Abstract
Objective
Optimism and social support serve as protective factors against distress in medically ill patients. Very few studies have specifically explored the ways in which these variables interact to impact quality of life (QOL), particularly among patients with advanced cancer. The present study examined the role of optimism as a moderator of the relationship between social support and anxiety, depression, hopelessness, and QOL among patients with advanced cancer.
Methods
Participants (N = 168) completed self-report assessments of psychosocial, spiritual, and physical well-being, including social support, optimism, hopelessness, depressive and anxious symptoms, and QOL. Hierarchical multiple regression analyses were conducted to determine the extent to which social support and optimism were associated with depressive and anxious symptomatology, hopelessness and QOL, and the potential role of optimism as a moderator of the relationship between social support and these variables.
Results
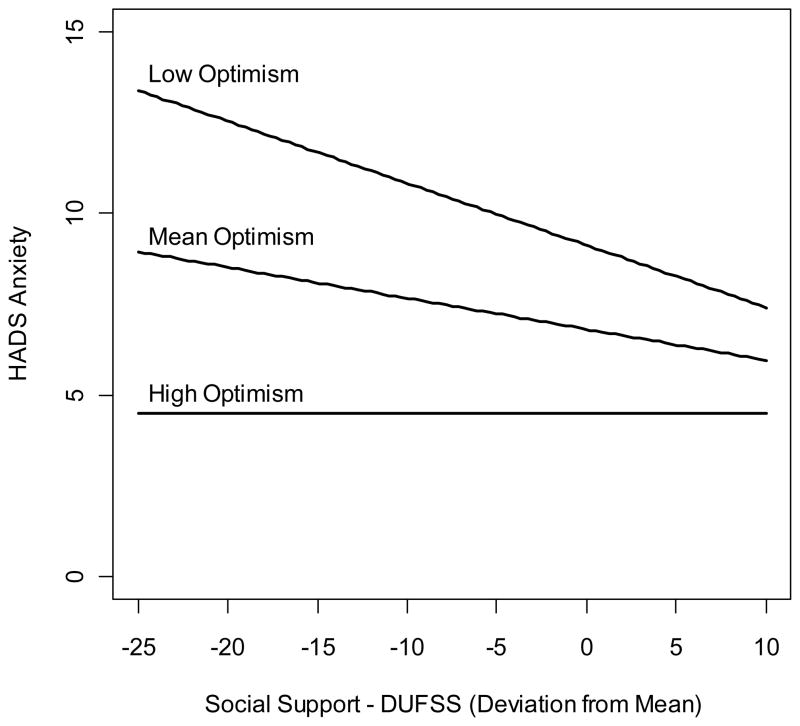
Higher levels of optimism were significantly associated with fewer anxious and depressive symptoms, less hopelessness and better QOL. Higher levels of perceived social support were also significantly associated with better QOL. Additionally, optimism moderated the relationship between social support and anxiety, such that there was a strong negative association between social support and anxiety for participants with low optimism.
Conclusions
This study highlights the importance of optimism and social support in the QOL of patients with advanced cancer. As such, interventions that attend to patients’ expectations for positive experiences and the expansion of social support should be the focus of future clinical and research endeavors.
Keywords: advanced cancer, optimism, social support, psychological distress, quality of life
A growing number of studies focus on variables that promote psychological resilience, or the capacity to continue functioning normally or even optimally soon after a traumatic event [1–3]. This literature extends to the field of psycho-oncology, where resilience has been associated with decreased psychiatric symptoms and improved quality of life (QOL) in patients with cancer and their caregivers [4–8]. Quality of life is a multidimensional construct, including physical, psychological, and social well-being [9]. Studies of resilience and QOL focus on variables that impact patients’ ability to successfully navigate the transitions of the cancer trajectory, from diagnosis and treatment, to survivorship and recurrences. Two variables that have received increasing attention as correlates of QOL and potential sources of resilience are optimism and social support.
Optimism is defined as the degree to which one expects positive experiences in the future [10]. It is positively associated with psychological well-being both in the general population and among medically ill patients [11]. This relationship holds for patients with cancer, among whom optimism is positively associated with psychological well-being and negatively associated with distress and depression [12, 13], and pessimism is positively associated with poorer health-related QOL [14] and increased anxiety and depression [15]. Several mechanisms driving the relationship between optimism and psychological well-being have been suggested, including higher expectations of the results of health related behaviors and the use of more adaptive coping strategies [11]. In what appears to be the only study of optimism among patients with metastatic cancer, optimism specifically regarding treatment outcome was negatively associated with psychological distress [16]. While an optimistic outlook specifically regarding survival and prognosis has the potential to negatively impact treatment decision making among patients with advanced cancer [17], there is evidence that maintaining a generally optimistic attitude, including optimism regarding the quality of life left to live, is associated with reduced anxious and depressive symptomatology among such patients [18].
Social support has also been widely examined across the psychiatric, medical, and sociological literature, and has been found to have beneficial effects on overall well-being. For example, social support serves as a protective factor against physical morbidity and mortality [19], protects against distress and psychopathology [20–22], and promotes psychological adjustment to chronic medical illnesses, including cancer [23, 24]. Among patients with cancer, social support is associated with fewer psychological symptoms and greater well-being [25–33], and appears to serve as a protective factor against negative health outcomes, including mortality [34]. There is also evidence that perceived social support may be more critical than actual support available or received in terms of these QOL outcomes [35, 36].
Similar to optimism, several mechanisms driving the relationship between social support and mental health outcomes have been suggested. Research suggests that social support promotes QOL through an enhancement of mood and sense of identity, a decrease in the burden associated with instrumental activities of daily living, positive appraisals of coping resources, and the provision of information [37]. Furthermore, in accord with the social-cognitive model of emotional adjustment to stressors, the discussion of stressors with supportive individuals can facilitate cognitive processing and adaptation to such stressors [38]. Social support may also help individuals focus on the positive aspects and potential benefits of a difficult situation [39], and is therefore connected to optimism.
While many studies have examined the unique relationships between optimism and social support on mental health outcomes, few have focused specifically on the ways in which these two variables might interact to promote psychological well-being. In the general population, it has been proposed that social support serves as either a mediator or moderator of the relationship between optimism and QOL [40–47]. Studies of cancer patients similarly suggest that these variables may serve as mediators and moderators for one another in relation to QOL [48–50]. For example, in their study of optimism and social support among breast cancer survivors, Trunzo and Pinto (2003) suggested that significant others may find it easier to provide support to more optimistic patients, as they may be less likely to place intense emotional demands on others and hence create less stressful social environments than less optimistic patients [50]. Indeed, there is evidence in the general population that optimistic individuals receive more positive responses from others than pessimistic individuals, and that an optimistic disposition attracts others and promotes the development of social support [40, 42, 51]. Optimists tend to have greater overall social support [52] and increases in social support during stressful experiences [42]. It is therefore likely that the potential beneficial impact of social support on mental health outcomes, such as anxiety and depression, may be greater for individuals who have low levels of optimism, and thus there may be a need for interventions that foster the development of social support among such individuals.
Currently, there is no consensus on the nature of the relationship between optimism, social support and mental health outcomes among patients with cancer and research has yet to examine these relationships specifically in patients with advanced cancer. Due to the high rates of psychological distress experienced by patients with advanced disease [53–55] and the unique protective benefits - including the promotion of resilience - conferred by optimism and social support, a clearer understanding of the ways in which these variables impact each other likely has significant implications for clinical practice. The purpose of this study was to examine the relationship between optimism, social support and mental health outcomes in patients with advanced cancer. Specifically, we examined the role of optimism as a moderator of the relationship between social support and depression, anxiety, hopelessness, and quality of life, variables which have each been shown to impact resilience among patients with cancer [56–59]. In light of previous research findings among patients with earlier stage disease, we hypothesized that the positive impact of social support on anxiety, depression, hopelessness and quality of life would be greater for patients with low levels of optimism.
Method
Participants and Procedures
Participants were recruited from outpatient clinics at Memorial Sloan-Kettering Cancer Center (MSKCC) in New York City between August 2007 and May 2012. Recruitment was primarily through posted flyers or physician referral, soliciting participants for a randomized controlled trial evaluating the impact of Meaning-Centered Group Psychotherapy (MCGP) on advanced cancer patients’ sense of meaning, psychological distress, and QOL. Eligible patients were diagnosed with stage III or IV solid tumor cancers or non-Hodgkin’s lymphoma, were ambulatory, over 18 years old, and English speaking. Patients were excluded if they had significant cognitive impairment or psychosis, or physical limitations that precluded participation in an outpatient group intervention. Prospective participants were informed of the risks and benefits of study participation and were provided written informed consent. The study was approved by the Institutional Review Boards of MSKCC and Fordham University. The data presented here represent a cross-section from patients recruited for the randomized trial of MCGP who completed the baseline assessment. This assessment was completed in person via paper-and-pencil measures before the initiation of the psychotherapy.
Measures
Life Orientation Test – Revised (LOT-R) [60]
The LOT-R is a ten-item scale with four items used as unscored fillers. Scores range from 0 to 24 with higher scores representing greater optimism. It was revised from the 12-item (four-item filler) version as a means of better assessing expectations of good versus bad outcomes. It has demonstrated a moderately high degree of internal consistency (Cronbach’s alpha of .78), discriminant validity with measures of anxiety (ρ=−.53 with Trait version of State-Trait Anxiety Inventory) and neuroticism (ρ=−.43 as assessed by Guilford-Zimmerman Temperament Survey), and convergent validity with measures of self-esteem (ρ=.50 with Rosenberg’s Self-Esteem Scale) and self-mastery (ρ=.48 with Self-Mastery Scale).
Hospital Anxiety and Depression Scale (HADS)[61]
The HADS is a 14-item self-rated questionnaire that has been well established as a measure of overall psychological distress in cancer patients, with Depression and Anxiety subscales of seven items each. It was developed without physical indicators of anxiety and depression so that it could be used with medically ill patients [61]. Scores range from 0 to 21 for each subscale, and cut-off scores for identifying clinically significant depression and anxiety range from eight [62, 63] to eleven [64]. Singer and colleagues demonstrated that the optimal diagnostic cutoff scores for use with a cancer population receiving acute care were ≥ 5 HADS-D (depression subscale), ≥ 7 HADS-A (anxiety subscale), and ≥ 13 HADS-T (total score) [65].
Beck Hopelessness Scale (BHS)[66]
The BHS is comprised of 20 true/false questions that assess degree of pessimism and hopelessness. Several studies have demonstrated a high degree of internal consistency (KR-20 mostly in the .90s) and concurrent validity (e.g., correlations of .74 with clinical ratings of hopelessness) [67]. Scores range from 0 to 20 with higher scores representing greater hopelessness.
Duke-UNC Functional Social Support Questionnaire (DUFSS) [68]
The DUFSS is an 8-item multidimensional, functional social support questionnaire that measures perceived social support [68]. The DUFSS is a reliable and valid self-report instrument that generates a total score representing overall social support, and two subscale scores corresponding to confidant support and affective support and has been used in studies with medically ill patients [69]. The measure has adequate demonstrated levels of internal consistency (Cronbach’s alpha of approximately .80-.85) and test-test reliability (.50-.77), as well as significant correlations with other measures of social functioning. Scores range from 8 to 40 with higher scores representing more perceived social support [70].
McGill Quality of Life Questionnaire (MQOL) [71]
This is a brief, self-report instrument designed to assess various domains of psychological, spiritual, and physical functioning among terminally ill patients. Patients rate their current functioning on a scale of 0 to 10. The physical and psychological domains of the MQOL are highly correlated with other measures of quality of life, although the existential/spiritual domain assessed by this measure has not typically been included in other QOL measures. The MQOL has demonstrated reliability (internal consistency > .70 for the non-physical subscales), and adequate levels of concurrent validity (e.g., correlation of .34 with the Spitzer Quality of Life Index; correlation of .48 with the Single Item Scale).
Additional data gathered at baseline included demographic (e.g., age, race, education, distance from home to treatment center) and clinical data (e.g., cancer diagnosis, stage of disease, Karnofsky Performance Rating Scale (KPRS)) [72, 73]. Demographic and clinical data were collected via self-report, but participants’ cancer diagnosis and stage was verified via review of medical records. KPRS was rated by the study staff.
Statistical Analyses
Separate hierarchical regression analyses, in which sets of variables were added sequentially, were conducted using IBM SPSS Statistics for Windows, version 20.0 (IBM Corp., Armonk, NY, Released 2011) for each of the four dependent psychological well-being variables (Hopelessness, Anxiety, Depression, and Quality of Life). Within each hierarchical regression, step 1 included demographic variables, step 2 added optimism, step 3 added social support, and step 4 added the interaction of optimism and social support. Based on previous studies, the demographic variables of age, gender, employment status, marital status, and education were analyzed for inclusion in the regressions [74–77]. Missing data were examined and ranged from 1–3% across study measures. Due to the small number affected, cases missing values were deleted from each regression analysis. A sensitivity analysis was conducted using mean substitution and differences in all cases were negligible.
Results
Demographic characteristics of the study sample are presented in Table 1. Of the 3,291 patients who were screened and found eligible for the study, 253 patients were consented to participate, and of these, 168 completed the baseline assessment. Participants were predominantly female (N=126, 75.0%) and white (N=132, 78.6%), on average, 58.4 years old (SD=11.3, range: 27 to 91), and had on average 16.1 years of education (SD = 2.4, range 9–23). Half of the sample (N=85, 50.6%) were partnered. The most common cancer site was breast (N = 56, 33.3%), followed by pancreas/liver/stomach/kidney (N = 34, 20.2%).
Table 1.
Sociodemographic and Medical Characteristics of Participants (N=168)
| Variable | N (%) |
|---|---|
| Sex | |
| Male | 42 (25.0) |
| Female | 126 (75.0) |
| Race | |
| White | 132 (78.6) |
| African American | 22 (13.1) |
| Other | 14 (8.3) |
| Ethnicity | |
| Hispanic/Latino | 21 (12.5) |
| Non-Hispanic/Latino | 145 (86.3) |
| Relationship Status | |
| Partnered | 85 (50.6) |
| Non-partnered | 83 (49.4) |
| Employment Status | |
| Working | 56 (33.3) |
| Retired | 46 (27.4) |
| Unemployed/disabled/homemaker/other | 66 (39.3) |
| Religion | |
| Catholic | 61 (36.3) |
| Protestant | 16 (9.5) |
| Jewish | 38 (22.6) |
| None | 16 (9.5) |
| Other | 37 (26.6) |
| Cancer Diagnosis | |
| Breast | 56 (33.3) |
| Colon/Rectal/Prostate/Testis | 27 (16.1) |
| Pancreas/Liver/Stomach/Kidney | 34 (20.2) |
| Lung/Bronchi | 28 (16.7) |
| Other | 23 (13.7) |
| Cancer Stage | |
| Stage III | 18 (10.7) |
| Stage IV | 148 (88.1) |
| Mean (SD) | |
|
| |
| Age | 58.4 (11.3) |
| Years of Education | 16.1 (2.4) |
In terms of the psychosocial variables, approximately 55% of participants had a score of 7 or higher on the HADS-A indicating clinically significant anxiety, and 52.7% of participants had a score of 5 or higher on the HADS-D indicating clinically significant depression [65]. Participants’ average score on BHS (M = 5.7, SD = 5.0) was indicative of moderate levels of hopelessness. Additionally, participants exhibited moderate levels of optimism (LOT-R, M = 17.1, SD = 5.7) and social support (DUFSS, M = 32.0, SD = 6.6), and average levels of QOL (MQOL, M = 6.6, SD = 1.7) [78].
Table 2 illustrates the Pearson product moment correlation coefficients among all study variables. Social support and optimism were moderately correlated (r = .34, p < .01), and consistent with previous findings, social support was negatively related to anxiety, depression, and hopelessness and positively related to QOL (r = −.34, r = −.34, r = −.35, and r = .43, ps < .01) [79, 80]. Optimism showed stronger negative correlations than social support with anxiety, depression and hopelessness (r = −.61, r = −.62, r = −.70, ps < .01), and a stronger positive correlation with quality of life (r = .64, p < .01). These correlations suggest no issues of multi-collinearity among the predictors, but do highlight the related nature of the four psychosocial outcome variables.
Table 2.
Correlations among Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Hopelessness (BHS) | -- | ||||||||||||||
| 2. Anxiety (HADS-A) | .52** | -- | |||||||||||||
| 3. Depression (HADS-D) | .69** | .58** | -- | ||||||||||||
| 4. Quality of Life (MQOL) | −.68** | −.60** | −.69** | -- | |||||||||||
| 5. Social Support (DUFSS) | −.35** | −.34** | −.34** | .43** | -- | ||||||||||
| 6. Optimism (LOT-R) | −.70** | −.61** | −.62** | .64** | .34** | -- | |||||||||
| 7. Gender (Female) | .10 | .18* | .07 | −.13 | −.06 | −.12 | -- | ||||||||
| 8. Age | .01 | −.17* | .04 | .10 | .00 | .19* | .05 | -- | |||||||
| 9. Marital Status (Partnered) | .18* | .05 | .16* | −.15 | −.23** | −.10 | .24** | .17* | -- | ||||||
| 10. Retired | −.06 | −.14 | .05 | .06 | .09 | .15 | −.11 | .48** | .06 | -- | |||||
| 11. Working | −.26** | −.16* | −.24** | .23** | .24** | .21** | −.06 | −.18* | −.09 | −.43** | -- | ||||
| 12. Education (Yrs) | .02 | −.03 | −.06 | −.07 | .13 | .09 | .11 | .06 | −.02 | −.13 | .13 | -- | |||
| 13. Race (Non-Caucasian) | −.09 | .02 | .02 | −.04 | −.01 | .03 | .13 | −.10 | .05 | −.02 | −.02 | −.12 | -- | ||
| 14. Ethnicity (Hispanic) | −.09 | .04 | −.01 | .03 | −.10 | .01 | −.03 | −.20* | −.09 | −.07 | .04 | −.25** | − .26** | -- | |
| 15. Cancer Diagnosis | .04 | −.09 | .09 | .12 | .03 | .08 | −.33** | .17* | −.12 | .12 | .06 | −.03 | .16* | −.10 | -- |
p < .05;
p < .01 (n=168)
Regression Analyses
Separate hierarchical regression analyses were conducted for each of the four psychosocial outcome variables (anxiety, depression, hopelessness, and QOL). Marital status, employment status, gender, and age were controlled for in step 1, as these demonstrated significant correlations with the outcome measures (Table 3). Social support was entered in step 2 and optimism in step 3. The interaction between social support and optimism was entered in step 4 of the regression analyses. Additionally, social support and optimism were centered to reduce issues of multicollinearity with the interaction variable, and age was centered to improve interpretability.
Table 3.
Changes in R2 in Each Step of the Hierarchical Regression Analyses
| Psychological Well-Being Variables | Step 1: Sociodemographics | Step 2: Social Support | Step 3: Optimism | Step 4: Interaction | Total R2 |
|---|---|---|---|---|---|
| Anxiety | .116** | .075** | .216** | .020* | 0.426** |
| Depression | .078* | .066** | .296** | .001 | 0.440** |
| Hopelessness | .125** | .051** | .356** | .004 | 0.537** |
| Quality of Life | .109** | .116** | .243** | .006 | 0.474** |
p < .05;
p < .01
Overall, the amount of explained variance in each of the four outcomes ranged from 42.6% for anxiety to 53.7% for hopelessness (Table 3), with more than half of the explained variance coming from the addition of optimism as a predictor. The demographic variables accounted for 7.8%–12.5%, and the addition of social support accounted for 5.1%–11.6% of the variance in the outcome variables.
As can be seen in the standardized regression coefficients resulting from the full regression completed in step 4 (Table 4), higher optimism was significantly associated with fewer anxious and depressive symptoms, lower levels of hopelessness, and higher QOL (β=−.500, β=−.611, β=−.659, β=.538, ps<.001, respectively). Higher social support was also significantly associated with higher QOL (β=.204, p=.003).
Table 4.
Standardized Regression Coefficients of Social Support, Optimism, and Sociodemographic Variables from Full Regression (Step 4)
| Predictors | Psychological Well-Being
|
|||
|---|---|---|---|---|
| Anxiety | Depression | Hopelessness | Quality of Life | |
| Social Support | −.123 | −.117 | −.060 | .204** |
| Optimism | −.500** | −.611** | −.659** | .538** |
| Interaction – Social Support and Optimism | .153* | .029 | .071 | −.087 |
| Sociodemographics: | ||||
| Gender | .108 | −.048 | −.030 | −.043 |
| Age | −.059 | .088 | .120 | .038 |
| Marital Status | −.056 | .034 | .070 | −.025 |
| Employment Status: | ||||
| Working | −.013 | −.017 | −.077 | .019 |
| Retired | −.018 | .113 | −.050 | −.063 |
p < .05;
p < .01
Note: Regression coefficients are standardized for purposes of comparison. However, p-values are based on unstandardized regression coefficients.
Our examination of the role of optimism as a moderator of social support uncovered a significant interaction between optimism and social support in the outcome of anxiety (β=.153, p=.024). Figure 1 illustrates how, among participants with low optimism (one standard deviation below the mean), higher social support was associated with fewer anxious symptoms, while among participants with high optimism (one standard deviation above the mean), there was no relationship between social support and anxiety.
Figure 1.
Discussion
This is the first study to examine the relationship between optimism and social support and mental health outcomes in patients with advanced cancer. Optimism was significantly associated with fewer anxious and depressive symptoms, less hopelessness and better QOL, while social support was significantly associated with better QOL. As previously noted, there is evidence that both optimism and social support are associated with improved overall well-being for cancer patients [12–15, 25–32, 81] and these results extend such findings to patients with advanced cancer. Our findings, however, highlight a particularly robust role for optimism in mental health outcomes for patients with advanced cancer, which may be a reflection of the importance of attitude when confronting the challenges of end of life issues.
Additionally, optimism emerged as a moderator of the relationship between social support and anxiety. Among participants with low optimism, social support was associated with fewer anxious symptoms, while among participants with high optimism, social support was not associated with fewer anxious symptoms. As noted previously [40, 42, 82], optimistic individuals are responded to more positively than pessimistic individuals and an optimistic disposition attracts others and promotes the development of social support. It is possible that for individuals with low levels of optimism, increases in social support may have been experienced as more meaningful than similar increases for individuals with high levels of optimism, for whom social support was more consistent. It is also possible that, for individuals with high levels of optimism for whom social support is generally present, additional social support may signal to the patient decreasing health status, as family and friends traditionally increase their support as cancer patients’ physical well-being declines [83]. This may account for why increases in social support for these patients did not translate into decrease in anxious symptomatology. Additionally, as anxiety may be more malleable than other types of distress examined here, it may have been more susceptible to the influence of social support than depression or hopelessness. Importantly, in light of the small effect size found here, it is also possible that this interaction was due to chance. Future studies with larger samples are needed to provide additional evidence for this specific relationship between social support and anxiety.
Interestingly, optimism and social support were relatively high in this sample. This may be due to the high level of education of participants, as increased education has been associated with high levels of optimism [74, 84]. Moreover, individuals with higher levels of optimism may be more likely to believe a psychotherapy group will be beneficial to them and accordingly more likely to enroll in such an intervention. Additionally, the high levels of optimism and social support in this sample may explain their relatively low levels of psychopathology. Indeed, higher levels of optimism are generally associated with improved psychological functioning in cancer patients [12, 15, 85] and social support has been found to minimize the risk of psychological distress [20]. There is also evidence that optimism may be higher among patients with cancer than among individuals in the general population [86]. It is possible that the experience among many cancer patients across the disease trajectory of periods of medical challenges and then well-being may foster a deeper appreciation for life and an optimistic outlook.
Limitations
Several limitations of this study should be acknowledged. The demographic profile of participants, and in particular, the high level of education, underrepresentation of ethnic minorities and exclusion of those who lacked English fluency, limit our findings’ generalizability. Additionally, the sample’s comparatively low level of psychopathology precludes comparisons to samples of medically ill patients who exhibited more significant psychiatric symptomatology. Moreover, the study sample consisted entirely of individuals who agreed to participate in a randomized controlled clinical trial of a novel group psychotherapy that was free of charge. While complementary participation may have attracted individuals who could not on their own afford psychiatric treatment, participants were limited to those who had the financial and temporal resources needed to commit to travel to and participate in eight in-person group therapy sessions, in addition to being interested in receiving such support. This latter point is particularly important in light of this study’s focus on social support. Also, while the sample size was adequate for the investigation of main effects, it may have been underpowered to detect the interaction effects given the small effect sizes. Finally, conclusions regarding causal relationships between any of the variables examined cannot be drawn due to the cross-sectional design of this study.
Conclusions and Future Directions
This study highlights the significance of optimism and social support in the QOL of patients with advanced cancer. In light of the importance of addressing psychopathology among these patients [87], future studies should include more comprehensive examinations of variables that impact mental health and well-being, such as optimism and social support. While challenging in the setting of managed care, the incorporation of screening for these variables into routine clinical care will allow for the prompt identification and referral of patients with low levels of optimism and social support to psychosocial programs that either directly provide (e.g., through group psychotherapy) or facilitate (e.g., through focused interventions targeting the expansion of social support networks) social support, and promote the recognition of the possibility of benefit and growth despite suffering (e.g., meaning-centered interventions [88]). This will ultimately foster resilience and serve as a protective factor against psychopathology among patients with advanced cancer.
Footnotes
Conflict of interest:
There is no conflict of interest.
References
- 1.Bonanno GA. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? The American Psychologist. 2004;59(1):20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- 2.Bonanno GA, Kennedy P, Galatzer-Levy IR, Lude P, Elfstrom ML. Trajectories of resilience, depression, and anxiety following spinal cord injury. Rehabilitation Psychology. 2012;57(3):236–247. doi: 10.1037/a0029256. [DOI] [PubMed] [Google Scholar]
- 3.Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annual Review of Clinical Psychology. 2011;7:511–535. doi: 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- 4.Wu LM, Sheen JM, Shu HL, Chang SC, Hsiao CC. Predictors of anxiety and resilience in adolescents undergoing cancer treatment. Journal of Advanced Nursing. 2013;69(1):158–166. doi: 10.1111/j.1365-2648.2012.06003.x. [DOI] [PubMed] [Google Scholar]
- 5.Schrier M, Amital D, Arnson Y, Rubinow A, Altaman A, Nissenabaum B, et al. Association of fibromyalgia characteristics in patients with non-metastatic breast cancer and the protective role of resilience. Rheumatology International. 2012;32(10):3017–3023. doi: 10.1007/s00296-011-2104-7. [DOI] [PubMed] [Google Scholar]
- 6.Loprinzi CE, Prasad K, Schroeder DR, Sood A. Stress Management and Resilience Training (SMART) program to decrease stress and enhance resilience among breast cancer survivors: a pilot randomized clinical trial. Clinical Breast Cancer. 2011;11(6):364–368. doi: 10.1016/j.clbc.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Mays D, Black JD, Mosher RB, Heinly A, Shad AT, Tercyak KP. Efficacy of the Survivor Health and Resilience Education (SHARE) program to improve bone health behaviors among adolescent survivors of childhood cancer. Annals of Behavioral Medicine. 2011;42(1):91–98. doi: 10.1007/s12160-011-9261-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hou WK, Law CC, Yin J, Fu YT. Resource loss, resource gain, and psychological resilience and dysfunction following cancer diagnosis: a growth mixture modeling approach. Journal of Health Psychology. 2010;29(5):484–495. doi: 10.1037/a0020809. [DOI] [PubMed] [Google Scholar]
- 9.Felce D, Perry J. Quality of life: its definition and measurement. Research in Developmental Disabilities. 1995;16(1):51–74. doi: 10.1016/0891-4222(94)00028-8. [DOI] [PubMed] [Google Scholar]
- 10.Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Journal of Health Psychology. 1985;4(3):219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 11.Scheier MF, Carver CS. Effects of optimism on pychological and physical well-being: Theoretical overview and empirical update. Cognitive Therapy and Research. 1992;16(2):201–228. [Google Scholar]
- 12.Miller DL, Manne SL, Taylor K, Keates J, Dougherty J. Psychological distress and well-being in advanced cancer: The effects of optimism and coping. Journal of Clinical Psychology in Medical Settings. 1996;3(2):115–130. doi: 10.1007/BF01996132. [DOI] [PubMed] [Google Scholar]
- 13.Horney DJ, Smith HE, McGurk M, Weinman J, Herold J, Altman K, et al. Associations between quality of life, coping styles, optimism, and anxiety and depression in pretreatment patients with head and neck cancer. Head & Neck. 2011;33(1):65–71. doi: 10.1002/hed.21407. [DOI] [PubMed] [Google Scholar]
- 14.Petersen LR, Clark MM, Novotny P, Kung S, Sloan JA, Patten CA, et al. Relationship of optimism-pessimism and health-related quality of life in breast cancer survivors. Journal of Psychosocial Oncology. 2008;26(4):15–32. doi: 10.1080/07347330802359578. [DOI] [PubMed] [Google Scholar]
- 15.Schou I, Ekeberg O, Ruland CM, Sandvik L, Karesen R. Pessimism as a predictor of emotional morbidity one year following breast cancer surgery. Psycho-Oncology. 2004;13(5):309–320. doi: 10.1002/pon.747. [DOI] [PubMed] [Google Scholar]
- 16.Cohen L, de Moor C, Amato RJ. The association between treatment-specific optimismand depressive symptomatology in patients enrolled in a Phase I cancer clinical trial. Cancer. 2001;91(10):1949–1955. doi: 10.1002/1097-0142(20010515)91:10<1949::aid-cncr1218>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 17.Applebaum A, Kolva E, Kulikowski J, Jacobs J, DeRosa A, Lichtenthal W, Olden M, Rosenfeld B, Breitbart B. Conceptualizing prognostic awareness in advanced cancer: A systematic review. Journal of Health Psychology. 2013 Oct 24; doi: 10.1177/1359105313484782. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Winterling J, Wasteson E, Sidenvall B, Sidenvall E, Glimelius B, Sjoden PO, Nordin K. Relevance of philosophy of life and optimism for psychological distress among individuals in a stage where death is approaching. Supportive Care in Cancer. 2006;14(4):310–319. doi: 10.1007/s00520-005-0870-z. [DOI] [PubMed] [Google Scholar]
- 19.House JS, Landis KR, Umberson D. Social Relationships and Health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 20.Smith SK, Herndon JE, Lyerly HK, Coan A, Wheeler JL, Staley T, et al. Correlates of quality of life-related outcomes in breast cancer patients participating in the Pathfinders pilot study. Psycho-Oncology. 2011;20(5):559–564. doi: 10.1002/pon.1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sarason BR, Sarason IG, Gurung RAR. Close personal relationships and health outcomes: A key to the role of social support. In: Duck S, editor. Handbook of Personal Relationships. Wiley; New York: 1997. pp. 547–573. [Google Scholar]
- 22.Lin N, Ye X, Ensel WM. Social support and depressed mood: A structural analysis. Journal of Health and Social Behavior. 1999;40(4):344–359. [PubMed] [Google Scholar]
- 23.Penninx BWJH, van Tilburg T, Boeke AJP, Deeg DJH, Kriegsman DMW, van Eijk JTM. Effects of social support and personal coping resources on depressive symptoms: Different for various chronic diseases? Health Psychology. 1998;17(6):551–558. doi: 10.1037//0278-6133.17.6.551. [DOI] [PubMed] [Google Scholar]
- 24.Stone AA, Mezzacappa ES, Donatone BA, Gonder M. Psychosocial stress and social support are associated with prostate-specific antigen levels in men: Results from a community screening program. Health Psychology. 1999;18(5):482–486. doi: 10.1037//0278-6133.18.5.482. [DOI] [PubMed] [Google Scholar]
- 25.Andrykowski MA, Cordova MJ. Factors associated with PTSD symptoms following treatment for breast cancer: test of the Andersen model. Journal of Traumatic Stress. 1998;11(2):189–203. doi: 10.1023/A:1024490718043. [DOI] [PubMed] [Google Scholar]
- 26.Bowers B. Providing effective support for patients facing disfiguring surgery. British Journal of Nursing. 2008;17(2):94–98. doi: 10.12968/bjon.2008.17.2.28135. [DOI] [PubMed] [Google Scholar]
- 27.Deno M, Tashiro M, Miyashita M, Asakage T, Takahashi K, Saito K, et al. The mediating effects of social support and self-efficacy on the relationship between social distress and emotional distress in head and neck cancer outpatients with facial disfigurement. Psycho-Oncology. 2012;21(2):144–152. doi: 10.1002/pon.1877. [DOI] [PubMed] [Google Scholar]
- 28.Maunsell E, Brisson J, Deschenes L. Social support and survival among women with breast cancer. Cancer. 1995;76(4):631–637. doi: 10.1002/1097-0142(19950815)76:4<631::aid-cncr2820760414>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 29.Rodin G, Walsh A, Zimmermann C, Gagliese L, Jones J, Shepherd FA, et al. The contribution of attachment security and social support to depressive symptoms in patients with metastatic cancer. Psycho-Oncology. 2007;16(12):1080–1091. doi: 10.1002/pon.1186. [DOI] [PubMed] [Google Scholar]
- 30.Schnoll RA, Mackinnon JR, Stolbach L, Lorman C. The relationship between emotional adjustment and two factor structures of the Mental Adjustment to Cancer (MAC) scale. Psycho-Oncology. 1995;4(4):265–272. [Google Scholar]
- 31.Schroevers MJ, Helgeson VS, Sanderman R, Ranchor AV. Type of social support matters for prediction of posttraumatic growth among cancer survivors. Psycho-Oncology. 2010;19(1):46–53. doi: 10.1002/pon.1501. [DOI] [PubMed] [Google Scholar]
- 32.Schwarzer R, Luszczynska A, Boehmer S, Taubert S, Knoll N. Changes in finding benefit after cancer surgery and the prediction of well-being one year later. Social Science and Medicine. 2006;63(6):1614–1624. doi: 10.1016/j.socscimed.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 33.Nenova M, DuHamel K, Zemon V, Rini C, Redd WH. Posttraumatic growth, social support, and social constraint in hematopoietic stem cell transplant survivors. Psycho-Oncology. 2013;22(1):195–202. doi: 10.1002/pon.2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Levin T, Kissane DW. Psychooncology – the state of its development in 2006. European Journal of Psychiatry. 2006;20(3):183–197. [Google Scholar]
- 35.Wethington E, Kessler RC. Perceived support, received support, and adjustment to stressful life events. Journal of Health and Social Behavior. 1986;27(1):78–89. [PubMed] [Google Scholar]
- 36.Dunkel-Schetter C, Bennett TL. Differentiating the cognitive and behavioral aspects of social support. In: Sarason BR, Sarason IG, Pierce GR, editors. Social Support: An Interactional View. John Wiley & Sons, Inc; New York: 1990. pp. 267–296. [Google Scholar]
- 37.Helgeson VS. Social support and quality of life. Quality of Life Research. 2003;12 (Suppl 1):25–31. doi: 10.1023/a:1023509117524. [DOI] [PubMed] [Google Scholar]
- 38.Lepore SJ, Silver RC, Wortman CB, Wayment HA. Social constraints, intrusive thoughts, and depressive symptoms among bereaved mothers. Journal of Personality and Social Psychology. 1996;70(2):271–282. doi: 10.1037//0022-3514.70.2.271. [DOI] [PubMed] [Google Scholar]
- 39.Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social Behavior. 1978;19(1):2–21. [PubMed] [Google Scholar]
- 40.Brissette I, Scheier MF, Carver CS. The role of optimism in social network development, coping, and psychological adjustment during a life transition. Journal of Personality and Social Psychology. 2002;82(1):102–111. doi: 10.1037//0022-3514.82.1.102. [DOI] [PubMed] [Google Scholar]
- 41.Cannella BL. Mediators of the relationship between social support and positive health practices in pregnant women. Nursing Research. 2006;55(6):437–445. doi: 10.1097/00006199-200611000-00008. [DOI] [PubMed] [Google Scholar]
- 42.Dougall AL, Hyman KB, Hayward MC, McFeeley S, Baum A. Optimism and traumatic stress: The importance of social support and coping. Journal of Applied Social Psychology. 2001;31(2):223–245. [Google Scholar]
- 43.Ekas NV, Lickenbrock DM, Whitman TL. Optimism, social support, and well-being in mothers of children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2010;40(10):1274–1284. doi: 10.1007/s10803-010-0986-y. [DOI] [PubMed] [Google Scholar]
- 44.Ferguson SJ, Goodwin AD. Optimism and well-being in older adults: the mediating role of social support and perceived control. International Journal of Aging & Human Development. 2010;71(1):43–68. doi: 10.2190/AG.71.1.c. [DOI] [PubMed] [Google Scholar]
- 45.Khan A, Husain A. Social support as a moderator of positive psychological strengths and subjective well-being. Psychological Reports. 2010;106(2):534–538. doi: 10.2466/pr0.106.2.534-538. [DOI] [PubMed] [Google Scholar]
- 46.Mosher CE, Prelow HM, Chen WW, Yackel ME. Coping and social support as mediators of the relation of optimism to depressive symptoms among black college students. Journal of Black Psychology. 2006;32(1):72–86. [Google Scholar]
- 47.Rius-Ottenheim N, Kromhout D, van der Mast RC, Zitman FG, Geleijnse JM, Giltay EJ. Dispositional optimism and loneliness in older men. International Journal of Geriatric Psychiatry. 2012;27(2):151–159. doi: 10.1002/gps.2701. [DOI] [PubMed] [Google Scholar]
- 48.Bozo O, Gundogdu E, Buyukasik-Colak C. The moderating role of different sources of perceived social support on the dispositional optimism--posttraumatic growth relationship in postoperative breast cancer patients. Journal of Health Psychology. 2009;14(7):1009–1020. doi: 10.1177/1359105309342295. [DOI] [PubMed] [Google Scholar]
- 49.Shelby RA, Crespin TR, Wells-Di Gregorio SM, Lamdan RM, Siegel JE, Taylor KL. Optimism, social support, and adjustment in African American women with breast cancer. Journal of Behavioral Medicine. 2008;31(5):433–444. doi: 10.1007/s10865-008-9167-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Trunzo JJ, Pinto BM. Social support as a mediator of optimism and distress in breast cancer survivors. Journal of Consulting and Clinical Psychology. 2003;71(4):805–811. doi: 10.1037/0022-006x.71.4.805. [DOI] [PubMed] [Google Scholar]
- 51.Carver CS, Kus LA, Scheier MF. Effects of good versus bad mood and optimistic versus pessimistic outlook on social acceptance versus rejection. Journal of Social and Clinical Psychology. 1994;13(2):138–151. [Google Scholar]
- 52.Park CL, Folkman S. Stability and change in psychosocial resources during caregiving and bereavement in partners of men with AIDS. Journal of Personality. 1997;65(2):421–447. doi: 10.1111/j.1467-6494.1997.tb00960.x. [DOI] [PubMed] [Google Scholar]
- 53.Zabora JR, Blanchard CG, Smith ED, Roberts CS, Glajchen M, Sharp JWHedlund SC. Prevalence of psychological distress among cancer patients across the disease continuum. Journal of Psychosocial Oncology. 1997;15(2):73–87. [Google Scholar]
- 54.Potash M, Breitbart W. Affective disorders in advanced cancer. Hematology-Oncology Clinics of North America. 2002;16(3):671–700. doi: 10.1016/s0889-8588(02)00013-8. [DOI] [PubMed] [Google Scholar]
- 55.Miovic M, Block S. Psychiatric disorders in advanced cancer. Cancer. 2007;110(8):1665–1676. doi: 10.1002/cncr.22980. [DOI] [PubMed] [Google Scholar]
- 56.Hou WK, Lam JH. Resilience in the year after cancer diagnosis: a cross-lagged panel analysis of the reciprocity between psychological distress and well-being. Journal of Behavioral Medicine. 2013 doi: 10.1007/s10865-013-9497-6. [DOI] [PubMed] [Google Scholar]
- 57.Llewellyn CD, Horney DJ, McGurk M, Weinman J, Herold J, Altman K, Smith HE. Assessing the psychological predictors of benefit finding in patients with head and neck cancer. Psycho-oncology. 2013;22(1):97–105. doi: 10.1002/pon.2065. [DOI] [PubMed] [Google Scholar]
- 58.Min JA, Yoon S, Lee CU, Chae JH, Lee C, Song KY, Kim TS. Psychological resilience contributes to low emotional distress in cancer patients. Suppotive Care in Cancer. 2013;21(9):2469–2476. doi: 10.1007/s00520-013-1807-6. [DOI] [PubMed] [Google Scholar]
- 59.Teall T, Barrera M, Barr R, Silva M, Greenberg M. Psychological resilience in adolescent and young adult survivors of lower extremity bone tumors. Pediatric Blood Cancer. 2013;60(7):1223–1230. doi: 10.1002/pbc.24441. [DOI] [PubMed] [Google Scholar]
- 60.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem) - a reevaluation of the life orientation test. Journal of Personality and Social Psychology. 1994;67(6):1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 61.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiat Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 62.Carroll BT, Kathol RG, Noyes R, Jr, Wald TG, Clamon GH. Screening for depression and anxiety in cancer patients using the Hospital Anxiety and Depression Scale. General Hospital Psychiatry. 1993;15(2):69–74. doi: 10.1016/0163-8343(93)90099-a. [DOI] [PubMed] [Google Scholar]
- 63.Moorey S, Greer S, Watson M, Gorman C, Rowden L, Tunmore R, et al. The factor structure and factor stability of the hospital anxiety and depression scale in patients with cancer. The British Journal of Psychiatry. 1991;158:255–259. doi: 10.1192/bjp.158.2.255. [DOI] [PubMed] [Google Scholar]
- 64.Hopwood P, Howell A, Maguire P. Screening for psychiatric morbidity in patients with advanced breast cancer: validation of two self-report questionnaires. British Journal of Cancer. 1991;64(2):353–356. doi: 10.1038/bjc.1991.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Singer S, Kuhnt S, Gotze H, Hauss J, Hinz A, Liebmann A, et al. Hospital anxiety and depression scale cutoff scores for cancer patients in acute care. British Journal of Cancer. 2009;100(6):908–912. doi: 10.1038/sj.bjc.6604952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Beck AT, Weissman A, Lester D, Trexler L. Measurement of Pessimism - Hopelessness Scale. Journal of Consulting and Clinical Psychology. 1974;42(6):861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 67.Fernandez E. Review of the test Beck Hopelessness Scale [Revised] The Thirteenth Mental Measurements Yearbook. 1998 [Google Scholar]
- 68.Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH. The Duke-UNC Functional Social Support Questionnaire. Measurement of social support in family medicine patients. Medical Care. 1988;26(7):709–723. doi: 10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- 69.Broadhead WE, Gehlbach SH, deGruy FV, Kaplan BH. Functional versus structural social support and health care utilization in a family medicine outpatient practice. Medical Care. 1989;27(3):221–233. doi: 10.1097/00005650-198903000-00001. [DOI] [PubMed] [Google Scholar]
- 70.McDowell I. Measuring Health: A Guide to Rating Scales and Questionnaires. 3. Oxford Univeristy Press; New York: 2006. [Google Scholar]
- 71.Cohen SR, Mount BM, Strobel MG, Bui F. The McGill Quality of Life Questionnaire: a measure of quality of life appropriate for people with advanced disease. A preliminary study of validity and acceptability. Palliative Medicine. 1995;9(3):207–219. doi: 10.1177/026921639500900306. [DOI] [PubMed] [Google Scholar]
- 72.Karnofsky DA, Burchenal JH. The clinical evaluation of chemotherapeutic agents in cancer. In: MacLeod CM, editor. Evaluation of Chemotherapeutic Agents. Columbia University Press; 1949. p. 196. [Google Scholar]
- 73.Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: reliability, validity, and guidelines. Journal of Clinical Oncology. 1984;2(3):187–193. doi: 10.1200/JCO.1984.2.3.187. [DOI] [PubMed] [Google Scholar]
- 74.Mazanec SR, Daly BJ, Douglas SL, Lipson AR. The relationship between optimism and quality of life in newly diagnosed cancer patients. Cancer Nursing. 2010;33(3):235–243. doi: 10.1097/NCC.0b013e3181c7fa80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dunn J, Occhipinti S, Campbell A, Ferguson M, Chambers SK. Benefit finding after cancer: the role of optimism, intrusive thinking and social environment. Journal of Health Psychology. 2011;16(1):169–177. doi: 10.1177/1359105310371555. [DOI] [PubMed] [Google Scholar]
- 76.Matthews EE, Cook PF. Relationships among optimism, well-being, self-transcendence, coping, and social support in women during treatment for breast cancer. Psycho-Oncology. 2009;18(7):716–726. doi: 10.1002/pon.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rini C, Redd WH, Austin J, Mosher CE, Meschian YM, Isola L, et al. Effectiveness of partner social support predicts enduring psychological distress after hematopoietic stem cell transplantation. Journal of Consulting and Clinical Psychology. 2011;79(1):64–74. doi: 10.1037/a0022199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Cohen SR, Mount BM. Living with cancer: “good” days and “bad” days--what produces them? Can the McGill quality of life questionnaire distinguish between them? Cancer. 2000;89(8):1854–1865. doi: 10.1002/1097-0142(20001015)89:8<1854::aid-cncr28>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 79.Mehnert A, Lehmann C, Graefen M, Huland H, Koch U. Depression, anxiety, post-traumatic stress disorder and health-related quality of life and its association with social support in ambulatory prostate cancer patients. European Journal of Cancer Care. 2010;19(6):736–745. doi: 10.1111/j.1365-2354.2009.01117.x. [DOI] [PubMed] [Google Scholar]
- 80.Helgeson VS, Cohen S. Social support and adjustment to cancer: reconciling descriptive, correlational, and intervention research. Journal of Health Psychology. 1996;15(2):135–148. doi: 10.1037//0278-6133.15.2.135. [DOI] [PubMed] [Google Scholar]
- 81.Nenova M, Duhamel K, Zemon V, Rini C, Redd WH. Posttraumatic growth, social support, and social constraint in hematopoietic stem cell transplant survivors. Psycho-Oncology. 2011 doi: 10.1002/pon.2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Carver CS, Kus LA, Scheier MF. Effects of Good Versus Bad Mood and Optimistic Versus Pessimistic Outlook on Social Acceptance Versus Rejection. Journal of Social and Clinical Psychology. 1994;13(2):138–151. [Google Scholar]
- 83.Rolland JS. Chronic illness and the life cycle: a conceptual framework. Family Process. 1987;26(2):203–221. doi: 10.1111/j.1545-5300.1987.00203.x. [DOI] [PubMed] [Google Scholar]
- 84.Glaesmer H, Rief W, Martin A, Mewes R, Brahler E, Zenger M, et al. Psychometric properties and population-based norms of the Life Orientation Test Revised (LOT-R) British Journal of Health Psychology. 2012;17(2):432–445. doi: 10.1111/j.2044-8287.2011.02046.x. [DOI] [PubMed] [Google Scholar]
- 85.Carver CS, Pozo-Kaderman C, Harris SD, Noriega V, Scheier MF, Robinson DS, et al. Optimism versus pessimism predicts the quality of women’s adjustment to early stage breast cancer. Cancer. 1994;73(4):1213–1220. doi: 10.1002/1097-0142(19940215)73:4<1213::aid-cncr2820730415>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 86.Stiegelis HE, Hagedoorn M, Sanderman R, van der Zee KI, Buunk BP, van den Bergh AC. Cognitive adaptation: a comparison of cancer patients and healthy references. British Journal of Health Psychology. 2003;8(Pt 3):303–318. doi: 10.1348/135910703322370879. [DOI] [PubMed] [Google Scholar]
- 87.Kadan-Lottick NS, Vanderwerker LC, Block SD, Zhang B, Prigerson HG. Psychiatric disorders and mental health service use in patients with advanced cancer: a report from the coping with cancer study. Cancer. 2005;104(12):2872–2881. doi: 10.1002/cncr.21532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Breitbart W, Rosenfeld B, Gibson C, Pessin H, Poppito S, Nelson C, Olden M. Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psycho-oncology. 2010;19(1):21–28. doi: 10.1002/pon.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]