Abstract
Background
We evaluated stroke risk associated with HT in younger women, women recently menopausal, and in older women.
Methods
Prospective, observational analyses in postmenopausal participants of the Nurses’ Health Study, from 1976–2004, with biennial mailed questionnaires. We used proportional hazards models to calculate multivariable-adjusted relative risks and 95% confidence intervals.
Results
We found a significantly increased risk of stroke for women currently taking HT (estrogen alone: RR=1.39, 95% CI 1.18,1.63; estrogen with progestin: RR=1.27, 95% CI 1.04,1.56); nearly identical results to the Women’s Health Initiative. This increased risk was observed for women initiating hormone therapy at young ages or near menopause, and at older ages or >10 years after menopause. Short-term (<5 years) HT initiated at younger ages was not associated with a clear increase in stroke; however this was based on a small number of cases. The incidence of stroke was relatively low in younger women, and the attributable risk in women aged 50–54 years indicated approximately an additional 2 cases of stroke per 10,000 women per year taking hormones. We found a strong relation between dose of oral conjugated estrogen and stroke, with relative risks of 0.93, 1.54, 1.62, for doses of 0.3, 0.625, and 1.25mg respectively (p-trend<0.0001).
Conclusions
Hormone therapy increases risk of stroke, and this elevation does not appear related to timing of hormone initiation. In younger women, with lower stroke risk, the attributable risk of stroke due to hormone use is modest and might be minimized by lower doses and shorter treatment duration.
INTRODUCTION
Many controversies remain regarding the risks and benefits of postmenopausal hormone therapy. In particular, there are relatively limited data regarding the effects of hormone use on stroke. We have previously reported a significant, 35% increased risk of stroke with current use of hormone therapy (HT) in the Nurses’ Health Study.1 The Women’s Health Initiative (WHI), a randomized trial of postmenopausal hormone therapy (HT), also reported a 30–40% elevated risk of stroke for women given estrogen combined with progestin or estrogen alone.2,3 Although these risks appeared similar in the WHI for women who initiated hormone therapy at younger and older ages, the WHI included few women who were recently menopausal, when hormone therapy is most commonly initiated in clinical settings. Thus, the stroke risk for women taking HT near menopause, in terms of both relative and absolute risks, remains unclear; since HT is the most effective treatment for menopausal symptoms, it is important to determine whether stroke risk is an important consideration for younger women, taking HT near the onset of menopause. In addition, although national recommendations suggest taking the lowest possible HT dose to minimize risks, sparse data are available regarding the relation between lower doses of estrogen and stroke.
In a previous publication,1 we had reported results for the relation of current and past HT, including HT duration and estrogen dose, to total stroke, ischemic stroke and hemorrhagic stroke, and also presented the associations of HT regimen (estrogen alone versus combined with progestin) to total stroke. Thus, in the present analyses, we examined the most critical current questions regarding stroke risk: we both explored the timing of hormone therapy initiation, and also further examined varying estrogen doses, since we had limited power to address this in the previous analyses. In addition, given important differences in the etiology of ischemic stroke and hemorrhagic stroke, we also updated our analyses of hormone regimen to specifically address the stroke type.
METHODS
The Nurses’ Health Study Cohort
The Nurses’ Health Study began in 1976 when 121,700 female nurses, aged 30 to 55 years returned a mailed questionnaire, including detailed information on menopause and postmenopausal hormone use, as well as diagnosis of cardiovascular disease and cardiovascular risk factors. We update health and lifestyle information with biennial follow-up questionnaires. Dietary and physical activity questionnaires were added in 1980. Cohort follow-up is over 90%.
Ascertainment of Postmenopausal Hormone Use
On each biennial questionnaire, women were asked details regarding postmenopausal hormone therapy, including current use (within the last month), duration of use, type of hormones taken and dose of oral conjugated estrogen (data on estrogen dose were first collected in 1980).
Identification of Stroke
We identified first occurrences of nonfatal and fatal stroke between the return of the 1976 questionnaire and June 1, 2004. Nurses who reported a nonfatal stroke were asked for permission to review their medical records. Medical records were reviewed by physicians without knowledge of the participant’s self-reported exposure status. Nonfatal strokes for which medical records were unavailable were not included in analyses. Deaths were ascertained by reports from relatives or postal authorities and a search of the National Death Index.4 Only fatal stroke cases documented by medical records were included in analyses. Overall, medical records were available for 74 percent of reported stroke cases. In contrast, in our previous publications on stroke,1 we had included both cases confirmed by medical record review as well as “probable” cases, defined as strokes for which medical records were unavailable but which required hospitalization and were corroborated by letter or interview with the subject or next of kin. However, in the current analyses, we were more interested in stroke type, and thus could not include cases without medical records. This difference in our analytic approach would have little impact on the relative risk estimates. Characteristics of the subset of cases with medical records were very similar to those of all women with stroke; for example, of those with medical records available, 46% had never taken HT, 36% used estrogen alone and 18% used estrogen with progestin, while in the entire group of stroke cases, these figures were 48%, 35% and 17%, respectively. However, the exclusion of probable cases decreases our estimates of absolute stroke rates and attributable risks. Thus, for the purposes of comparison, we provide data on stroke rates and attributable risks both excluding and including the probable cases.
Incident strokes were confirmed using National Survey of Stroke criteria,5 which require a constellation of neurologic deficits, sudden or rapid in onset, and duration of at least 24 hours or until death. Cerebrovascular pathology due to infection, trauma, or malignancy was excluded. We classified strokes as ischemic (embolic or thrombotic) and hemorrhagic (subarachnoid or intracerebral) according to standard criteria based on symptoms and diagnostic imaging or pathology.6
Population for Analysis
In primary analyses, women who reported stroke, as well as myocardial infarction, angina, coronary revascularization, or cancer (except non-melanoma skin cancer) on the 1976 questionnaire were excluded, because these are among the most common major diseases which may have caused women to alter their hormone use. Similarly, women who reported such diagnoses on a subsequent questionnaire were censored at that point and excluded from further analysis. Thus, at the start of each two-year interval, the base population included no women reporting these diagnoses.
We classified women as postmenopausal from the time of natural menopause or hysterectomy with bilateral oophorectomy. Women who underwent hysterectomy without bilateral oophorectomy were considered postmenopausal when they reached the age at which natural menopause had occurred in 90% of the cohort (54 years for smokers and 56 for nonsmokers). The women’s reports of age at7 and type of menopause8 were highly accurate in this cohort.
We explored the effects of initiating hormone therapy at varying intervals since menopause and at different ages. A primary interest was to investigate stroke risk in younger women, near menopause. To provide data for women initiating hormones near menopause, we examined women who began hormone use within 4 years of menopause. We chose a cut-off of 4 years to define “near” menopause since our follow-up occurs in 2-year intervals and we believed that a 2-year cutoff was excessively short but that a 6-year cut-off was too long. Moreover, most HT use in the general population occurs within four years of menopause onset. In these analyses, we excluded women with unknown age at menopause (eg, those with no uterus, but intact ovaries). In addition, we also examined women initiating hormone therapy at younger ages (50–59 years, or <55 years) to women who never used hormones.
Statistical Analysis
For each participant, person-months were allocated to hormone categories according to the 1976 data, and updated every two years (for estrogen dose, follow-up began in 1980). We specifically assessed dose of oral conjugated estrogen with or without oral medroxyprogesterone acetate, as these two were the most common regimens as well as the hormones used in the Women’s Health Initiative. If no data were available on hormones in a given time period, women were assigned to a missing category for that time period. Follow-up for a participant ended with a first diagnosis of stroke, or death, or June 1, 2004, whichever came first. In total, we included 485,987 person-years of follow-up among women who had never taken HT, and 409,629 among current HT users. Compared to our previous publication with follow-up through 1996,1 the present data represent substantially greater power to detect effects, with a 36% increase in the person-years among women who had never used hormone therapy and a 54% increase among women who were currently taking HT. The greater increase of current hormone use than “non-use” likely reflects both the aging of the population, as well as changing prescription patterns over the different time periods.
Analyses are based on incidence rates using person-years of follow-up as the denominator. We used relative risk (RR) as the measure of association, defined as the incidence rate of stroke among women in various categories of hormone use divided by the rate among women who never used hormones. We computed age-specific rates using 5-year categories, and calculated age-adjusted relative risks using Mantel-Haenszel rate ratios, with 95% confidence intervals (CI).
We calculated adjusted relative risks with Cox proportional hazards models, controlling for: age (continuous), body mass index (<21 kilograms/meter2, 21–22, 23–25, 26–29, 30–31, 32+), cigarette smoking (never, past, current smoker of 1–14, 15–24, 25–34, 35+ cigarettes/day), history of hypertension (yes, no), diabetes (yes, no), and elevated cholesterol (yes, no), husband’s education, and parental myocardial infarction before age 60 (yes, no). For certain analyses, alcohol use (none, <5g/day, 5–14.9, 15+), vitamin E supplementation (yes, no), multivitamin use (yes, no), regular aspirin use (none, 1–6/week, 7+/week), and physical activity (quintiles of MET hours of activity) were added to the model; in these analyses, follow-up began in 1980 when that information was first collected and included only women who completed the diet questionnaires (approximately 80% of the subjects). Finally, adjusting for hysterectomy status had no impact on our results, thus we did not include this variable in our models.
We calculated rate differences based on the rate of total stroke among participants who had never used HT. For ease of calculation, we multiplied this rate by the overall, multivariable-adjusted relative risk we found for the association of current HT use to total stroke (ie, RR=1.4), to obtain the stroke rate for HT users. We then subtracted the rate estimated for women taking HT from the rate among women who never used hormones to obtain rate differences, or the number of stroke cases that would be incurred with hormone use.
RESULTS
For estrogen alone, the age-adjusted relative risk of total stroke for current users was 1.33 (95% CI 1.13,1.55), compared to women who never used hormone therapy (Table 1). For combined hormone therapy, this RR was generally similar (RR=1.17, 95% CI 0.96,1.42). After adjustment for major stroke risk factors, these estimates became slightly stronger: the relative risk for estrogen alone rose to 1.39 and the relative risk for estrogen with progestin rose to 1.27. When we further adjusted for dietary factors, physical activity, regular aspirin use and vitamin supplementation (data not shown in table), the results did not materially change (eg, for total stroke, RR=1.43, 95% CI 1.19,1.71 with estrogen alone and RR=1.45, 95% CI 1.18,1.80 with combined therapy); thus, we did not include these additional covariates in primary analyses. Relative risks were generally similar across stroke types (ie, ischemic stroke, hemorrhagic stroke, non-fatal stroke, fatal stroke), although with the small number of hemorrhagic strokes or fatal strokes, those relative risks were not statistically significant (Table 1).
Table 1.
Risk for Stroke among Current Postmenopausal Hormone Users Compared to Women Who Never Used Hormones
| Cases | Person-Years | Age-adjusted Relative Risk (95% confidence interval) | Multivariate adjusted Relative Risk* | |
|---|---|---|---|---|
| Relative Risk | ||||
| Total Stroke | ||||
| Never Used Hormones | 360 | 485,987 | 1.0 (reference) | |
| Current Use of: | ||||
| Estrogen Alone | 276 | 256,437 | 1.33 (1.13,1.55) | 1.39 (1.18,1.63) |
| Estrogen + Progestin | 138 | 153,192 | 1.17 (0.96,1.42) | 1.27 (1.04,1.56) |
| Ischemic Stroke | ||||
| Never Used Hormones | 235 | 485,987 | 1.0 (reference) | |
| Current Use of: | ||||
| Estrogen Alone | 183 | 256,437 | 1.33 (1.09,1.61) | 1.43 (1.17,1.74) |
| Estrogen + Progestin | 103 | 153,192 | 1.32 (1.05,1.67) | 1.53 (1.21,1.95) |
| Hemorrhagic Stroke | ||||
| Never Used Hormones | 85 | 485,987 | 1.0 (reference) | |
| Current Use of: | ||||
| Estrogen Alone | 61 | 256,437 | 1.35 (0.97,1.88) | 1.37 (0.98,1.91) |
| Estrogen + Progestin | 24 | 153,192 | 0.88 (0.56,1.38) | 0.87 (0.55,1.39) |
| Fatal Stroke | ||||
| Never Used Hormones | 50 | 485,987 | 1.0 (reference) | |
| Current Use of: | ||||
| Estrogen Alone | 33 | 256,437 | 1.20 (0.77,1.86) | 1.22 (0.78,1.90) |
| Estrogen + Progestin | 15 | 153,192 | 0.93 (0.52,1.66) | 1.03 (0.57,1.86) |
| Non-fatal Stroke | ||||
| Never Used Hormones | 310 | 485,987 | 1.0 (reference) | |
| Current Use of: | ||||
| Estrogen Alone | 243 | 256,437 | 1.35 (1.14,1.60) | 1.41 (1.19,1.68) |
| Estrogen + Progestin | 123 | 153,192 | 1.20 (0.98,1.48) | 1.31 (1.05,1.62) |
Adjusted for age, BMI, high cholesterol, diabetes, high blood pressure, husband’s education, smoking, family history premature MI.
Timing of HT initiation in relation to onset of menopause or age (table 2), did not appear to change the observed associations (eg, for estrogen alone: RR=1.20, 95% CI 1.06,1.58 initiated near menopause; RR=1.31, 95% CI 1.06,1.63 initiated 10+ years after menopause). These elevations in stroke risk were consistent for women taking estrogen alone and estrogen combined with progestin (eg, for estrogen with progestin: RR=1.22, 95% CI 0.95,1.55 initiated near menopause; RR=1.18, 95% CI 0.87,1.60 initiated 10+ years after menopause).
Table 2.
Risk for Total Stroke Comparing Women Currently Taking Hormone Therapy and Those Who Never Used Hormone Therapy, by Timing of Hormone Initiation with Respect to Onset of Menopause and Age
| Cases | Person-Years | Relative Risk* (95% confidence interval) | |
|---|---|---|---|
| HORMONE INITIATION BY TIME SINCE MENOPAUSE†: | |||
| INITIATION NEAR MENOPAUSE | |||
| Never | 312 | 370,831 | 1.0 (ref) |
| Estrogen Alone | 146 | 163,092 | 1.29 (1.06,1.58) |
| Estrogen + Progestin | 93 | 119,912 | 1.22 (0.95,1.55) |
| INITIATION 10+ YEARS AFTER MENOPAUSE | |||
| Never | 240 | 193,066 | 1.0 (ref) |
| Estrogen Alone | 133 | 87,038 | 1.31 (1.06,1.63) |
| Estrogen + Progestin | 53 | 35,909 | 1.18 (0.87,1.60) |
| HORMONE INITIATION BY AGE‡: | |||
| INITIATED AT AGE 50–59 YEARS | |||
| Never | 108 | 239,967 | 1.0 (ref) |
| Estrogen Alone | 31 | 49,590 | 1.58 (1.06,2.37) |
| Estrogen + Progestin | 25 | 51,904 | 1.34 (0.84,2.13) |
| INITIATED AT AGE 60+ YEARS | |||
| Never | 242 | 202,856 | 1.0 (ref) |
| Estrogen Alone | 41 | 18,513 | 1.82 (1.30,2.54) |
| Estrogen + Progestin | 37 | 17,588 | 1.72 (1.21,2.44) |
Adjusted for age, BMI, high cholesterol, diabetes, high blood pressure, husband’s education, smoking, family history premature MI.
Near menopause defined as within four years; data not shown for 5–9 years since menopause.
Data not shown for women who initiated hormone therapy in their forties.
Since HT is most commonly initiated to treat menopausal symptoms, which generally last less than five years, we also examined the impact of HT duration on stroke risk; in these analyses we focused on the very youngest women, within four years of menopause or less than 55 years of age (data not shown in table). We combined women taking estrogen alone and estrogen with progestin, since both regimens appeared to have a similar relation with stroke. Although the number of cases with shorter duration of HT use was somewhat small, the relative risks of stroke were not significant, especially for women less than age 55 years; among women within four years of menopause, taking hormones for <5 years, the relative risk was 1.32 (95% CI 0.95–1.83), and among women less than age 55 years, this estimate was 0.94 (95% CI 0.58–1.53).
When we examined the absolute stroke rates, considering only the confirmed stroke cases (Figure 1), stroke rates were low among younger women, but increased greatly at older ages. For example, among women who had never taken HT, the rate of stroke was 3.8/10,000PY for those aged 50–54 years; this rate more than doubled at age 60–64 years to 7.1/10,000 and rose almost five-fold to 17.9/10,000 for women aged 65+ years. Correspondingly, the attributable risk of stroke due to current HT use was relatively low in the younger women. For example, if 10,000 women aged 50–54 years used HT for one year -- applying the relative risk of 1.4 for HT and stroke seen in the overall cohort to all women -- one would expect an extra 1.5 cases of stroke compared to an extra 7.2 cases for women aged 65+ years.
Figure 1.
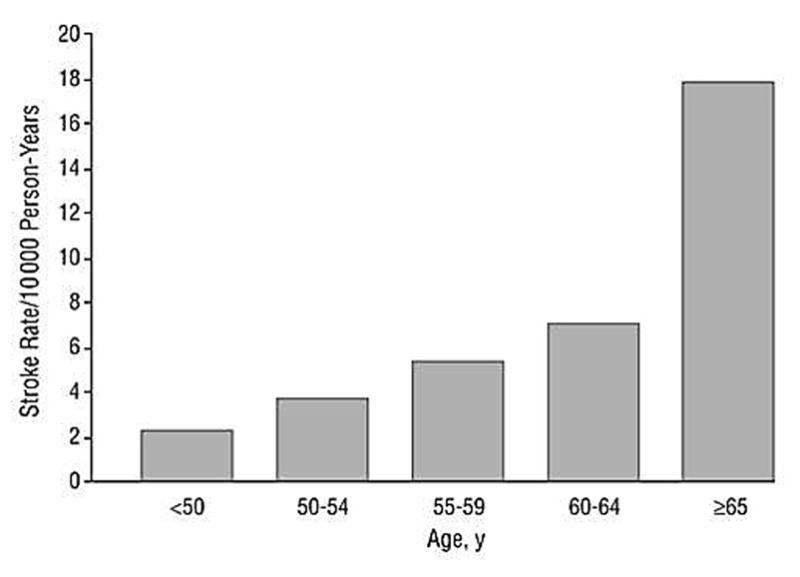
Rate of total stroke among women who never used hormone therapy (HRT) in the Nurses’ Health Study.
In alternate analyses, including both the confirmed and probable cases, absolute stroke rates were higher, ranging from 5.4/10,000PY among women aged 50–54 years, to 10.6/10,000PY among women aged 60–64 years and 26.0/10,000 among women aged 65+ years (data not shown in table). Similarly, the attributable risk of stroke due to current HT use was higher. For example, if 10,000 women used HT for one year, we would expect an extra 2.2 cases of stroke for women aged 50–54 years, and an extra 10.4 cases for women aged 65+ years (data not shown in table).
Finally, when we examined the dose of estrogen (Table 3), we found a strong trend of increasing risk of stroke with increasing dose of oral conjugated estrogen (p-trend<0.0001). Specifically, for total stroke, there was a similar rate of stroke for women currently taking 0.3mg of estrogen compared to women who had never taken HT (multivariable-adjusted RR=0.93, 95% CI 0.62,1.40), while there were statistically significant increases for those taking 0.625mg (RR=1.54, 95% CI 1.31,1.81) and 1.25mg (RR=1.62, 95% CI 1.23,2.14).
Table 3.
Risk for Total Stroke among Current Postmenopausal Hormone Users Compared to Women Who Never Used Hormones, by Dose of Oral Conjugated Estrogen*
| Cases | Person-years | Multivariable-adjusted Relative Risk† (95% confidence interval) | |
|---|---|---|---|
| Never Used | |||
| Hormones | 349 | 452,957 | 1.00 (reference) |
| Current Estrogen | |||
| 0.3mg | 25 | 33,391 | 0.93 (0.62,1.40) |
| 0.625mg | 268 | 233,249 | 1.54 (1.31,1.81) |
| 1.25mg | 60 | 59,373 | 1.62 (1.23,2.14) |
Follow-up is from 1980–2004, since data on dose were first collected in 1980.
Adjusted for age, BMI, high cholesterol, diabetes, high blood pressure, husband’s education, smoking, family history premature MI.
DISCUSSION
Overall, we found approximately a 30–40% increased risk of stroke for women currently taking postmenopausal hormone therapy, either estrogen alone or combined with progestin. These findings are virtually identical to those of the Women’s Health Initiative trials.2,3 Similar to the WHI, we did not find any clear difference in the relation of HT to stroke for women initiating therapy at younger ages versus at older ages. However, considering the low rate of stroke development in younger women, the attributable risk of stroke associated with hormone use in the younger age groups was modest. Moreover, although confidence intervals were wide, there was not a clear increase in the risk of stroke for the youngest women, who used HT for less than five years.
In addition, we found a strong trend of increasing risk of stroke with increasing dose of estrogen. At the lowest estrogen dose (0.3mg of oral conjugated estrogen), there was not a statistically significantly greater risk of stroke, although the confidence interval was fairly wide. These current findings are generally similar to our previously-published data on HT and stroke,1 where we had also reported a trend of increasing stroke risk with increasing estrogen dose. However, in the previous report, with just 9 stroke cases among women taking 0.3mg of estrogen, we had found a nearly 50% decrease in stroke rates compared to women who had never taken HT (RR=0.54, 95% CI 0.28–1.06), although the confidence interval was wide. In these analyses, with almost three times as many stroke cases in the low-dose estrogen group, the relative risk was 0.93 (95% CI 0.62–1.40), consistent with the prior estimate, but ruling out the previously-reported 50% reduction in stroke for low-dose estrogen users. Very limited additional research has been conducted on the relation of hormone dose to risk of stroke. However, in a randomized trial, low-dose estrogen did not increase certain inflammatory or thrombotic markers to the same extent as higher doses.9 Clearly, substantially more research is needed on the cardiovascular effects of 0.3mg of estrogen, since this dose has now become common in clinical practice.
Interestingly, in contrast to data on heart disease in both our study and the WHI,10–12 suggesting a lower risk of heart disease with HT initiation at younger ages or near menopause, the risk of stroke appeared similar regardless of the timing of HT initiation. Still, we found a low absolute rate of stroke in younger women, leading to a modest attributable risk; both the absolute rate and the attributable risk remained modest among younger women even after we included stroke cases for whom we had no medical records available. Since Nurses’ Health Study participants are a select group of educated health professionals, these data on stroke rates and attributable risks likely underestimate those in the general population. However, our rates were only somewhat lower than estimates across studies of more general populations,13 especially when we included stroke cases for which we could not obtain medical records. For comparison, among women aged 55–64 years, the American Heart Association Statistical Committee13 reported a rate of 19.0/10,000 for cerebral infarction and hemorrhagic strokes compared to our finding of 12.5/10,000 in this age group after excluding those without medical records, and 18.2/10,000 including cases without medical records.
Finally, confounding is always a concern in observational studies. However, we found that adjustment for potential confounding factors did not substantially alter associations between postmenopausal hormone therapy and stroke (ranging from a 10–20% increase in the relative risk) – indicating that the relation would likely not be largely changed with either more accurate data on known confounding factors, or additional data on currently unknown confounding factors. Our results on the relation of HT to stroke are entirely consistent with those from the Women’s Health Initiative trials, strongly indicating that our data on stroke are valid.
In summary, our findings in the Nurses’ Health Study indicate that HT is associated with an increased risk of stroke, regardless of the hormone regimen or timing of hormone initiation. However, in younger women, at lower absolute risk of stroke, the attributable risk of stroke due to hormone use is modest and our data suggested that risk might be further minimized by lower doses and shorter duration of treatment.
Acknowledgments
The work described in this manuscript was supported by grants HL34594 and CA87969 from the National Institutes of Health. The funding source had no role in the design, analysis or interpretation of the study.
References
- 1.Grodstein F, Manson JE, Colditz GA, Willett WC, Speizer FE, Stampfer MJ. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med. 2000;133:933–41. doi: 10.7326/0003-4819-133-12-200012190-00008. [DOI] [PubMed] [Google Scholar]
- 2.Hendrix SL, Wassertheil-Smoller S, Johnson KC, et al. Effects of conjugated equine estrogen on stroke in the Women’s Health Initiative. Circulation. 2006;113:2425–2434. doi: 10.1161/CIRCULATIONAHA.105.594077. [DOI] [PubMed] [Google Scholar]
- 3.Wassertheil-Smoller S, Hendrix SL, Limacher M, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative. JAMA. 2003;289:2673–2684. doi: 10.1001/jama.289.20.2673. [DOI] [PubMed] [Google Scholar]
- 4.Stampfer MJ, Willett WC, Speizer FE, et al. Test of the National Death Index. Am J Epidemiol. 1984;119:937–9. doi: 10.1093/oxfordjournals.aje.a113804. [DOI] [PubMed] [Google Scholar]
- 5.Walker AE, Robins M, Weinfeld FD. The National Survey of Stroke. Clinical findings Stroke. 1981;12:113–44. [PubMed] [Google Scholar]
- 6.Anderson CS, Jamrozik KD, Burvill PW, et al. Determining the incidence of different subtypes of stroke: results from the Perth Community Stroke Study, 1989–1990. Med J Aust. 1993;158:85–9. doi: 10.5694/j.1326-5377.1993.tb137529.x. [DOI] [PubMed] [Google Scholar]
- 7.Willett WC, Stampfer MJ, Bain C, et al. Cigarette smoking, relative weight and menopause. Am J Epidemiol. 1983;117:651–8. doi: 10.1093/oxfordjournals.aje.a113598. [DOI] [PubMed] [Google Scholar]
- 8.Colditz GA, Stampfer MJ, Willett WC, et al. Reproducibility and validity of self-reported menopausal status in a prospective cohort study. Am J Epidemiol. 1987;126:319–25. doi: 10.1093/aje/126.2.319. [DOI] [PubMed] [Google Scholar]
- 9.Koh KK, Shin MS, Sakuma I, et al. Effects of conventional or lower doses of hormone replacement therapy in postmenopausal women. Arterioscler Thromb Vasc Biol. 2004;24:1516–21. doi: 10.1161/01.ATV.0000133683.65877.bc. [DOI] [PubMed] [Google Scholar]
- 10.Grodstein F, Manson JE, Stampfer MJ. Hormone therapy and coronary heart disease: The role of time since menopause and age at hormone initiation. J Womens Health. 2006;15:35–44. doi: 10.1089/jwh.2006.15.35. [DOI] [PubMed] [Google Scholar]
- 11.Manson JE, Hsia J, Johnson KC, et al. Estrogen plus progestin and the risk of coronary heart disease. New Engl J Med. 2003;349:523–34. doi: 10.1056/NEJMoa030808. [DOI] [PubMed] [Google Scholar]
- 12.Hsia J, Langer RD, Manson JE, et al. Conjugated equine estrogens and coronary heart disease: the Women’s Health Initiative. Arch Intern Med. 2006;166:357–65. doi: 10.1001/archinte.166.3.357. [DOI] [PubMed] [Google Scholar]
- 13.Rosamond W, Flegal K, Friday G, et al. for the American Heart Association Statistical Committee. Heart disease and stroke statistics -- 2007 update. Circulation. 2007;115:e69–171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]


