Abstract
Recent studies have shown that the efficacy of benzimidazole drugs is influenced by the intensity of trichuriasis. Therefore, the objective of this study was to determine the efficacy of albendazole (ALB) and mebendazole (MBZ) administered randomly for 1 (ALB×1 and MBZ×1) or 2 days (ALB×2 and MBZ×2) to 385 school children with heavy-intensity trichuriasis (mean faecal egg counts (FEC) >1000 eggs per gram of stool (epg)) in Jimma Town, Ethiopia. The efficacies (95% confidence intervals) by means of reduction in faecal egg counts (FECs) were 29.3% (−9.9–56.2), 60.0% (48.5–70.9), 73.5% (64.2–81.3), and 87.1% (81.4–91.2) for ALB×1, MBZ×1, ALB×2, and MBZ×2, respectively. These observations highlight that assessment of the anthelmintic efficacy of existing or new compounds against Trichuris trichiura should be assessed under varying levels of infection intensity.
Keywords: Efficacy, Albendazole, Mebendazole, Trichuris trichiura
Introduction
Mass administration of albendazole (ALB) and mebendazole (MBZ) is the recommended strategy to control the morbidity of infections with soil-transmitted helminths, including Ascaris lumbricoides (roundworm), Trichuris trichiura (whipworm), and Necator americanus/Ancylostoma duodenale (hookworms). In contrast to A. lumbricoides and hookworms, a single dose of benzimidazole drugs shows poor efficacy for T. trichiura.1 For this, multiple dose regimens are likely to be more efficacious.2 Moreover, a recent study has shown that the treatment efficacy of a single dose 400 mg ALB against T. trichiura dropped significantly when the mean baseline faecal egg counts (FECs) increased.3 Hence, the infection intensity should be considered as an important determinant of drug efficacy.
The objective of this study was to determine the efficacy of different regimens of ALB and MBZ administered to 385 school children in Jimma Town, Ethiopia with heavy-intensity of T. trichiura infections.
Materials and Methods
From December 2010 to January 2011, a randomized multi-arm efficacy trial was conducted in Jimma Town, Ethiopia. In total, 605 school children from grade 2 to 8 were recruited and asked to provide one stool sample. In total, 425 school children excreting eggs of T. trichiura were randomly assigned to one of the four treatment arms using the ‘rand’ function in excel. The treatment arms included (1) a single dose of ALB 400 mg (Zentel; GlaxoSmithKline Pharmaceuticals Ltd, India) for 1 day (ALB×1); (2) a single-dose of ALB 400 mg for 2 consecutive days (ALB×2); (3) a single dose of MBZ 500 mg (Vermox, Johnson &Johnson) for 1 day (MBZ×1); and (4) a single dose of MBZ 500 mg for two consecutive days (MBZ×2). Fourteen days after the first treatment, a single stool sample per subjects was re-examined. All stool samples were processed with the McMaster egg counting method as described elsewhere.4 Subjects who were unable to provide a stool sample at baseline; experiencing a severe concurrent medical condition; had diarrhea at time of the first sampling; had known history of allergic reaction to benzimidazoles; or were pregnant were excluded from the study.
This trial was registered under Clinical trials.gov identifier B67020109355 and approved by the Ethical Committee of Jimma University (RPGC/11/2003) Ethiopia, Ghent University (2010/517), and Antwerp University (A10-55), Belgium. The school administrators, parents, and the children were informed about the nature and purpose of the study. Only those children, who were willing, and where the parents consented by signing, participated in the study.
The efficacy of the different treatment arms was evaluated quantitatively based on faecal egg count reduction (FECR) using the formula:
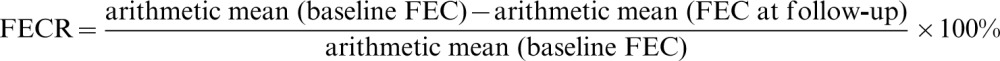 |
The 95% confidence intervals (95% CI) for age, sex ratio (females/males) and FECR were determined by bootstrap analysis (10 000 iterations). Finally, permutation tests and Bonferonni post-hoc corrections were performed to do a pairwise comparison of age, sex ratio, and FECR in the different treatment arms. The level of significance was set at P<0.05.
Result and Discussion
In total 425 subjects (prevalence of T. trichiura infection = 70.2%) were allocated to the different treatment arms (nALB×1 = 107; nALB×2 = 106; nMBZ×1 = 106; nMBZ×2 = 106). Of these 425 subjects, 385 subjects received the assigned treatment regimen and provided a stool sample at follow-up (compliance rate of 90.6%). The mean (95% CI) age and ratio of females/males of the subjects included in the final analysis were 11.0 (10.8–11.2) and 1.35 (1.11–1.65) years, respectively. These parameters did not significantly differ between the four treatment arms. No adverse events were reported.
Table 1 summarizes the mean baseline FEC of T. trichiura and the FECR of the four treatment arms. Across the treatment arms, there was no significant difference in mean baseline FEC, ranging from 1075 to 1262 eggs per gram of stool (epg). MBZ treatment arms were more efficacious than ALB arms and repeated doses were more efficacious than single dose arms. However, this difference in efficacy between treatment arms was not significant for pairwise comparison of ABZ×1–MBZ×1 (P = 0.21) and ALB×2–MBZ×1 (P = 0.29).
Table 1. Mean baseline faecal egg counts (FEC) and reduction in faecal egg counts (FECR) of four treatment arms against Trichuris trichiura.
| n | Mean FEC (epg) (95% CI) | FECR (%) (95% CI) | Significant pairwise comparison | |
| ALB×1 | 102 | 1193 (867.2–1590) | 29.3 (−9.9–56.2) | ALB×2, MBZ×2 |
| MBZ×1 | 103 | 1075 (863.2–1305) | 60.0 (48.5–70.9) | MBZ×2 |
| ALB×2 | 90 | 1262 (977–1578) | 73.5 (64.2–81.3) | ALB×1, MBZ×2 |
| MBZ×2 | 90 | 1122 (899–1371) | 87.1 (81.4–91.2) | ALB×1 and 2, MBZ×1 |
Note: ALB×1: a single-dose albendazole 400 mg; ALB×2: a repeated single-dose albendazole 400 mg across 2 consecutive days; MBZ×1: a single-dose mebendazole 500 mg; MBZ×2: a repeated single-dose mebendazole 500 mg across 2 consecutive days; 95% CI: 95% confidence interval; epg: eggs per gram stool; n: number of subjects.
In agreement with a previous review,2 both drugs show limited efficacy against T. trichiura and repeated doses of MBZ are the most efficacious. However, administering multiple doses has some important logistic implications in mass drug administration programmes. Compared to a previous study which was conducted by our group under comparable demographic [mean (95% CI) age = 11.1 years (10.7–11.5); sex ratio = 1.1 (0.75–1.63)], environmental (Jimma Town, December 2009), and research conditions (McMaster egg counting method, same lot no. of ALB), but including light-intensity T. trichiura infection (mean baseline FEC = 420 epg),5 a single-dose ALB was significantly less efficacious: (92.4% (88.1–95.9) versus 29.3% (−9.9–56.2)). These observations highlight that assessment of the anthelmintic efficacy of existing or new compounds against T. trichiura should be assessed under varying levels of infection intensity. This is in particular for MBZ, for which trials assessing the drug efficacy based on a standard protocol are lacking.
Funding
The fieldwork received financial support from the Flemish interuniversity Council (VLIR-IUC/JU) programme. BL is funded by the Fund for Scientific Research-Flanders (Belgium) (F.W.O.-Vlaanderen).
Conflicts of Interest
None declared.
Ethical Approval
This trial was registered under Clinical trials.gov identifier B67020109355 and approved by the Ethical Committee of Jimma University (RPGC/11/2003) Ethiopia, Ghent University (2010/517) and Antwerp University (A10-55), Belgium. The school administrators, parents, and the children were informed about the nature and purpose of the study. Only those children, who were willing, and where the parents consented by signing, participated in the study.
Authors’ Contribution
ZM, BL, GB, J-PB, and JV designed the study. ZM and BL have examined the samples, carried out statistical analysis and interpretation of the data. ZM drafted the manuscript. BL GB, J-PB, and JV critically revised and approved the final manuscript. ZM and BL are the guarantor of the paper.
References
- 1.Keiser J, Utzinger J. Efficacy of current drugs against soil-transmitted helminth infections: systematic review and meta-analysis. JAMA. 2008;299:1937–48. doi: 10.1001/jama.299.16.1937. [DOI] [PubMed] [Google Scholar]
- 2.Bennett A, Guyatt H. Reducing intestinal nematode infection: efficacy of albendazole and mebendazole. Parasitol Today. 2000;16:71–4. doi: 10.1016/s0169-4758(99)01544-6. [DOI] [PubMed] [Google Scholar]
- 3.Levecke B, Mekonnen Z, Albonico M, Vercruysse J. The impact of baseline faecal egg counts on the efficacy of single-dose albendazole against Trichuris trichiura. Trans R Soc Trop Med Hyg. 2012;106:128–30. doi: 10.1016/j.trstmh.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Levecke B, Behnke JM, Ajjampur SS, Albonico M, Ame SM, Charlier J, et al. A comparison of the sensitivity and fecal egg counts of the McMaster egg counting and Kato-Katz thick smear methods for soil-transmitted helminths. PLoS Negl Trop Dis. 2011;5:e1201. doi: 10.1371/journal.pntd.0001201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vercruysse J, Behnke JM, Albonico M, Ame SM, Angebault C, Bethony JM, et al. Assessment of the anthelmintic efficacy of albendazole in school children in seven countries where soil-transmitted helminths are endemic. PLoS Negl Trop Dis. 2011;5:e948. doi: 10.1371/journal.pntd.0000948. [DOI] [PMC free article] [PubMed] [Google Scholar]


