Abstract
Aim:
The aim of this study was to investigate the anti-inflammatory action of isoflurane preconditioning in a model of lipopolysaccharide (LPS)-induced inflammation in RAW 264.7 macrophages and examine the role of heme oxygenase (HO)-1 in this process.
Methods:
Murine 264.7 macrophages were pretreated with or without 1%–3% isoflurane for 1 h. Thirty minutes later, the cells were incubated with or without LPS for 24 h. Cell viability was assessed using a 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay and cell injury was assessed by measuring the release of lactate dehydrogenase (LDH). HO-1 and inducible nitric oxide synthase (iNOS) protein expression was analyzed by Western blotting. Tumor necrosis factor (TNF)-α levels, nitrite production and HO activity were also determined.
Results:
Pretreatment with the nontoxic and clinically approved anesthetic isoflurane potently attenuated the cell injury and the decrease in cell viability that was induced by LPS. Treatment or pretreatment with 2% isoflurane induced HO-1 protein expression and caused an induction of HO activity. This result correlated with a decrease in iNOS expression, a decrease in the production of nitric oxide (NO) and impaired release of TNF-α in LPS-stimulated macrophages. Blockade of HO activity with tin protoporphyrin (SnPP) reversed these effects.
Conclusion:
Isoflurane preconditioning exerts its anti-inflammatory activity through the HO-1 pathway in an in vitro inflammation model.
Keywords: anesthesia, lipopolysaccharide, heme oxygenase, inflammation
Introduction
Preconditioning is the phenomenon in which prior exposure to a stimulus induces protection against the detrimental effects of a subsequent insult1. The presence of volatile anesthetics before the insult has been shown to be protective2, 3. This phenomenon is termed volatile anesthetic preconditioning. Isoflurane pretreatment has been shown to inhibit lipopolysaccharide (LPS)-induced inflammatory responses both in vivo4, 5 and in vitro6. However, the underlying mechanisms for this inhibition remain elusive.
Heme oxygenases (HOs) are responsible for catalyzing the breakdown of heme into equimolar concentrations of carbon monoxide, biliverdin, and iron. This breakdown utilizes molecular oxygen and reducing equivalents from NADPH:cytochrome P450 reductase7. Three different mammalian HO isoforms have been described, and the HO-1 isoform is ubiquitously distributed and known to suppress inflammation8. The beneficial effect of isoflurane preconditioning may originate from its ability to induce endogenous cytoprotective pathways, such as the HO-1 pathway. Our group has previously reported that isoflurane induces HO-1 accumulation and that this effect is associated with the activation of the transcription factor HIF-1 in vitro9, 10. Other groups have demonstrated the induction of HO-1 by isoflurane in liver tissue in vivo11, 12. Furthermore, studies have shown that HO-1 and its product, carbon monoxide (CO), can reduce edema, leukocyte adhesion, migration and the production of cytokines13, 14. The fact that inflammatory stimuli induce the expression of HO-1 suggests that HO-1 production is an adaptive cellular response to inflammation15.
To better understand the role of isoflurane preconditioning in inflammation, we investigated the effect of isoflurane preconditioning on HO-1 expression in RAW 264.7 macrophages. Further, we assessed whether HO-1 was involved in the anti-inflammatory action of isoflurane preconditioning in macrophages stimulated with LPS.
Materials and methods
Reagents
Rabbit polyclonal antibodies against inducible nitric oxide synthase (iNOS) and HO-1 were obtained from 51AB Biotech Company (Shanghai China). A 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT)-based colorimetric assay kit was obtained from Roche Applied Science (Roche, IN). Isoflurane was purchased from Abbott Laboratories (North Chicago, IL). Tin protoporphyrin (SnPP) was obtained from Porphyrin Products (Logan, UT). All other reagents were purchased from Sigma-Aldrich (St Louis, MO) unless otherwise specified.
Cell culture
Murine 264.7 macrophages were purchased from the Cell Bank of Shanghai Institutes for Biological Science (Shanghai, China) and cultured in Dulbecco's modified Eagle's medium containing 2 mmol/L glutamine, 100 U/mL penicillin, 0.1 mg/mL streptomycin, and 10% fetal bovine serum, as previously described16. The medium was changed every 3 days. For viability experiments using the MTT assay, the cells were plated at a density of 3.5×104–5×104 cells/well in 96-well tissue culture plates. The cells were grown at a density of 2×106 cells/well in 6-well plates or 100-mm dishes for experiments other than the viability assay.
Isoflurane exposure and application of chemicals
Isoflurane pretreatment of the cells was performed in an airtight chamber, as previously described9. Briefly, cell dishes were kept in an airtight chamber that was housed within a water-jacketed incubator maintained at 37 °C. An in-line calibrated anesthetic agent vaporizer was used to deliver isoflurane to the gas phase of the cultured wells. Normoxic gas was administered at a flow rate of 3 L/min, until the appropriate effluent concentration of the anesthetic was achieved. This required approximately 10–20 min (the total isoflurane exposure time was 1 h). The flow rate was then decreased and maintained at 900 mL/min for the indicated periods at 37 °C. Effluent isoflurane, oxygen, and carbon dioxide concentrations were continuously monitored via a sampling port connected to an anesthetic agent analyzer (5250, RGM; Datex-Ohmeda, Madison, WI). The pH of the medium before and after exposure was 7.4. The cells were then removed from the chamber and were kept under normal and isoflurane-free culture conditions for 30 min before they were exposed to 1 μg/mL LPS for 24 h at 37 °C. To determine the involvement of HO during isoflurane preconditioning, the HO inhibitor SnPP (10 μmol/L) was added just before the application of isoflurane. After isoflurane exposure, the incubation medium was replaced with fresh medium without SnPP before the cells were exposed to 1 μg/mL LPS.
Cell viability and injury assessment
Cell viability was assessed using the MTT assay. Cells were seeded and cultured as described above. After treatment with vehicle or isoflurane at 37 °C for 1 h, the cells were stimulated with 1 μg/mL of LPS for 24 h. MTT (0.5 mg/mL) was added during the last 3 h of culture. After the medium was removed and dimethyl sulfoxide (DMSO) was added to the flask, the absorbance at 570 nm was measured using a microplate reader. In each experiment, the results of the MTT measurements from the controls (samples receiving no treatment) were set at 100%. The results from the sister cultures that were subjected to various treatments were then calculated as a percentage of the controls. Cell injury was assessed by measuring the amount of lactate dehydrogenase (LDH) released using a cytotoxicity detection kit according to the manufacturer's instructions (Roche, IN). The absorbance was measured at 490 and 690 nm. LDH activity was expressed as a percentage of the LDH release in control cultures.
Western blot analysis
Western blot analysis was performed as previously described17. Briefly, 100 μg of total protein was loaded onto a 10% SDS-polyacrylamide gel, which was blotted onto nitrocellulose membranes after electrophoresis. The primary rabbit anti-rat iNOS (Abcam, UK), HO-1(Abcam, UK) and β-actin monoclonal antibodies (Sigma, A1978) were used at 1:500, 1:1000, and 1:4000 dilutions, respectively. The anti-rabbit IgG secondary antibody (KPL, USA) was used at a 1:2000 dilution, and the signal was analyzed by enhanced chemiluminescence. The abundance of HO-1 and iNOS proteins was normalized to β-actin using Quantity One-4.2.3 software (Bio-Rad, Hercules, CA).
Determination of nitrite levels
Cells in six well culture plates were pretreated with or without 2% isoflurane for 1 h. Thirty minutes after the isoflurane pretreatment, the cells were exposed to 1 μg/mL of LPS or PBS for 24 h at 37 °C. At the end of the incubation, the medium from the treated cells was removed and placed into a 96-well plate (50 μL per well). The concentration of nitrite, a stable oxidation product of nitric oxide (NO), in the culture medium was measured using the Griess Reagent Kit according to the instructions. The absorbance of the samples was read at 570 nm against a standard curve using a microplate reader (Bio-Rad Laboratories).
Heme oxygenase activity assay
Heme oxygenase activity was determined at the end of each treatment as described previously18. Briefly, microsomes from harvested cells were added to a reaction mixture containing nicotinamide adenine dinucleotide phosphate (NADPH), glucose-6-phosphate dehydrogenase, rat liver cytosol as a source of biliverdin reductase, and the substrate hemin. The reaction mixture was incubated in the dark at 37 °C for 1 h and terminated by the addition of 1 mL of chloroform. After being vigorously vortexed and centrifuged, the amount of extracted bilirubin in the chloroform layer was determined by measuring the difference in absorbance between 464 and 530 nm [extinction coefficient=40 (mmol/L)−1·cm−1].
Measurement of TNF-α production
The level of TNF-α in each sample was determined using a commercially available kit from R&D Systems (Abingdon, UK) performed according to the manufacturer's instructions. Briefly, cell culture supernatants were collected immediately after being treated and were spun at 13 000×g for 2 min to remove any particulates. The medium was added to a 96-well plate that was pre-coated with affinity-purified polyclonal antibodies specific for mouse TNF-α. An enzyme-linked polyclonal antibody specific for mouse TNF-α was added to the wells and allowed to react for 2 h. Finally, the plate was washed to remove any unbound antibody-enzyme reagent. The intensity of the color detected at 450 nm (correction wavelength 570 nm) was measured after the addition of a substrate solution and was proportional to the amount of TNF-α produced.
Statistical analysis
Differences between the groups were analyzed using a one-way ANOVA and Student's t-test. Values were expressed as means±SD and differences between groups were considered significant at P<0.05.
Results
Isoflurane preconditioning reduces LPS-induced cell injury
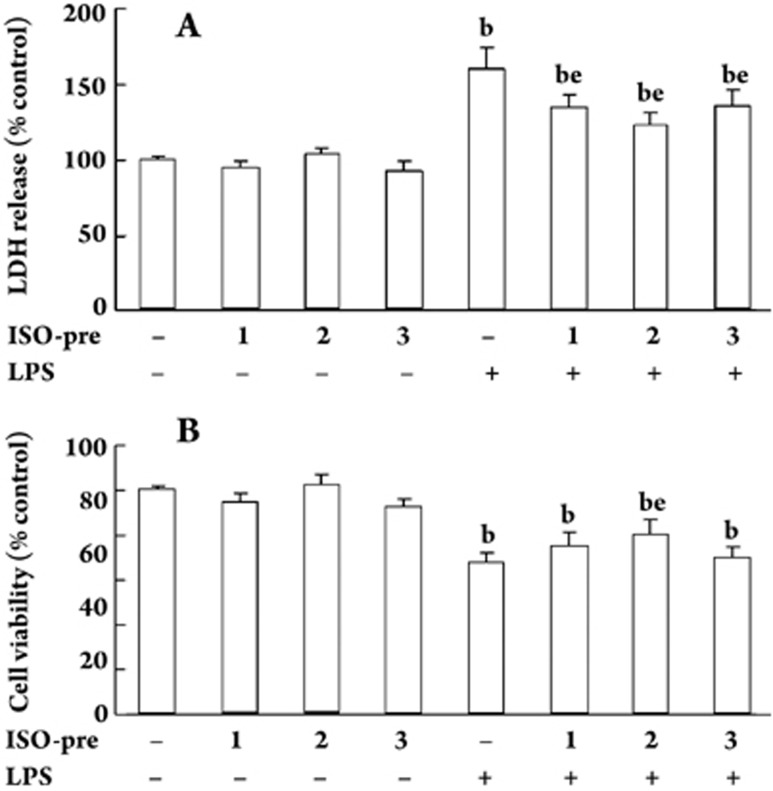
The LDH release, an index of cell damage, indicated that incubation of macrophages for 1 h with increasing concentrations of isoflurane preconditioning did not induce cytotoxicity compared with control cultures (Figure 1A). However, exposure to LPS alone resulted in increased cell injury and the pretreatment of cells with 1%, 2%, or 3% isoflurane significantly attenuated the LPS-induced cell injury (Figure 1A). Cell viability, as assessed by the MTT assay, also showed a protective effect induced by 2% isoflurane preconditioning. These results suggested that isoflurane induced a preconditioning effect in these cells (Figure 1B). Because 2% isoflurane caused maximal protection, we used this concentration for all subsequent experiments.
Figure 1.
Viability of cells exposed to isoflurane pretreatment and LPS. Cells were pretreated with or without various concentrations of isoflurane (1%, 2%, and 3%) for 1 h. They were then exposed to 1 μg/mL of LPS or PBS for 24 h. Thirty minutes after the isoflurane pretreatment the cell injury was determined by LDH release (A) and MTT assay (B). Cells treated with medium alone represent the control group. ISO-pre=isoflurane preconditioning. n=12–14. Mean±SD. bP<0.05 vs cells without isoflurane preconditioning or LPS stimulation. eP<0.05 vs cells with LPS stimulation.
Isoflurane induces HO activity and HO-1 expression in RAW 264.7 macrophages
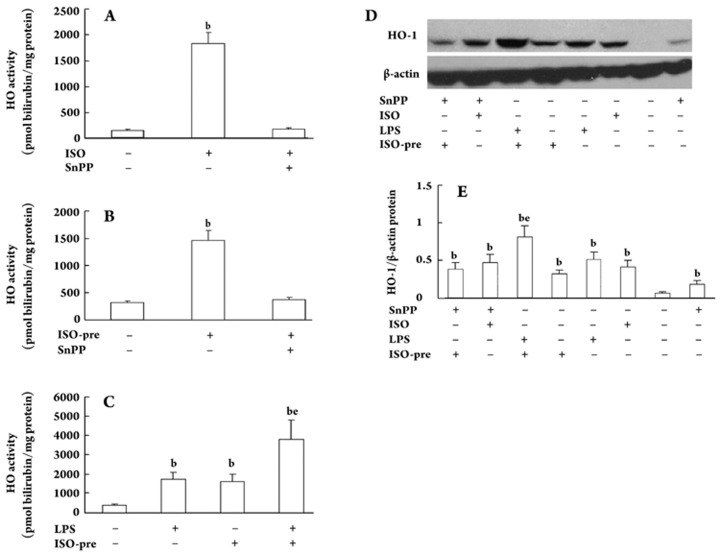
Macrophages respond to LPS challenge by up-regulating many endogenous protective pathways, including the HO-1 pathway19. Therefore, we determined the HO activity and protein expression of HO-1 in RAW 264.7 cells incubated or pre-incubated with isoflurane before LPS exposure. As shown in Figure 2A, exposure of cells to isoflurane for 1 h resulted in increased HO activity. We also assessed whether this effect was long lasting. For this purpose, HO activity was measured in macrophages incubated with isoflurane for 1 h, followed by 24 h of exposure to medium alone. Interestingly, HO activity remained elevated even after isoflurane was removed (Figure 2B), suggesting that isoflurane has a preconditioning effect on HO activity. This possibility was further substantiated by the fact that the level of HO activity was similar between cells incubated for 1 h with isoflurane and cells exposed to isoflurane for 1 h followed by 24 h of incubation in medium alone. The addition of an inhibitor of HO activity (SnPP, 10 μmol/L) completely abolished the effect of isoflurane treatment or isoflurane pretreatment on HO activity (Figure 2A and B). Furthermore, treatment with isoflurane or pretreatment with isoflurane before incubation also induced HO-1 protein expression (Figure 2D and 2E). Our results demonstrated that cells incubated with LPS alone exhibited a marked increase in HO activity, which reached very high levels when LPS and isoflurane pretreatment were used simultaneously (Figure 2C).
Figure 2.
The effect of isoflurane on HO activity and HO-1 protein expression. (A) and (B) Isoflurane treatment and isofurane pretreatment on HO activity. ISO, cells treated with 2% isoflurane for 1 h. ISO-pre, cells incubated with isoflurane for 1 h, followed by 24 h exposure to medium alone. HO activity was measured at the end of incubation. HO activity was inhibited by SnPP. (C) Cells were exposed to 2% isoflurane for 1 h, followed by 24 h incubation with or without 1 μg/mL of LPS. (D)The Western blot is representative of 3 independent experiments. (E) Densitometric quantification of the result of (D). n=6–9 for A, B and C. Mean±SD. bP<0.05 vs cells without isoflurane preconditioning or LPS stimulation. eP<0.05 vs cells with LPS stimulation.
Isoflurane preconditioning reduces LPS-stimulated nitrite production: involvement of the HO pathway
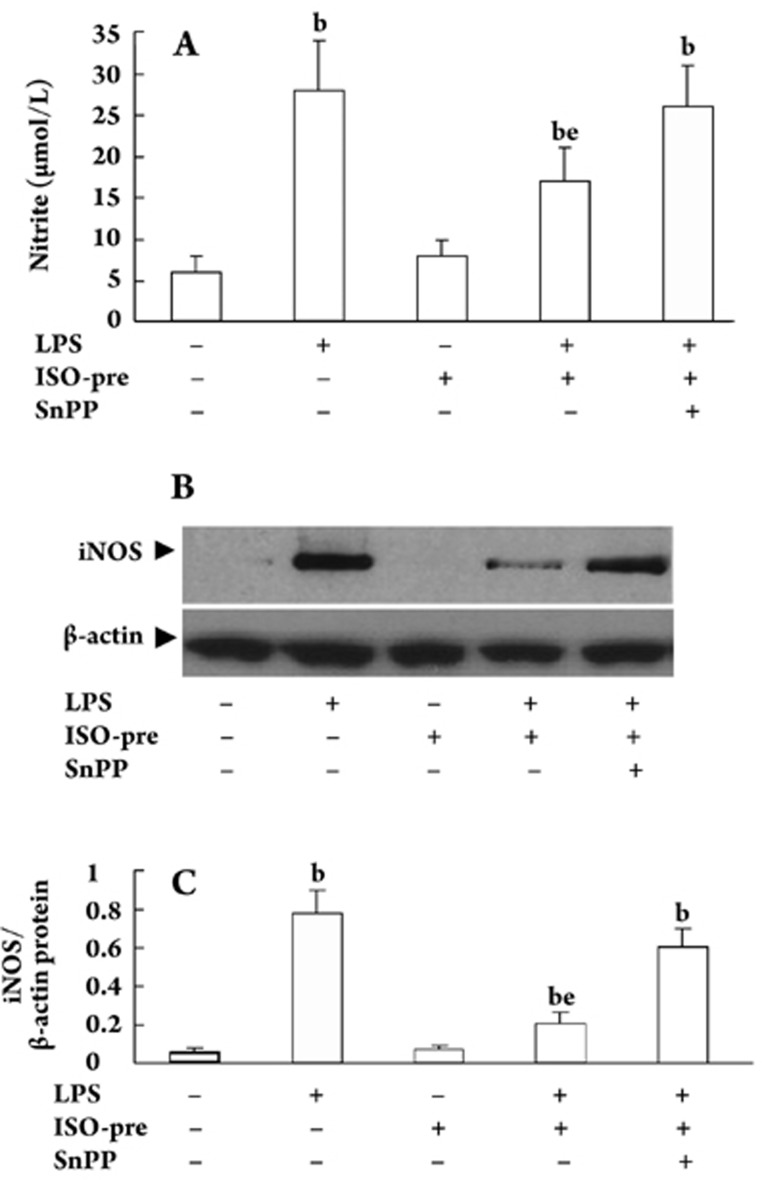
We next assessed the anti-inflammatory action of isoflurane preconditioning by measuring nitrite produced by macrophages challenged with LPS. As shown in Figure 3A, isoflurane preconditioning effectively impaired the increase in nitrite levels elicited by LPS treatment. Because isoflurane preconditioning upregulated HO-1 protein levels, we examined whether the HO pathway played a role in the observed reduction of nitrite using an inhibitor of HO activity (SnPP, 10 μmol/L) during the incubation of cells with LPS and after isoflurane preconditioning. The results in Figure 3A indicate that SnPP completely blocked the isoflurane preconditioning-mediated decrease in nitrite production, thereby sustaining the active involvement of HO in this process.
Figure 3.
Inhibition of nitrite production and iNOS protein expression by isoflurane pretreatment in LPS-stimulated RAW 264.7 cells. (A) Cells were pretreated with 2% isoflurane for 1 h in the presence or absence of SnPP before being incubated with LPS (1 μg/mL) for 24 h. Control cells were incubated with vehicle alone. The culture supernatants were subsequently isolated and analyzed for nitrite production. Data were expressed as mean±SD of six independent experiments. (B) The Western blot is representative of 3 independent experiments. Equal loading of proteins was verified by β-actin immunoblotting (lower panel). (C) Densitometric quantification of the results of (B). bP<0.05 vs cells without isoflurane preconditioning, LPS or SnPP stimulation. eP<0.05 vs cells with LPS stimulation.
Because iNOS is involved in the inflammatory process, we monitored iNOS protein expression in macrophages exposed to isoflurane preconditioning. We examined the effects of isoflurane preconditioning on protein expression by Western blot analysis. Isoflurane preconditioning caused an inhibition of iNOS protein expression in LPS-stimulated RAW 264.7 cells (Figure 3B and 3C). These results indicate that inhibition of iNOS expression by isoflurane preconditioning occurred in parallel with the comparable inhibition of NO production.
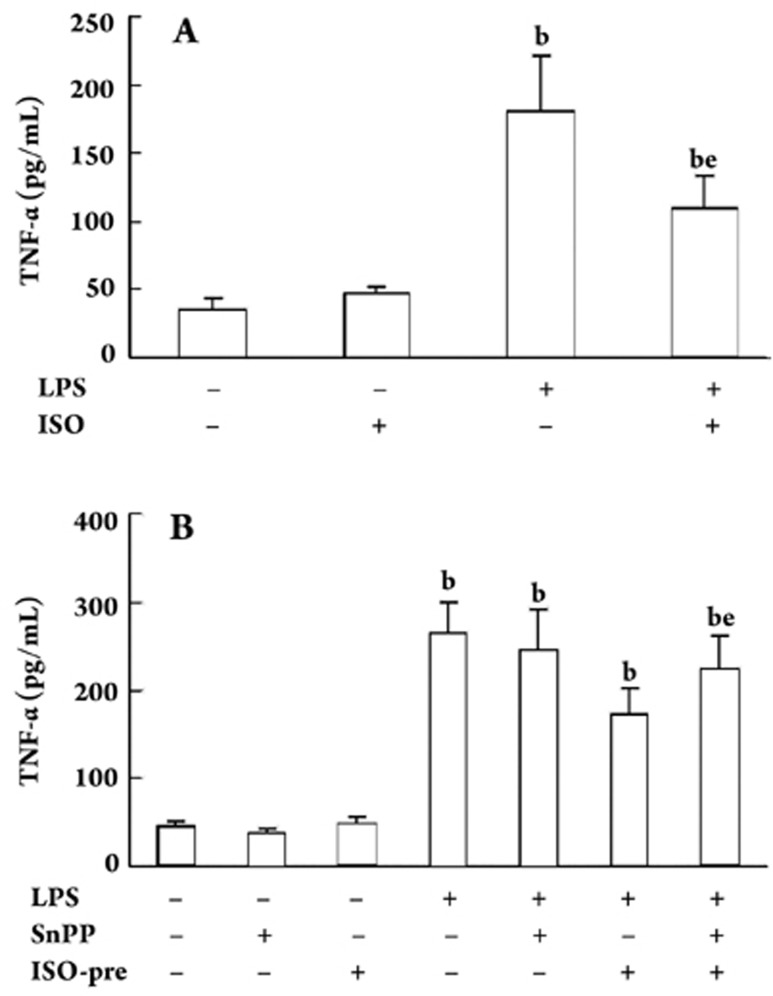
Isoflurane preconditioning attenuates LPS-stimulated TNF-α production
Because TNF-α is a major cytokine involved in the inflammatory response triggered by LPS20, we tested the effect of isoflurane and isoflurane pretreatment on LPS-induced TNF-α production. Consistent with the results obtained with nitrite levels, isoflurane and isoflurane pretreatment markedly decreased TNF-α production by LPS (Figure 4A and 4B). Importantly, inhibition of the HO pathway with SnPP significantly prevented this preconditioning effect (Figure 4B).
Figure 4.
Isoflurane modulates LPS-stimulated TNF-α production. (A) Cells were exposed to LPS (1 μg/mL) for 24 h in the presence or absence of isoflurane for 1 h (ISO) and TNF-α production was determined. (B) Cells were pretreated with 2% isoflurane or vehicle for 1 h (ISO-pre) and SnPP (10 μmol/L), followed by incubation with or without LPS (1 μg/mL) for 24 h and TNF-α production was determined. n=5–6. Mean±SD. bP<0.05 vs cells without isoflurane, LPS or SnPP stimulation. eP<0.05 vs cells with LPS stimulation.
Discussion
In the present study, we examined the potential involvement of HO-1 in the anti-inflammatory activity elicited by isoflurane preconditioning. We found that isoflurane preconditioning potently induced HO activity and HO-1 expression in RAW 264.7 macrophages and that this induction correlated with a decrease in iNOS expression and impaired NO and TNF-α production by LPS-stimulated macrophages. Inhibition of HO activity by SnPP reversed these effects, suggesting that the anti-inflammatory properties of isoflurane preconditioning involve the dynamic action of this cytoprotective protein.
We have recently reported that isoflurane can induce HO-1 expression in Hep3B cells9 and hippocampal neurons10, and here we extend our previous findings by showing a similar effect in macrophages. In the present study, we emphasize that the strong anti-inflammatory activity of this volatile anesthetic is mediated by HO-1. Because a decrease in nitrite production and TNF-α release was also observed when macrophages were preincubated with isoflurane before LPS challenge, we can exclude that this effect was due to a direct interaction of isoflurane with LPS. The persistent HO-1 induction observed after the removal of isoflurane from the culture medium may be due to the ability of isoflurane to modulate the expression of HO-1 genes. Although the contribution of HO-1 products (ie, CO, biliverdin, and iron) has not been examined, several studies13, 21, 22 point to HO-1-derived CO as the potential metabolite to combat inflammation, which is the common denominator of cardiovascular and neurodegenerative diseases. On the other hand, isoflurane preconditioning protected macrophages from the LPS-induced release of LDH, highlighting the ability of isoflurane preconditioning to protect against specific types of cellular damage. Consistent with previous reports4 using 1.4% isoflurane preconditioning, we also found that LPS-stimulated TNF-α production was significantly diminished by isoflurane pretreatment, further sustaining the role of isoflurane as a potent inhibitor of proinflammatory mediators induced by endotoxin. Notably, inhibition of HO activity by SnPP completely abolished this effect, indicating that the HO pathway contributes to the isoflurane pretreatment-mediated anti-inflammatory action by modulating crucial steps of the inflammatory response.
Proinflammatory cytokines and bacterial products trigger iNOS expression and NO production in various cells, including macrophages treated with volatile anesthetics23. The NO can then produce proinflammatory and other effects detrimental to the cell. Our study demonstrated that isoflurane preconditioning reduced LPS-induced iNOS expression within the cells and prevented nitrite accumulation in the incubation medium. Recently, Xu et al demonstrated that 2% isoflurane inhibited iNOS and nitrite accumulation induced by LPS and interferon-γ in rat macrophages6. Blockade of the HO enzyme by administration of SnPP abolished this induction in isoflurane-pretreated cells, indicating that HO is directly involved in the mechanism of isoflurane preconditioning. Because the activation of the iNOS-NO pathway may mediate LPS-induced injury, our results suggest that attenuation of the activation of this pathway may be the mechanism by which isoflurane preconditioning induces protection.
In conclusion, our results provide the evidence that pretreatment with the nontoxic and clinically approved anesthetic isoflurane potently induced HO activity and HO-1 expression in RAW 264.7 macrophages. This induction correlated with a decrease in iNOS expression and impaired production of NO and TNF-α by LPS-stimulated macrophages. Inhibition of HO activity by SnPP reversed these effects, suggesting that the anti-inflammatory properties of isoflurane preconditioning involve the dynamic action of this cytoprotective protein. Our findings may also have implications for clinical medicine and experimental biology because isoflurane is frequently used in animal studies and in patients with ongoing pulmonary infection and inflammation.
Author contribution
Ye-sen ZHU and Hong JIANG designed the research; Qi-fang LI performed the research; Hui XU contributed new analytical reagents and tools; Yu SUN analyzed data; Qi-fang LI and Hong JIANG wrote the paper.
Acknowledgments
This work was supported by the Natural Science Foundation of the Shanghai Science Committee (No 07ZR14069), the Shanghai Rising-Star Program (No 08QA14044) and the National Natural Science Foundation of China (No 30801079).
References
- Barry U, Zuo Z. Opioids: old drugs for potential new applications. Curr Pharm Design. 2005;11:1343–50. doi: 10.2174/1381612053507459. [DOI] [PubMed] [Google Scholar]
- Zheng S, Zuo Z. Isoflurane preconditioning induces neuroprotection against ischemia via activation of p38 mitogen-activated protein kinases. Mol Pharmacol. 2004;65:1172–80. doi: 10.1124/mol.65.5.1172. [DOI] [PubMed] [Google Scholar]
- Zheng S, Zuo Z. Isoflurane preconditioning decreases glutamate receptor overactivation-induced Purkinje neuronal injury in rat cerebellar slices. Brain Res. 2005;1054:143–51. doi: 10.1016/j.brainres.2005.06.064. [DOI] [PubMed] [Google Scholar]
- Plachinta RV, Hayes JK, Cerilli LA, Rich GF. Isoflurane pretreatment inhibits lipopolysaccharide-induced inflammation in rats. Anesthesiology. 2003;98:89–95. doi: 10.1097/00000542-200301000-00017. [DOI] [PubMed] [Google Scholar]
- Reutershan J, Chang D, Hayes JK, Ley K. Protective effects of isoflurane pretreatment in endotoxin-induced lung injury. Anesthesiology. 2006;104:511–7. doi: 10.1097/00000542-200603000-00019. [DOI] [PubMed] [Google Scholar]
- Xu X, Feng J, Zuo Z. Isoflurane preconditioning reduces the rat NR8383 macrophage injury induced by lipopolysaccharide and interferon gamma. Anesthesiology. 2008;108:643–50. doi: 10.1097/ALN.0b013e318167aeb4. [DOI] [PubMed] [Google Scholar]
- Otterbein LE, Choi AM. Heme oxygenase: colors of defense against cellular stress. Am J Physiol. 2000;279:L1029–37. doi: 10.1152/ajplung.2000.279.6.L1029. [DOI] [PubMed] [Google Scholar]
- Otterbein LE. Carbon monoxide: innovative anti-inflammatory properties of an age-old gas molecule. Antioxid Redox Signal. 2002;4:309–19. doi: 10.1089/152308602753666361. [DOI] [PubMed] [Google Scholar]
- Li QF, Wang XR, Yang YW, Su DS. Up-regulation of hypoxia inducible factor 1alpha by isoflurane in Hep3B cells. Anesthesiology. 2006;105:1211–9. doi: 10.1097/00000542-200612000-00021. [DOI] [PubMed] [Google Scholar]
- Li Q, Zhu Y, Jiang H, Xu H, Liu H. Up-regulation of heme oxygenase-1 by isoflurane preconditioning during tolerance against neuronal injury induced by oxygen glucose deprivation. Acta Biochim Biophys Sin. 2008;40:803–10. [PubMed] [Google Scholar]
- Hoetzel A, Leitz D, Schmidt R, Tritschler E, Bauer I, Loop T, et al. Mechanism of hepatic heme oxygenase-1 induction by isoflurane. Anesthesiology. 2006;104:101–9. doi: 10.1097/00000542-200601000-00016. [DOI] [PubMed] [Google Scholar]
- Schmidt R, Tritschler E, Hoetzel A, Loop T, Humar M, Halverscheid L, et al. Heme oxygenase-1 induction by the clinically used anesthetic isoflurane protects rat livers from ischemia/ reperfusion injury. Ann Surg. 2007;245:931–42. doi: 10.1097/01.sla.0000256891.45790.4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otterbein LE, Bach FH, Alam J, Soares M, Tao Lu H, Wysk M, et al. Carbon monoxide has anti-inflammatory effects involving the mitogen-activated protein kinase pathway. Nat Med. 2000;6:422–8. doi: 10.1038/74680. [DOI] [PubMed] [Google Scholar]
- Otterbein LE, Soares MP, Yamashita K, Bach FH. Heme oxygenase-1: unleashing the protective properties of heme. Trends Immunol. 2003;24:449–55. doi: 10.1016/s1471-4906(03)00181-9. [DOI] [PubMed] [Google Scholar]
- Wagener FA, Volk HD, Willis D, Abraham NG, Soares MP, Adema GJ, et al. Different faces of the heme-heme oxygenase system in inflammation. Pharmacol Rev. 2003;55:551–71. doi: 10.1124/pr.55.3.5. [DOI] [PubMed] [Google Scholar]
- Sawle P, Foresti R, Mann BE, Johnson TR, Green CJ, Motterlini R. Carbon monoxide-releasing molecules (CO-RMs) attenuate the inflammatory response elicited by lipopolysaccharide in RAW264.7 murine macrophages. Br J Pharmacol. 2005;145:800–10. doi: 10.1038/sj.bjp.0706241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li QF, Wang XR, Yang YW, Lin H. Hypoxia upregulates hypoxia inducible factor (HIF)-3alpha expression in lung epithelial cells: characterization and comparison with HIF-1alpha. Cell Res. 2006;16:548–58. doi: 10.1038/sj.cr.7310072. [DOI] [PubMed] [Google Scholar]
- Foresti R, Clark JE, Green CJ, Motterlini R. Thiol compounds interact with nitric oxide in regulating heme oxygenase-1 induction in endothelial cells. Involvement of superoxide and peroxynitrite anions. J Biol Chem. 1997;272:18411–7. doi: 10.1074/jbc.272.29.18411. [DOI] [PubMed] [Google Scholar]
- Camhi SL, Alam J, Wiegand GW, Chin BY, Choi AM. Transcriptional activation of the HO-1 gene by lipopolysaccharide is mediated by 5′ distal enhancers: role of reactive oxygen intermediates and AP-1. Am J Respir Cell Mol Biol. 1998;18:226–34. doi: 10.1165/ajrcmb.18.2.2910. [DOI] [PubMed] [Google Scholar]
- Tracey KJ, Cerami A. Tumor necrosis factor: a pleiotropic cytokine and therapeutic target. Ann Rev Med. 1994;45:491–503. doi: 10.1146/annurev.med.45.1.491. [DOI] [PubMed] [Google Scholar]
- Bak I, Papp G, Turoczi T, Varga E, Szendrei L, Vecsernyes M, et al. The role of heme oxygenase-related carbon monoxide and ventricular fibrillation in ischemic/reperfused hearts. Free Radic Biol Med. 2002;33:639–48. doi: 10.1016/s0891-5849(02)00913-9. [DOI] [PubMed] [Google Scholar]
- Bak I, Szendrei L, Turoczi T, Papp G, Joo F, Das DK, et al. Heme oxygenase-1-related carbon monoxide production and ventricular fibrillation in isolated ischemic/reperfused mouse myocardium. FASEB J. 2003;17:2133–5. doi: 10.1096/fj.03-0032fje. [DOI] [PubMed] [Google Scholar]
- Zuo Z, Johns RA. Inhalational anesthetics up-regulate constitutive and lipopolysaccharide-induced inducible nitric oxide synthase expression and activity. Mol Pharmacol. 1997;52:606–12. doi: 10.1124/mol.52.4.606. [DOI] [PubMed] [Google Scholar]