Abstract
Using telephone survey data from 1111 retired older adults (≥65 years; 634 male, 477 female), we tested the hypothesis that exposure to shift work might result in increased self-reported diabetes. Five shift work exposure bins were considered: 0 years, 1-7 years, 8-14 years, 15-20 years, and >20 years. Shift work exposed groups showed an increased proportion of self-reported diabetes (χ2 = 22.32, p < 0.001), with odds ratios (ORs) of about 2 when compared to the 0-year group. The effect remained significant after adjusting for gender and body mass index (BMI) (OR ≥ 1.4; χ2 = 10.78, p < 0.05). There was a significant shift work exposure effect on BMI (χ2 = 80.70, p < 0.001) but no significant gender effect (χ2 = 0.37, p > 0.50).
Keywords: shiftwork, night work, diabetes, BMI, old, seniors, human
In a recent laboratory study, Buxton and colleagues (2012) used a circadian forced desynchrony (FD) protocol to investigate the metabolic sequelae of circadian desynchrony and partial sleep loss in human subjects. Exposure to prolonged sleep restriction with concurrent circadian disruption resulted in decreased resting metabolic rates and increased plasma glucose concentrations. In the rat model, it appears that the disruption of circadian rhythms accelerates the development of diabetes through pancreatic β-cell loss and dysfunction (Gale et al., 2011). Buxton and colleagues’ (2012) circadian FD work complemented earlier human sleep studies (Buxton and Marcelli, 2010; Knutson et al., 2007), which had revealed similar metabolic dysfunction when partial or complete sleep deprivation was compared to a full-sleep condition. Outside of the research laboratory, sleep insufficiency and circadian desynchrony are most commonly associated with shift work (Buxton and Marcelli, 2010; Knutson and Van Cauter, 2008). Thus, the aim of the present analysis was to determine whether prior shift work exposure was related to current diabetes in a heterogenous sample of retired U.S. workers.
Most shift workers spend their working lives with a good deal of circadian desynchrony and sleep restriction. Sleep is shortened by an average of about 2 hours every time a shift worker pulls a night shift (Drake et al., 2004; Akerstedt, 2005). The circadian desynchrony experienced by shift workers (often for several decades) can be likened to that associated with weekly round-trip flights from Moscow to Chicago (Monk, 2000), with some workers on irregular schedules suffering even worse assaults on the circadian system. Various adverse health consequences have been attributed to shift work (Costa, 2003; Yoshizaki et al., 2013). Several studies have shown that shift work adversely affects metabolic health. A study in the Netherlands concluded that body mass index (BMI) increases with shift work experience (van Amelsvoort et al., 1999). Current shift work has been shown to be associated with increased metabolic syndrome in Sweden (Karlsson et al., 2001), Italy (Pietroiusti et al., 2010), and Taiwan (Lin et al., 2009). Studies in Japan have shown that shift work is associated with insulin resistance (Nagaya et al., 2002), impaired glucose metabolism (Suwazono et al., 2009), and the likelihood that those with impaired fasting glucose would become diabetic (Toshihiro et al., 2008). In the U.S., the Nurses’ Health Study has shown an increased risk of diabetes associated with overtime work and shift work (Kroenke et al., 2007); the risk of shift work is “dose dependent” based on the duration of exposure (Pan et al., 2011). Although simple shift work versus day-work comparisons are useful, there is often a “survivor effect” in play, whereby those surviving shift work for several decades are particularly resilient. For this reason, we divided shift work exposure into several “bins,” as others have done (Pan et al., 2011). The present study is novel in that it concerns a heterogenous sample of U.S. retirees who are no longer subject to the stresses of shift work.
As a small part of a recent telephone interview study of more than 1000 retired (≥65 years) shift workers living in Western Pennsylvania, which was mostly concerned with sleep (Monk et al., 2013), we asked the following: “Do you suffer from diabetes, also called sugar, requiring either pills or injections?” (“Sugar” is a local colloquial term for diabetes.) We also asked respondents their height and weight so we could calculate their self-reported BMI. The interview started by collecting data from which an accurate estimate of the duration of shift work exposure could be calculated. This included the schedule worked for each job and starting and ending dates. Shift work was defined as nonovertime scheduled work (≥35 h/wk) outside the home, overlapping the 0000 h to 0600 h window on either a fixed or rotating basis. There were 5 shift work exposure groups: 0 years, 1-7 years, 8-14 years, 15-20 years, and >20 years. The 0-years group excluded anyone ever working past 2100 h on a nonovertime basis. Telephone lists were purchased that had a high likelihood of having an older adult in the household. Local postal codes having a higher incidence of shift working occupations were selected. As the study progressed, an effort was made to ensure approximately equal numbers in the 5 exposure groups. This involved terminating an interview if the respondent reported being in an exposure group currently over-represented. Thus, the sampling was not random but equally was not simply a convenience sample. All subjects were aged ≥65 years and were retired (i.e., not working >10 h/wk for pay outside the home). None had performed shift work within the past year. From a total of 1166 respondents who gave a full work history, 1111 (634 male, 477 female) gave full data regarding all relevant measures presently required. Sample size, age, and percentage of men are given in Table 1. Analyses used both unadjusted and adjusted (for gender and BMI) models using Wald χ2 and odds ratios (ORs) and their confidence intervals (CIs).
Table 1. Descriptive statistics for the 5 shift work exposure groups.
| Exposure | 0 Years | 1-7 Years | 8-14 Years | 15-20 Years | >20 Years |
|---|---|---|---|---|---|
| n | 385 | 230 | 140 | 127 | 229 |
| Male, % | 48.3 | 49.1 | 57.1 | 63.8 | 76.0 |
| Age,a y | 75.6 ± 6.1 | 74.2 ± 6.7 | 73. 8 ± 6.4 | 74.2 ± 6.1 | 75.0 ± 6.4 |
Ages are expressed as mean ± SD.
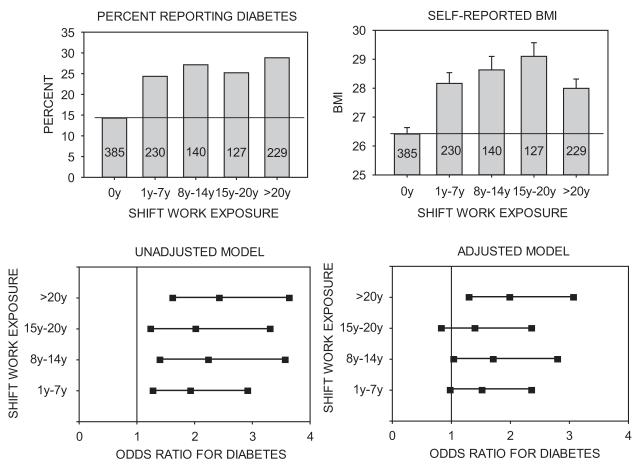
As illustrated in Figure 1 (upper panels), both the percentage of those reporting diabetes and selfreported BMI were greater in each of the 4 shift work exposed groups as compared to the non-exposed group. In the unadjusted model, shift work exposure had a significant effect on reported diabetes (χ2 = 22.32, p < 0.001). Pairwise comparisons of each of the shift work exposed groups with the non-exposed group in the unadjusted model revealed OR values of 1.93 to 2.43, with the CI not overlapping 1.0 (i.e., significant) for all 4 groups (Fig. 1, lower left). In the adjusted model, shift work exposure again had a significant effect (χ2 = 10.78, p < 0.05). There was also a significant shift work exposure effect on BMI (χ2 = 80.70, p < 0.001) but no significant gender effect (χ2 = 0.37, p > 0.50). Pairwise comparisons in the adjusted model indicated OR values of 1.40 to 1.99, with the CI not overlapping 1.0 for two of the groups (Fig. 1, lower right). In neither model did any of the shift work exposed groups significantly differ from each other.
Figure 1.
Upper panels: Self-reported diabetes and BMI. The percentage of subjects reporting diabetes (left), and mean ± SEM self-reported BMI (right) are given for each of the 5 shift work exposure groups. Sample sizes are given within each bar. The horizontal line is at the unexposed (0-years group) level. Lower panels: The OR (relative to the 0-years group) of reporting diabetes, together with 95% Wald CIs, for each of the 4 shift work exposed groups. Given are results from the unadjusted model (left), and from the adjusted model (right) as adjusted for BMI and gender. The vertical lines are at an OR of 1.0; intervals not overlapping the line are deemed significant.
The present study can only be regarded as tentative, given its reliance on simple self-reports over the telephone, with all of the resulting inaccuracies. No distinction was made between type 1 and type 2 diabetes (although the prevalence of type 1 is likely 1%-3% for this age group), and only those requiring medication (rather than common simply dietary interventions) were included. Strengths include the careful determination of shift work exposure and the use of retired, rather than current, workers in a heterogenous sample involving both genders. Our findings are in broad agreement with much more comprehensive studies in the literature, albeit on current workers, rather than retirees. Pan and colleagues (2011) recently reported prospective studies from 177,184 female nurses, showing both a shiftwork exposure effect on diabetes and also an attenuation (but not elimination) of the shift work exposure effect when BMI was controlled for. It is noteworthy, and perhaps indicative of a “survivor effect,” that our >20-years group had a lower than expected BMI. This effect may also have diminished inter-group differences in diabetes.
These results are of significant concern, given the reported epidemic of diabetes and obesity in the U.S. (Kirkman et al., 2012). In line with points made by the sleep and circadian rhythms community for several decades now (Mitler et al., 1988; Drake et al., 2004), the results suggest that a 3-fold strategy from a public health perspective may be needed: 1) Society should recognize that while it is often absolutely necessary for 24-hour operations because of the nature of the work, there are also situations where work at night is optional and should perhaps be avoided by employers; 2) intensive educational campaigns should be put in place regarding the increased need for shift workers to adopt behavioral strategies regarding diet, exercise, and circadian adjustment because of their increased vulnerability to metabolic problems; and 3) there is a need for a general campaign to increase societal awareness regarding the need for regularity in daily rhythms including the sleep-wake cycle, the best ways to facilitate circadian adjustment (Monk, 2000), and the need for an adequate opportunity for sleep.
ACKNOWLEDGMENTS
The authors thank Amy Begley, Jean Miewald, Mary Fletcher, Kathy Kennedy, Mary Gasiorowski, Melissa Clark, Janet Schlarb, Scott Beach, and the UCSUR interviewing team. Support for this work was provided by AG-13396 and AG-20677 and by RR-024153. Neither the University of Pittsburgh, nor the funding agencies necessarily holds the views reported in this paper.
Footnotes
CONFLICT OF INTEREST STATEMENT
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
REFERENCES
- Akerstedt T. Shift work and sleep disorders. Sleep. 2005;28:9–11. [PubMed] [Google Scholar]
- Buxton OM, Cain SW, O’Connor SP, Porter JH, Duffy JF, Wang W, Czeisler CA, Shea SA. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med. 2012;4:129ra43. doi: 10.1126/scitranslmed.3003200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71:1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- Costa G. Shift work and occupational medicine: an overview. Occup Med (Lond) 2003;53:83–88. doi: 10.1093/occmed/kqg045. [DOI] [PubMed] [Google Scholar]
- Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep. 2004;27:1453–1462. doi: 10.1093/sleep/27.8.1453. [DOI] [PubMed] [Google Scholar]
- Gale JE, Cox HI, Qian J, Block GD, Colwell CS, Matveyenko AV. Disruption of circadian rhythms accelerates development of diabetes through pancreatic beta-cell loss and dysfunction. J Biol Rhythms. 2011;26:423–433. doi: 10.1177/0748730411416341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people. Occup Environ Med. 2001;58:747–752. doi: 10.1136/oem.58.11.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, Huang ES, Korytkowski MT, Munshi MN, Odegard PS, et al. Diabetes in older adults: a consensus report. J Am Geriatr Soc. 2012;60:2342–2356. doi: 10.1111/jgs.12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007;11:163–178. doi: 10.1016/j.smrv.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci. 2008;1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke CH, Spiegelman D, Manson J, Schernhammer ES, Colditz GA, Kawachi I. Work characteristics and incidence of type 2 diabetes in women. Am J Epidemiol. 2007;165:175–183. doi: 10.1093/aje/kwj355. [DOI] [PubMed] [Google Scholar]
- Lin YC, Hsiao TJ, Chen PC. Persistent rotating shift-work exposure accelerates development of metabolic syndrome among middle-aged female employees: a five-year follow-up. Chronobiol Int. 2009;26:740–755. doi: 10.1080/07420520902929029. [DOI] [PubMed] [Google Scholar]
- Mitler MM, Carskadon MA, Czeisler CA, Dement WC, Dinges DF, Graeber RC. Catastrophes, sleep and public policy: consensus report. Sleep. 1988;11:100–109. doi: 10.1093/sleep/11.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monk TH. What can the chronobiologist do to help the shift worker? J Biol Rhythms. 2000;15:86–94. doi: 10.1177/074873040001500202. [DOI] [PubMed] [Google Scholar]
- Monk TH, Buysse DJ, Billy BD, Fletcher ME, Kennedy KS, Begley AE, Schlarb JE, Beach SR. Shiftworkers report worse sleep than day workers, even in retirement. J Sleep Res. 2013;22:201–208. doi: 10.1111/jsr.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagaya T, Yoshida H, Takahashi H, Kawai M. Markers of insulin resistance in day and shift workers aged 30-59 years. Int Arch Occup Environ Health. 2002;75:562–568. doi: 10.1007/s00420-002-0370-0. [DOI] [PubMed] [Google Scholar]
- Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 2011;8:e1001141. doi: 10.1371/journal.pmed.1001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietroiusti A, Neri A, Somma G, Coppeta L, Iavicoli I, Bergamaschi A, Magrini A. Incidence of metabolic syndrome among night-shift healthcare workers. Occup Environ Med. 2010;67:54–57. doi: 10.1136/oem.2009.046797. [DOI] [PubMed] [Google Scholar]
- Suwazono Y, Dochi M, Oishi M, Tanaka K, Kobayashi E, Sakata K. Shiftwork and impaired glucose metabolism: a 14-year cohort study on 7104 male workers. Chronobiol Int. 2009;26:926–941. doi: 10.1080/07420520903044422. [DOI] [PubMed] [Google Scholar]
- Toshihiro M, Saito K, Takikawa S, Takebe N, Onoda T, Satoh J. Psychosocial factors are independent risk factors for the development of type 2 diabetes in Japanese workers with impaired fasting glucose and/or impaired glucose tolerance. Diabet Med. 2008;25:1211–1217. doi: 10.1111/j.1464-5491.2008.02566.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Amelsvoort LG, Schouten EG, Kok FJ. Duration of shiftwork related to body mass index and waist to hip ratio. Int J Obes Relat Metab Disord. 1999;23:973–978. doi: 10.1038/sj.ijo.0801028. [DOI] [PubMed] [Google Scholar]
- Yoshizaki T, Kawano Y, Tada Y, Hida A, Midorikawa T, Hasegawa K, Mitani T, Komatsu T, Togo F. Diurnal 24-hour rhythm in ambulatory heart rate variability during the day shift in rotating shift workers. J Biol Rhythms. 2013;28:227–236. doi: 10.1177/0748730413489957. [DOI] [PubMed] [Google Scholar]