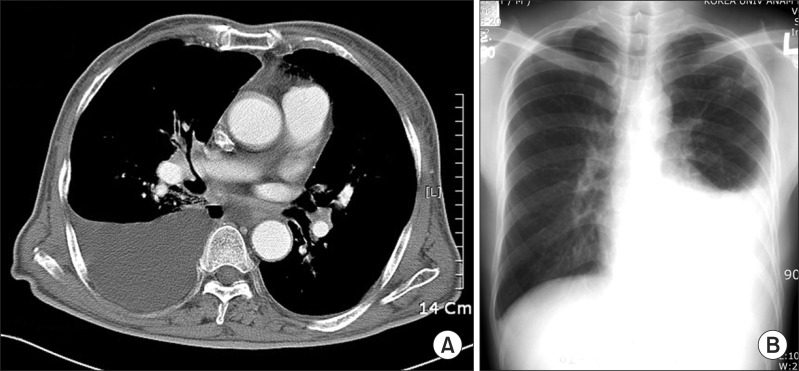
Fig. 1.
Radiological findings upon preprocedural evaluation. (A) Chest computed tomography of a 78-year-old male patient. A biopsy revealed the presence of metastatic squamous cell carcinoma. (B) A chest posterior-anterior view of a 27-year-old male patient. Tubercular pleurisy was diagnosed by biopsy.
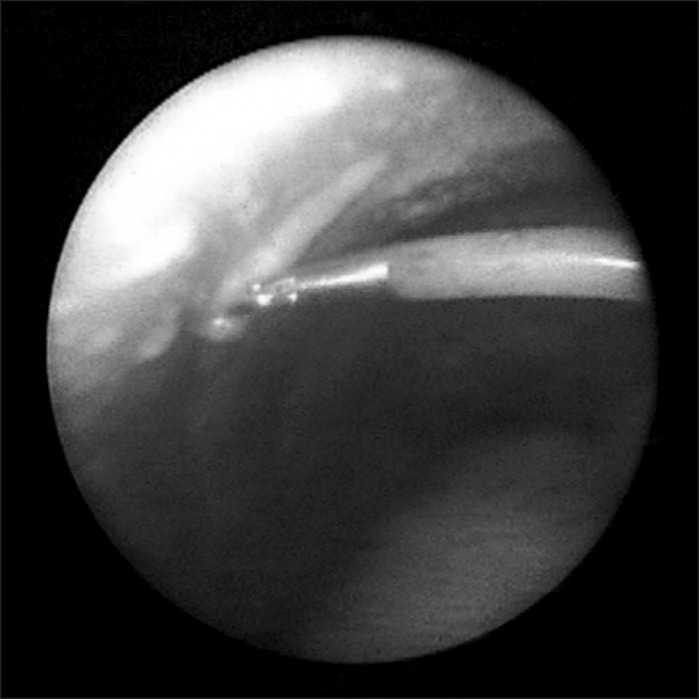
Fig. 2.
Gross finding of pleural nodules yielded by 2-mm-diameter needle thoracoscopy. The multiple yellowish lesions were diagnosed as metastatic adenocarcinoma.
SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. The independent samples t-test was employed to evaluate the significance of inter-group differences among continuous variables, all of which were expressed as mean±standard deviation. The chi-square test was used to evaluate the significance of differences in the non-continuous variables. A p-value<0.05 was considered to reflect statistical significance.
RESULTS
Sixty-seven procedures were performed over a period of 18 months; these were associated with a low level of morbidity in group A patients (only) and no mortality in either group. The mean patient age and gender distribution did not differ between the two groups. In group A, closed pleural biopsy was diagnostic in 20 of the 36 patients (diagnostic yield, 55.6%) (Table 1). Sixteen of these patients were diagnosed with tuberculosis, and four with malignancy. Nine patients had non-specific conditions, and inadequate tissue samples were obtained from seven. Procedure-related complications developed in seven patients (19.5%), all of whom were managed appropriately. Two patients developed vasovagal syncope, which was managed conservatively; the procedures were completed at a later date. Five patients developed pneumothorax. Three of these patients required closed thoracostomy for the treatment of problematic symptoms, whereas the two other patients were managed conservatively by administering oxygen. In group B, needle thoracoscopic pleural biopsy was diagnostic in 29 of the 31 patients (diagnostic yield, 93.5%) (Table 1). The diagnosis was tuberculosis in 17 patients, malignancy in 12, and non-specific in 2. Adequate tissue samples were obtained in all cases. No procedure-related morbidity occurred. Of the 31 patients, we placed chest drains in 25 at the end of the procedure, but these were removed from most patients by the end of the second post-operative day (mean time to removal, 1.9±1.1 days).
Table 1.
Patient profiles and summary of the results
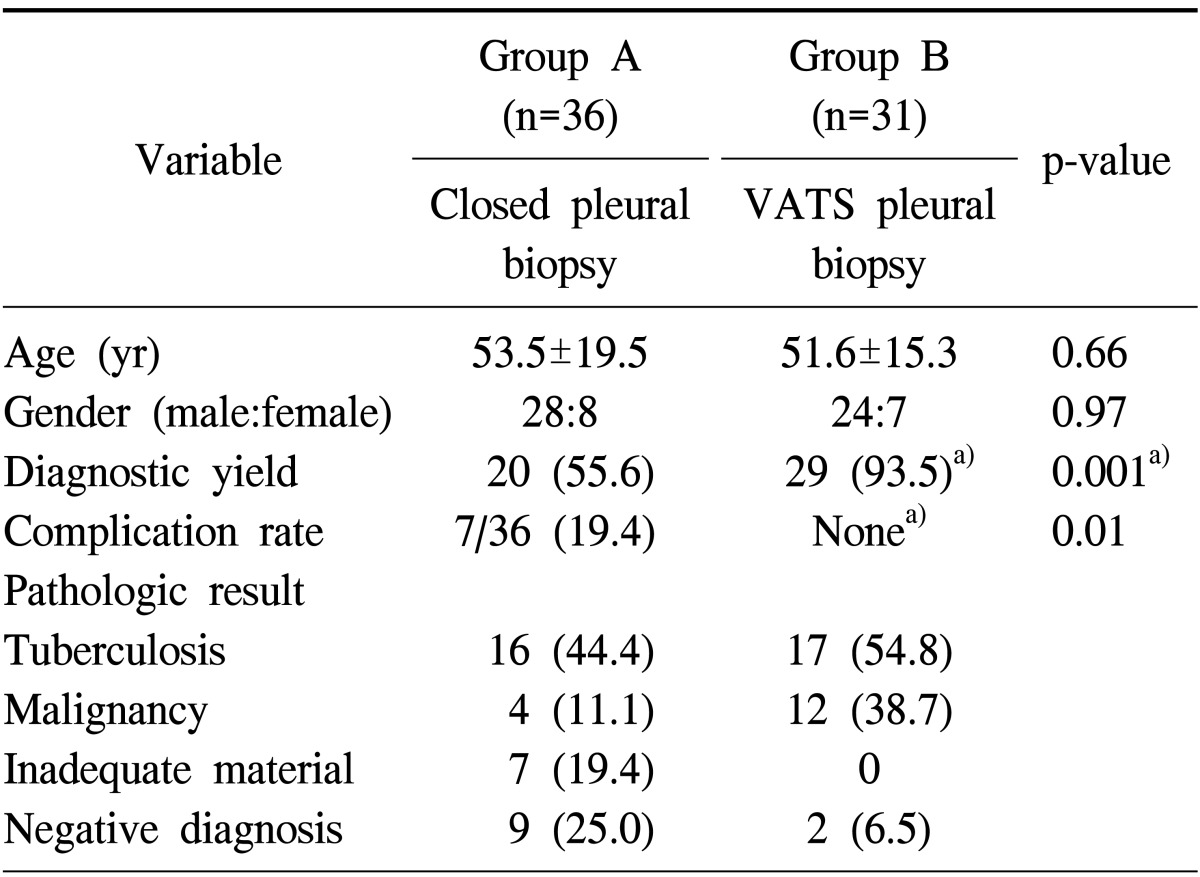
Values are presented as mean±standard deviation or number (%).
VATS, video-assisted thoracoscopic surgery.
a)p-value<0.05.
DISCUSSION
Adequate treatment of patients with pleural effusion not diagnosed via prior thoracentesis requires the use of a tool that yields accurate diagnosis. Usually, to this end, a blind closed pleural biopsy is performed. However, this technique is associated with a low and variable diagnostic yield (range, 29% to 70%) [2,6,7]. Prakash et al. reported that closed pleural biopsy failed to yield adequate tissue samples from 13.3% of the patients, thus explaining the low diagnostic yield in our group A patients [1]. Although the technique is simple and easy to perform, the associated low diagnostic yield is problematic. Thus, the technique is being gradually superseded by imaging modalities, including video-assisted and medical thoracoscopy, ultrasound, and CT guidance [8,9]. Thoracoscopic or image-guided pleural biopsy is superior to blind pleural biopsy when used for exploring patients with suspected malignant pleural effusion, and closed pleural biopsy is diminishing in popularity [4,8,9]. However, this technique continues to be used when other facilities are not available. Furthermore, closed pleural biopsy is simple, can be performed even by inexperienced clinicians, and costs less than thoracoscopy [10,11].
The diagnostic accuracy of VATS, a procedure for diagnosing pleural effusion, approaches 100%. This is true even when prior thoracentesis and closed pleural biopsy have failed in diagnostic terms [2,3,12,13,14,15,16]. Although conventional thoracoscopy conducted using a 5- to 10-mm-diameter instrument under general anesthesia affords high diagnostic accuracy, the patient must assume the risks associated with general anesthesia and a high medical cost. Thus, we hypothesized that needle thoracoscopic pleural biopsy performed under local anesthesia would be valuable. Conventional thoracoscopy performed under local anesthesia is poorly accepted by patients because of the pain and discomfort caused by the passage of relatively large instruments through narrow intercostal spaces. However, needle thoracoscopy is not associated with such problems. In addition, the latter technique affords increased angular movement, reduction in the torque applied to narrow intercostal spaces upon tube insertion into the pleural cavity, and better cosmetic effect (small incision). It is vital to minimize patient discomfort when thoracoscopy is performed under local anesthesia. If a patient tolerates pain poorly or a relatively large specimen is required, 1% [w/v] lidocaine may be injected locally into the parietal pleura of the biopsy site using a spinal needle. Then, an adequate biopsy sample can be obtained easily.
The diameter of the visualizing instrument is critical in terms of the image quality obtained during surgery. In general, instruments having smaller diameters are considered inferior. Janssen et al. [17] reported that a 7-mm-diameter thoracoscopy set afforded image quality superior to that of 3.5- and 2.0-mm-diameter sets. However, the histopathological diagnostic yield was maximal when 3.5- and 5-mm-diameter biopsy forceps were used and suboptimal when 2-mm-diameter forceps were employed. When using a modern instrument, we did not experience any problem with image quality and achieved a high diagnostic yield (93.5%) with video-assisted thoracoscopy performed using a 2-mm-diameter biopsy forceps.
Recently, it has become clear that more invasive and sophisticated investigation of pleural effusions is required because the etiology of such effusions remains unknown in 20% to 40% of the cases [18]. In such situations, performing needle thoracoscopic pleural biopsy under local anesthesia yields valuable information. Furthermore, the procedure is simple and safe, and exhibits high diagnostic accuracy. Thus, useful data are delivered to both the patient and the referring physician. However, a number of patients continue to be vaguely diagnosed with 'idiopathic pleural effusion' even after complete workup, and several studies have found that 5% to 15% of such patients develop malignant effusions on long-term follow-up [18,19,20]. Physicians must be aware of this and exercise great caution when following up with such patients.
In conclusion, the use of needle thoracoscopy under local anesthesia for obtaining pleural biopsy samples is simple and safe, and exhibits high diagnostic accuracy without the risks and high costs associated with the use of general anesthesia. This technique is a valuable diagnostic tool when a patient with a pleural effusion has not been adequately diagnosed via thoracentesis.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Prakash UB, Reiman HM. Comparison of needle biopsy with cytologic analysis for the evaluation of pleural effusion: analysis of 414 cases. Mayo Clin Proc. 1985;60:158–164. doi: 10.1016/s0025-6196(12)60212-2. [DOI] [PubMed] [Google Scholar]
- 2.Harris RJ, Kavuru MS, Mehta AC, et al. The impact of thoracoscopy on the management of pleural disease. Chest. 1995;107:845–852. doi: 10.1378/chest.107.3.845. [DOI] [PubMed] [Google Scholar]
- 3.Loddenkemper R. Thoracoscopy: results in non cancerous and idiopathic pleural effusions. Poumon Coeur. 1981;37:261–264. [PubMed] [Google Scholar]
- 4.Silvestri GA, Strange C. Rest in peace: the decline in training and use of the closed pleural biopsy. J Bronchology. 2005;12:131–132. [Google Scholar]
- 5.The American Thoracic Society and the European Respiratory Society. Pretreatment evaluation of non-small-cell lung cancer. Am J Respir Crit Care Med. 1997;156:320–332. doi: 10.1164/ajrccm.156.1.ats156.1. [DOI] [PubMed] [Google Scholar]
- 6.Nusair S, Breuer R, Amir G, Berkman N. Closed pleural needle biopsy: predicting diagnostic yield by examining pleural fluid parameters. Respir Med. 2002;96:890–894. doi: 10.1053/rmed.2002.1379. [DOI] [PubMed] [Google Scholar]
- 7.Frank W. Current diagnostic approach to pleural effusion. Pneumologie. 2004;58:777–790. doi: 10.1055/s-2004-830084. [DOI] [PubMed] [Google Scholar]
- 8.Ahrar K, Wallace M, Javadi S, Gupta S. Mediastinal, hilar, and pleural image-guided biopsy: current practice and techniques. Semin Respir Crit Care Med. 2008;29:350–360. doi: 10.1055/s-2008-1081279. [DOI] [PubMed] [Google Scholar]
- 9.Rahman NM, Gleeson FV. Image-guided pleural biopsy. Curr Opin Pulm Med. 2008;14:331–336. doi: 10.1097/MCP.0b013e3282fe9a04. [DOI] [PubMed] [Google Scholar]
- 10.Chakrabarti B, Ryland I, Sheard J, Warburton CJ, Earis JE. The role of Abrams percutaneous pleural biopsy in the investigation of exudative pleural effusions. Chest. 2006;129:1549–1555. doi: 10.1378/chest.129.6.1549. [DOI] [PubMed] [Google Scholar]
- 11.Baumann MH. Closed pleural biopsy: not dead yet! Chest. 2006;129:1398–1400. doi: 10.1378/chest.129.6.1398. [DOI] [PubMed] [Google Scholar]
- 12.Greillier L, Cavailles A, Fraticelli A, et al. Accuracy of pleural biopsy using thoracoscopy for the diagnosis of histologic subtype in patients with malignant pleural mesothelioma. Cancer. 2007;110:2248–2252. doi: 10.1002/cncr.23034. [DOI] [PubMed] [Google Scholar]
- 13.Canto A, Blasco E, Casillas M, et al. Thoracoscopy in the diagnosis of pleural effusion. Thorax. 1977;32:550–554. doi: 10.1136/thx.32.5.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Camp PT, Moseley PW, Scott ML, Hatch HB., Jr Diagnostic thoracoscopy. Ann Thorac Surg. 1973;16:79–84. doi: 10.1016/s0003-4975(10)65814-6. [DOI] [PubMed] [Google Scholar]
- 15.Page RD, Jeffrey RR, Donnelly RJ. Thoracoscopy: a review of 121 consecutive surgical procedures. Ann Thorac Surg. 1989;48:66–68. doi: 10.1016/0003-4975(89)90179-3. [DOI] [PubMed] [Google Scholar]
- 16.Petrakis I, Katsamouris A, Drossitis I, Chalkiadakis G. Video-assisted thoracoscopic surgery in the diagnosis and treatment of chest diseases. Surg Laparosc Endosc Percutan Tech. 1999;9:409–413. [PubMed] [Google Scholar]
- 17.Janssen JP, Thunnissen F, Visser F. Comparison of the 2.0 mm and the 3.5 mm minithoracoscopy set to standard equipment for medical thoracoscopy. Eur Respir J. 2003;22(suppl 45):S451. [Google Scholar]
- 18.Ferrer JS, Munoz XG, Orriols RM, Light RW, Morell FB. Evolution of idiopathic pleural effusion: a prospective, long-term follow-up study. Chest. 1996;109:1508–1513. doi: 10.1378/chest.109.6.1508. [DOI] [PubMed] [Google Scholar]
- 19.Janssen JP, Ramlal S, Mravunac M. The long-term follow-up of exudative pleural effusion after nondiagnostic thoracoscopy. J Bronchol. 2004;11:169–174. [Google Scholar]
- 20.Venekamp LN, Velkeniers B, Noppen M. Does 'idiopathic pleuritis' exist? Natural history of non-specific pleuritis diagnosed after thoracoscopy. Respiration. 2005;72:74–78. doi: 10.1159/000083404. [DOI] [PubMed] [Google Scholar]