Abstract
Isolated tuberculous liver abscess (TLA) without active pulmonary or miliary tuberculosis, or other clinical evidence of tuberculosis, is distinctly rare and only few cases have been reported in the literature. We report two cases of isolated TLA in immunocompetent children, treated successfully by percutaneous aspiration followed by systemic antituberculous drugs.
Keywords: Tuberculous liver abscess, Children, Immunocompetent
Introduction
Tuberculous liver abscess (TLA) is usually associated with an immune-compromised state, with a focus of infection in the lungs, gastrointestinal tract, or as a part of congenital or miliary tuberculosis.1 Isolated TLA is a rare entity and only few cases have been reported in the literature.2 Here, we report two cases of isolated TLA in the pediatric age group, which were successfully treated with antituberculous drugs.
Case 1
An eight-year-old male child presented with high-grade fever and non-radiating pain in the right upper abdomen for 15 days. He was immunized and a BCG scar was present. There was no history of cough or weight loss. The patient had a history of contact with tuberculosis as the patient’s mother had been treated for tuberculous pleural effusion 1 year earlier. On examination there was no jaundice or lymphadenopathy. The weight and height percentile of the patient were 50th and 65th, respectively, as per WHO growth charts. The patient’s temperature was 39.8°C, pulse rate 108/min, respiratory rate 20/min, and blood pressure 118/64 mm Hg. Systemic examination revealed tender hepatomegaly 4 cm below the subcostal margin. There was no splenomegaly or ascites. The rest of the systemic examination was unremarkable.
Investigations revealed a hemoglobin content of 12.8 g%, total leukocyte count of 22 000/mm3 (neutrophils 72%, lymphocytes 25%, and monocytes 3%), and ESR of 22 mm fall in the first hour. Total bilirubin was 0.8 mg/dl, alanine transaminase (ALT) 35 U/l, aspartate transaminase (AST) 42 U/L (normal ALT and AST<15–40), alkaline phosphatase 122 IU/l (50–130), and total serum protein 6.8 g/l (albumin 4.0 g/l and globulin 2.8 g/l). Renal function tests, prothrombin time, and aPTT were normal. Blood culture and urine culture were sterile. A Mantoux test was positive and a HIV test was non-reactive. Serum immunoglobulins and components of complement, C3 and C4, were normal and there was normal nitroblue-tetrazolium (NBT) reduction. Chest radiograph was normal. Ultrasonography (USG) of the abdomen revealed a 350-ml, partially liquefied abscess in the right lobe of the liver (Fig. 1). USG-guided aspiration of the abscess revealed yellow colored pus. The patient was given vancomycin, ceftriaxone, and metronidazole empirically. Gram stain and culture of the aspirate did not reveal any bacteria and analysis for amoebic trophozoites and serology was negative. Despite 10 days of antibiotic therapy, fever persisted and the abscess size remained the same. Antibiotics were upgraded to ofloxacin and piperacillin and tazobactum, following which fever and pain subsided. However, there was no decrease in the size of the abscess despite continuing antibiotics for a period of 3 weeks. Repeat USG-guided aspiration was performed and sent for AFB staining, culture, and polymerase chain reaction (PCR) for Mycobacterium tuberculosis, keeping in mind other rarer possibilities of liver abscess. Aspirated fluid showed numerous AFB bacilli on Ziehl–Neelsen (Z–N) staining. Polymerase chain reaction assay was positive for M. tuberculosis. Multiplex PCR assay was used to differentiate M. tuberculosis from non-tuberculous mycobacteria, as per our protocol. However, mycobacteria culture (BACTEC MGIT-960) was negative in this patient. The patient was started on four drugs ATT (Isoniazid, Ethambutol, Rifampcin, and Pyrazinamide) for 2 months following which the abscess completely disappeared in a month duration (Fig. 2). The patient is presently on a two-drug regimen and recovering well on follow up.
Figure 1.
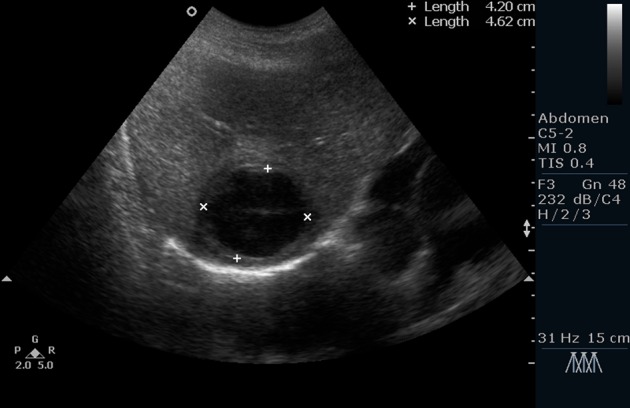
Ultrasonography (USG) of the abdomen revealed a partially liquefied abscess in the right lobe of the liver.
Figure 2.
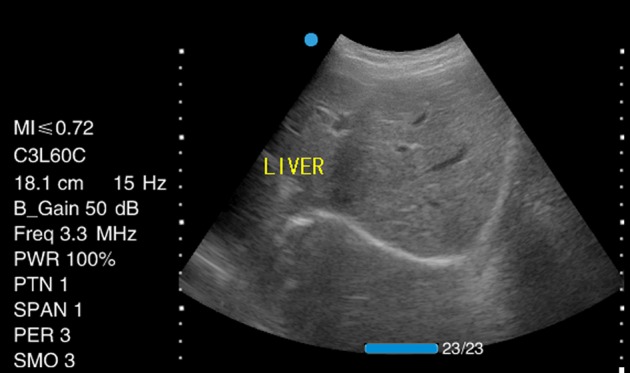
Ultrasonography (USG) of the abdomen showing complete resolution of abscess on ATT for 2 months.
Case 2
A three-year-old male child presented with high-grade fever for 10 days, along with vomiting and pain in the right upper abdomen for 3 days. There was no history of cough or tubercular contact. The child was BCG vaccinated. An abdominal examination revealed a tender hepatomegaly (4 cm below costal margin) with a liver span of 16 cm.
Investigations revealed hematocrit of 28%; hemoglobin of 9.4 gm%; total leukocyte count of 18 600/mm3 (neutrophils 62%, lymphocytes 37%, monocytes 1%); and ESR of 48 mm. Total bilirubin was 1.4 mg/dl (direct 0.7 mg/dl); ALT, and AST were normal. Mantoux test was negative and HIV test was non-reactive. Serum immunoglobulins (IgA, IgG, and IgM), C3, and C4 were normal. Chest X-ray was normal and USG of the abdomen revealed 210 ml of partially liquefied abscess cavity in the right lobe of liver. Aspiration from cavity did not reveal any growth on culture. Empirical antibiotics were started (vancomycin, ceftriaxone, and metronidazole) to which the patient did not respond. Repeat USG-guided aspirate was sent for AFB staining, culture, and PCR for M. tuberculosis, which showed numerous AFB on Z–N staining. This was further confirmed by the growth of M. tuberculosis in BACTEC MGIT-960. Polymerase chain reaction assay was positive for M. tuberculosis. The patient was started on four drugs ATT (Isoniazid, Ethambutol, Rifampcin, and Pyrazinamide) and showed a good response. The general condition of the patient improved; abdomen pain and fever subsided. By the second week of ATT, the abscess size decreased to about one-third of its original size. At the sixth-month follow up, the patient was recovering well with USG showing complete resolution of abscess cavity.
Discussion
Isolated TLA without active pulmonary or miliary tuberculosis, or other clinical evidence of tuberculosis, is distinctly rare.1 Tubercle bacilli reach the liver by hematogenous dissemination, the portal of entry in the case of hepatic miliary tuberculosis is the hepatic artery, whereas in the case of focal liver tuberculosis it is the portal vein.3 The rarity of the focal form of hepatic tuberculosis may be because of the relatively low hepatic tissue oxygen tension.4
The symptoms and signs of tuberculous abscess are non-specific and include fever, vague abdominal pain, anorexia, and weight loss.5 Hepatomegaly is common,6 while jaundice is a rare7 finding. Derangements in liver function tests and alkaline phosphatase have been reported.8,9
Systemic multi drug antituberculous treatment is the preferred treatment in TLA. Surgery is advocated in cases where percutaneous aspiration is not successful or not possible because of the site and multiseptate nature of the abscess or ruptured liver abscess. Some authors have reported successful treatment of TLA through transcatheter infusion of isoniazid followed by antituberculous treatment.5,10,11
The presence of caseating granulomatous lesions in the biopsy and/or presence of AFB in such material is the hallmark of diagnosis.12 Sometimes demonstration of an acid fast mycobacterium in the aspirated pus or a histopathology examination or culture of the scrapings from the abscess wall may be required.10 Recently, PCR has been used for the detection of M. tuberculosis DNA, which also has the added advantage of distinguishing M. tuberculosis from non-tuberculous mycobacterium.13
In our first case, pus examination revealed AFB and PCR assay of the aspirate was positive for M. tuberculosis. Multiplex PCR assay was used to differentiate M. tuberculosis from non-tuberculous mycobacterium as per our protocol.14 In the second case, pus examination revealed AFB and PCR assay of the aspirate was positive for M. tuberculosis, along with positive culture results (BACTEC MGIT-960). In the first case, M. tuberculosis bacilli could not be isolated in culture, probably due to fluoroquinolone treatment received by the patient before culture.
Thus, to conclude, signs and symptoms of isolated TLA are non–specific, and a high index of suspicion is required for its diagnosis, especially in endemic areas and in patients with a known risk factor for tuberculosis. Early diagnosis and prompt treatment with systemic ATT are associated with a favorable outcome.
Acknowledgments
The authors would like to thank editor in chief of Paediatrics and International Child Health for giving permission to include case 2 in this series.
References
- 1.Nampoory MR, Halim MM, Shreedharan R, Al-Sweih WA, Gupta RK, Costandi JN. Liver abscess and disseminated intravascular coagulation in tuberculosis. Postgrad Med J. 1995;71:490–2. doi: 10.1136/pgmj.71.838.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nandan D, Bhatt GC, Dewan V, Yadav TP, Singh S. Isolated tuberculous liver abscess in a 3-year old immunocompetent child. Paediatr Int Child Health. doi: http://dx.doi.org/10.1179/2046905512Y.0000000033. [DOI] [PubMed] [Google Scholar]
- 3.Javid G, Khan BA, Shah AH, Khan MA. Isolated tuberculous liver abscess. J Assoc Physicians India. 1998;46:973–4. [PubMed] [Google Scholar]
- 4.Nand N, Aggarwal HK, Singh M Dayanand. Tuberculous liver abscess. J Assoc Physicians India. 2000;48:244–6. [PubMed] [Google Scholar]
- 5.Kubota H, Ageta M, Kubo H, Wada S, Nagamachi S, Yamanaka T. Tuberculous liver abscess treated by percutaneous infusion of antituberculous agents. Intern Med. 1994;33:351–6. doi: 10.2169/internalmedicine.33.351. [DOI] [PubMed] [Google Scholar]
- 6.Baveja CP, Gumma CP, Chaudhary M, Jha H. Primary tubercular liver abscess in an immunocompetent adult: a case report. J Med Case Rep. 2009;3:78. doi: 10.1186/1752-1947-3-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desai CS, Joshi AG, Abraham P, Desai DC, Deshpande RB, Bhaduri A, et al. Hepatic tuberculosis in absence of disseminated abdominal tuberculosis. Ann Hepatol. 2006;51:41–3. [PubMed] [Google Scholar]
- 8.Rangabashyam N. Abdominal tuberculosis. In: Oxford Textbook of Surgery. Vol. II. Oxford: Oxford University Press; 1994, p. 2491. [Google Scholar]
- 9.Yapp SK, Kok KY. Isolated hepatic tuberculosis: report of five cases and review of the literature. J Hepatobiliary Pancreat Surg. 1999;6:195–8. doi: 10.1007/s005340050106. [DOI] [PubMed] [Google Scholar]
- 10.Debnath PR, Tripathi R, Kandpall D, Kumar B, Malik E, Sharma SB. Isolated tubercular liver abscess in children treated with percutaneous isoniazid infusion. Indian J Tuberc. 2007;54:149–51. [PubMed] [Google Scholar]
- 11.Mustard RA, Mackenzie RL, Gray RG. Percutaneous drainage of a tuberculous liver abscess. Can J Surg. 1986;29:449. [PubMed] [Google Scholar]
- 12.Roy R, Goyal RK, Gupta N. Tuberculous liver abscess. J Assoc Physicians India. 2000;48:241–3. [PubMed] [Google Scholar]
- 13.Diaz ML, Herrera T, Vidal YL, Calva JJ, Hernandez R, Palacios GR, et al. Polymerase chain reaction for the detection of Mycobacterium tuberculosis DNA in tissue and assessment of its utility in the diagnosis of hepatic granuloma. J Lab Clin Med. 1996;127:359–63. doi: 10.1016/s0022-2143(96)90184-5. [DOI] [PubMed] [Google Scholar]
- 14.Gopinath K, Singh S. Multiplex PCR assay for simultaneous detection and differentiation of Mycobacterium tuberculosis, Mycobacterium avium complexes and other Mycobacterial species directly from clinical specimens. J Appl Microbiol. 2009;107:425–35. doi: 10.1111/j.1365-2672.2009.04218.x. [DOI] [PubMed] [Google Scholar]


