Abstract
Surgical knots are simply a necessary evil needed to anchor smooth suture to allow it to function in its role in tissue reapproximation. Surgical knots reduce the tensile strength of all sutures by thinning and stretching the material. The tying of surgical knots introduces the potential of human error and interuser variability. Knot-secured smooth suture must create an uneven distribution of tension across the wound with the higher tension burdens placed at the knots. Given the excessive relative wound tension on the knot and the reasonable concerns of surgeons for suture failure due to knot slippage, there is a natural tendency toward overcoming these concerns by over-tightening knots; however, tighter knots may be worse for wound healing and strength than looser knots. In minimally invasive laparoscopic surgeries, the ability to quickly and properly tie surgical knots presents a new challenge. In cases in which knot tying is difficult, the use of knotless barbed suture can securely reapproximate tissues with less time, cost, and aggravation. This article reviews the technology behind barbed sutures with a focus on understanding how they differ from traditional smooth sutures and how barbed sutures have performed in in vitro and animal model testing, as well as in human clinical trials.
Key words: Laparoscopic myomectomy, Barbed suture, Smooth suture, Soft tissue reapproximation
In 2008, Greenberg and Einarsson1 reported the first use of a barbed suture for tissue reapproximation in a laparoscopic myomectomy. In the 5 years since that early report, the use of barbed suture in obstetric and gynecologic procedures has exploded, with tens of thousands of these operations now employing this technology. This article reviews the technology behind barbed sutures with a focus on understanding how they differ from traditional smooth sutures and how barbed sutures have performed in in vitro and animal model testing, as well as in human clinical trials.
Why Not Knots?
A full appreciation of the technical advantages of barbed sutures necessitates a basic understanding of the downside of surgical knots. To most surgeons, knots are as integral to the use of suture as gasoline once was to the operation of automobiles—that is, it is difficult to imagine the proper functioning of one component without the other. Yet surgical knots are simply a necessary evil needed to anchor smooth suture to allow it to function in its role in tissue reapproximation. Other than its anchoring function, the surgical knot offers no benefit whatsoever and introduces a variety of untoward features.
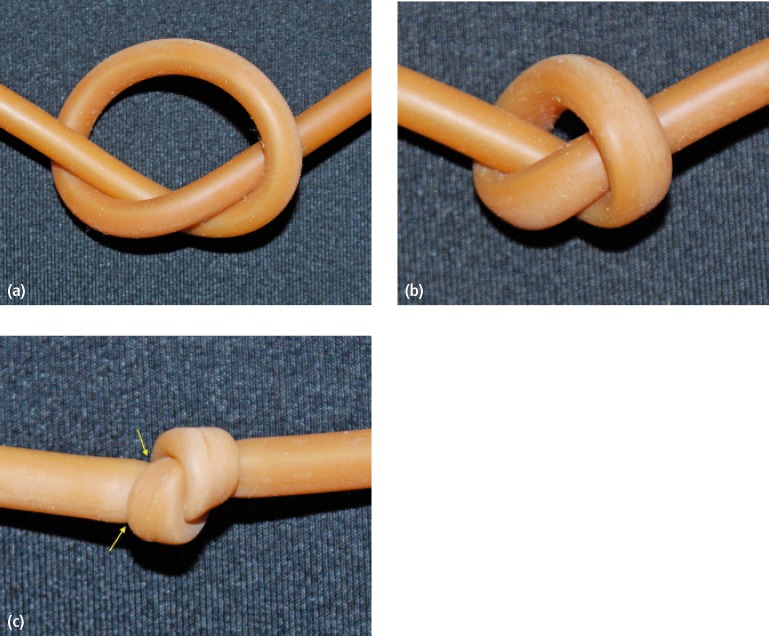
Surgical knots reduce the tensile strength of all sutures by thinning and stretching the material. A modeled representation of this effect can be appreciated by tying a knot in a piece of rubber tubing (Figure 1). The weakest portion of any suture line is the knot and the second weakest point is the portion immediately adjacent to the knot, with reductions in tensile strength reported from 35% to 95%, depending on the studies and suture material used.2
Figure 1.
(A) Piece of latex tubing early in the knot formation. (B) Piece of latex tubing as the knot begins to tighten. Notice the thinning of the diameter of the tubing. (C) Piece of latex tubing after the knot is tightened. Notice the thinning of the diameter of the tubing and the pinching of the area immediately before the knot (arrows).
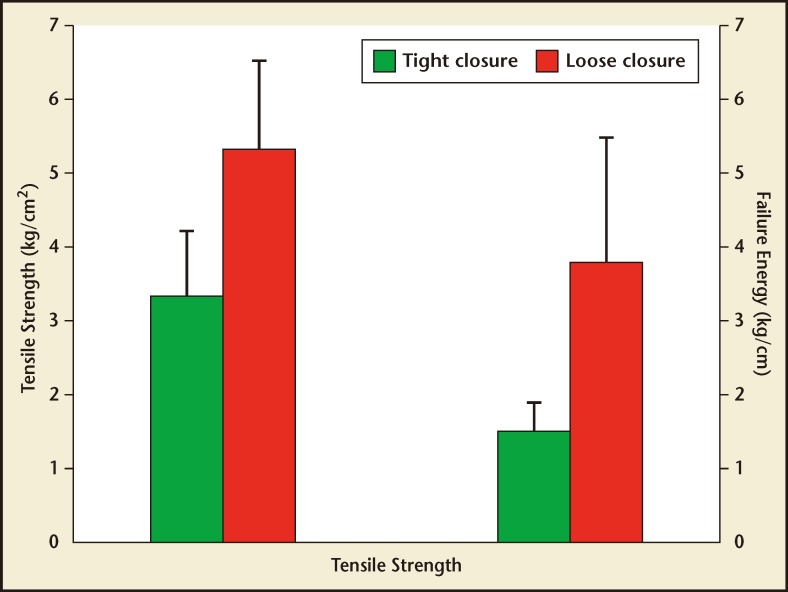
The tying of surgical knots introduces the potential of human error and interuser variability. Intuitively, knot-secured smooth suture must create an uneven distribution of tension across the wound with the higher tension burdens placed at the knots. Given the excessive relative wound tension on the knot and the reasonable concerns of surgeons for suture failure due to knot slippage, there is a natural tendency toward overcoming these concerns by over-tightening knots. However, Stone and colleagues3 demonstrated, in their classic 1986 study, that tighter knots may be worse for wound healing and strength than looser knots. Surgical knots, when tied too tightly, can cause localized hypoxia, reduced fibroblast proliferation, and excessive tissue overlap, leading to reduced strength in the healed wound (Figure 2).3
Figure 2.
Tensile strength and energy-to-failure of tightly and loosely approximated fascial incisions. Reproduced with permission from Stone IK et al.3
A surgical knot yields the highest density of foreign body material in any given suture line and the volume of a knot is directly related to the total amount of surrounding inflammatory reaction.4 If minimizing the inflammatory reaction in a wound is important for optimized wound healing, then minimizing knot sizes or eliminating knots altogether should be beneficial as long as the wound-holding strength of the suture line is not compromised.
Finally, with minimally invasive laparoscopic surgeries, the ability to quickly and properly tie surgical knots has presented a new challenge. In cases in which knot tying is difficult, the use of knotless barbed suture can securely reapproximate tissues with less time, cost, and aggravation.5,6 Although the skills necessary to properly perform intra- or extracorporeal knot tying for laparoscopic surgery can be achieved with practice and patience, it is a difficult skill that most surgeons need to master in order to properly perform closed procedures. In addition, laparoscopic knot tying is more mentally and physically stressful on surgeons7,8 and, more importantly, laparoscopically tied knots are often weaker than those tied by hand or robotically.9,10
History of Barbed Sutures
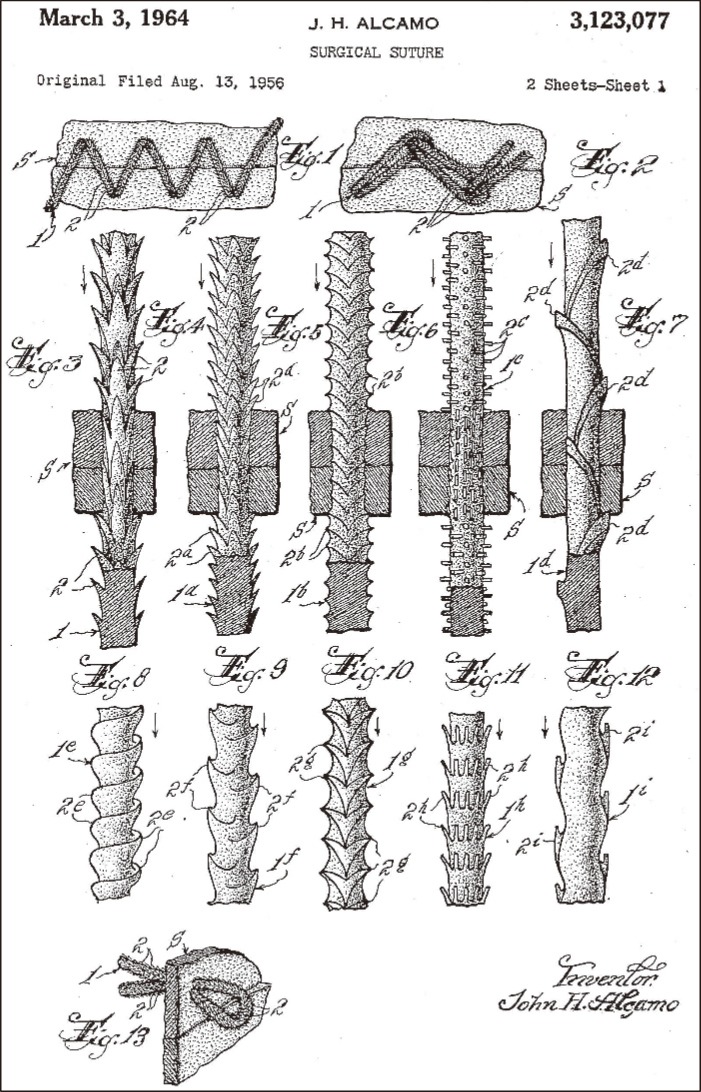
Modern barbed suture can trace its origins to Dr. John H. Alcamo, who submitted his idea to the US Patent office on August 13, 1956 and was issued US Patent number 3,123,077 on March 3, 1964 for “…a suture so formed that it prevents slippage in sutured incisions or wounds…” (Figure 3).11 Although Dr. Alcamo described the design for this suture, the first reports of the clinical use of barbed suture do not appear until 1967, when Dr. A.R. McKenzie reported its use in vitro in human cadavers and in vivo in dogs for the repair of long flexor tendons.12 However, these early spear-like barbed suture designs needed to be pushed into the patient’s tissue; therefore, they had to be of sufficient stiffness and diameter to be capable of being pushed into the tissue. Between 1967 and 1999, various authors and inventors presented an array of evolving thoughts and techniques in this niche, with the most notable being Dr. Harry J. Buncke (the so-called father of modern microsurgery) who received US Patent 5,931,855 on August 3, 1999 for “several surgical procedures for binding together living tissue using one-way sutures having barbs on their exterior surfaces and a needle on one or both ends.”13 His patents were acquired by Quill Medical (acquired by Angiotech Pharmaceuticals [Vancouver, BC, Canada] in 2006) in 2002 and, in conjunction with the inspired work of Dr. Gregory Ruff, the first widely commercialized barbed suture, Quill™ Knotless Tissue-Closure Device (Angiotech Pharmaceuticals), was approved by the US Food and Drug Administration (FDA) in 2004. In 2009, Covidien introduced V-Loc™ (Covidien Healthcare, Mansfield, MA) unidirectional barbed suture with a fixed loop, and in 2013 both Angiotech Pharmaceuticals and Ethicon Endo-Surgery (Cincinnati, OH) introduced unidirectional barbed sutures with a variable loop at the end for facilitated fixation.
Figure 3.
Original drawings for barbed suture. Reproduced from Alcamo JH.11
Production of Barbed Suture
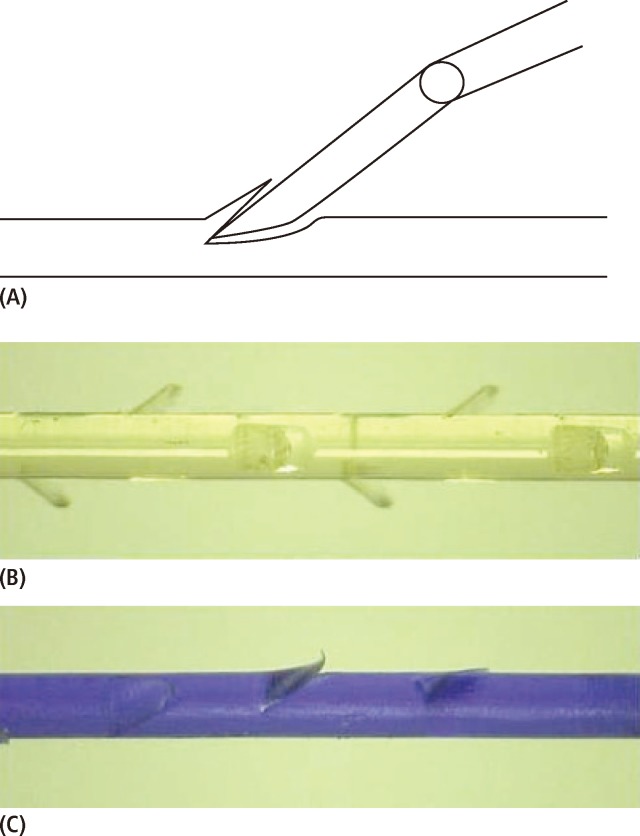
To fully appreciate the uses, characteristics, and limitations of barbed suture, a rudimentary understanding of their production is helpful; specifically, how the same materials that are traditionally used to produce strands of smooth suture are reconfigured to produce suture with barbs on their surfaces. More or less the same method is used in the manufacturing of Quill, V-Loc, and STRATAFIX™ Spiral (Ethicon Endo-Surgery), and involves cutting into the shaft of a strand of smooth suture with some type of blade (Figure 4).14,15 Although this method presents many manufacturing advantages, perhaps the most important drawback from a clinical perspective is that cutting barbs into suture reduces the tensile strength of the suture by weakening its core and narrowing its functional diameter. Thus, it is vital that clinicians understand the individual tensile strength of the particular suture being used rather than relying on measurements of traditional smooth sutures. Further, this difference has a significant practical implication—all cut barbed sutures (Quill, V-Loc, and STRATAFIX Spiral) carry an FDA-mandated warning in their instructions for use stating “the safety and effectiveness…has not been established for use in fascial closures (abdominal wall, thoracic, extremity fascial closures)…”16–18
Figure 4.
(A) Quill™ Knotless Tissue-Closure Device (Angiotech Pharmaceuticals, Inc; Vancouver, BC, Canada). (B) V-Loc™ Wound Closure Device (Covidien; Mansfield, MA). (C) Quill Knotless Tissue-Closure Device.
In Vitro and Animal Testing of Barbed Suture Products
Strength and tissue reactivity are integral to the functionality of suture material and, therefore, understanding these properties is essential when choosing suture for various procedures. Directly assessing these features in human clinical trials presents numerous logistical and ethical challenges that make in vitro and animal studies better suited for determining these characteristics. Although many of these trials were not performed in an obstetric or gynecologic setting, their findings can likely be translated to all surgical specialties.
Suture Strength
Tensile strength is an essential feature that surgeons must consider when choosing a suture. Put simply, the measure of tensile strength of a suture is the linear force required to cause it to break. Several in vitro studies have measured differences in strength between barbed and smooth suture. In 2011, Vakil and colleagues19 hypothesized that using #2 Quill polydioxanone (PDO) barbed suture would have equivalent closure integrity to #1 VICRYL™ (Ethicon Endo-Surgery) interrupted sutures in arthrotomy closure on cadaveric knees.19 They also surmised that barbed suture closures would be more likely to fail should there be a cut in the suture line. Supporting their hypothesis, they found that after 2000 flexion cycles, neither the closures using the smooth nor the barbed suture had a single failure. The authors further tested the integrity of the sutures by cutting sequential throws/stitches and continuing cyclical testing. Perhaps surprisingly, they found that although both smooth and barbed suture closures survived first-throw cutting, the barbed suture fared much better when multiple cuts were made. Once interrupted suture closures sustained three cuts, they all failed, whereas the barbed suture closures endured up to seven cuts. The authors found that barbed suture is better able to maintain tissue tension when cuts are made and may maintain the integrity of the full closure.
A recent study in the veterinary surgical literature used a cadaveric canine gastropexy model to compare tensile strength between 2-0 and 3-0 standard glycomer 631 with 2-0 and 3-0 V-Loc 90.20 The authors performed 4-cm incisional gastropexies on four groups, then sutured the incisions in a simple continuous fashion using one of the sutures above. Strength of the suture was measured using load to failure, defined as the force (in Newtons) required to cause suture breakage or tissue tearing. To measure load to failure, a distraction device was used to stress the sample at a rate of 0.4 mm/s. The authors found that the knotless barbed sutures had greater load to failure than the smooth standard suture. They found that failure occurred due to tissue tearing, not suture breakage, and concluded that the barbs themselves enabled the higher load to failure in those samples. This is likely due to the barb’s ability to distribute the force over a larger contact area, reducing pressure on the tissue.
Hemostasis and Leakage
Hemostasis and leakage prevention are paramount to a suture’s performance. In 2012, Gözen and coworkers21 demonstrated the superior performance of knotless barbed sutures following closure of cadaveric pig bladders compared with smooth suture. Porcine bladders were used to create bladder defects that were closed laparoscopically using (1) barbed poly glyconate in a running fashion, (2) polyglactin 910 in a running fashion, or (3) polyglactin 910 in an interrupted fashion. Leak pressures were evaluated using cystometry. Significantly higher leak pressures were noted in the barbed suture group than in either of the smooth suture groups, and average bladder capacity at the time to leakage was significantly higher in the barbed suture group (419.7 mL) compared with 353.8 mL in the smooth suture in a running fashion group and 276.2 mL in the interrupted suture group.
Similar findings were found in a study by Nett and colleagues,22 who demonstrated the superiority of bidirectional knotless barbed absorbable suture over conventional interrupted absorbable suture in producing a water-tight knee arthrotomy closure using cadaveric knees. They found that after 3 minutes of simulating a tense hemarthrosis, arthrotomy leakage was only 89 mL in the barbed suture group compared with 356 mL in the interrupted absorbable smooth suture group.
Efficiency
One of the most costly parts of a surgical procedure is time in the operating room. With rising health care costs, efficiency in the operating room is becoming more of a priority.23 New and innovative tools that can help experienced surgeons operate faster continue to play a large role in improving operator efficiency.24
In the porcine bladder study by Gözen and colleagues,21 one of the primary outcomes was time to complete the closure of a bladder defect laparoscopically. A single expert surgeon with extensive laparoscopic experience performed each closure. The expert surgeon was able to complete the closure in significantly less time using barbed suture (7.13 min) than with both smooth suture groups (9.14 min with running suture and 15.2 min with interrupted suture).
Significantly faster closure times with barbed suture were also seen in several in vivo studies. In a prospective, randomized study performed at the Cleveland Clinic (Cleveland, OH), Ting and coworkers25 demonstrated a 32% faster closure time when using barbed suture (9.3 min) compared with an average 13.6-minute closure in the traditional suture group during primary total hip and knee arthroplasties. Similar findings have been seen in the plastic surgery literature. Grigoryants and Baroni26 compared closure time of lipoabdominoplasty wounds using barbed suture in a two-layer closure to conventional smooth suture in a three-layer closure. Each surgeon closed half of the wound with barbed suture and the other half of the same wound with smooth suture. At the conclusion of this study, authors demonstrated an approximately 36% faster average closure time using the barbed suture. Finally, in a bariatric surgery study by De Blasi and coworkers,27 jejunal anastamosis using V-Loc barbed suture was 25% faster than anastomosis using smooth suture (of note, there is an FDA warning against its use in gastrointestinal anastomoses).17 Cost required to complete the closure was significantly less in the barbed suture group.
Inflammation and Wound Healing
Although barbed suture may prove to be a superior technology with regard to both efficiency and strength, it is equally important to consider how barbed suture interacts with tissue over time and how that translates to wound healing and inflammatory potential. Einarsson and colleagues28 used a sheep model to explore the impact of barbed suture versus traditional smooth suture on the adhesion formation following closure of myometrium. In this animal study, 5-cm myometrial defects were created in each horn of a sheep’s bicornuate uterus. One horn was then closed with 2-0 VICRYL, and the other with barbed 0-PDO. In this way, each sheep acted as her own control subject. Three months later the animals were sacrificed and necropsy was performed to grossly assess adhesion formation. The authors found that adhesion formation was not different between the two groups. The majority of the animals that formed adhesions did so at both horns. Similar to prior studies, the side of the uterus closed with barbed suture was more efficient.
As a follow-up to this study, Einarsson and colleagues29 demonstrated that at the microscopic level, barbed suture and standard smooth suture had similar effects on cellular composition following myometrial closure in the sheep model. The uterine tissue of the sacrificed animals was fixed and immunohistochemistry was performed to determine the ratio between smooth muscle cells and connective tissue elements, which are generally increased during wound healing. The authors again found no difference between groups: connective tissue cells typical of a proliferating wound were found in equal amounts in myometrium sutured with barbed and smooth suture, suggesting that both sutures confer similar healing characteristics. Sutured myometrium in both groups had more connective tissue cells and fewer smooth muscle cells than myometrium that was not sutured at all. Although these early animal clinical data are encouraging, more studies are clearly needed before any final conclusions regarding inflammation and wound healing can be made.
Clinical Trials Using Barbed Suture
Myomectomy
The obstetrics and gynecology literature has expanded in recent years to include clinical trials assessing the use of barbed suture. One of the most common procedures performed by gynecologists using barbed sutures is myomectomy. Huang and colleagues30 devised a study that took place in Taiwan to evaluate the safety and effectiveness of barbed suture during a minilaparotomy myomectomy. Each procedure was performed by a single experienced surgeon. Patients undergoing minilaparotomy myomectomies had their uterine defects closed with either barbed suture in a continuous fashion or traditional suture in an interrupted fashion. Authors found that overall surgical time was significantly less in the group whose uteri were closed using the barbed suture. Intraoperative blood loss was lower in this group as well, although the difference in blood loss was not statistically significant. Similarly, two recent studies have assessed the use of barbed suture for closure during laparoscopic myomectomy. Angioli and colleagues31 used either barbed suture or traditional smooth suture with intracorporeal knot tying to close uterine wall defects following laparoscopic myomectomy. They found that in the barbed suture group, suturing time was shorter and intraoperative blood loss and drop in postoperative hematocrit levels were lower. In a similar study performed by Alessandri and coworkers,32 women undergoing laparoscopic myomectomies for symptomatic myoma were randomized to receive either barbed suture or traditional smooth suture in a continuous fashion during closure of uterine defects. As in the study by Angioli and associates,31 the authors found that defect closure time was faster in the barbed suture group. Similarly, intraoperative blood loss was lower in the barbed suture group. In addition, these authors assessed the degree of surgical difficulty by each surgeon at the completion of the procedure and concluded that the overall difficulty in the barbed suture group was lower.
Many patients undergo myomectomies in an attempt to increase fertility. It is therefore prudent to study pregnancy outcomes after myomectomy to determine whether the short-term benefits of barbed suture such as efficiency are congruous with later goals. To this end, Sandberg and colleagues33 retrospectively looked at pregnancy outcomes among women who had uterine defect closures with barbed suture. In addition to reviewing medical records, patients were sent a survey to further elucidate pregnancy outcomes. The authors found that > 50% of women who attempted pregnancy following myomectomy closure with barbed suture were able to do so, with an average time to conception of 9.6 months after surgery. Of the women who became pregnant, more than half resulted in live births and > 10% had ongoing pregnancies. Approximately 35% resulted in miscarriage. These outcomes were comparable with pregnancy outcomes following uterine defect closures with traditional smooth suture during myomectomy.
Hysterectomy Cuff Closure
Cuff dehiscence is a rare but serious complication of hysterectomy that can result in significant morbidity for a patient. As surgeons increasingly perform total hysterectomies using barbed suture for closure of the cuff, it is important to establish the overall effectiveness and safety of the practice. In a retrospective cohort study by Siedhoff and colleagues,34 the impact of barbed suture on cuff dehiscence was studied over the period of 1 year. The authors found that although there was an approximate 4% occurrence of cuff dehiscence among all women who underwent laparoscopic vaginal closure, there were no cases in women who had closure using the bidirectional barbed suture. Additionally, there were lower incidences of postoperative bleeding, cellulitis, and granulation tissue among women with barbed suture closures. These data were recently corroborated by Einarsson and coworkers35 in a randomized trial in which 63 women received either bidirectional 0-PDO barbed suture or running 2-0 VICRYL suture.35 There were no differences in cuff dehiscence, complications, or sexual dysfunction between the groups. Finally, in an abstract presented in 2011, Giddings and Naumann36 retrospectively reviewed outcomes of patients undergoing cuff closures with either V-Loc 90 or V-Loc 180 barbed suture during total laparoscopic hysterectomy. In their small cohort of 86 patients, there were only two cuff dehiscences (2.3%), but both occurred in patients on whom V-Loc 90 was used. This led some to question the appropriate suture absorption profile in these patients, which is an avenue that merits further investigation.
Cesarean Delivery
To date, no articles have looked at the use of barbed suture for closing the uterus during cesarean delivery in humans. In 2006, Murtha and colleagues37 designed a randomized controlled trial to study cosmetic outcomes of dermal closure of Pfannenstiel skin incisions during cesarean deliveries. The authors randomly assigned women to receive either smooth or barbed suture for skin closure, and the incisions were evaluated 5 weeks later by an independent plastic surgeon. There was no difference in cosmesis between the groups. Similarly, there were no differences in time to close, infection, wound dehiscence, or pain.
In a sheep model, Greenberg and colleagues38 assessed the effects of suture type on uterine and fascial healing during cesarean delivery in pregnant ewes. The ewes served as their own control subjects by having two different suture types randomized for both the myometrial and fascial closures. The uterine sutures included barbed Monoderm™ (Ethicon Endo-Surgery), smooth Monocryl™ (Ethicon Endo-Surgery), VICRYL, and chromic. The fascial sutures included barbed 0-PDO, barbed 0-Monoderm, 0-Vicryl, smooth 0-Monocryl, and 0-chromic. The fascial closures on four of the ewes (44%) that were randomized to receive either chromic or barbed Monoderm failed prematurely. In this small trial, both chromic and Monoderm were inadequate for tissue reapproximation on the fascia. Given their tensile strength profiles, this was not surprising. In all nine ewes, all the sutures were adequate to reapproximate the uterus. From this limited study, the authors concluded that barbed sutures were as good as knotted smooth sutures for reapproximating the hysterotomy closure in ewes. Additional human studies are required to determine the adequacy of barbed suture during cesarean deliveries. Based on the extensive use of chromic and polyglycolic acid sutures on the closure of hysterotomies during cesarean delivery, as well as the absorption profiles of the currently available barbed sutures, we suspect that barbed suture may be suitable for use during these deliveries.
Conclusions
Technologic advances and the evolution of increasingly complex surgical procedures inevitably progress hand-in-hand. Whether one leads the other is a matter of debate, but their symbiosis is undeniable. The introduction and evolution of barbed suture material elegantly serves as a reminder of this relationship. From its earliest days as a crudely fabricated device for tendon reapproximation to its current mass-produced, high-quality reality with numerous broad applications, this exciting technology is unquestionably still in its infancy.
The clinical literature reviewed herein supports the performance of absorbable barbed sutures is, at least, equivalent to conventional absorbable smooth sutures for soft tissue reapproximation in obstetrics and gynecology. In addition, the literature reviewed has shown that the use of barbed sutures can shorten surgical time and possibly reduce intraoperative blood loss. With the introduction of newer barbed suture products, the applications of this exciting technology will undoubtedly expand, although more randomized clinical trials are needed to better elucidate its full potential.
Main Points.
Surgical knots are simply a necessary evil needed to anchor smooth suture to allow it to function in its role in tissue reapproximation. Other than their anchoring function, surgical knots offer no benefit and introduce a variety of untoward features. Surgical knots reduce the tensile strength of all sutures by thinning and stretching the material.
A surgical knot yields the highest density of foreign body material in any given suture line and the volume of a knot is directly related to the total amount of surrounding inflammatory reaction. If minimizing the inflammatory reaction in a wound is important for optimized wound healing, then minimizing knot sizes or eliminating knots altogether should be beneficial as long as the wound-holding strength of the suture line is not compromised.
With minimally invasive laparoscopic surgeries, the ability to quickly and properly tie surgical knots has presented a new challenge for surgeons. In cases in which knot tying is difficult, the use of knotless barbed suture can securely reapproximate tissues with less time, cost, and aggravation. The skills necessary to properly perform intra- or extracorporeal knot tying for laparoscopic surgery can be achieved with practice and patience.
Significantly faster closure times with barbed suture have been seen in several in vivo studies.
Clinical literature supports the theory that the performance of absorbable barbed sutures is equivalent to conventional absorbable smooth sutures for soft tissue reapproximation in obstetrics and gynecology.
Footnotes
Dr. Greenberg has worked in the past as a per diem paid consultant for Ethicon (Somerville, NJ), the makers of the STRATAfIx™ suture. Dr. Goldman has no disclosures to report. Development of this article was made possible by a grant from Ethicon.
References
- 1.Greenberg JA, Einarsson JI. Bidirectional barbed suture for laparoscopic myomectomy. J Minim Invasive Gynecol. 2008;15(suppl):S11. doi: 10.1016/j.jmig.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 2.Chu CC, von Fraunhofer JA, Greisler HP. Wound Closure Biomaterials and Devices. Boca Raton, FL: CRC Press;; 1997. p. 122. [Google Scholar]
- 3.Stone IK, von Fraunhofer JA, Masterson BJ. The biomechanical effects of tight suture closure upon fascia. Surg Gynecol Obstet. 1986;163:448–452. [PubMed] [Google Scholar]
- 4.van Rijssel EJ, Brand R, Admiraal C, et al. Tissue reaction and surgical knots: the effect of suture size, knot configuration, and knot volume. Obstet Gynecol. 1989;74:64–68. [PubMed] [Google Scholar]
- 5.Hashemi L, Hart S, Morseon M. Comparison of surgery time and cost in using barbed suture versus the traditional suture in robotic hysterectomy: a retrospective cohort study. J Minim Invasive Gynecol. 2012;19(suppl):S6. [Google Scholar]
- 6.Moran ME, Marsh C, Perrotti M. Bidirectionalbarbed sutured knotless running anastomosis v classic Van Velthoven suturing in a model system. J Endourol. 2007;21:1175–1178. doi: 10.1089/end.2007.9913. [DOI] [PubMed] [Google Scholar]
- 7.Berguer R, Smith WD, Chung YH. Performing laparoscopic surgery is significantly more stressful for the surgeon than open surgery. Surg Endosc. 2001;15:1204–1207. doi: 10.1007/s004640080030. [DOI] [PubMed] [Google Scholar]
- 8.Berguer R, Chen J, Smith WD. A comparison of the physical effort required for laparoscopic and open surgical techniques. Arch Surg. 2003;138:967–970. doi: 10.1001/archsurg.138.9.967. [DOI] [PubMed] [Google Scholar]
- 9.Kadirkamanathan SS, Shelton JC, Hepworth CC, et al. A comparison of the strength of knots tied by hand and at laparoscopy. J Am Coll Surg. 1996;182:46–54. [PubMed] [Google Scholar]
- 10.Lopez PJ, Veness J, Wojcik A, Curry J. How reliable is intracorporeal laparoscopic knot tying? J Laparoendosc Adv Surg Tech A. 2006;16:428–432. doi: 10.1089/lap.2006.16.428. [DOI] [PubMed] [Google Scholar]
- 11.Alcamo JH, inventor. Surgical suture. US patent. 1964 Mar 3;
- 12.McKenzie AR. An experimental multiple barbed suture for the long flexor tendons of the palm and fingers. Preliminary report. J Bone Joint Surg. 1967;49B:440–447. [PubMed] [Google Scholar]
- 13.Buncke HJ, inventor. Surgical methods using one-way suture. US patent. 1999 Aug 3;
- 14.Genova P, Williams RC, Jewett W, inventors. Quill Medical, Inc, assignees. Method for cutting a suture to create tissue retainers of a desired shape and size. US patent. 2011 Sep 13;
- 15.Maiorino N, Buchter MS, Primavera M, Kosa TD, inventors. Tyco Healthcare Group LP, assignees. Method of forming barbs on a suture. US patent. 2012 Apr 24;
- 16.Quill™ Self-Retaining System [instructions for use] Reading, PA: Angiotech Pharmaceutics, Inc; 2009. [Google Scholar]
- 17.V-Loc™ 180 Absorbable Wound Closure Device [instructions for use] Norwalk, CT: United States Surgical, a division of Tyco Healthcare Group LP; 2009. [Google Scholar]
- 18.STRATAFIX™ Spiral PDO Knotless Synthetic Absorbable Surgical Suture Material [instructions for use] Blue Ash, OH: Ethicon Endo-Surgery; 2012. [Google Scholar]
- 19.Vakil JJ, O’Reilly MP, Sutter EG, et al. Knee arthrotomy repair with a continuous barbed suture: a biomechanical study. J Arthroplasty. 2011;26:710–713. doi: 10.1016/j.arth.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Arbaugh M, Case JB, Monnet E. Biomechanical comparison of glycomer 631 and glycomer 631 knotless for use in canine incisional gastropexy. Vet Surg. 2013;42:205–209. doi: 10.1111/j.1532-950X.2012.01051.x. [DOI] [PubMed] [Google Scholar]
- 21.Gözen AS, Arslan M, Schulze M, Rassweiler J. Comparison of laparoscopic closure of the bladder with barbed polyglyconate versus polyglactin suture material in the pig bladder model: an experimental in vitro study. J Endourol. 2012;26:732–736. doi: 10.1089/end.2011.0194. [DOI] [PubMed] [Google Scholar]
- 22.Nett M, Avelar R, Sheehan M, Cushner F. Water-tight knee arthrotomy closure: comparison of a novel single bidirectional barbed self-retaining running suture versus conventional interrupted sutures. J Knee Surg. 2011;24:55–59. doi: 10.1055/s-0031-1275400. [DOI] [PubMed] [Google Scholar]
- 23.Seim A, Andersen B, Sandberg WS. Statistical process control as a tool for monitoring nonoperative time. Anesthesiology. 2006;105:370–380. doi: 10.1097/00000542-200608000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Agnoletti V, Buccioli M, Padovani E, et al. Operating room data management: improving efficiency and safety in a surgical block. BMC Surg. 2013;13:7. doi: 10.1186/1471-2482-13-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ting NT, Moric MM, Della Valle CJ, Levine BR. Use of knotless suture for closure of total hip and knee arthroplasties: a prospective, randomized clinical trial. J Arthroplasty. 2012;27:1783–1788. doi: 10.1016/j.arth.2012.05.022. [DOI] [PubMed] [Google Scholar]
- 26.Grigoryants V, Baroni A. Effectiveness of wound closure with V-Loc 90 sutures in lipoabdominoplasty patients. Aesthet Surg J. 2013;33:97–101. doi: 10.1177/1090820X12467797. [DOI] [PubMed] [Google Scholar]
- 27.De Blasi V, Facy O, Goergen M, et al. Barbed versus usual suture for closure of the gastrojejunal anastomosis in laparoscopic gastric bypass: a comparative trial. Obes Surg. 2013;23:60–63. doi: 10.1007/s11695-012-0763-4. [DOI] [PubMed] [Google Scholar]
- 28.Einarsson JI, Grazul-Bilska AT, Vonnahme KA. Barbed vs standard suture: randomized singleblinded comparison of adhesion formation and ease of use in an animal model. J Minim Invasive Gynecol. 2011;18:716–719. doi: 10.1016/j.jmig.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 29.Einarsson JI, Vonnahme KA, Sandberg EM, Grazul-Bilska AT. Barbed compared with standard suture: effects on cellular composition and proliferation of the healing wound in the ovine uterus. Acta Obstet Gynecol Scand. 2012;91:613–619. doi: 10.1111/j.1600-0412.2012.01381.x. [DOI] [PubMed] [Google Scholar]
- 30.Huang MC, Hsieh CH, Su TH, et al. Safety and efficacy of unidirectional barbed suture in mini-laparotomy myomectomy. Taiwan J Obstet Gynecol. 2013;52:53–56. doi: 10.1016/j.tjog.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 31.Angioli R, Plotti F, Montera R, et al. A new type of absorbable barbed suture for use in laparoscopic myomectomy. Int J Gynaecol Obstet. 2012;117:220–223. doi: 10.1016/j.ijgo.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 32.Alessandri F, Remorgida V, Venturini PL, Ferrero S. Unidirectional barbed suture versus continuous suture with intracorporeal knots in laparoscopic myomectomy: a randomized study. J Minim Invasive Gynecol. 2010;17:725–729. doi: 10.1016/j.jmig.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 33.Sandberg EM, Cohen SL, Hill-Lydecker CI, et al. Pregnancy outcomes after laparoscopic myomectomy with barbed suture. J Minim Invasive Gynecol. 2012;19(suppl):S48. [Google Scholar]
- 34.Siedhoff MT, Yunker AC, Steege JF. Decreased incidence of vaginal cuff dehiscence after laparoscopic closure with bidirectional barbed suture. J Minim Invasive Gynecol. 2011;18:218–223. doi: 10.1016/j.jmig.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 35.Einarsson JI, Cohen SL, Gobern JM, et al. Barbed versus standard suture: a randomized trial for laparoscopic vaginal cuff closure. J Minim Invasive Gynecol. 2013;20:492–498. doi: 10.1016/j.jmig.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 36.Giddings A, Naumann RW. Closure of the vaginal cuff after a total laparoscopic hysterectomy (TLH) with a running barbed suture. J Minim Invasive Gynecol. 2011;18(suppl):S84–S85. [Google Scholar]
- 37.Murtha AP, Kaplan AL, Paglia MJ, et al. Evaluation of a novel technique for wound closure using a barbed suture. Plast Reconstr Surg. 2006;117:1769–1780. doi: 10.1097/01.prs.0000209971.08264.b0. [DOI] [PubMed] [Google Scholar]
- 38.Greenberg JA, Walden S, Hammer CM, et al. A comparison of barbed and smooth sutures for ovine cesarean delivery. Int J Gynaecol Obstet. 2011;113:215–217. doi: 10.1016/j.ijgo.2010.12.017. [DOI] [PubMed] [Google Scholar]