Abstract
Objective
To verify the prevalence of intestinal parasitic infections among preschoolers and to identify the associated risk factors.
Methods
The study is a cross-sectional study nested in a cohort of children who were born and resident in Diamantina, Minas Gerais, Brazil. At the time of the study, all children were aged 60 months ± five months. They were recruited after written informed consent was obtained from parents or guardians. The study was carried out between July 2009 and July 2010. In total 214 children provided a stool sample for examination on intestinal parasitic infections. Information on potential risk factors for parasitosis was obtained from parents and guardians of the children by a questionnaire. Logistic regression was used for analysis.
Results
Intestinal parasitic infections were found in 27.5% (n = 59) of children. The boys' infection prevalence (26.1%, n = 36) was slightly lower than the infection prevalence of the girls (30.3%, n = 23), but not statistically different (p = 0.51). Fourteen children, (23.7%) were infected with two or more parasite species and forty-five (76.3%) with single parasites. A low per capita income of family was strongly associated with an increased risk for an infection (OR = 2.89; P = 0.003). Preschoolers whose mothers did not work outside home had a significantly lower risk for infection (OR = 0.41; p = 0.01).
Conclusion
Intestinal parasite infection is a health problem among Diamantina preschoolers. Poverty was implicated as an important risk factor for infection, while the presence of the mother at home full-time was a protective factor.
Keywords: Intestinal parasite, Preschool, Risk factor, Poverty
Introduction
Intestinal parasitic infections remain a serious public health issue in Brazil. They affect large segments of the population in terms of their ability to perform mental, physical, and social activities.1 It is estimated that, globally, over a billion individuals currently host at least one species of intestinal parasite, having the soil-transmitted helminths (STH), such as Ascaris lumbricoides, Trichuris trichiura, and Ancylostomatidae species, the highest prevalence rates.2 This study aimed to estimate the prevalence and to identify factors associated with parasitic infections among 5 year old preschoolers residing in a poor urban community of Brazil.
Method
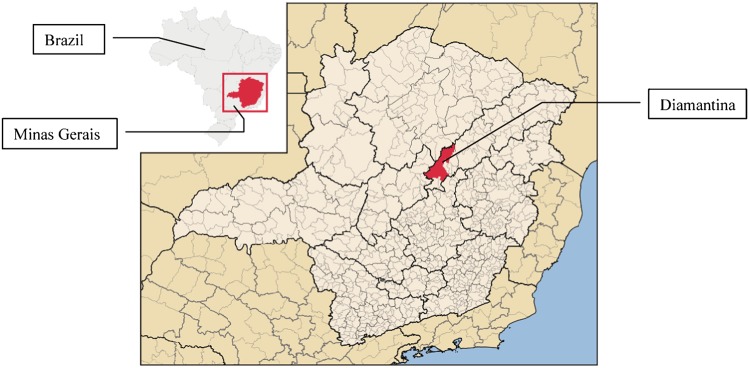
This study was carried out in Diamantina, a city located in the Jequitinhonha Valley, one of the poorest areas of the state of Minas Gerais, Brazil (Fig. 1). The total population of Diamantina in 2010 was 45 884;3 90.8% of households were supplied with treated water, 70.7% with a sewage, and 69.7% with garbage collection system.4
Figure 1.
Location of the study areas in Minas Gerais, Brazil.4
The study is a cross-sectional study nested in a cohort of children who were born and resident in Diamantina, Minas Gerais, Brazil between September 2004 and July 2005.5 At the moment of the study, all children were aged 60 months±5 months. They were recruited after written informed consent was obtained from parents or guardians. The study was carried out between July 2009 and July 2010.
In total 214 children provided a stool sample (male: 138; female: 76) for examination on intestinal parasitic infections. Each stool sample was examined with the method described by Hoffman et al.6 and Baerman-Moraes.6 Non-pathogenic parasites (e.g. Entamoeba coli and Endolimax nana) were not recorded.
Data were entered in excel with simples entry. Statistical analysis was performed using SPSS software system (SPSS Inc., Chicago, IL, USA). Logistic regression was used for analysis. First bivariate analysis was performed. Then, variables associated with a P-value <0.2 were included in the multivariate logistic regression analysis. We used a significance level of P<0.05. Odds ratio (OR) and 95% confidence intervals (95% CIs) of odds ratio were reported.
Information on potential risk factors was obtained from parents and guardians of the children by a questionnaire. Ethics approval (ref. no. ETIC 545/08) was obtained from the Federal University of Minas Gerais.
Results
The mean age of children was 4.9 years (SD = 0.1 years); 138 were boys (64.5%). Two-third (66.8%) of the children live in brickwork houses owned by their families. Almost two-third of the families (59.3%) had a per capita income lower than half of minimum wage. Household sanitary conditions were satisfactory; 95% of the houses had access to treated tap water and 92.2% were connected to a sewage system.
Intestinal parasitic infections were found in 27.5% (n = 59) of children. The boys’ infection prevalence (26.1%, n = 36) was slightly lower than the infection prevalence of the girls (30.3%, n = 23), but not statistically different (P = 0.51). Fourteen children (23.7%) were infected with two or more parasite species. From those with multiple parasites, most consisted of Entamoeba histolytica/dispar and Giardia lamblia (50.2%) and A. lumbricoides and G. lamblia (42.8%) combinations. E. histolytica/dispar (56.2%) and G. lamblia (29.0%) were the most frequent protozoans. Most prevalent helminths were A. lumbricoides (39.0%) and T. trichiura (2.0%). Almost all children (93.6%) were free of any intestinal symptoms of the infection.
Univariate analysis showed that low family income was significantly associated with an increased risk for an intestinal parasitic infection (OR = 2.03, 95% CI = 1.06–3.88, Table 1). In addition, those family with a less space per person had a higher risk for an infection (OR = 1.84, 95% CI = 0.99–3.40).
Table 1. Crude and adjusted odds ratio (OR) associated with occurrence of intestinal parasite infection among preschoolers in Diamantina, Minas Gerais, Brazil.
| Variables | OR | P-value | 95% CI |
| Bivariate analyses | |||
| Per capita family income (MW)* | |||
| <½ | 2.03 | 0.03 | 1.06–3.88 |
| ≧½ | 1 | ||
| Mother’s education (median of full years) | |||
| <9 | 1.13 | 0.68 | 0.62–2.06 |
| ≧9 | 1 | ||
| Mother’s age (median of years) | |||
| <29 | 1.24 | 0.48 | 0.68–2.26 |
| ≧29 | 1 | ||
| Outside-home work mother | |||
| No | 0.62 | 0.15 | 0.33–1.19 |
| Yes | 1 | ||
| Receives government assistance† | |||
| No | 1 | ||
| Yes | 1.78 | 0.07 | 0.94–3.37 |
| Number of room per person in the house | |||
| ≤1.25 | 1 | ||
| >1.25 | 1.84 | 0.05 | 0.99–3.40 |
| Child attends school | |||
| Yes | 0.91 | 0.85 | 0.36–2.33 |
| No | 1 | ||
| Characteristics of domicile | |||
| Completed brickwork | 1 | ||
| Incomplete brickwork | 1.74 | 0.07 | 0.94–3.24 |
| Gender | |||
| Girls | 1 | ||
| Boys | 0.86 | 0.51 | 0.55–1.34 |
| Connected to sewage network | |||
| Yes | 1 | ||
| No | 1.95 | 0.19 | 0.71–5.39 |
| Multivariate analyses‡ | |||
| Per capita income (MW)* | |||
| <½ | 2.89 | 0.003 | 1.43–5.87 |
| ≧½ | 1 | ||
| Outside-home work mother | |||
| No | 0.41 | 0.013 | 0.19–0.83 |
| Yes | 1 | ||
Note: *Minimum wage of US$288.1.
†Receives government assistance included: Bolsa Família (Program of conditional income transfer to families in a situation of poverty) and/or milk distribution program.
‡Analysis adjusted for variables with P-value <0.2 in bivariate analyses.
Multivariable logistic regression identified two risk factors. A low per capita income of a family was strongly associated with an increased risk for parasitic infection (OR = 2.89, 95% CI = 1.43–5.87, P = 0.003) compared with those at higher per capita income. Preschoolers whose mothers did not work outside-home had a significantly lower risk for an infection (OR = 0.41, 95% CI = 0.19–0.83, P = 0.01), compared with those children whose mothers work outside-home.
Discussion
Our findings about intestinal parasitic infection prevalence rates are consistent with reports of other studies conducted in Brazilian cities, when similar socio-economic population groups were examined. They ranged between 24.6% and 58.7%.7–9 Our results are also consistent with studies from other countries, which had rates between 19% and 85.1%.10–12 The wide variations observed in these studies can be attributed to methodological differences between the studies, but also to socio-economic and ecological different conditions as well as varying health services of the studied areas.13
Although we have identified high infection rates with E. histolytica/E. dispar (56.2%), this finding may be underestimated. Hung and colleagues14 showed that microscopy examination in routine clinical laboratories has a low sensitive for E. histolytica/E. dispar detection. Diagnosis is best performed with molecular tests, which have a high sensitivity, e.g. PCR-based.14
Protozoan infection such as E. histolytica/E. dispar and G. lamblia and STH infections are associated with poor sanitary conditions.15 Most common infection routes are food, contaminated water, and close person-to-person contacts (fecal–oral transmission). Surprisingly, we did not find any infection with Blastocystis hominis. It has been reported in previous Brazilian studies in considerable infection, prevalence ranging from 3.4 to 38.3%.16 The absence of this parasite in our study may be, in part, due to the relative unfamiliarity with this protozoan and the low sensitivity of our diagnostic methods with regard to this intestinal protozoa.17
In our study, poverty was the main predictor for a parasitic infection in these preschool children. This is consistent with other reports. Poverty is usually associated with poor personal and food hygiene habits such as eating raw/unwashed vegetables, absence of hand washing before eating,12 large family size,18 poor sewage network coverage,11 and poor environmental conditions, such as living in crowded houses with insufficient indoor spaces and living in shanty areas.19
As observed in studies from other countries,19–21 intestinal parasitic infections occur less frequently among children whose mother does not work outside-home. The mother’s presence at home enables more care in terms of health and nutrition, including the children’s personal and food hygiene practices.
Our study has certain limitations. The most important was the difficulty of collecting more than one stool sample at the age studied. If a greater number of samples had been collected on different days, it would have increased the possibility of detecting parasites or cysts, eggs, and larvae. Some family stored the stool sample in their refrigerator, which may explain the absence of Strongyloides stercoralis and hookworm in our samples. Eggs and larvae of the parasites are very sensitive to low temperatures.
In conclusion, intestinal parasite infection is a health problem among Diamantina preschoolers. Lower income and employment status of mothers were significant factors related to these infections. Therefore, interventions including improvement of socioeconomic status, sanitation, health education to promote awareness about health and hygiene, and a periodic deworming are measures that must be considered and implemented.
References
- 1.Oliveira AA, Nascimento AS, Santos TA, Carmo GM, Dimech CP, Alves RM, et al. Estudo da prevalência e fatores associados à fasciolose no Município de Canutama, Estado do Amazonas, Brasil. Epidemiol Serv Saúde. 2007;16:251–9. [Google Scholar]
- 2.World Health Organization. Deworming for health and development. Report of the Third Global Meeting of the Partners for Parasite Control. Geneva: World Health Organization; 2005. [Google Scholar]
- 3.Instituto Brasileiro de Geografia e Estatística. Informações estatísticas [sitio da Internet] [cited 2012 Jan 3]. Available from: http://www.ibge.gov.br/cidadesat/topwindow.htm. [Google Scholar]
- 4.Wikipédia [Internet] Diamantina [cited 2012 Jan 3]. Available from: http://pt.wikipedia.org/wiki/Diamantina. [Google Scholar]
- 5.Lessa AC.Alimentação e crescimento no primeiro ano de vida: um estudo de coorte. [Tese] Salvador: Universidade Federal da Bahia, Programa de Pós-Graduação em Saúde Pública2010. p122 [Google Scholar]
- 6.WHO. Basic laboratory methods in medical parasitology. Geneva: WHO; 1991. [Google Scholar]
- 7.Menezes AL, Lima VM, Freita MT, Rocha MO, Silva EF, Dolabella SS. Prevalence of intestinal parasites in children from public daycare centers in the city of Belo Horizonte, Minas Gerais, Brazil. Rev Inst Med Trop. 2008;50:57–9. doi: 10.1590/s0036-46652008000100013. [DOI] [PubMed] [Google Scholar]
- 8.Maia MM, Fausto MA, Vieira EL, Benetton ML, Carneiro M. Intestinal parasitic infection and associated risk factors, among children presenting at outpatient clinics in Manaus, Amazonas state, Brazil. Ann Trop Med Parasitol. 2009;103:583–91. doi: 10.1179/000349809X12459740922417. [DOI] [PubMed] [Google Scholar]
- 9.Gonçalves AL, Belizário TL, Pimentel JB, Penatti MP, Pedroso RS. Prevalence of intestinal parasites in preschool children in the region of Uberlândia, State of Minas Gerais, Brazil. Rev Soc Bras Med Trop. 2011;44:191–3. doi: 10.1590/s0037-86822011005000022. [DOI] [PubMed] [Google Scholar]
- 10.Nyantekyi LA, Legesse M, Belay M, Tadesse K, Manaye K, Macias C, et al. Intestinal parasitic infections among under-five children and maternal awareness about the infections in Shesha Kekele, Wondo Genet, Southern Ethiopia. Ethiop J Health Dev. 2010;24:185–90. [Google Scholar]
- 11.Sejdini A, Mahmud R, Lim YA, Mahdy M, Sejdini F, Gjoni V, et al. Intestinal parasitic infections among children in central Albania. Ann Trop Med Parasitol. 2011;105:241–50. doi: 10.1179/136485911X12987676649584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tappe KH, Mohammadzadeh H, Khashaveh S, Rezapour B, Barazesh A. Prevalence of intestinal parasitic infections among primary school attending students in Barandooz-Chay rural region of Urmia, West Azerbaijan province, Iran in 2008. Afr J Med Res. 2011;5:788–91. [Google Scholar]
- 13.Fonseca EO, Teixeira MG, Barreto ML, Carmo EH, Costa MC. Prevalência e fatores associados às geo-helmintíases em crianças residentes em municípios com baixo IDH no Norte e Nordeste brasileiros. Cad Saúde Pública. 2010;26:143–52. doi: 10.1590/s0102-311x2010000100015. [DOI] [PubMed] [Google Scholar]
- 14.Hung CC, Chang SY, Ji DD. Entamoeba histolytica infection in men who have sex with men. Lancet Infec Dis. 2012;12:729–36. doi: 10.1016/S1473-3099(12)70147-0. [DOI] [PubMed] [Google Scholar]
- 15.Chaves EM, Vazquez L, Lopes K, Flores J, Oliveira L, Rizzi L, et al. Levantamento de Protozoonoses e Verminoses nas sete creches municipais de Uruguaiana, Rio Grande do Sul – Brasil. Rev Bras An Clinc. 2006;38:39–41. [Google Scholar]
- 16.Macedo HW, Gonçalves AM, Almeida CB, Dias LV, Muniz MF. Infecção por Blastocystis hominis e Entamoeba histolytica/Entamoeba dispar em pacientes atendidos em um hospital localizado em Niterói, Rio De Janeiro. Rev Patol Trop. 2010;39:56–62. [Google Scholar]
- 17.Eymael D, Schuh GM, Tavares RG. Padronização do diagnóstico de Blastocystis hominis por diferentes técnicas de coloração. Rev Soc Bras Med Trop. 2010;43:309–12. doi: 10.1590/s0037-86822010000300019. [DOI] [PubMed] [Google Scholar]
- 18.Zonta ML, Navone GT, Oyhenart EE. Parasitic infection intestinales en niños de edad preescolar y escolar: situación actual en poblaciones urbanas, periurbanas y rurales en Brandsen, Buenos Aires, Argentina. Parasitol Latinoam. 2007;6:54–60. [Google Scholar]
- 19.Al-Mohammed HI, Amin TT, Aboulmagd E, Hablus HR, Zaza BO. Prevalence of intestinal parasitic infections and its relationship with socio-demographics and hygienic habits among male primary schoolchildren in Al-Ahsa, Saudi Arabia. Asian Pac J Trop Med. 2010;3:906–12. [Google Scholar]
- 20.Östan I, Kilimcioğlu AA, Girginkardeşler N, Özyurt BC, Limoncu ME, Ok ÜZ. Health inequities: lower socio-economic conditions and higher incidences of intestinal parasites. BMC Public Health. 2007;7:342. doi: 10.1186/1471-2458-7-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quihui L, Valencia ME, Crompton DW, Phillips S, Hagan P, Morales G, et al. Role of the employment status and education of mothers in the prevalence of intestinal parasitic infections in Mexican rural schoolchildren. BMC Public Health. 2006;6:225–33. doi: 10.1186/1471-2458-6-225. [DOI] [PMC free article] [PubMed] [Google Scholar]