Abstract
The antimicrobials crisis is a ticking time bomb which could lead to millions of people dying from untreatable infections. With the worsening trends of antimicrobial resistance, we are heading towards a pre-antibiotic era. Thus, there is a need for newer and more powerful antibiotic agents. The search for new antibiotic compounds originating from natural resources is a promising research area. Animals living in germ-infested environments are a potent source of antimicrobials. Under polluted milieus, organisms such as cockroaches encounter different types of bacteria, including superbugs. Such creatures survive the onslaught of superbugs and are able to ward off disease by producing antimicrobial substances which show potent activity in the nervous system. We hope that the discovery of antimicrobial activity in the cockroach brain will stimulate research in finding antimicrobials from unusual sources, and has potential for the development of novel antibiotics. Nevertheless, intensive research in the next few years will be required to approach or realize these expectations.
Keywords: Infectious diseases, Antimicrobials, Natural products, Insects
Introduction
Infectious diseases remain a significant threat to human health, contributing to more than 14 million annual deaths, more than half of them occurring in children,1 even with advances in antimicrobial chemotherapy. For example, tuberculosis caused by Mycobacterium tuberculosis alone contributes to approximately 1.6 million deaths per year.1 Other bacteria causing acute respiratory infections, food-borne illnesses, cutaneous and central nervous system infections remain a major threat to human health. In the recent years, the burden of infectious diseases has exacerbated with the emergence of antimicrobial resistance and lessening efficacy of the available antimicrobial compounds.2,3 For example, in 1990, almost all cholera isolates in New Delhi (India) were sensitive to furazolidone, ampicillin, co-trimoxazole, and nalidixic acid. In 2000, these drugs became largely obsolete in the treatment of cholera. Today, vancomycin-resistant Enterococcus, methicillin-resistant Staphylococcus aureus (MRSA), Pseudomonas aeruginosa, Acinetobacter baumannii, Klebsiella pneumonia, and Escherichia coli pose a serious threat to public health with economic and social implications. Thus new and novel antimicrobial agents are urgently needed to meet the challenge posed by the emergence of multiple drug-resistant microorganisms. The search for new antibiotic compounds originating from unusual natural resources will generate potentially useful leads in the identification of new drugs. For example, the recent discovery of potent antimicrobial properties in brain lysates of cockroaches and locusts has intrigued the scientific community and generated significant public interest (http://www.radionz.co.nz/national/programmes/thiswayup/audio/2492112/cockroach-healing; http://economictimes.indiatimes.com/news/news-by-industry/et-cetera/cockroach-scientist-seeks-indian-help/articleshow/8542680.cms; http://www.sciencenews.org/index/generic/activity/view/id/63286/title/Cockroach_brains%2C_coming_to_a_pharmacy_near_you; http://www.tcetoday.com/tcetoday/NewsDetail.aspx?nid = 13129; http://www.futurity.org/health-medicine/unlikely-source-of-antibiotics-cockroaches/; http://www.healthzone.ca/health/newsfeatures/article/860802-mashed-up-cockroach-brains-kill-e-coli-study-finds; http://news.nationalgeographic.com/news/2010/09/100909-cockroach-brains-mrsa-ecoli-antibiotics-science-health/; http://www.bbc.co.uk/news/science-environment-11182437; http://blogs.discovermagazine.com/80beats/2010/09/10/cockroaches-have-super-antibiotics-in-their-brains-we-must-steal-them/; http://www.newscientist.com/article/dn19404-locust-brains-could-thwart-superbug-plagues.html;). Such novel hypothesis will pave the way in our ‘war on terror cells’, i.e. infectious agents.
Antimicrobial Chemotherapy: The Historical Perspective
As long ago as 1550 BC, the Egyptians were using a mixture of lard, honey, and lint as an ointment for dressing wounds. Wine and vinegar have been used to treat infected wounds since the time of Hippocrates. Although oblivious to the scientific basis of these therapies at the time, modern science has subsequently confirmed the antibacterial activity of many of these substances. Honey kills bacterial cells by drawing water out of them and via the production of hydrogen peroxide resulting from the activity of the enzyme glucose oxidase on glucose and oxygen.4 The antibacterial activity of wine cannot be fully attributed to its relatively low alcohol content. Chemical analysis of wine has unearthed the antibacterial compound, malvoside5 and it is now known that the acidity of vinegar is responsible for its antiseptic qualities.
The ‘germ theory’ of disease linking bacteria and other microbes to the causation of numerous human diseases was widely accepted by the late nineteenth century. This enabled the search for substances specifically targeted against disease-causing microbes to begin in earnest. In 1928, the work of Alexander Fleming paved the way for the golden era of antibiotic discovery by demonstrating antibacterial properties of Penicillium notatum.6 During the late 1930s and early 1940s, Florey and Chain enabled penicillin to enter clinical use. In 1935, Gerhard Domagk demonstrated that the dye prontosil red could cure Streptococcal-infected mice.7 This dye proved to be the precursor for a new class of antibacterial drugs called the sulphonamides that are widely used today. Waksman8 discovered streptomycin from a soil microbe in 1943, while cephalosporins were identified by Florey’s research group.
The golden age of antibiotic discovery stretched from the 1940s through the 1970s when much of the ‘low hanging fruit’ was picked. During the 1960s, semi-synthetic chemically modified derivatives of these various classes of antibiotics were produced resulting in a wave of second generation antibiotics.9 A semi-synthetic derivative of penicillin called methicillin was produced specifically to overcome rapidly spreading bacterial resistance to penicillin. Methicillin was hailed as a major victory in the fight against bacterial penicillin resistance. Unfortunately, this euphoria was short-lived as bacterial resistance to methicillin has now emerged.10 Ampicillin and amoxicillin are other chemical modifications of the basic penicillin structure developed during this era and are widely used today.11 New antibiotics were introduced in the 1980s and 1990s but at a much lower rate.
Unfortunately, although new antimicrobial drugs were discovered, our ability to commercialize targeted microbial therapy was limited. Instead, broad spectrum antibiotics were overused (blind therapy) and this increased the selective pressure on bacteria to become resistant to these drugs. Extensive use of antibiotics in the farming industry also led to overexposure of bacteria to these drugs and the development of resistance.12 Poor infection control measures, highly immune-compromised patients, and rapid/frequent air travel further exacerbates the problem.13
Clear and Present Danger
The discovery of antibiotics led to significant optimism of eradicating infectious diseases. In 1969, the US Surgeon General, William H. Stewart, proclaimed to congress ‘The time has come to close the book on infectious disease’. However, infectious diseases remain the second leading cause of death globally.1 Despite the early successes in antibiotic discovery, only three new antibacterial classes have been licensed since 1970 (mupirocin in 1985, linezolid in 2000, and daptomycin in 2003).14 Over the last 20 years, there has been a significant decline in the number of new approved antibiotics (Fig. 1). Despite the urgent need for new antibacterial drugs with novel mechanisms of action, many pharmaceutical companies have greatly reduced or completely ceased their antimicrobial drug discovery research and development.15 It is extremely expensive to develop and establish the safety and efficacy of a new antibiotic and there is no guarantee that a drug will be approved even after a huge investment of time and money. Of particular concern is the emergence of multidrug resistant bacteria such as MRSA which kills more people in the USA than HIV/AIDS and TB combined.16 Some strains of MDR Gram-negative bacilli like Pseudomonas aeruginosa and Acinetobacter baumannii are now resistant to all known antibiotics.17 Apart from the problem of acquired and intrinsic resistance among bacteria, new antibiotics are continually required to combat the threat of newly recognized infectious diseases (30 were described in the 1980s and 1990s alone) and to provide alternatives to some of the unacceptably toxic antibiotics that are currently available.17 Most currently available antibacterial drugs were discovered between 1940 and 1980 using traditional approaches, such as the screening of soil microbes, which have now become saturated.18 Most of the newer antibacterial drugs have arisen from chemical modification of existing antibiotic structures. Efforts to create new drugs using existing antibiotic scaffolds are challenging because these semi-synthetic derivatives are often not able to penetrate the bacterial cell wall adequately. More innovative, non-traditional strategies are therefore required in order to provide the urgently needed next generation of antimicrobial drugs.
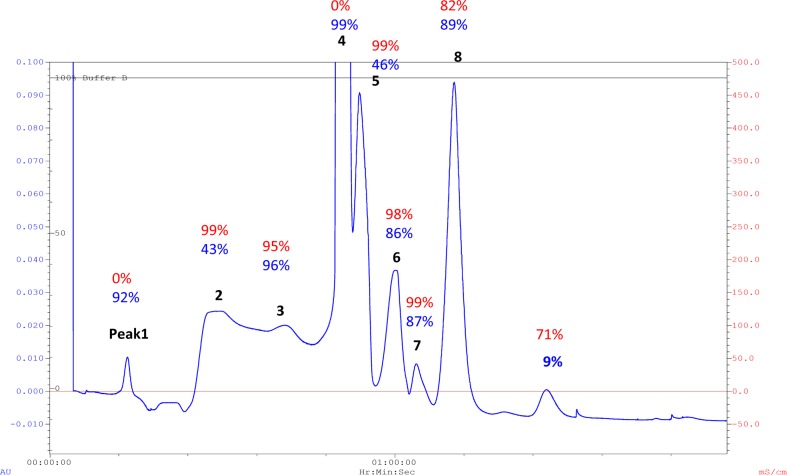
Figure 1.
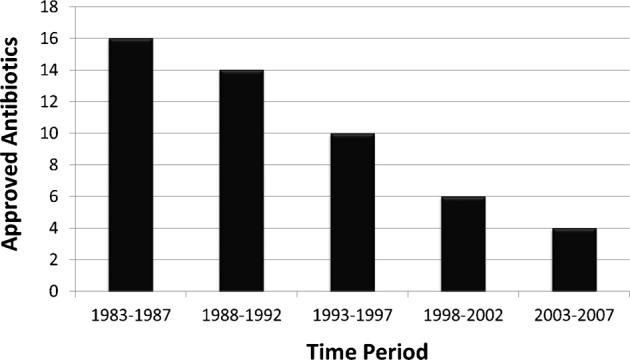
Decline in new antibiotics approved for clinical use in humans (numbers taken from Demain, 2009).
Natural Products as Drug Leads
The search for new antimicrobial compounds from natural sources is an important research area. Natural products have led to numerous medical breakthroughs and life saving drugs particularly in the treatment of infectious diseases, cancer, hyper-cholesterolaemia, and immune dysfunction. During the period 2003–2008, 21 drugs originating from natural product leads (mainly from actinomycete, bacterial, or fungal sources) were approved for marketing19 and there are 36 drug candidates from natural products in the pipeline. The unique ‘chemical space’ that is occupied by natural chemicals is largely responsible for the success\ of these compounds as drug candidates. Secondary metabolites from plants, microbes and, to a lesser extent, marine invertebrates and their associated microbes have provided the main sources of natural product based drugs. Advances in high-throughput screening technology with better biological screening together with improved chromatography and analytical techniques have significantly speeded up the process of arriving at purified active compounds of known chemical structure for synthetic compounds, but shown limited success for crude extracts with potential antimicrobial activity. For crude extracts with antimicrobial activity, structures can be determined rapidly using hyphenated instrumental techniques.
Natural products are produced by living cells either as primary metabolites, which are involved in normal growth, development, and reproduction, or as secondary metabolites, which are not directly involved in these processes but usually have an important ecological function. Most drug leads originate from secondary metabolites from plants, fungi, bacteria, and marine organisms. These natural product molecules are generally architecturally complex and constitute over half of all clinically used drugs.20 Organisms produce these molecules for their own use and so can be deficient in certain pharmaceutical properties applicable to humans. Structural modifications are sometimes performed on these molecules to improve physicochemical properties to favourably alter absorption, distribution, metabolism, and excretion in humans. However, many of these natural products are suitable for clinically useful drugs without any modification to the molecular structure. Natural products cover a much wider and larger chemical space than that covered by synthetic chemicals. Natural products possess many chiral centres, ring fusions, and functional groups resulting in better affinity and specificity towards biological targets that is generally lacking in synthetic drugs which are usually architecturally flat in comparison. Natural products often have unexpectedly beneficial properties with regard to cellular penetration, absorption, and solubility that are not well understood. Presumably, these beneficial properties of natural products as drug candidates are a consequence of co-evolution with cellular proteins over many millennia.21
Invertebrates (e.g. Cockroach and Locusts) as Potential Source of Antimicrobials
The recent development in research on multi-drug-resistant bacteria suggests that animals living in unsanitary and unhygienic conditions have developed ways of protecting themselves against pathogenic microorganisms.22,23 Such animals could be a good source of antimicrobials. Insects such as cockroaches represent a plentiful and untapped potential source of new antimicrobial drugs prompting us to investigate the antibacterial activity of their various tissues.24 Our studies have shown that cockroach and locust brain tissues have powerful antibiotic properties and may serve as potential sources of antimicrobials in the future.23,24 They often inhabit environment niches that present a significant threat in terms of microbial infection and have evolved defences to counter this threat. It was interesting that brain lysates but not muscle, fat body or haemolymph of cockroaches (Periplaneta americana) and locusts (Locusta migratoria or Schistocerca gregaria) showed remarkable antimicrobial activity killing more than 90% of different bacteria including Staphylococcus aureus, MRSA, S. epidermidis, and a neuropathogenic Escherichia coli K1 (Fig. 2). What is more remarkable is that the antimicrobial activity of the brain lysates was retained even when only 5 μg of lysates was tested against 1×106 cfu (Fig. 3). The bactericidal activity was heat-resistant, but SDS-labile and pronase-sensitive indicating its proteinaceous nature. However, it is noteworthy that glycopeptide molecules (e.g. vancomycin) and lipopeptide molecules (e.g. daptomycin) are currently used as antibiotics clinically and there are several antimicrobial compounds undergoing development in phase 2 or later clinical studies that are lipoglycopeptides in chemical nature.25 Insect brain lysates had no and/or minimal cytotoxic effects on human brain microvascular endothelial cell cytotoxicity. The potent antimicrobial activity of cockroach or locust brain lysates is not surprising as their nervous system needs to be well-protected because if the nervous system goes down, the insect dies, but they can suffer damage to their peripheral structures. Additionally, the nervous system has limited cell-mediated immunity; thus, it was hypothesized that the nervous system possesses molecules with powerful antimicrobial properties.
Figure 2.
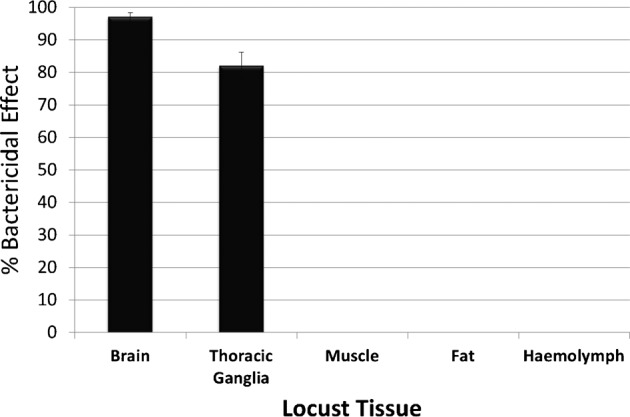
Insect (locust) tissue samples were collected into 500 μl of sterile water in batches of samples obtained from 30 insects. The samples were subjected to four cycles of freeze–thawing by placing at −20°C followed by 37°C in order to cause cellular disruption and lysis. The samples were then homogenized aseptically with a tissue grinder, prior to centrifugation at 10 000g for 10 minutes. The supernatant (crude extract) was then aspirated and stored at −20°C until needed for antibacterial bioassay testing. Approximately 1×106 bacterial cells (MRSA) were mixed with 80 μg of crude extract and incubated for 2 hours at 37°C. Control samples included bacteria incubated without lysates. Percentage bactericidal activity was calculated using the formula: % Bactericidal activity = 100−(cfu crude extract/cfu control×100). Note that locust muscle, fat, and haemolymph exhibited no bactericidal activity against MRSA. In contrast, locust brain and thoracic ganglia crude extracts showed high bactericidal activity against MRSA. Similar findings were observed against neuropathogenic E. coli K1. Values shown are the mean of several experiments with error bars showing ±SE.
Figure 3.
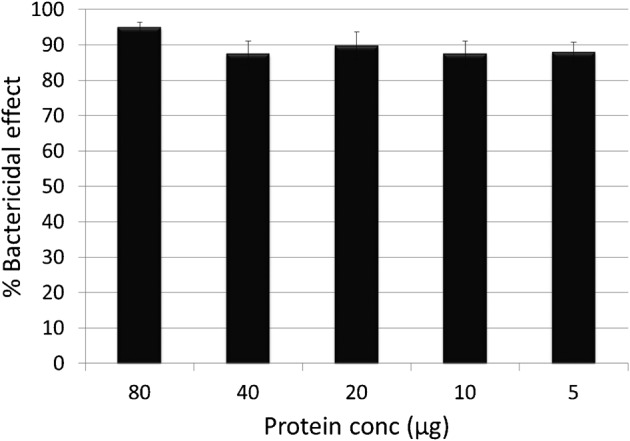
Insect (locust) ganglia antibacterial activity against MRSA is potent. Decreasing amounts of brain lysates were used ranging from 80 to 5 μg of total protein with no significant loss of antibacterial activity against MRSA.
The size exclusion filters of 30, 10, and 3 kDa pore size showed that the majority of antibacterial activity is present in the 10-kDa eluate (Fig. 4). Fast protein liquid chromatography (FPLC) separation of brain lysates using a size exclusion column provided evidence of multiple antibacterial molecules (Fig. 5). Solid phase extraction was used to fractionate lysates into lipophilic and hydrophilic components. Subsequent antibacterial bioassay testing of these lipophilic and hydrophilic fractions revealed that antimicrobial activity resides in the lipophilic fractions with none detected in the hydrophilic fractions (Fig. 6). By combining size-exclusion spin columns and FPLC, eight different molecules in the region of 3–10 kDa in molecular mass in brain lysates were identified that were toxic both to MRSA and neuropathogenic E. coli K1. Of interest, 50 neuropeptides have been characterized biochemically in locusts.26 However, the biological significance and in vivo function of most of these neuropeptides remains unknown. Some of these are likely to be novel members of known peptide families, whereas others could represent previously unknown peptide families. It is noteworthy that to date none of these neuropeptides have been identified as belonging to the rapidly expanding antimicrobial peptide (AMP) family of molecules. Large neuropeptide precursor molecules such as proenkephalin27 and prodermaseptin28 are known to be processed into smaller peptides, some of which have antibacterial activity. These precursors have similar N-terminal preprosequences followed by variable C-terminal sequences that produce AMPs. Some of these peptides are 24–34 residues long and form stable amphipathic alpha-helices, some are disulphide linked peptides 20–46 amino-acid long, and others are very hydrophobic and only 10–13 residues long representing the smallest antimicrobial peptides currently known.29 The processing of proenkephalin releases these AMPs, peptide B, and enkelytin, which are in turn associated with immune related opioid peptides. These opioid peptides stimulate immunocyte chemotaxis and phagocytosis, as well as the production of other immunostimulatory factors. The antibacterial proenkephalin fragment released during this process can attack bacteria immediately, while the opioid peptides immunostimulatory responses take time to manifest. The relative lack of genomic sequence hampers peptide identification. Precise chemical identification of the antibacterial molecules and subsequent use of purified metabolites rather than the complex mixture of biomolecules present in crude extracts will provide more meaningful data. Work is currently underway to characterize further the antibacterial properties of insect brain lysates and to investigate the spectrum of activity against a panel of wild-type and resistant human bacterial pathogens. It is hoped that these molecules could eventually be developed into treatments for bacterial infections that are increasingly resistant to current drugs. These new antibiotics could potentially provide alternatives to currently available drugs that may be effective but have serious and unwanted side effects.
Figure 4.
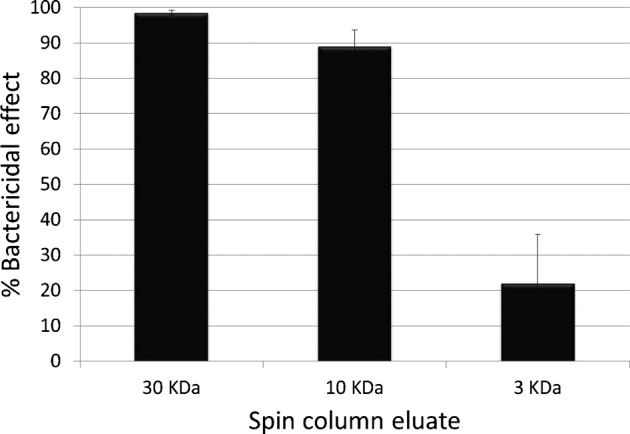
Locust brain lysate were passed through 30, 10, and 3 kDa size exclusion spin columns and antibacterial activity of eluate and retentate was tested against MRSA. The 30 kDa eluate retained full bactericidal activity (98%) comparable to whole crude lysate. The 10 kDa eluate showed a small reduction in bactericidal activity (89%), whereas the bactericidal activity of the 3 kDa eluate was significantly reduced to 22% suggesting the presence of more than one antibacterial substance ranging from 30 to 3 kDa.
Figure 5.
FPLC size exclusion chromatograph of locust brain lysate 10 kDa eluate. Nine distinct peaks were obtained by UV absorbance (280 nm). Fractions associated with each peak were tested for antibacterial activity against MRSA (shown in red) and E. coli (shown in blue).
Figure 6.
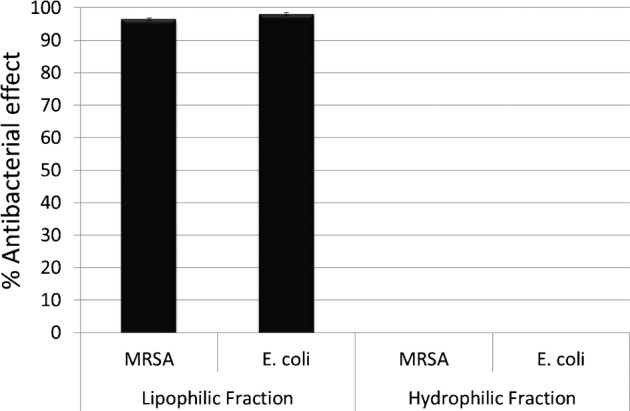
C-18 reverse phase chromatograph on locust brain extracts to obtain lipophilic fractions (acetonitrile eluate) and hydrophilic fractions (water eluate). Both lipophilic and hydrophobic fractions were tested for bactericidal activity against MRSA and E. coli with all antibacterial activity subsequently detected in the lipophilic fraction and none detected in the hydrophilic fraction. Control samples were included consisting of solvent only (acetonitrile, water) passed through the C-18 column and treated in an identical manner as test samples showed no antibacterial activity associated with the column or downstream sample processing.
Overall, natural products are often superior to synthetic products as antibacterial drugs because they display optimal cellular penetration and privileged structures allowing interaction with the finite structural spaces in protein folds. Since the pharmaceutical industry has largely lost interest in developing antimicrobial drugs, government-sponsored research in universities and small biotech companies must endeavour to develop the next generation of these drugs. The discovery of antimicrobial activity in cockroach/locust brains will stimulate research in finding novel antimicrobials from rare sources in a hypothesis-driven manner, and explore their therapeutic potential as anti-infective drug candidates.
Acknowledgments
The authors are grateful to Mary Lightfoot and Graham Goldsworthy (Birkbeck, University of London, UK) for providing guidance and skilled technical assistance and to Helen Atkins (Defence Science and Technology Laboratory, Salisbury, UK) for providing partial funds. Additionally, we are thankful to the University of Nottingham and the Aga Khan University for financial support and resources to carry out this work.
References
- 1.World Health Organization. Mortality Report. Geneva: WHO; 2002. Available from: http://www.who.org (Accessed 14 December 2011) [Google Scholar]
- 2.Alanis AJ. Resistance to antibiotics: are we in the post-antibiotic era? Arch Med Res. 2005;36:697–705. doi: 10.1016/j.arcmed.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Nordmann P, Naas T, Fortineau N, Poirel L. Superbugs in the coming new decade; multidrug resistance and prospects for treatment of Staphylococcus aureus, Enterococcus spp. and Pseudomonas aeruginosa in 2010. Curr Opin Microbiol. 2010;10:436–40. doi: 10.1016/j.mib.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Wahdan HA. Causes of the antimicrobial activity of honey. Infection. 1998;26:26–31. doi: 10.1007/BF02768748. [DOI] [PubMed] [Google Scholar]
- 5.Hart GD. Asclepius: the god of medicine. London: The Royal Society of Medicine Press; 2000. [Google Scholar]
- 6.Birch B, Fleming A. Farmington Hills, MI: Greenhaven Press; 2002. Alexander Fleming: pioneer with antibiotics. [Google Scholar]
- 7.Bankston J. Gerhard Domagk and the discovery of sulfa. Hockessin, DE: Mitchell Lane Publishers; 2002. [Google Scholar]
- 8.Waksman SA. My life with the microbes. New York: Simon and Schuster; 1954. [Google Scholar]
- 9.Fayerman JT. Second-generation products: antibiotics. Bioprocess Technol. 1991;13:415–24. [PubMed] [Google Scholar]
- 10.Goto H, Shimada K, Ikemoto H, Oguri T. Study Group on Antimicrobial Susceptibility of Pathogens Isolated from Respiratory Infections. Antimicrobial susceptibility of pathogens isolated from more than 10,000 patients with infectious respiratory diseases: a 25-year longitudinal study. J Infect Chemother. 2009;15:347–60. doi: 10.1007/s10156-009-0719-3. [DOI] [PubMed] [Google Scholar]
- 11.Drawz SM, Bonomo RA. Three decades of beta-lactamase inhibitors. Clin Microbiol Rev. 2010;23:160–201. doi: 10.1128/CMR.00037-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Refsdal AO. To treat or not to treat: a proper use of hormones and antibiotics. Anim Reprod Sci. 2000;60–61:109–19. doi: 10.1016/s0378-4320(00)00094-4. [DOI] [PubMed] [Google Scholar]
- 13.Gould IM. The epidemiology of antibiotic resistance. Int J Antimicrob Agents. 2008;1:2–9. doi: 10.1016/j.ijantimicag.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 14.Demain AL. Antibiotics: natural products essential to human health. Med Res Rev. 2009;29:821–42. doi: 10.1002/med.20154. [DOI] [PubMed] [Google Scholar]
- 15.Butler MS. Natural products to drugs: natural product-derived compounds in clinical trials. Nat Prod Rep. 2008;25:475–516. doi: 10.1039/b514294f. [DOI] [PubMed] [Google Scholar]
- 16.Pantosi A, Venditti M. What is MRSA? Eur Respir J. 2009;34:1190–6. doi: 10.1183/09031936.00007709. [DOI] [PubMed] [Google Scholar]
- 17.Giamarellou H, Poulakou G. Multidrug-resistant Gram-negative infections: what are the treatment options? Drugs. 2009;69:1879–901. doi: 10.2165/11315690-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 18.Devasahayam G, Scheld WM, Hoffman PS. Newer antibacterial drugs for a new century. Expert Opin Investig Drugs. 2010;19:215–34. doi: 10.1517/13543780903505092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Butler MS, Buss AD. Natural products — the future scaffolds for novel antibiotics? Biochem Pharmacol. 2006;71:919–29. doi: 10.1016/j.bcp.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 20.Newman DJ. Natural products as leads to potential drugs: an old process or the new hope for drug discovery? J Med Chem. 2008;51:2589–99. doi: 10.1021/jm0704090. [DOI] [PubMed] [Google Scholar]
- 21.Dobson CM. Chemical space and biology. Nature. 2004;432:824–8. doi: 10.1038/nature03192. [DOI] [PubMed] [Google Scholar]
- 22.Fischbach MA, Walsh CT. Antibiotics for emerging pathogens. Science. 2009;325:1089–93. doi: 10.1126/science.1176667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee S, Atkins H, Duce I, Khan NA. Cockroach and locust: physicians’ answer to infectious diseases. Int J Antimicrob Agents. 2011;37:279–80. doi: 10.1016/j.ijantimicag.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Khan NA, Osman K, Goldsworthy GJ. Lysates of locusta migratoria brain exhibit potent broad-spectrum antibacterial activity. J Antimicrob Chemother. 2008;62:634–5. doi: 10.1093/jac/dkn239. [DOI] [PubMed] [Google Scholar]
- 25.Talbot GH, Bradley J, Edwards JE, Jr, Gilbert D, Scheld M, Bartlett JG. Bad bugs need drugs: an update on the development pipeline from the antimicrobial availability task force of the infectious diseases society of America. Clin Infect Dis. 2006;42:657–68. doi: 10.1086/499819. [DOI] [PubMed] [Google Scholar]
- 26.Clynen E, Schoots L. Peptidomic survey of the locust neuroendocrine system. Insect Biochem Mol Biol. 2009;39:491–507. doi: 10.1016/j.ibmb.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 27.Metz-Boutigue MH, Goumon Y, Strub JM, Lugardon K, Aunis D. Antimicrobial chromogranins and proenkephalin-A-derived peptides: antibacterial and antifungal activities of chromogranins and proenkephalin-A-derived peptides. Ann NY Acad Sci. 2003;992:168–78. doi: 10.1111/j.1749-6632.2003.tb03147.x. [DOI] [PubMed] [Google Scholar]
- 28.Amiche M, Seon AA, Pierre TN, Nicolas P. The dermaseptin precursors: a protein family with a common preproregion and a variable C-terminal antimicrobial domain. FEBS Lett. 1999;456:352–6. doi: 10.1016/s0014-5793(99)00964-3. [DOI] [PubMed] [Google Scholar]
- 29.Salzet M. Vertebrate innate immunity resembles a mosaic of invertebrate immune responses. Trends Immunol. 2001;22:285–8. doi: 10.1016/s1471-4906(01)01895-6. [DOI] [PubMed] [Google Scholar]