Summary
We sought to assess neurologists' interest in sports neurology and learn about their experience in treating sports-related neurologic conditions. A survey was sent to a random sample of American Academy of Neurology members. A majority of members (77%) see at least some patients with sports-related neurologic issues. Concussion is the most common sports-related condition neurologists treat. More than half of survey participants (63%) did not receive any formal or informal training in sports neurology. At least two-thirds of respondents think it is very important to address the following issues: developing evidence-based return-to-play guidelines, identifying risk factors for long-term cognitive-behavioral sequelae, and developing objective diagnostic criteria for concussion. Our findings provide an up-to-date view of the subspecialty of sports neurology and identify areas for future research.
Sports neurology is the subspecialty of neurology concerned with the study and management of sports-related neurologic injuries that may develop as a result of participation in athletic activities. Concussion is the most recognized example of a sport-related injury. However, athletes also experience injuries to the spine (spinal cord), peripheral nerves, and the neuromuscular system, and rarely, traumatic brain injuries of greater severity. Sports neurology also deals with the safe participation in sports and athletics by patients with neurologic conditions, such as epilepsy, multiple sclerosis, and migraine. Also important is a richer understanding of the neurologic benefit that occurs as a result of exercise and participation in sports, which may augment normal neurologic function and forestall the progression of neurodegenerative disorders.
The field has likely been around since ancient Greek and Roman times. Modern sports neurology dates back to 1768, with the publication by Percivall Pott1 on sports-related head trauma. During the last 3 decades, however, there has been a consolidated movement to develop the discipline of sports neurology. The 1989 publication of Sports Neurology by Jordan et al.2 led to a much more public and academic recognition of this discipline. However, only recently have neurologists become more active participants in diagnosing and managing neurologic injuries in sport. Sports neurology is the fastest growing subspecialty of neurology and a major focus of the American Academy of Neurology (AAN). In 2010, the AAN formed the Sports Neurology Section, which as of April 2013 had 512 members. One of the initial goals of the Section's strategic plan was to assess neurologists' interest in sports neurology and learn about their involvement and experience in treating sports-related neurologic conditions. To address these goals, the Section collected data from AAN members via a survey. This information could be used to develop educational programs and core curriculum for residency programs, serve as a guide for future research, and assess the need and interest in the development of sports neurology fellowship programs.
METHODS
The survey instrument was designed by representatives of the AAN Sports Neurology Section in the spring of 2012. The AAN Member Research Subcommittee reviewed the survey draft in May 2012 and provided suggestions for improvement. The final instrument included questions on current topics in sports neurology, members' training, types of sports-related neurologic issues seen in practice, and opinions on future education options in sports neurology topics. The full survey instrument is available as appendix e-1.
A random sample of 900 AAN members residing in the United States was selected for the survey. The sample included practicing neurologists, residents, and fellowship trainees. The survey was first sent to the entire sample on June 27, 2012. Participants received an e-mail with a link to the online version of the survey and a paper survey that was sent via mail or fax. A letter signed by the Sports Neurology Section Chair introduced the survey. Reminders to participate were sent to nonrespondents on July 18 and July 31; each time, paper and online versions of the survey were resent to members. Data collection was closed on August 17, 2012. During data collection, 20 members were removed from the sample due to invalid contact information, which resulted in the final sample size of 880.
The results were analyzed using descriptive statistical measures. For determination of significance, t test or χ2 tests were used as appropriate; p values less than 0.05 were considered significant.
RESULTS
Response rate
A response rate of 28.1% (247/880) was achieved for the survey. The margin of error for all respondents at a 95% confidence level was ±6.2%. There were no significant differences between survey respondents and nonrespondents on age (p = 0.17), sex (p = 0.49), or AAN membership type (p = 0.33).
Practice and experience
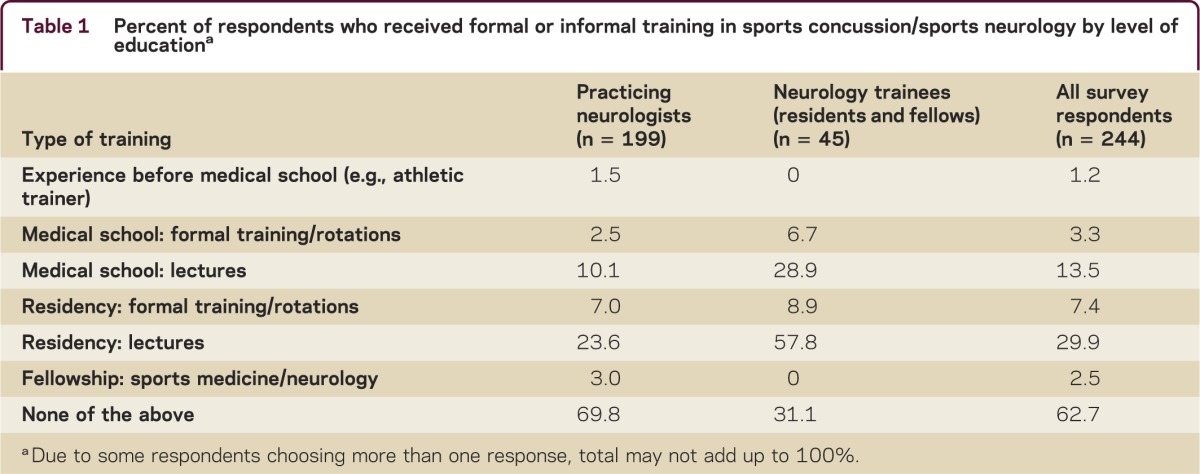
Several survey questions asked about respondents' level of training and exposure to the field of sports neurology. Table 1 shows that more than half of all survey participants (63%) did not receive any formal or informal training in sports neurology. There were differences in responses based on members' level of training, with at least twice as many neurology trainees having formal training/rotations in medical school, lectures in medical school, and lectures in residency.
Table 1.
Percent of respondents who received formal or informal training in sports concussion/sports neurology by level of educationa
An overwhelming majority of members (77%) see at least some patients with sports-related neurologic issues, but for most of them the percent of all patients with these conditions is fairly small, between 1% and 10%. On average, the following conditions represent all the sports-related neurologic issues neurologists see in their practice: sports concussion (51%), preexisting neurologic conditions requesting permission to participate in sports (17%), peripheral nerve injuries (16%), spine injuries (11%), and other issues (5%).
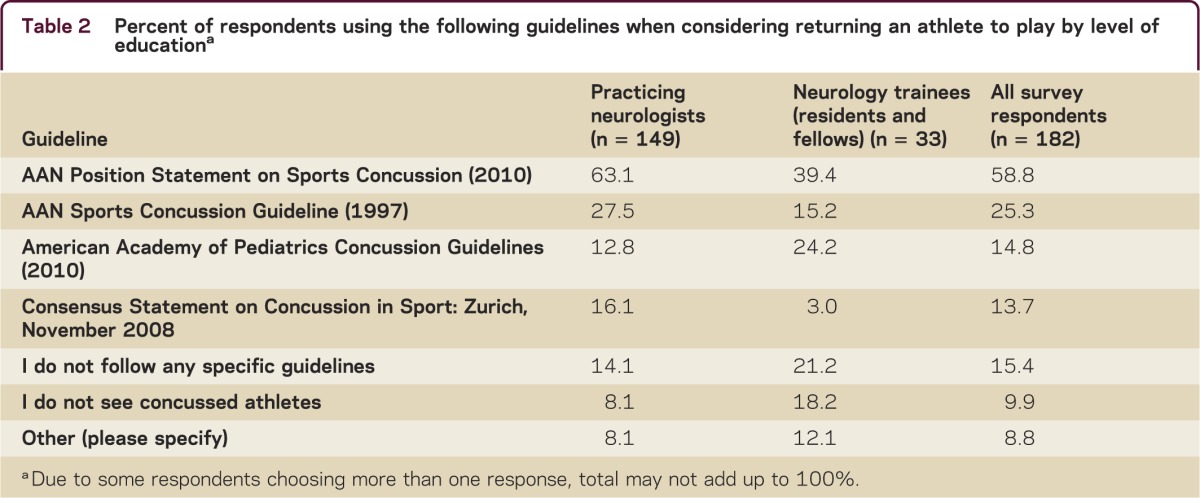
Table 2 shows which guidelines are used when considering returning an athlete to play. Among all respondents, the 2010 AAN Position Statement on Sports Concussion is the guideline that is used the most. There were differences in guideline use by level of education: more practicing neurologists rely on AAN guidelines compared to residents and fellows, and more neurology trainees use the 2010 American Academy of Pediatrics Concussion Guidelines or no guidelines at all.
Table 2.
Percent of respondents using the following guidelines when considering returning an athlete to play by level of educationa
Overall, survey respondents rely on the following sources to stay current with sports-related neurologic issues: medical journals (75%), Web-based sources (42%), lectures/workshops at AAN meetings (30%), lectures/workshops at other meetings (16%), and other sources (9%). Neurologists used more lectures/workshops at AAN meetings compared to residents/fellows (33% vs 15%) and lectures/workshops at other meetings (19% vs 0%). Neurology trainees had a slight preference for using Web-based resources compared to practicing neurologists (46% vs 41%).
Very few survey respondents (4%) are formally affiliated with a sports team. The most common level of affiliation is college, with 86% of neurologists who have a formal sports team appointment reporting this level of affiliation.
Current issues in sports neurology
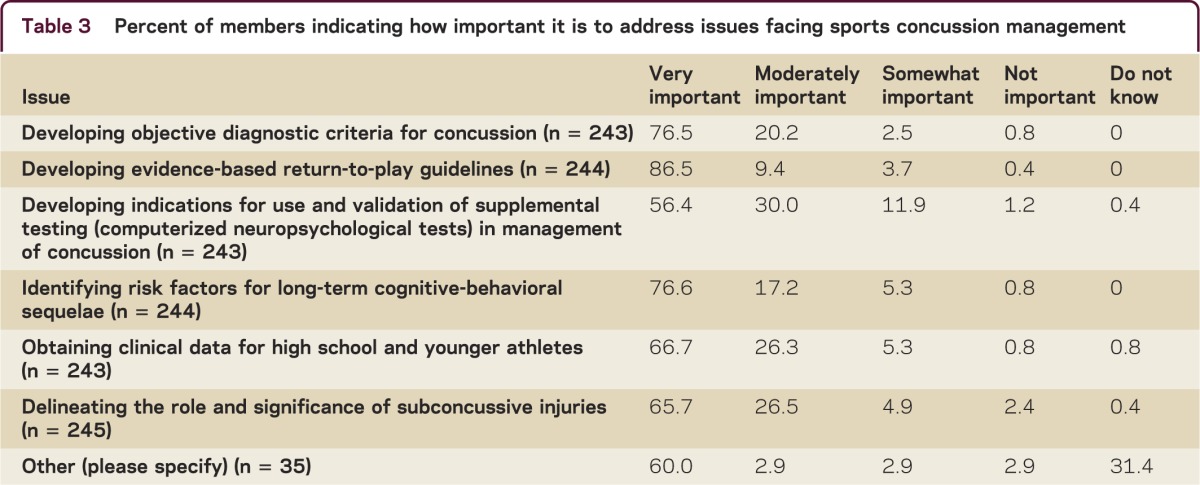
Table 3 shows member ratings of importance to address various issues currently facing sports concussion management. At least two-thirds of survey participants think it is very important to address the following issues: developing evidence-based return-to-play guidelines (87%), identifying risk factors for long-term cognitive-behavioral sequelae (77%), and developing objective diagnostic criteria for concussion (77%).
Table 3.
Percent of members indicating how important it is to address issues facing sports concussion management
While the majority (68%) of members endorsed neurologists as the specialist they think best qualified to manage sports concussion, other health care providers were also recognized, including primary care physicians, neuropsychologists, physiatrists, neurosurgeons, athletic trainers, and other specialists.
When asked what their current practice is (or would be their choice) if an athlete is suspected of having sustained a concussion, 84% indicated that an athlete should not be allowed back in the game, 8% suggested an athlete can return to play if symptoms clear within 15 minutes, 7% were not sure, and 1% indicated an athlete should be allowed back in the game.
Prior to receiving the survey, fewer than half of all survey respondents (43%) were aware that the AAN had a Sports Neurology Section. Practicing neurologists were more likely to have knowledge of the Section compared to neurology trainees (47% vs 29%, p = 0.03).
Future education on sports neurology
The majority of survey respondents (85%) would like to see more sports neurology–related educational programs offered by the AAN. The 3 topics they would most be interested in are as follows: 1) sports concussions, 2) evaluation of the patient with preexisting neurologic conditions who desires to participate in sports, and 3) spine injuries. The majority of members (80%) are also interested in CME courses on sports concussion and sports-related neurologic issues. The preferred formats of CME courses are Web-based courses (79%), AAN annual meeting (47%), and AAN-sponsored events separate from the AAN meeting, such as the fall conference (29%).
DISCUSSION
This study is the first comprehensive effort to assess neurologists' interest in sports neurology and learn about their involvement and experience in treating sports-related neurologic conditions.
More than three-quarters of neurologists see patients with sports-related neurologic issues, with concussion being the most prevalent. Despite this, more than half of all neurologists have no formal training in the diagnosis and management of sports-related concussion. This is reminiscent of the Kaye et al.3 study, where 89% of pediatricians believed they were the appropriate provider for mild traumatic brain injury (mTBI) follow-up, but 60% indicated they had not participated in any CME related to mTBI. The study helped identify several key issues in sports neurology, including developing evidence-based return-to-play guidelines, identifying risk factors for long-term cognitive-behavioral sequelae, and developing objective diagnostic criteria for concussion.
At the time of the survey, the latest published guideline on sports concussion was from 1997. In order to update this guideline, a position statement on sports concussion was developed by the AAN in 2010, recommending immediate removal of any athlete from sports participation if he or she is suspected of having sustained a concussion. It is encouraging that 84% of neurologists who participated in the survey indicated they will follow this recommendation if they are faced with a decision to give permission to participate in the game when concussion is suspected. However, the remaining 16% were either not sure of what the appropriate action should be or indicated they would allow an athlete to continue participating in the game. This indicates an opportunity to educate neurologists and other medical professionals on the latest guidelines in sports concussion management. On March 18, 2013, the AAN issued a new evidence-based guideline on sports concussion management.4 This is the first sports concussion guideline constructed using formal evidence-based medicine methodology to minimize bias and objectively arrive at management recommendations. The new guideline replaces the 1997 AAN guideline, reviews all the literature from 1950 to June 2012, and was developed using a multidisciplinary committee. It is our hope that all physicians and other medical professionals use these guidelines as the basis for sports concussion evaluation and management.
Among neurologists who are still in training, there are more respondents who reported receiving sports neurology rotations and lectures, which is a positive sign, suggesting that medical schools and residency programs are adapting their curriculum to address current issues and patient needs. With regard to those neurologists who did not undergo any type of specialized sports neurology training, their general education in neurology still gives them a strong foundation to treat patients involved in sports. Most if not all concussion symptoms are neurologic in nature. Headache, for example, is the most common symptom of concussion, and neurologists have a long tradition of treating this condition.
This survey also uncovered that very few neurologists are currently formally affiliated with a sports team. This is another opportunity where neurologists' knowledge and training could be utilized to a greater extent. Recently, professional football players through the National Football League Players Association (NFLPA) have demanded that physicians with special qualifications in concussion be present on the sidelines of every game. The National Football League (NFL) appears to be moving in that direction this season. Since it appears that few neurologists understand how they can get involved with a sports team, the AAN could facilitate educational opportunities in this area, perhaps in the form of courses on sideline management or establishing a formal collaboration with the NFL. We hope that more neurologists will be involved at all levels of team affiliation, including professional, collegiate, and amateur.
The study has several limitations. As with any survey project, our findings can be subject to self-reporting and selection bias. The response rate of 28% was not as high as desired, but was still within the range of other similar surveys conducted by the AAN. Because survey respondents did not differ from nonparticipants on major demographic variables, there is no evidence of response bias, but it is possible that survey participants could be different from the general population of neurologists on other characteristics that were not directly assessed.
The AAN Sports Neurology Section has seen tremendous growth since its establishment in 2010 with just a handful of members. The Section grew to 310 members in 2011 and had 512 members in April 2013. Given the young age of the Sports Neurology Section, it was not surprising that more than half of AAN members were not aware of its existence at the time of the survey. There is a great need for and interest in the issues of sports neurology, demonstrated by the fact that a majority of survey participants indicated that they would like to see more sports neurology–related educational programs offered by the AAN. The AAN and the Sports Neurology Section could provide several opportunities for involvement, including educational programs (e.g., sideline management, sports concussion), dissemination of the AAN's new guideline on sports management, and suggestions for collaborations with other specialties involved in treating athletes.
CONCLUSION
The field of sports neurology is in great demand and has a bright future. Neurologists' training positions them well to be at the forefront of patient care and research. Many neurologists are interested in learning more about sports neurology. While neurologists are not the only specialists who are qualified to take care of concussion and other sports management issues, they should continue to be at the forefront of new developments in the field of sports neurology and actively participate in recommending best practices. In addition, they should strive to establish prevention and treatment protocols that call for collaboration with other specialists. Similar to some neurologic diseases, such as stroke, where neurologists collaborate with other medical specialists to provide care, there is an opportunity for neurologists interested in treating athletes to work in unison with other specialties in order to ensure better patient outcomes. Such arrangements could include primary care physicians, pediatricians, physical medicine and sports medicine specialists, orthopedic surgeons, neurosurgeons, athletic trainers, neuropsychologists, allied health specialists, and school administrators.
Supplementary Material
Footnotes
Supplemental Data: Neurology.org/cp
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
F. Conidi is the team neurologist for the National Hockey League Florida Panthers; served as a neurology consultant to the New York Mets; is Co-Chair of the Florida High School Athlete Association Concussion Committee; is a member of the Food and Drug Administration (FDA) Diagnostic and Radiological Device Committee for Concussion in Sport; is Founder and Chair of the Seeing Stars Foundation for research and education on concussion in sport; has received research funding from Allergan and NINDS; has served on a Scientific Advisory Board and speakers' bureau for and received travel and speaker honoraria from Allergan; has received speaker honoraria from the American Headache Society; and has acted as a witness or consultant or has prepared an affidavit for 8–10 legal cases per year. O. Drogan was a salaried employee of the American Academy of Neurology. C. Giza serves on the data safety monitoring board for LA Biomed Institute at Harbor-UCLA Medical Center; has received funding for travel to attend meetings from the Major League Soccer Concussion Program Committee, California State Athletic Commission, and NCAA; is a commissioner on the California State Athletic Commission; serves as a consultant for the National Hockey League Players' Association (NHLPA) and a subcommittee chair for the Centers for Disease Control and Prevention (CDC) Pediatric Mild Traumatic Brain Injury Guideline Workgroup; serves on the steering committee for the Sarah Jane Brain Project, the Concussion Program Committee for Major League Soccer, the Advisory Board for the American Association for Multi-Sensory Environments (AAMSE), and the NCAA Concussion Task Force; serves on the Medical Education Speakers Network; has received funding for travel and speaker honoraria for invited lectures on traumatic brain injury (TBI)/concussion; has received publishing royalties for Neurological Differential Diagnosis: A Prioritized Approach (Blackwell Publishing, 2005–present); has received research support from the National Institute of Neurological Disorders and Stroke (NINDS)/NIH, University of California, Department of Defense (DOD), NFL Charities, Thrasher Research Foundation, Today's and Tomorrow's Children Fund, Richie's Fund, Joseph Drown Foundation, NCAA, and the Child Neurology Foundation/Winokur Family Foundation; and has given (and continues to give) expert testimony, has acted as a witness or consultant, or has prepared an affidavit for 2–4 legal cases per year. J. Kutcher has received travel and speaker honoraria from the University of Toronto; is the Director of the National Basketball Association Concussion Program, Team Physician for the United States Ski and Snowboard Association, consultant to the National Football League Players Association (NFLPA) and the National Hockey League Players' Association (NHLPA), and a member of the NCAA Concussion Task Force; and receives research support from ElMindA, Ltd. A. Alessi is a consultant for the National Football League Players Association (NFLPA) and CBS Radio. K. Crutchfield is the Independent Neurological Consultant to the Baltimore Ravens, serves as neurology consultant to Baltimore Orioles, DC United Soccer, Chesapeake Bayhawks Lacrosse, and Washington Divas Football, and is Director of the Return to Play Committee for NFLPA Mackey-White TBI Committee; has performed limited work as expert witness for TBI cases; and is author on a patent re: computer analysis of physiologic variables obtained by cerebral ultrasound. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Pott P. Observations on the Nature and Consequences of Those Injuries to Which the Head Is Liable from External Violence. London: Printed for L Hawes, W Clarke, R Collins; 1768 [Google Scholar]
- 2.Jordan B, Tsaris P, Warren R, eds. Sports Neurology. 2nd ed Philadelphia: Lippincott-Raven; 1998 [Google Scholar]
- 3.Kaye AJ, Gallagher R, Callahan JM, Nance ML. Mild traumatic brain injury in the pediatric population: the role of the pediatrician in routine follow-up. J Trauma 2010;68:1396–1400 [DOI] [PubMed] [Google Scholar]
- 4.Giza CC, Kutcher JS, Ashwal S, et al. Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology Epub 2013 Mar 18 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


