Abstract
Antimicrobial resistance and hospital infections have increased alarmingly in India. Antibiotic stewardship and hospital infection control are two broad strategies which have been employed globally to contain the problems of resistance and infections. For this to succeed, it is important to bring on board the various stakeholders in hospitals, especially the clinical pharmacologists. The discipline of clinical pharmacology needs to be involved in themes such as antimicrobial resistance and hospital infection which truly impact patient care. Clinical pharmacologists need to collaborate with faculty in other disciplines such as microbiology to achieve good outcomes for optimal patient care in the hospital setting. The ASPIC programme was initiated by the Indian Council of Medical Research (ICMR) in response to the above need and was designed to bring together faculty from clinical pharmacology, microbiology and other disciplines to collaborate on initiating and improving antibiotic stewardship and concurrently curbing hospital infections through feasible infection control practices. This programme involves the participation of 20 centres per year throughout the country which come together for a training workshop. Topics pertaining to the above areas are discussed in addition to planning a project which helps to improve antibiotic stewardship and infection control practices in the various centres. It is hoped that this programme would empower hospitals and institutions throughout the country to improve antibiotic stewardship and infection control and ultimately contain antimicrobial resistance.
Keywords: Antimicrobial Stewardship, ASPIC, ICMR workshop
Introduction
Clinical pharmacology, a bridge discipline between basic sciences and clinical disciplines, was started in India in the 1960s1. The development of pharmaceutical industry, clinical trials, accreditation issues in hospitals, and the commitment of the Government to provide essential medicines have necessitated a sea change in the role of the clinical pharmacologist. Capacity building with training in various skills for roles and responsibilities of the clinical pharmacologist is therefore needed. The Indian Council of Medical Research (ICMR) in its centenary year 2011-2012 gave a major boost to development of clinical pharmacology in India and planned workshops in thrust areas2. One of the major thrust areas was that of antibiotic use, resistance and infection control. This area is unique in that it is truly an integrated area covered by the disciplines of clinical pharmacology, microbiology and infectious diseases.
Bacterial infections are a major contributing factor to mortality in the world3, and bacterial resistance to antibiotics has become an all pervading problem throughout the world4,5, and in India6,7. One of the major contributing factors towards resistance has been antibiotic use8. Antibiotic use has been seen to be high in India with one recent surveillance study indicating 40 per cent of patients in the community on antibiotics9, and an even higher rate of inappropriate use10. One of the strategies to counter this would be to initiate antibiotic stewardship programmes11. Antibiotic stewardship is a multidisciplinary programme with interventions and strategies to encourage appropriate use of antibiotics. Stewardship programmes aim to restrict inappropriate use of antibiotics, optimize selection, dose, route and duration of treatment for best outcomes, minimizing detrimental adverse events, excessive costs and emergence of resistance. The team involved in Antibiotic Stewardship is multidisciplinary and consists of an infectious disease physician, clinical pharmacologist/pharmacist, clinical microbiologist, infection control nurse and hospital administrator.
These programmes have been shown to have both clinical and economic impact in hospitals12. Strategies such as development and implementation of treatment guidelines, audit and feedback, and parenteral to oral conversion have been shown to be effective. There have however, been barriers also such as lack of awareness and support from physicians, lack of trained manpower and sometimes administrative shortsightedness.
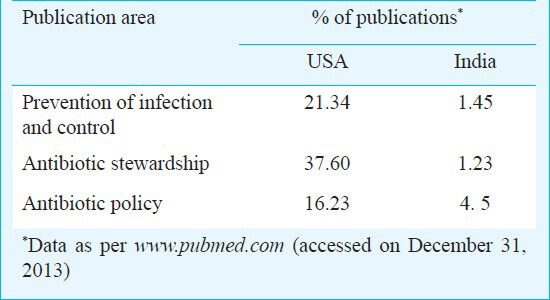
In India, while infection control guidelines and training programme had started relatively early13, Antimicrobial Stewardship programme, guidelines and training have lagged behind. Publications from India on prevention of infection and control are only a few and on antibiotic stewardship are even fewer (Table).
Table.
Number of publications on ASPIC
It was, therefore, deemed important by the ICMR that the discipline of clinical pharmacology takes on this void through a training programme not just to build capacity in antibiotic stewardship and infection control and impact hospitals, but also to initiate research projects in different hospital centres which would help in baseline studies and improve the situation with interventional strategies. The ASPIC programme was initiated through the collaboration of the Office of the National Chair of Clinical Pharmacology, ICMR, and the Christian Medical College, Vellore. This report outlines the content of the Antibiotic Stewardship, Prevention of Infection and Control (ASPIC) programme, the primary workshop conducted in 2012 in Vellore, Tamil Nadu, India, the issues in capacity building in Antibiotic Stewardship (AS) and the way forward.
The overall programme was of one year with two contact sessions (workshops) and a project.
ASPIC workshop
The workshop was planned to provide training to participants to equip them with (i) skills and understanding required for infection prevention and control practice; (ii) knowledge and skills required for development and implementation of antimicrobial policy guidelines for rational use of antibiotics to curb antibiotic resistance; and (iii) ability to plan and conduct research projects in antibiotic policy, infection prevention and control practice.
Selection of participants: Twenty participants were selected on the basis of their qualification, past experience and quality of the concept research paper on antimicrobial stewardship and infection control. Among the participants selected, 15 were microbiologists, four were pharmacologists and one was a physician (Figure).
Fig.
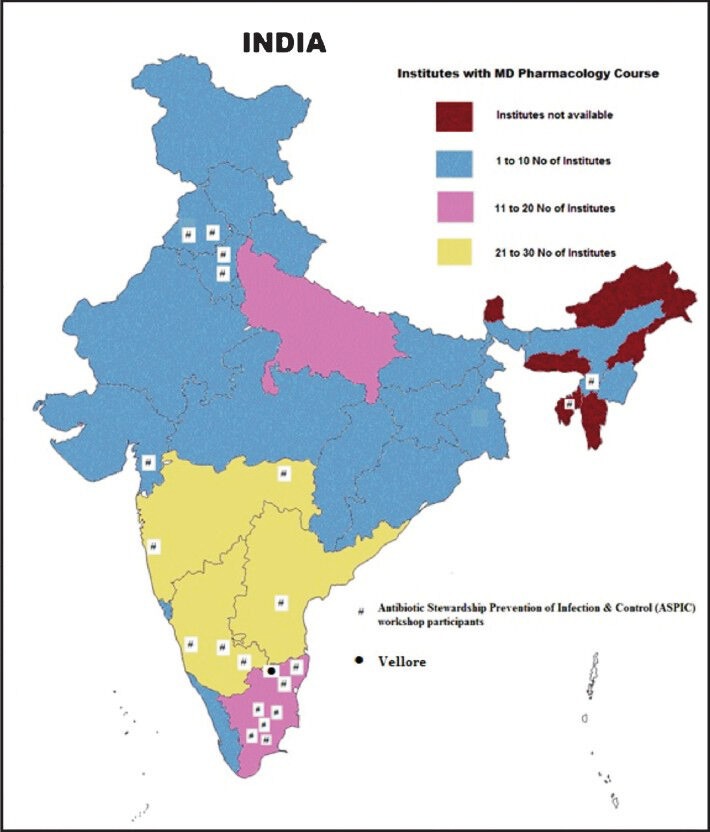
Map showing ASPIC workshop participants coming from different parts of the country.
Description of the workshop: The first contact session of five days (April 16-20, 2012) consisted of 40 hours of lectures, site visits, hands on practical training, demonstrations, and project discussion. The main topics covered and types of training assignments given during the workshop were: (i) Patient safety - Lectures, practical demonstration and site visits; (ii) Health care associated infections - Definitions, preventions, demonstration and visits; (iii) Health care workers health and audits in infection control- Lectures and case discussions; (iv) Antimicrobial stewardship- Lectures and case discussions; and (v) Project discussion.
Resource persons for the workshop were faculty from various specialties (Infectious disease, Clinical microbiology, Clinical pharmacology, Nursing, Intensive care, Surgical specialties, and Hospital infection control).
Session outcomes: By the end of the session on patient safety the participants were able to describe the standard precautions to be used to provide patient safety, principles and methods of, hand hygiene, biomedical waste management and its ultimate disposal, and sterilization of instruments.
After the session on health care associated infections (HCAI), the participants were able to describe the definitions, surveillance and prevention of the following HCAI: (i) Catheter related blood stream infection (CR-BSI); (ii) Ventilator associated pneumonia (VAP); (iii) Skin and soft tissue infection (SSI); and (iv) Catheter associated urinary tract infection (CA-UTI).
By the end of the session on health care workers (HCW) health and infection control related audits the participants were able to describe the dos and dont's of needle stick injury prevention, protection of HCW by immunization and post exposure prophylaxis, main steps of outbreak investigation, different audit on various aspects of infection control, and disinfection of various areas and equipment in the hospital.
By the end of the session on the antimicrobial resistance and stewardship the participants were able to describe the following: (i) Surveillance of antimicrobial resistance and antibiotic consumption in their hospital; (ii) Principles of planning standard treatment guidelines and antimicrobial stewardship for their hospitals; and (iii) Principles of epidemiological investigation of antimicrobial resistance in the laboratory.
Project
During the first contact session, research projects to be undertaken at the participant's institution were discussed. Two projects were selected based on the common problems of the centres and the need for improvement. These projects were aimed at assessing the knowledge and practices in two areas in the hospital, viz. use of antimicrobials in surgical prophylaxis, and use of carbapenems/3rd generation cephalosporins in intensive care units.
After assessment, each centre would develop focused learning modules as an intervention strategy which would be pilot tested and then used as part of the stewardship practice of that hospital. After dissemination of these modules their effectiveness would be assessed by determining the practices once again.
Summary of feedback: All participants found the workshop productive and useful, and they enjoyed the style of teaching, the visits to see various laboratories, processes and facilities. The content of the workshop was felt to be adequate. However, some of the participants were of the opinion that the microbiological aspects could be reduced. The most appreciated session was on antimicrobial stewardship. Many participants wanted more time for project discussion and finalization.
Overall outcomes and evaluation of programme: At the end of the programme, it was hoped that each participant's institution would have a comprehensive systematic Infection Control and Antibiotic Stewardship programme, an Antibiotic Guidelines manual based on the local antimicrobial resistance pattern, and completed research projects and papers for publication.
The programme will be evaluated using the following parameters: (i) Participant attendance for workshops; (ii) Pre- and post-test workshop scores; (iii) Workshop feedback; (iv) Training others in participant's institution and region; (v) Implementation of antibiotic stewardship in participant's institution; (vi) Implementation of infection control practices in participant's institution; (vii) Development of antibiotic policy manual in participant's institution; (viii) Research project initiation and completion; and (ix) Dissemination of findings through publication.
Follow up: The project is expected to be completed within 6-8 months after initiation. The second contact workshop was held in July 2013. The projects were presented, discussed and evaluated. The improvements made in the area of antimicrobial stewardship and infection control in each site hospital were discussed.
Practical issues in the ASPIC programme
The commitment of the participants during the first workshop was commendable. The programme had applications from microbiologists and pharmacologists. The mix of personnel from different disciplines also created the need for a balance of topics between the disciplines in the short span of workshop time.
The participants were from both private and government medical colleges and hospitals. The presence of an infection control team, quality assured microbiology laboratory, and access to various groups of antibiotics, were highly variable across the institutions. This was a challenge when designing projects that would be able to capture the practices and data uniformly from all institutions. The variation in approach of ethics committees in granting permission for projects was time consuming. It was also important to generate projects which were feasible and doable within the short span of time. Planning for collaborative projects when there is a great variation between participating centres, is challenging. Individual institutional projects may be another approach but the comparison as to which is better between both approaches is debatable.
Conclusion
This workshop was the beginning of a programme initiated by the ICMR, National Chair for Clinical Pharmacology and Christian Medical College, Vellore, to train pharmacologists and microbiologists to address the need for Antibiotic Stewardship and Infection Control in various institutions and hospitals throughout India. The focus was to bring together different disciplines and faculty in working towards a common cause, assessing the ground level realities in antibiotic use and hospital infections as well as developing strategic interventions through a collaborative approach to improve infection control and rational antibiotic use. It is hoped that this programme will raise awareness about these issues and empower the participating centres to train other centres so that antimicrobial resistance and hospital infections can be optimally contained.
Acknowledgment
Authors acknowledge the ICMR for funding and granting permission for the ASPIC project, and thank Drs V.M. Katoch, Ranjit Roy Chaudhury and the other members of TAG, Drs Rajini Kaul and Vijayakumar for their constant support and advice. Authors also thank all the participants and their institutions for their participation in this project, and acknowledge the support received from the Office of the National Chair in Clinical Pharmacology and the Christian Medical College, Vellore for hosting and organizing the ASPIC programme.
References
- 1.Kshirsagar NA. History of clinical pharmacology in India: a brief account. In: Patil PN, Gulati OD, Balaraman R, editors. Topics in the history of pharmacology. Ahmadabad: RK Goyal Publisher; 2005. pp. 148–69. [Google Scholar]
- 2.Indian Council of Medical Research. Thrust Areas of Research for Basic Medical Sciences. [accessed on March 20, 2013]. Available from: www.icmr.nic.in/thrust/thrustbms.htm .
- 3.World Health Organization. The World Health Report 2008 - Primary Health Care (Now More Than Ever), The challenges of a changing world. Figure 8. The shift towards non-communicable diseases and accidents as causes of death. [accessed on January 3, 2012]. Available from: http://www.who.int/whr/2008/08_chap1_fig08_en.pdf .
- 4.Gales AC, Jones RN, Turnidge J, Rennie R, Ramphal R. Characterization of Pseudomonas aeruginosa isolates: occurrence rates, antimicrobial susceptibility patterns, and molecular typing in the global SENTRY Antimicrobial Surveillance Program, 1997-1999. Clin Infect Dis. 2001;32(Suppl 2):S146–5. doi: 10.1086/320186. [DOI] [PubMed] [Google Scholar]
- 5.Hoa NQ, Trung NV, Larsson M, Eriksson B, Phuc HD, Chuc NT, et al. Decreased Streptococcus pneumoniae susceptibility to oral antibiotics among children in rural Vietnam: a community study. BMC Infect Dis. 2010;10:85. doi: 10.1186/1471-2334-10-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mathai E, Chandy S, Thomas K, Antoniswamy B, Joseph I, Mathai M, et al. Antimicrobial resistance surveillance among commensal Escherichia coli in rural and urban areas in Southern India. Trop Med Int Health. 2008;13:41–5. doi: 10.1111/j.1365-3156.2007.01969.x. [DOI] [PubMed] [Google Scholar]
- 7.Jain D, Sinha S, Prasad KN, Pandey CM. Campylobacter species and drug resistance in a north Indian rural community. Trans R Soc Trop Med Hyg. 2005;99:207–14. doi: 10.1016/j.trstmh.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Goossens H, Ferech M, Vander Stichele R, Elseviers M ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365:579–87. doi: 10.1016/S0140-6736(05)17907-0. [DOI] [PubMed] [Google Scholar]
- 9.Chandy SJ, Thomas K, Mathai E, Antonisamy B, Holloway KA, Stalsby Lundborg C. Patterns of antibiotic use in the community and challenges of antibiotic surveillance in a lower-middle-income country setting: a repeated cross-sectional study in Vellore, South India. J Antimicrob Chemother. 2013;68:229–36. doi: 10.1093/jac/dks355. [DOI] [PubMed] [Google Scholar]
- 10.Indira Kumari S, Chandy SJ, Jeyaseelan L, Kumar R, Suresh S. Antimicrobial prescription patterns for common acute infections in some rural & urban health facilities of India. Indian J Med Res. 2008;128:165–71. [PubMed] [Google Scholar]
- 11.Dellit TH, Owens RC, McGowan JE, Jr, Gerding DN, Weinstein RA, Burke JP, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44:159–77. doi: 10.1086/510393. [DOI] [PubMed] [Google Scholar]
- 12.Ng CK, Wu TC, Chan WM, Leung YS, Li CK, Tsang DN, et al. Clinical and economic impact of an antibiotics stewardship programme in a regional hospital in Hong Kong. Qual Saf Health Care. 2008;17:387–92. doi: 10.1136/qshc.2007.023267. [DOI] [PubMed] [Google Scholar]
- 13.Rattan A, Bhujwala RA, Kumar R, Safaya AN. Organization of infection control program. J Acad Hosp Adm. 1992;4:21–5. [PubMed] [Google Scholar]


