Clinical Question
How can carpal tunnel syndrome be diagnosed and managed in a primary care setting?
INTRODUCTION
Carpal tunnel syndrome (CTS) is a symptomatic compression neuropathy of the median nerve at the level of the wrist; characterised by hand pain, numbness, and tingling in the distribution of the median nerve (thumb, index, middle finger, and the radial side of the ring finger) and a reduction in grip strength and hand function. The severity of symptoms can be clinically categorised into mild, moderate, and severe. A figure of 55–65% of CTS cases present bilaterally1 and the condition can be associated with conditions such as hypothyroidism, diabetes, and rheumatoid arthritis. CTS may present in late pregnancy but is usually transient.
A study from the UK General Practice Research Database in 2000, calculated the incidence in males to be 88 per 100 000 and in females to be 193 per 100 000, with new presentations being most frequent at ages 45–54 years in females and 75–84 years in males.2 CTS is a recognised work-related musculoskeletal disorder (WMSD) caused by strain and repeated movements (biomechanical overload) and is hence more common in manual workers. Work absence and associated healthcare costs contribute to a significant socioeconomic burden on the UK economy.3
Consultations and surgical referrals appear to be increasing and commissioners are engaged in the review of referral protocols, incorporating conservative treatments for mild-to-moderate disease, to help manage surgical demand.
ASSESSMENT
A clear history and targeted examination, which identifies standard features and provocative factors, increases the likelihood of a diagnosis.4
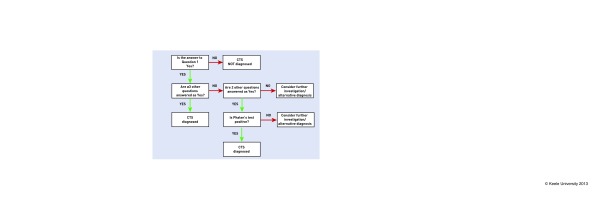
Diagnosis can be achieved by use of criteria agreed by GPs with a special interest in musculoskeletal health, from the Primary Care Rheumatology Society. The criteria comprise eight questions (Box 1) followed by a decision tree (Figure 1).5
Box 1. Questions to be asked to a patient presenting with hand or wrist symptoms
Do you have numbness or tingling in your wrist, hand, or fingers?
Do your symptoms spare your little finger?
Are the symptoms worse at night?
Do the symptoms wake you up at night?
Have you noticed your hand is weak; for example, have you found yourself dropping things?
Do you find shaking your hand, holding your hand or running it under warm water improves your symptoms?
Are the symptoms made worse by activities such as driving, holding a telephone, using vibrating tools, or typing?
Have splints or injections helped with your pain if you have had it in the past?
Figure 1.
Decision tree to be used in conjunction with the questions in Box 1. © Keele University.
Alternative diagnoses that should be considered include: cervical radiculopathy, peripheral neuropathy, wrist/trapeziometacarpal, arthrosis, wrist tendonitis/tenosynovitis and ulnar neuropathy.4 Contributing factors such as diabetes, hypothyroidism, and inflammatory conditions should be considered and managed appropriately, although there is no evidence that routine screening should be undertaken.6
Electromyography and nerve conduction studies may be considered if the diagnosis is uncertain, if surgery is being considered, or in the case of litigation;4,6,7 although care pathways and local availability may vary.
MANAGEMENT
CTS may improve spontaneously in up to one-third of patients over a 10–15 month period.8 Treatment options depend on severity. Non-surgical management (splinting or injection) should be considered in cases of mild to moderate disease, whereby pain and numbness are intermittent and there is no wasting or weakness of the thenar muscles. Referral for surgical management (decompression of the carpal tunnel) should be considered if: symptoms are severe or constant, the motor or sensory deficit is progressive, or there is no improvement within 3 months of conservative treatment.6
The use of non-steroidal anti-inflammatory drugs or diuretics should not be routinely recommended. Patients should be advised to minimise activities that exacerbate symptoms but it should be explained that evidence for work place modifications is lacking.6
Night splinting holds the wrist in a near neutral position preventing wrist flexion and limiting extension. Splints are inexpensive with no reported serious adverse effects7 and, although there is limited evidence as to their effectiveness,9 are recommended as a treatment option in primary care with the proviso that benefits should be apparent within 8 weeks.6
Corticosteroid injections are considered a safe and effective treatment option in the management of CTS and are believed to act by decreasing the symptomatic swelling of the flexor synovialis.
Cochrane review evidence exists for the short-term improvement of symptoms following an injection, while longer-term effects beyond 3 months are uncertain.10 An accepted method for injection is shown in Figure 2; appropriate training is necessary.
Figure 2.
- Equipment: chlorhexidine wipe; 1 ml syringe, 23 gauge (blue) or 25 gauge (orange) needle for injection; corticosteroid without lidocaine; simple dressing.
- Explain and consent the patient for the treatment. Ensure there are no contraindications to a local steroid injection.
- Use a sterile ‘no-touch’ technique.
- The patient places hand palm up in a neutral or slightly extended wrist position (patient sitting).
- Clean skin following standard local practice.
- Insert needle at proximal skin crease at wrist, avoiding median nerve which lies under palmaris longus.
- Aspirate back into the syringe to avoid intravascular injection.
- Inject. Do not inject against resistance or if severe pain: if this occurs, reposition the needle and inject again.
- Ensure haemostasis and apply dressing.
- Provide patient with leaflet regarding the carpal tunnel steroid injection.
- The patient should be advised to wait in the surgery for 30 minutes following injection or alternatively ensure that they are accompanied by a responsible adult for that time.
CONCLUSION
CTS is a common, disabling, and distressing condition. Wrist splinting and corticosteroid injections are non-surgical treatment options that can be considered in primary care for the management of mild-to-moderate disease.
Patients with severe symptoms or who fail to respond to non-surgical management should be referred for surgical consideration.
Funding
Claire Burton is funded by a National Institute for Health Research (NIHR) In-Practice Fellowship (IPF 07/002). Components of this report are from independent research arising from this In Practice Fellowship supported by the NIHR. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests
Discuss this article
Contribute and read comments about this article: www.bjgp.org/letters
REFERENCES
- 1.Bland JDP, Rudolfer SM. Clinical surveillance of carpal tunnel syndrome in two areas of the United Kingdom, 1991–2001. J Neurol Neurosurg Psychiatry. 2003;74(12):1674–1679. doi: 10.1136/jnnp.74.12.1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Latinovic R, Gulliford MC, Hughes RA. Incidence of common compressive neuropathies in primary care. J Neurol Neurosurg Psychiatry. 2006;77(2):263–265. doi: 10.1136/jnnp.2005.066696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ibrahim I, Khan WS, Goddard N, Smitham P. Carpal tunnel syndrome: a review of the recent literature. Open Orthop J. 2012;6:69–76. doi: 10.2174/1874325001206010069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Academy of Orthopaedic Surgeons Clinical practice guideline on the diagnosis of carpal tunnel syndrome. 2007 doi: 10.2106/JBJS.I.00643. http://www.aaos.org/Research/guidelines/CTS_guideline.pdf (accessed 11 Apr 2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burton C, Chesterton L, Davenport G, et al. Developing agreed clinical criteria for the diagnosis of carpal tunnel syndrome in primary care — a clinical consensus exercise. Society of Academic Primary Care Annual Conference; 4 July 2013; Nottingham. p. 2E.2. [Google Scholar]
- 6.National Institute for Health and Care Excellence Carpal tunnel syndrome. 2012 NIHR, http://cks.nice.org.uk/carpal-tunnel-syndrome#!scenariorecommendation:1 (accessed 10 Apr 2014). [Google Scholar]
- 7.Bland JD. Carpal tunnel syndrome. BMJ. 2007;335(7615):343–346. doi: 10.1136/bmj.39282.623553.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Padua L, Aprile I, Caliandro P, et al. Carpal tunnel syndrome in pregnancy: multiperspective follow-up of untreated cases. Neurology. 2002;59(10):1643–1646. doi: 10.1212/01.wnl.0000034764.80136.ef. [DOI] [PubMed] [Google Scholar]
- 9.Page MJ, Massy-Westropp N, O’Connor D, Pitt V. Splinting for carpal tunnel syndrome. Cochrane Database Syst Rev. 2012;7:CD010003. doi: 10.1002/14651858.CD010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marshall SC, Tardif G, Ashworth NL. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;2:CD001554. doi: 10.1002/14651858.CD001554.pub2. [DOI] [PubMed] [Google Scholar]