Abstract
Tuberculosis in the United Kingdom and other high-income countries is primarily a disease of the foreign-born arising from the synergy of migration from high TB burden regions and the reactivation of remotely acquired latent TB infection. UK immigrant screening policy primarily aims to identify active, rather than latent, TB although mounting evidence indicates that implementing latent TB screening for new entrants from intermediate and high incidence countries could cost-effectively reduce TB incidence in the UK.
Introduction
While much of the global tuberculosis (TB) burden is concentrated in low-income, high-burden countries, patterns of international migration have ensured that TB remains high on the public health agenda of most high-income, low-burden countries. Over the last three decades, historic reductions in UK TB incidence have reversed and TB is again a public health concern. Between 1998 and 2009 alone, TB notifications surged by almost 50% to 9040 cases – among the largest increases witnessed in all high-income countries. However this aggregate figure masks an important disparity because the increase is exclusively among the foreign-born, in whom notifications have risen by 98%. Foreign-born individuals now account for over 70% of UK TB notifications, have a 22-fold higher TB incidence (89 cases/100 000 p.a.) than UK-born individuals (4 cases/100 000 p.a.) and have an incidence rate which is particularly high in the initial years after migration.1
Underpinning this disproportionate burden is the synergy between migration from high TB burden nations in sub-Saharan Africa and the Indian subcontinent and the reactivation of latent tuberculosis infection (LTBI) acquired prior to migration. This has reignited debate about how best to screen immigrants for TB, with specific issues of import for policy-makers being: whether to screen for active TB or latent TB infection (LTBI) (or indeed both); which immigrant groups to screen for LTBI; how to screen for LTBI and in which healthcare setting to undertake screening.
Methods of new-entrant immigrant screening in the UK have essentially remained unchanged for over 40 years. UK policy, based around port-of-entry screening, was conceived in response to concerns about the high TB incidence in immigrants. Its primary aim was, and continues to be, to identify active, infectious, TB in new entrants at the time of their arrival to the UK with chest radiographs. However, given the low yield of active TB, the high and increasing proportion of extrapulmonary disease in immigrants (where chest radiographs would be unhelpful) and the fact that TB in the foreign-born population results largely from reactivation of LTBI, it is time critically to re-evaluate this policy.
Current screening and discussion
Since 2006 the National Institute of Health and Clinic Excellence (NICE) recommended that in addition to screening for active disease, TB services should identify LTBI in a very select subset of new entrants. Those aged <16 years from countries with TB incidence >40 cases/100 000 and those aged 16–35 years from countries with TB incidence >500 cases/100 000 or sub-Saharan Africa.2,3
Despite this national guidance having been in place for >5 years, it was not known, until recently, how screening was actually being undertaken at the front-line. Contemporary data, encompassing the previous 2006 guidelines, from a national evaluation of over 90% of primary care organisations in the UK found that screening for active, rather than latent, TB was prioritised. Remarkably, screening for LTBI was inversely related to regional TB burden with high-burden primary care organisations significantly less likely to attempt to follow-up and screen new entrants with normal chest-radiography for LTBI despite these areas having the highest proportion of immigrants from high-burden countries.4 In addition, those primary care organisations which screened for LTBI considerably deviated from NICE guidance – both in terms of which new-entrant subgroups were screened and which tools and algorithms were used.4 The heterogeneity in screening practices highlighted by this national survey probably reflected a pragmatic response by clinicians to the lack of empirical data on immigrant screening, limited service capacity and logistical issues in screening immigrants.
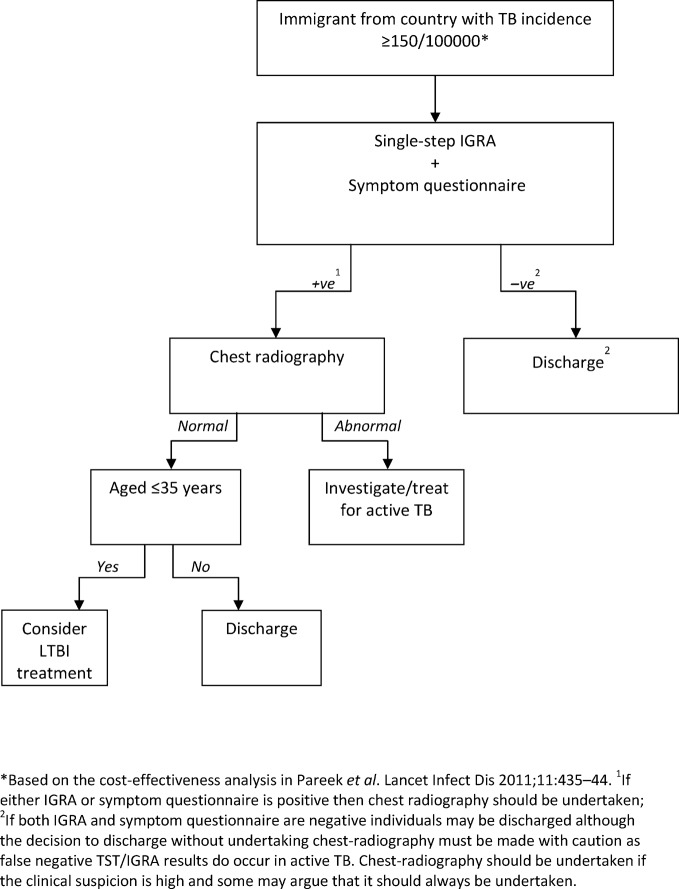
One of the key areas where evidence is lacking is which immigrant groups to screen. This was recently addressed by a large multi-centre study of immigrant screening in the UK which provided robust estimates of LTBI prevalence (stratified by TB incidence in countries of origin), calculated the yields when screening at different thresholds and, perhaps most importantly, computed the cost-effectiveness of LTBI screening (see Fig. 1).5 The conclusions of this analysis were that screening as per the 2006 NICE guidelines would miss 70% of imported LTBI and therefore immigrant screening would be most cost-effectively implemented by revising the screening threshold downwards to an intermediate incidence threshold of 150-250/100000 which would identify 90% of immigrants with LTBI, thereby preventing substantial numbers of future active TB cases.5
Figure 1.
Proposed algorithm for cost-effective immigrant screening for active and latent TB
In 2011 NICE published revised guidelines that actually dropped the threshold further to 40/100 000; however, it remains unclear whether this guidance will be acted upon. In view of limited service capacity and the huge logistical and cost implications of screening all new entrants from countries with TB incidence >40/100 000, TB services may instead use a higher threshold which would reduce the number of individuals eligible to be screened. Moreover, the 2011 guidelines were limited by the lack of real-life empirical data on screening outcomes using different testing modalities (TST vs. TST plus confirmatory IGRA vs. single-step IGRA), whether to continue with port-of-entry chest radiographs and where best to physically locate immigrant screening. This last issue is particularly important. Implementing a system that caters for the mobility of newentrants when they first arrive in the UK remains a challenge. Primary-care based screening, which additionally allows integration with wider migrant health programmes such as maternal and child health, and screening for treatable blood-borne viruses (including hepatitis B, hepatitis C and HIV), may be an effective alternative but timely registration of immigrants with primary care is unfortunately far from universal.
Conclusion
Important caveats which will alter the cost-effectiveness of screening must be borne in mind, including the need for better quality data on the rates of progression from LTBI to active TB in immigrants and the proportion of immigrants actually accepting, and then completing, a 3-month course of chemoprophylaxis.
In conclusion, although the evidence-base supporting the cost-effectiveness and potential benefit of immigrant screening for LTBI has grown in recent years, for screening significantly to impact on TB control in the UK there is a clear and present need for an up-to-date evidence-based co-ordinated national strategy predicated on close cooperation between the UK Department of Health, UK Border Agency, primary care organisations and TB services.
Disclosure
Professor Lalvani is inventor for several patents underpinning T cell-based diagnosis. The Lalvani ELISpot was commercialised by an Oxford University spin-out company (T-SPOT.TB®, Oxford Immunotec Ltd, Abingdon, UK) in which Oxford University and Professor Lalvani have a minority share of equity and royalty enitlements. MP has no conflict of interest.
References
- 1.Health Protection Agency. London: Health Protection Agency Centre for Infections; 2010. Tuberculosis in the UK: Annual report on tuberculosis surveillance and control in the UK 2010. [Google Scholar]
- 2.National Collaborating Centre for Chronic Conditions. London: Royal College of Physicians; 2006. Tuberculosis: clinical diagnosis and management of tuberculosis, and measures for its prevention and control. [PubMed] [Google Scholar]
- 3.National Collaborating Centre for Chronic Conditions. London: Royal College of Physicians; 2011. Tuberculosis: clinical diagnosis and management of tuberculosis, and measures for its prevention and control. [PubMed] [Google Scholar]
- 4.Pareek M, Abubakar I, White PJ, Garnett GP, Lalvani A. TB screening of migrants to low TB burden nations: insights from evaluation of UK practice. Eur Respir J. 2011;37:1175–82. doi: 10.1183/09031936.00105810. [DOI] [PubMed] [Google Scholar]
- 5.Pareek M, Watson JP, Ormerod LP, Kon OM, Woltmann G, White PJ, et al. Screening of immigrants in the UK for imported latent tuberculosis: a multicentre cohort study and cost-effectiveness analysis. Lancet Infect Dis. 2011;11(6):435–44. doi: 10.1016/S1473-3099(11)70069-X. [DOI] [PMC free article] [PubMed] [Google Scholar]