Abstract
Background & objectives:
Depression remains largely undiagnosed in women residing in rural India and consequently many do not seek help. Moreover, among those who are diagnosed, many do not complete treatment due to high rates of attrition. This study was aimed to compare the effectiveness of enhanced care with usual care in improving treatment seeking and adherence to antidepressant medication in women with depression living in rural India.
Methods:
Six villages from rural Bangalore were randomized to either community health worker supported enhanced care or usual care. A total of 260 adult depressed women formed the final participants for the analysis. The outcome measures were number of women who sought and completed treatment, number of clinic visits, duration of treatment with antidepressant, changes in severity of depression (HDRS) and changes in quality of life [WHO-QOL (Brev) scale].
Results:
A significantly greater number of women from the treatment intervention (TI) group completed the treatment and were on treatment for a longer duration compared to the treatment as usual (TAU) group. However, there were no significant differences in the severity of depression or quality of life between the TI and the TAU groups or between treatment completers and treatment dropouts at six months.
Interpretation & conclusions:
Enhanced care provided by the trained community health workers to rural women with major depression living in the community resulted in greater number of women seeking help and adhering to treatment with antidepressants. However, despite enhanced care a significant number of rural women diagnosed with depression either did not seek help or discontinued treatment prematurely. These findings have significant public health implications, as untreated depression is associated with considerable disability.
Keywords: Antidepressant adherence, community health workers, depression, primary healthcare, rural women
Depressive disorders are among the most important causes of psychiatric morbidity in primary health care facilities. Depression alone has been projected to be the second highest cause of disease burden by 20301. The prevalence of depression in primary care settings in India and other Southeast Asian countries ranges between 20 to 40.45 per cent2. It has been shown to be associated with female gender, poverty and low educational status. The lifetime prevalence of major depressive disorders (MDD) in women is 21.3 per cent, which is almost twice that of men3. A study by Patel et al4 highlighted that women living in rural and peri-urban communities, particularly those who have experienced gender disadvantages and economic difficulties, are at risk of common mental health disorders. Women generally have low autonomy, poor support from their family and experience domestic violence all of which are risk factors for common mental disorders (CMD)5,6. Depression is underdiagnosed and causes high morbidity and mortality in this vulnerable group, even though it can be easily identified and treated with medications and psychotherapy7. Hence, there is a need to evaluate methods to improve help seeking and treatment adherence in women with major depression.
The majority of patients with depression in India and other developing countries seeking help at primary health care settings receive pharmacotherapy. The clinical effectiveness of which is limited by patient adherence to the recommended treatment protocol and underdiagnosis and/or sub-optimal treatment by primary care doctors8. One of the most common reasons for inadequate treatment of depression is the high rate of attrition (discontinuing treatment prematurely). A study conducted in Goa, India, that compared imipramine and fluoxetine found that compliance to treatment among patients with depression was poor and that majority of patients had discontinued antidepressant medication due to side effects9. The same group of investigators did a randomized placebo controlled trial in patients with depression attending general outpatient clinic and reported adherence rates to antidepressant medication of 46 per cent at 2 months and 26 per cent at 6 months. Common reasons for non-adherence at two months were side effects, forgetting to take medication and feeling better. At six months, the main reasons were feeling better, being physically sick or taking medication10. Given such high rates of treatment non-adherence, it is surprising that adherence has rarely been the object of specific research when compared to the vast amount of research on the effectiveness of antidepressants11.
Studies from India have shown that a significant number of subjects diagnosed with depression living in the community do not seek help from the health care facilities even when help is available locally and this is more likely in the case of women diagnosed with depression12,13. A study in south India (rural) in community dwelling women with major depression found that 21.5 per cent continued antidepressant medication as defined by compliance criteria and regular clinic visits for more than two months, 32.1 per cent discontinued treatment prematurely (<2 months) and 46.4 per cent patients did not seek treatment even when it was made available in a nearby primary health centre. The reasons cited for premature discontinuation included feeling well after a single consultation (4%), lack of transportation (20%), financial difficulties (18%), inability to take time off from the job (14%), lack of efficacy (8%), side-effects (7%), stigma of attending the mental health clinic (5%) and a minority felt that there was no need for treatment (2%)12.
Katon14 has reported that implementation of multi-level interventions and collaborative care that involved case managers who acted as liaison between primary and secondary care clinicians significantly improved treatment adherence and outcomes of depression in patients seeking help from primary health centers. Furthermore, a systematic review found that collaborative care in primary care settings significantly improved medication adherence and associated clinical benefits in patients with major depression compared to education interventions15. These studies have been conducted in the West, and there is no literature, which specifically addresses issues related to improving treatment adherence to antidepressant medications in patients diagnosed with depression in rural India. Therefore, the primary objectives of the present study were to evaluate whether enhanced care resulted in greater number of treatment naïve women with depression living in the community sought help from the primary care center, and to examine whether adherence to antidepressant medication would be better in women receiving enhanced care compared to treatment as usual. The secondary objective included whether there was a change in the severity of depression and quality of life (QOL) before and after the treatment intervention.
Material & Methods
The study was conducted by the department of Psychiatry, St. John's Medical College and Hospital, Bangalore, Karnataka, India, in six villages covered under a primary health centre (PHC). There were 33 villages under this PHC covering a population of 29,117; of which, six villages were selected based on their proximity to the PHC. A house-to-house survey was conducted in the selected villages by a trained research investigator to screen for rural women with depression after obtaining a written informed consent. The institutional ethics committee approved the protocol of this study. The study was conducted from August 2006 till September 2009. CONSORT guidelines with extension to cluster randomised trials were followed16. General Health Questionnaire (GHQ) -28 item version17 was administered to all adult women (>18 yr) in each of the selected villages. GHQ has been used in previous community studies in India and a standardized translated version in the local Kannada language was used in the present study18. Only treatment naive women diagnosed with depression, who did not receive any treatment in the last six months were included in the study. Whole sampling frame was considered for this study.
Assessments: (i) A demographic profile of the women was obtained using a questionnaire designed for the purpose of the study. Age, marital status, education, family size, type of family, employment, past history and family history of mental illness and occupational history were obtained.
(ii) Socio-economic status of the women was obtained using Standard of living Index (SLI)19. This index was used in the National Family Health Survey 1998-1999 to compare the standards of living between rural and urban areas in India20. The scores were tabulated and residents were classified into three categories: Low SLI (0-14), Medium SLI (15-24) and high SLI (25-67).
(iii) Women who obtained a score of more than or equal to 5 on GHQ were interviewed on the Mini International Neuropsychiatric Interview (MINI)21, a structured interview schedule to confirm a psychiatric diagnosis of major depression according to DSM-IV TR (fourth edition of Diagnostic and Statistical Manual of Mental Disorders - Text Revision) criteria. Any axis I co-morbid psychiatric diagnosis was noted.
(iv) The severity of depression was assessed using Hamilton Depression Rating Scale23 (HDRS-17 item version). HDRS is available in the local Kannada language and has been used in previous studies in India12. Scores obtained on the HDRS were used as the outcome variable. HDRS was administered at baseline and later at six months.
(v) WHO Quality of Life (Brev) scale24 was used to assess the quality of life of the women with depression. This questionnaire is available in local languages and has been used in a previous study of CMD in rural populations in India13. The WHOQOL scale consists of 26 items and has four domains that measure physical, psychological, social and environmental components of quality of life. WHOQOL was administered at baseline and at six months.
Selection and training of personnel: The survey team consisted of four CHWs and a research assistant (RA). The CHWs were all women from the local community, had studied upto 10th standard and had a previous experience of working in community mental health programmes25. The research assistant was trained in the administration and scoring of various questionnaires. He was blind to the two groups and was lead through the villages by the CHWs who did not reveal which villages belonged to the intervention group. The participants were reviewed by a trained physician at the PHC, and was blind to the treatment randomization.
Data collection: A house-to-house survey was done in the six villages by the team of health workers and research investigator. All women aged 18 to 65 yr were interviewed after obtaining informed written consent. Initially, socio-demographic details were collected by the CHWs. The research assistant administered the GHQ. Women obtaining a score of more than or equal to five on GHQ and diagnosed to have major depression on MINI-Plus were referred to the weekly clinic in PHC. MINI-Plus has earlier been used in the Indian settings26,27.
Treatment randomization: The six villages covered by the PHC were randomized into two groups of three villages each namely ‘Treatment as usual (TAU)’ and ‘Treatment intervention (TI)’ groups. Cluster randomized analysis was used. Village was taken as the unit of randomization and the analysis was done at the participant level. In the TI group, patients were monitored regularly by the CHW. Patients diagnosed with depression needed to visit the primary health centre once a month to consult with the physician. In the TI group, the CHWs visited patients immediately following the first medical consultation, educated the patient and her family members about depression and its treatment. They also emphasised taking antidepressant medication and continuing the treatment regimen. This was followed by another visit in the subsequent week to enquire about any possible side effects of medication and clarification of any doubts concerning the medical treatment of depression. This pattern of visits was maintained after every monthly consultation with the physician in the TI group. In addition, CHWs visited those patients who discontinued medication and / or those who did not visit the PHC for an initial consultation and encouraged them to resume treatment in the intervention group. In the TAU group, patients diagnosed with depression were encouraged to seek help from the physician at PHC with no additional input from the CHW. Treatment completers were defined as those patients who had come for at least four visits or have taken antidepressants for at least 16 wk. A dropout in this study was defined as any patient who missed at least two consecutive appointments with the primary care physician.
Referral and treatment: Those women with depression who were referred to the PHC and visited the clinic were registered. They were given an identity card containing their name, survey number, village and a specific registration number. Separate case sheets were maintained for each of them. After evaluation by a trained physician at the PHC, they were offered treatment with antidepressant medication. The antidepressants selected included either amitryptiline or fluoxetine and the physician made the choice based on the symptom cluster of depression. Those with predominantly anxiety related symptoms were treated with selective serotonin uptake inhibitors (SSRIs) whereas those with predominantly depressive symptoms were treated with amitriptyline. These medications were not available in the essential drug list of the PHC.
Adherence assessment: Adherence to treatment recommendations was measured using the total number of PHC clinic related visits and the total number of weeks the subjects took antidepressant medication. In addition, during home visits the CHW performed pill counts to ensure that patients took medication as prescribed by the PHC doctor.
Statistical analysis: Adjustments were made in the statistical tests to account for the clustering effect of village for the primary outcomes. Intra-cluster correlation i.e. ICC (ρ) was calculated on the log transformed variable. Design effect was calculated by 1+ (n-1) ρ28,29. Descriptive statistics were reported using mean ± SD or number and percentages as appropriate. Independent t test was used to assess the difference between the TAU and the intervention group. Chi-square test or Fisher's exact test as appropriate, was used to find the association between the categorical variables. Mann-Whitney U test was used to compare the number of visits and duration of treatment between the groups. ANCOVA was used to assess the efficacy of intervention at endpoint (the post intervention quality of life and severity of depression) between the study groups adjusting for the baseline values. In ANCOVA, post intervention measures were the dependent variables, study group was the fixed factor and baseline measure were covariates. Intention to treat analysis was performed for the primary objective. The data were analysed using SPSS Inc Chicago, USA. Probability value of less than 5 per cent was considered as significant.
Results
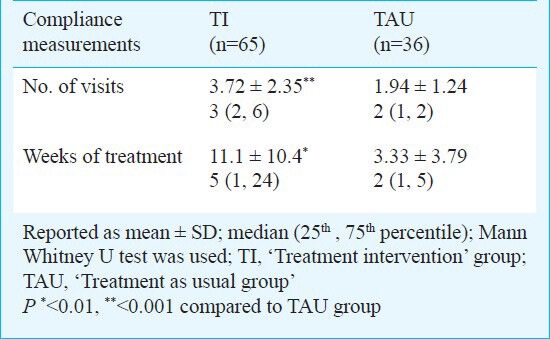
A total of 814 houses were surveyed in six villages. Of the 1055 women (18-65 yr) who were interviewed; 859 (81.4%) consented for the study; 260 subjects who had a diagnosis of major depression as per DSM-IV TR criteria using MINI-Plus formed the final sample for the study (Figure). Among the study participants, majority were married (87.3%), came from nuclear families (57.3%), were not formally educated (56.16%) and most were not employed in formal / informal sector (94.5%). At baseline, there were no significant differences between the TAU and the TI groups in terms of socio-demographic data, clinical characteristics and co-morbid diagnosis (Tables I & II). A significantly (P=0.001) greater number of depressed women from the TI (n=28) completed the treatment compared to the TAU (n=3). The rest of the participants had dropped out of the study. The reasons for the same were not collected. The number of clinic visits and weeks of treatment on antidepressant medication was significantly greater in the TI group compared to TAU group in participants who came for at least one visit to the clinic (Table III). The number of participants who did not come for any visits was higher in the TAU (n=86, 70.5%) compared to TI (n=73, 53%). After adjusting for the major depressive disorder, recurrent type, participants in the TI group were 2 times more likely to visit the clinic as compared to TAU group. Intention to treat analysis revealed significantly more number of visits in the TI group then TAU group (P<0.001). The choice of antidepressants did not influence the treatment adherence. Based on ICC, the estimated design effect was 2.25. After accounting for the clustering effect, the number of clinic visits and weeks of treatment on antidepressant medication was significantly greater in the TI group compared to TAU group (P<0.05).
Fig.
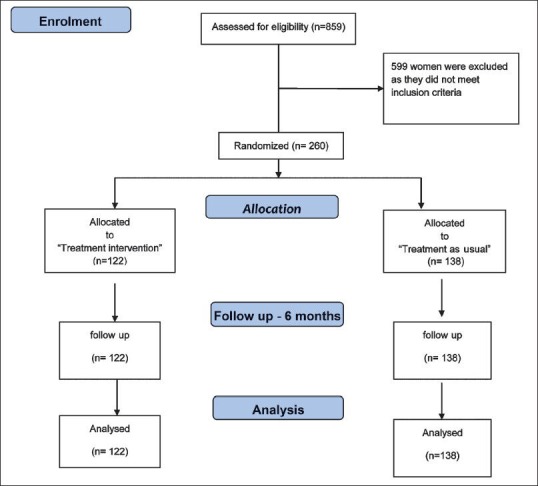
Flow diagram showing the study design.
Table I.
Socio-demographic and clinical profile of the study group (n=260)
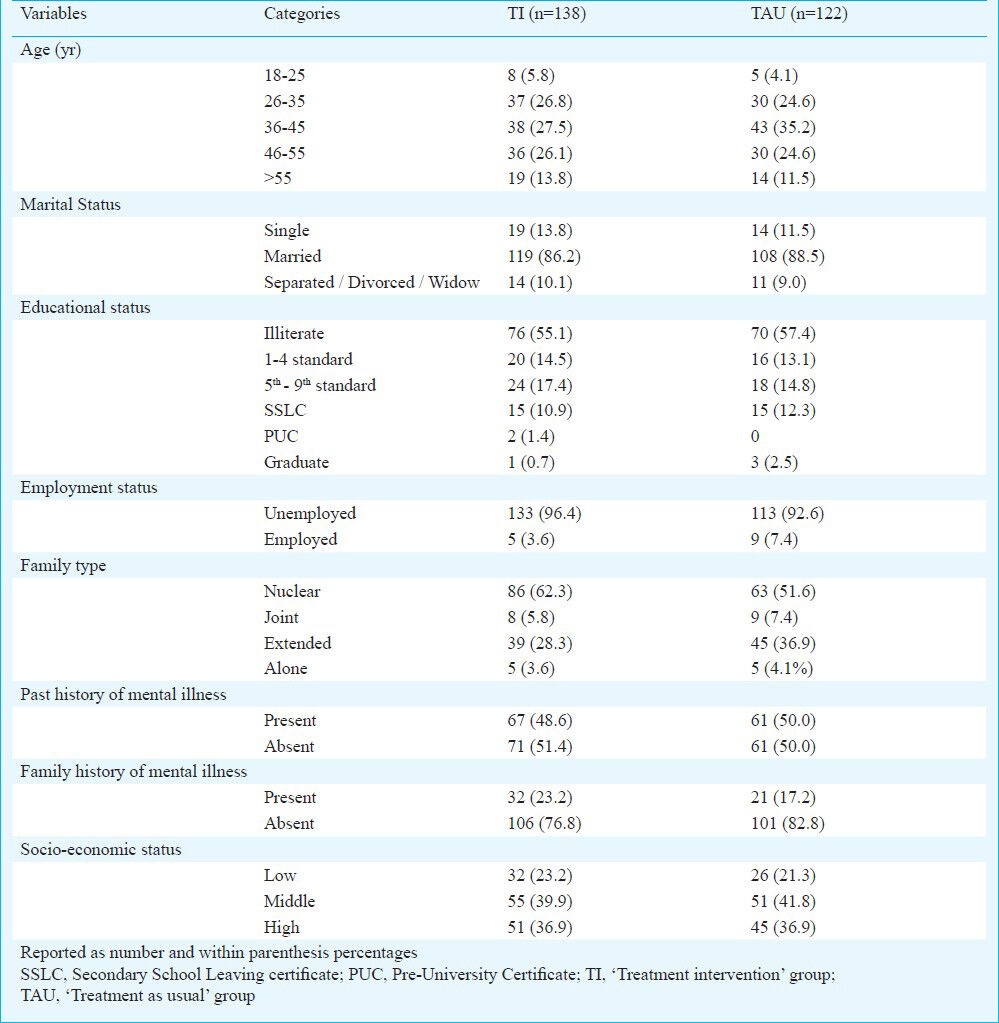
Table II.
Diagnostic categories based on MINI-PLUS in the study group
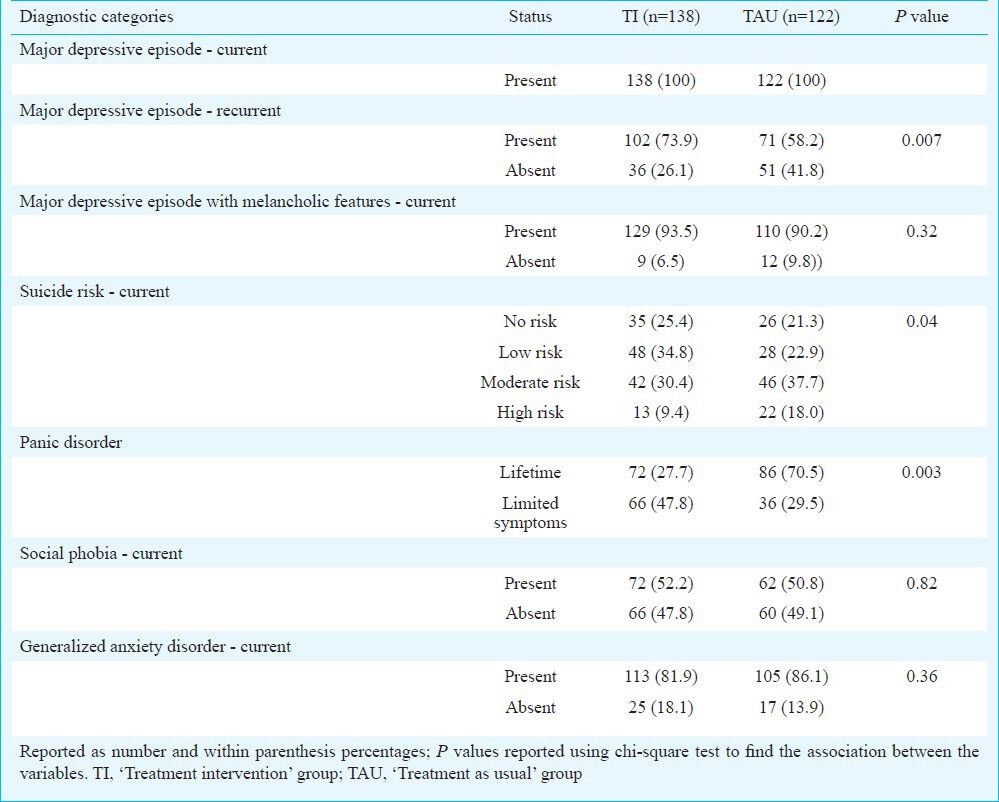
Table III.
Number of visits and duration of treatment of both groups of participants who visited the clinic at least once
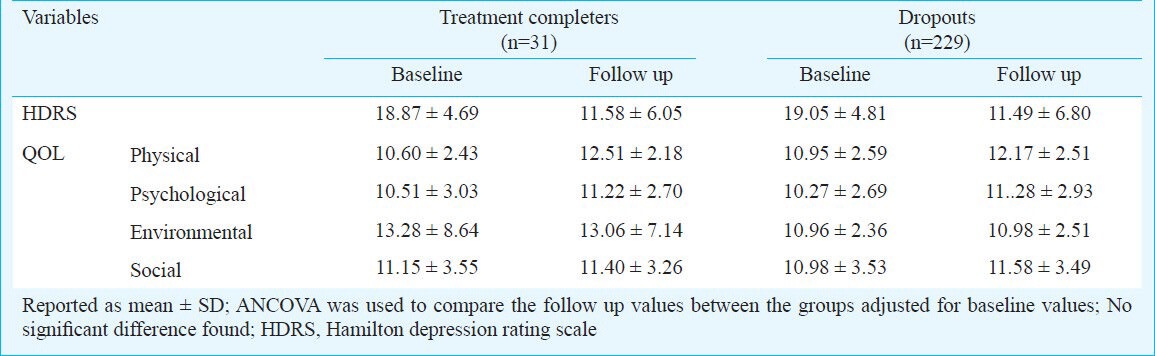
There was no significant difference in the outcome measures at six months on HDRS (11.73 ± 7.24 in TAU group vs 11.30 ± 6.22 in TI group) and quality of life using WHO-QOL (Brev) between the groups after controlling for baseline HDRS score (Table IV). Patients in both the groups had improved significantly at six months. The mean dose of amitryptiline was 54.27 ± 23.23 mg (95% CI=25 to 100) and of fluoxetine was 22.40 ± 6.63 mg (95% CI= 20 to 40), respectively. Additionally, in the entire study population, there was no significant difference in the outcome measures at six months on HDRS between treatment completers and treatment dropouts (11.58 ± 6.06 vs 11.48 ± 6.80) after controlling for baseline HDRS score (Table V).
Table IV.
Baseline and follow up variables of severity of depression and quality of life (QOL)
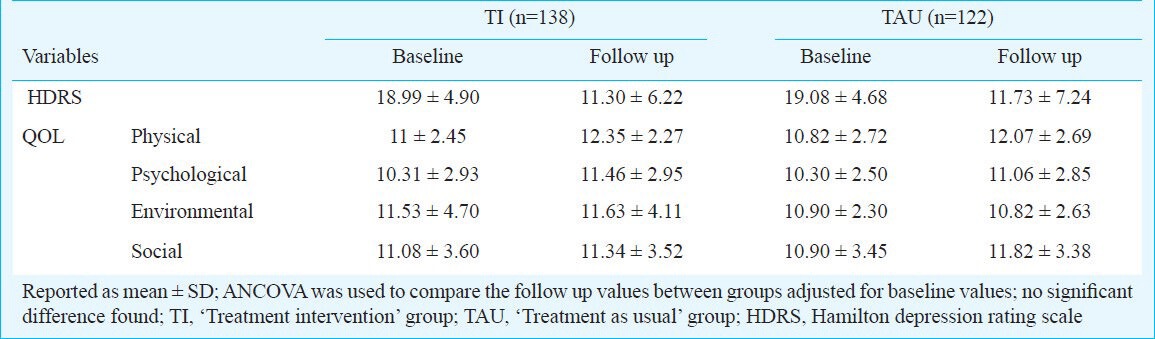
Table V.
Baseline and follow up variables of severity of depression and quality of life (QOL) in treatment completers and dropouts
Discussion
The present study was an attempt to improve treatment adherence to antidepressant medication in treatment naïve rural women diagnosed with major depression. Greater number of depressed women from the TI group contacted the physician compared to women from the TAU group. The dropout rate was higher in the TAU group when compared to the TI group. In addition, the number of clinic related visits and the duration of treatment (as measured by the number of weeks that subjects took antidepressant medication for) was significantly greater in the TI group compared to TAU group. It was difficult to compare findings from the present study to earlier studies on treatment adherence to antidepressant medication, owing to the fact that in majority of the earlier studies treatment adherence was estimated among subjects seeking help from a primary health center; whereas our study catered to women with major depression living in the community who had not sought any medical help. Nevertheless, findings from the present study were in broad agreement with earlier studies that noted better adherence and treatment compliance among patients with major depression who received a collaborative or stepped up care approach14,30.
Treatment adherence to the recommended protocol has been identified as one of the major factors in the effective treatment of depression8. While there have been various attempts to increase treatment retention using collaborative or stepped up care approach in industrialized countries, only a few studies have examined the application of such approaches in resource poor countries. Araya et al31 undertook a study with a resource limited and socio-economically deprived population in a developing country and found a significant improvement in the severity of depression (HDRS) and functional impairment (SF-36) in patients who received the stepped care approach compared to the usual care. The stepped-care programme where trained primary care physicians provided pharmacotherapy had several components such as patient education, behavioural activation, problem solving and structured follow up by non-medical health care workers31. Rickles et al32 in their study used a pharmacist-guided education and monitoring programme to enhance medication adherence. They found that the rate of missed doses at the end of the study was significantly lower in the pharmacist-guided education and monitoring (PGEM) group than the control group, hence suggesting the role of collaborative staff that could play a vital role in improving treatment adherence32.
Despite providing enhanced support through trained CHWs a large number of women living in the community diagnosed with depression did not seek help from the PHC. While other studies from India have made similar observations, it highlights the fact that there are considerable barriers to treatment of depression in rural women in India. In an earlier study on the outcomes of depression in a rural community, it was noted that financial problems, poor access to health care facilities and inability to take time off from work acted as significant barriers to seeking help from the PHC12. In addition, among women, factors such as interpersonal difficulties, heavy drinking in the spouse, and economic difficulties linked to depression, are embedded within the family set up and may act as additional barriers to help seeking33. There is a tendency for women to seek lay help due to both the lack of well-developed services in developing countries and the lack of awareness of mental health services34,35,36. Stigma was found to be more in depressed women in primary care37 and adherence to treatment was poor in women with high stigma38. Hence, these factors need to be considered for a comprehensive treatment of women in developing countries.
While there was a significant difference in the treatment adherence pattern between the two groups, there was no significant difference in the outcomes of depression as measured by HDRS and WHO-QOL at six month follow up. There was a significant reduction in the severity of depression and an improvement in the quality of life in both the groups. In addition, there were no significant differences in outcome measures between treatment completers and dropouts. Chishlom et al13 followed up patients who received standard primary health care and mental health care incorporated with standard primary health care and found that there was a significant improvement in both groups with respect to the outcome domains such as depression, disability and quality of life. They suggested that it could either be due to spontaneous remissions or that the act of interviewing individuals and advising them to seek care could itself have served as an intervention. This could have been the case in our study as well.
We did not do formal sample size estimation and power of the study was not calculated. In addition, a significant limitation of the study was that we did not ascertain the reasons for the large number of women with depression who either did not seek help and or dropped out of treatment.
To conclude, enhanced community support provided by trained CHWs to rural women with major depression resulted in greater number of women adhering to treatment with antidepressant medication and also better treatment retention. However, a significant number of women with major depression still defaulted from treatment recommendations and did not seek help from a local PHC. The finding that a high proportion of subjects with depression did not access locally available health services has important public health implications. In resource poor countries it is also important to examine whether trained community level workers who have far easier access to the community can provide psychosocial interventions. Finally, and importantly this programme helped in enhancing the skills of CHWs in the domain of diagnosis, early identification and counselling of patients with depression.
Acknowledgment
Authors acknowledge the Anuradha Foundation, Los Altos, CA, USA, for financial support.
References
- 1.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grover S, Dutt A, Avasthi A. An overview of Indian research in depression. Indian J Psychiatry. 2010;52:S178–88. doi: 10.4103/0019-5545.69231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noble RE. Depression in women. Metabolism. 2005;54(5 Suppl 1):49–52. doi: 10.1016/j.metabol.2005.01.014. [DOI] [PubMed] [Google Scholar]
- 4.Patel V, Kirkwood BR, Pednekar S, Weiss H, Mabey D. Risk factors for common mental disorders in women. Population-based longitudinal study. Br J Psychiatry. 2006;189:547–55. doi: 10.1192/bjp.bp.106.022558. [DOI] [PubMed] [Google Scholar]
- 5.Cohen A. Excess female mortality in India: the case of Himachal Pradesh. Am J Public Health. 2000;90:1369–71. doi: 10.2105/ajph.90.9.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jejeebhoy SJ. Convergence and divergence in spouses’ perspectives on women's autonomy in rural India. Stud Fam Plann. 2002;33:299–308. doi: 10.1111/j.1728-4465.2002.00299.x. [DOI] [PubMed] [Google Scholar]
- 7.Stewart DE, Ashraf IJ, Munce SE. Women's mental health: a silent cause of mortality and morbidity. Int J Gynaecol Obstet. 2006;94:343–9. doi: 10.1016/j.ijgo.2006.04.025. [DOI] [PubMed] [Google Scholar]
- 8.Geneva: WHO; 2003. World Health Organization. Non-communicable diseases and mental health. Adherence to long-term therapies Project. Evidence for action; pp. 61–6. [Google Scholar]
- 9.Pereira J, Patel V. Which antidepressants are best tolerated in primary care. A pilot randomized trial from Goa? Indian J Psychiatry. 1999;41:358–63. [PMC free article] [PubMed] [Google Scholar]
- 10.Patel V, Chisholm D, Rabe-Hesketh S, Dias-Saxena F, Andrew G, Mann A, et al. Efficacy and cost-effectiveness of drug and psychological treatments for common mental disorders in general health care in Goa, India: a randomised, controlled trial. Lancet. 2003;361:33–9. doi: 10.1016/S0140-6736(03)12119-8. [DOI] [PubMed] [Google Scholar]
- 11.Pampallona S, Bollini P, Tibaldi G, Kupelnick B, Munizza C. Patient adherence in the treatment of depression. Br J Psychiatry. 2002;180:104–9. doi: 10.1192/bjp.180.2.104. [DOI] [PubMed] [Google Scholar]
- 12.Srinivasan K, Isaacs AN, Thomas T, Jayaram G. Outcomes of common mental disorders in a rural community in South India. Indian J Soc Psychiatry. 2006;22:110–5. [Google Scholar]
- 13.Chisholm D, Sekar K, Kumar KK, Saeed K, James S, Mubbashar M, et al. Integration of mental health care into primary care. Demonstration cost-outcome study in India and Pakistan. Br J Psychiatry. 2000;176:581–8. doi: 10.1192/bjp.176.6.581. [DOI] [PubMed] [Google Scholar]
- 14.Katon W. Collaborative depression care models: from development to dissemination. Am J Prev Med. 2012;42:550–2. doi: 10.1016/j.amepre.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 15.Vergouwen AC, Bakker A, Katon WJ, Verheij TJ, Koerselman F. Improving adherence to antidepressants: a systematic review of interventions. J Clin Psychiatry. 2003;64:1415–20. doi: 10.4088/jcp.v64n1203. [DOI] [PubMed] [Google Scholar]
- 16.Campbell MK, Piaggio G, Elbourne DR, Altman DG CONSORT Group. Consort 2010 statement: extension to cluster randomised trials. BMJ. 2012;345:e5661. doi: 10.1136/bmj.e5661. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg, David P. Windsor, England: NFER Publishing; 1978. Manual of the general health questionnaire. [Google Scholar]
- 18.Shamasundar C, Murthy SK, Prakash OM, Prabhakar N, Krishna DK. Psychiatric morbidity in a general practice in an Indian city. Br Med J (Clin Res Ed) 1986;292:1713–5. doi: 10.1136/bmj.292.6537.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parasuraman S. Mumbai: Himalaya Publication; 1999. Role of women's education in shaping fertility in India: Evidences from National Family Health Survey. [Google Scholar]
- 20.Sharma PP, Kumar A, Singh P. A study of gender differentials in the prevalence of tuberculosis based on NFHS-2 and NFHS-3 data. Indian J Community Med. 2010;35:230–7. doi: 10.4103/0970-0218.66869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 22.(DSM-IV-TR) Text Revision. 4th ed. Washington, DC: American Psychiatric Association; 2000. American Psychiatric Association. Major depressive disorders. In: Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 23.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.WHOQoL Group. Development of the World Health Organization WHOQoL-BREF quality of life assessment. Psychol Med. 1998;28:551–8. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 25.Isaacs AN, Srinivasan K, Neerakkal I, Jayaram G. Initiating a community mental health programme in rural Karnataka. Indian J Community Med. 2006;31:86–7. [Google Scholar]
- 26.Rao GP, Moinuddin K, Sai PG, Sarma E, Sarma A, Rao PS. A study of stress and psychiatric morbidity in the central industrial security force. Indian J Psychol Med. 2008;30:39–47. [Google Scholar]
- 27.Sahoo S, Khess CR. Prevalence of depression, anxiety, and stress among young male adults in India: a dimensional and categorical diagnoses-based study. J Nerv Ment Dis. 2010;198:901–4. doi: 10.1097/NMD.0b013e3181fe75dc. [DOI] [PubMed] [Google Scholar]
- 28.Campbell MK, Mollison J, Steen N, Grimshaw JM, Eccles M. Analysis of cluster randomized trials in primary care: a practical approach. Fam Pract. 2000;17:192–6. doi: 10.1093/fampra/17.2.192. [DOI] [PubMed] [Google Scholar]
- 29.Donner A, Klar N. Methods for comparing event rates in intervention studies when the unit of allocation is a cluster. Am J Epidemiol. 1994;140:279–89. doi: 10.1093/oxfordjournals.aje.a117247. [DOI] [PubMed] [Google Scholar]
- 30.Boudreau DM, Capoccia KL, Sullivan SD, Blough DK, Ellsworth AJ, Clark DL, et al. Collaborative care model to improve outcomes in major depression. Ann Pharmacother. 2002;36:585–91. doi: 10.1345/aph.1A259. [DOI] [PubMed] [Google Scholar]
- 31.Araya R, Rojas G, Fritsch R, Gaete J, Rojas M, Simon G, et al. Treating depression in primary care in low-income women in Santiago, Chile: a randomised controlled trial. Lancet. 2003;361:995–1000. doi: 10.1016/S0140-6736(03)12825-5. [DOI] [PubMed] [Google Scholar]
- 32.Rickles NM, Svarstad BL, Statz-Paynter JL, Taylor LV, Kobak KA. Pharmacist telemonitoring of antidepressant use: effects on pharmacist-patient collaboration. J Am Pharm Assoc. 2005;45:344–53. doi: 10.1331/1544345054003732. [DOI] [PubMed] [Google Scholar]
- 33.Pereira B, Andrew G, Pednekar S, Pai R, Pelto P, Patel V. The explanatory models of depression in low income countries: listening to women in India. J Affect Disord. 2007;102:209–18. doi: 10.1016/j.jad.2006.09.025. [DOI] [PubMed] [Google Scholar]
- 34.Kermode M, Bowen K, Arole S, Pathare S, Jorm AF. Attitudes to people with mental disorders: a mental health literacy survey in a rural area of Maharashtra, India. Soc Psychiatry Psychiatr Epidemiol. 2009;44:1087–96. doi: 10.1007/s00127-009-0031-7. [DOI] [PubMed] [Google Scholar]
- 35.Kermode M, Bowen K, Arole S, Joag K, Jorm AF. Community beliefs about treatments and outcomes of mental disorders: a mental health literacy survey in a rural area of Maharashtra, India. Public Health. 2009;123:476–83. doi: 10.1016/j.puhe.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 36.De Toledo Piza Peluso E, Blay SL. Public beliefs about the treatment of schizophrenia and depression in Brazil. Int J Soc Psychiatry. 2009;55:16–27. doi: 10.1177/0020764008092351. [DOI] [PubMed] [Google Scholar]
- 37.Roeloffs C, Sherbourne C, Unützer J, Fink A, Tang L, Wells KB. Stigma and depression among primary care patients. Gen Hosp Psychiatry. 2003;25:311–5. doi: 10.1016/s0163-8343(03)00066-5. [DOI] [PubMed] [Google Scholar]
- 38.Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Raue P, Friedman SJ, et al. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. Am J Psychiatry. 2001;158:479–81. doi: 10.1176/appi.ajp.158.3.479. [DOI] [PubMed] [Google Scholar]


