Abstract
Aim:
To examine the mechanisms underlying the effects of atorvastatin on glucose and lipid metabolism.
Methods:
Mice with insulin resistance and obesity induced by monosodium glutamate (MSG) were used. Atorvastatin (80 mg·kg−1·d−1) or vehicle control treatment was given orally once a day for 30 days. Plasma levels of total cholesterol, triglycerides, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and free fatty acids were monitored. Serum insulin and glucose concentrations were used to calculate the insulin resistance index and insulin sensitivity index using a homeostasis model. Body length, waistline circumference, intraperitoneal adipose tissue mass, and total body mass were measured. Semi-quantitative RT-PCR and Western analysis were used to determine the expression of inflammatory factors and proteins involved in inflammation signaling pathways.
Results:
Atorvastatin improved insulin sensitivity, ameliorated glucose tolerance, and decreased plasma levels of total cholesterol, triglycerides, LDL-C, HDL-C and free fatty acids. Semi-quantitative RT-PCR and Western analysis revealed increased expression of interleukin 6 (IL-6) and tumor necrosis factor α (TNF-α) in serum and adipose tissue in MSG obese mice. Atorvastatin treatment decreased expression of IL-6, TNF-α, nuclear factor κB (NF-κB) and I-kappa-B (IκB) kinase-β, but increased the expression of IκB, in adipose tissue.
Conclusion:
Atorvastatin is a potential candidate for the prevention and therapy of diseases associated with insulin resistance such as type 2 diabetes mellitus and cardiovascular disease. One possible mechanism underlying the effects of atorvastatin on glucose and lipid metabolism may be to ameliorate a state of chronic inflammation.
Keywords: atorvastatin, insulin resistance, HMG-CoA reductase inhibitor, monosodium glutamate, obesity
Introduction
Obesity is frequently associated with metabolic syndrome, a disease state that includes glucose intolerance, insulin resistance, hypertension, hypertriglyceridemia, low level of high-density lipoprotein cholesterol (HDL-C), and type 2 diabetes mellitus (T2DM)1. Low-grade inflammation is associated with insulin resistance and precedes the onset of T2DM in obese individuals2. Adipose tissue is an important endocrine organ that regulates the insulin sensitivity of other peripheral insulin target tissues3. Excess adipose tissue, especially in the visceral compartment, results in excess secretion of peptide hormones and cytokines, which leads to whole-body insulin resistance and predisposes to T2DM4.
Tumor necrosis factor α (TNF-α), interleukin 6 (IL-6), and monocyte chemotactic protein 1 (MCP-1) are some of the inflammatory signaling molecules that may contribute to insulin resistance. TNF-α may enhance Ser307 phosphorylation of insulin receptor substrate 1 (IRS-1) proteins or other downstream effectors of the insulin signaling cascade that play negative regulatory roles in insulin action. Serine phosphorylation impairs insulin-stimulated tyrosine phosphorylation of IRS proteins, uncouples insulin signal transduction, and has been implicated in the development of insulin resistance5, 6, 7.
Previously, Hong8 implicated the signaling pathway of the transcription factor, nuclear factor κB (NF-κB), in the induction of insulin resistance. I-kappa-B (IκB) kinase (IKK) plays an important role in this pathway. IKKs, together with their upstream activating kinases, mediate signaling to NF-κB from a diverse array of stimuli, including TNF-α. TNF-α activates IKKs, which can in turn phosphorylate IκBs (the inhibitors of NF-κB) and activate NF-κB. Increased NF-κB activity up-regulates multiple inflammatory factors that aggravate insulin resistance9.
Statins, the inhibitors of 3-hydroxy-3-methyl glutaryl coenzyme A reductase (HMG-CoA) appear to have a number of potentially beneficial effects10, some of which are independent of their cholesterol-lowering effect. Some effects include improved endothelial function, anti-thrombotic and anti-proliferative effects, stabilization of atherosclerotic plaque, anti-cancer and anti-oxidant effects, and anti-inflammation. Regarding anti-inflammatory activity, statins may down-regulate activation of NF-κB in human endothelial and vascular smooth muscle cells11. By reducing the activity of this stimulator of IKK signaling, the anti-inflammatory consequences of statins may have benefits in insulin resistance. Therefore, we investigated the effects of atorvastatin, an HMG-CoA reductase inhibitor, on insulin resistance, glucose concentration, and lipid levels in an insulin-resistant mouse model of obesity.
Materials and methods
Reagents
Atorvastatin was obtained from Aifeimu Chemical Co (Zhejiang, China). Monosodium glutamate (MSG) was obtained from Huaboyuan Technologic Development Center (Beijing). RNAin protection liquid was from Applygen Technologies (Beijing). TRIzol reagent, random hexamer primers, and Superscript II reverse transcriptase were obtained from Invitrogen (Carlsbad, CA). Primary antibodies for NF-κB p65 and IκB-α were from Santa Cruz Biotechnology, Inc (Santa Cruz, CA). All other regents used in this paper were from Sigma Aldrich (St Louis, MO).
Animals and experimental protocol
Pregnant ICR mice were purchased from the Experimental Animal Center, Chinese Academy of Medical Sciences (Beijing), and cared for in accordance with the standards for laboratory animals established by the People's Republic of China (GB14925-2001). Monosodium glutamate (MSG) was subcutaneously injected in neonatal mice at 4 g/kg body weight once daily for 7 consecutive days after birth to induce obesity. Only mice with impaired insulin tolerance were used in this study12. Female and 6 months mice were divided into two groups (n=8 mice each) for treatment with vehicle (water) or atorvastatin (80 mg/kg), by oral administration. Treatment was given orally for 30 consecutive days, and mice underwent an insulin tolerance test (ITT) and oral glucose tolerance test (OGTT) and monitoring for plasma levels of cholesterol and triglycerides. On the last day of the experiment, mice were sacrificed by decapitatation. Plasma was collected for measurement of LDL-C, HDL-C, IL-6, and TNF-α. Body length, whole body mass, intraperitoneal adipose mass and waistline circumference were measured. The waistline index (waistline to body length) was calculated. Samples of plasma and adipose tissue were stored at −70 °C. Intraperitoneal adipose tissue was stored in an RNA protection liquid, RNAin, at −70 °C for later semi-quantitative RT-PCR analysis. Eight female ICR mice were used as normal non-obese controls.
Oral glucose tolerance test (OGTT) and insulin tolerance test (ITT)
After 10 days of oral atorvastatin treatment, obese mice were fasted 2 h before the OGGT. Two hours after atorvastatin (80 mg/kg) or vehicle (water) treatment, initial blood samples were drawn. Then, glucose (2 g/kg) was administered orally. Subsequent blood samples were taken at 0, 30, 60, and 120 min. The ITT was preceded by 20 days of atorvastatin or vehicle treatment. Fasted mice were given 0.4 U of insulin intraperitoneally, and then blood samples were taken at 0, 40, and 90 min. Plasma glucose concentrations were measured by the glucose oxidase method. The areas under the curve (AUC) from blood glucose recordings were calculated.
Biochemical analysis
Plasma levels of total cholesterol, triglycerides, LDL-C, HDL-C, and free fatty acids (FFAs) were determined by enzymatic colorimetric methods with commercial kits (Biosino Bio-Technology and Science Inc, Beijing). Plasma insulin (PI) was measured with a radioimmunoassay kit (Chinese Institute of Atomic Energy, Beijing). Adipose tissue samples were homogenized in ice-cold PBS buffer containing 10 mmol/L sodium fluoride, 10 μg/mL leupeptin, and 10 μg/mL aprotinin and centrifuged at 14 000×g for 15 min and the supernatants were collected for assay. The concentrations of TNF-α and IL-6 in plasma and adipose tissue were measured with a radioimmunoassay kit (North TZ-Biotech, Beijing).
Insulin resistance and insulin sensitivity index calculations
The homeostasis model assessment was used to calculate the insulin resistance (HOMA-IR) index and insulin sensitivity index (ISI) using the values of fasting plasma glucose (FPG) and PI as follows: ISI=1/(FPG×PI)×1000, with FPG expressed as mg/dL and PI as mU/L; HOMA-IR=FPG×PI/22.5, with FPG expressed as mmol/L and PI as mU/L.
RNA preparation and semi-quantitative RT-PCR
Total RNA was isolated from mouse adipose tissue with TRIzol reagent (Invitrogen, Carlsbad, CA). First-strand cDNA was synthesized from 5 μg of total RNA with random hexamer primers and Superscript II reverse transcriptase (Invitrogen). The reaction mixture was amplified with primers specific for inflammatory factors and proteins (Table 1) in a total volume of 20 μL. Linearity of the PCR amplification was tested with amplification cycles between 32 and 40. The PCR products were analyzed on a 2% agarose gel, and the intensity of the corresponding bands was determined using a Kodak image station 440CF and 1D image analysis software (Eastman Kodak; Rochester, NY). mRNA expression of the genes was normalized to that of GAPDH13.
Table 1. Primers used for RT-PCR of inflammatory factors and proteins in monosodium glutamate (MSG)-induced obese mice with insulin resistance.
| Target gene | Forward primer | Reverse primer |
|---|---|---|
| GAPDH | 5′-AGGTCGGTGTGAACGGATTTG-3′ | 5′-TGTAGACCATGTAGTTGAGGTCA-3′ |
| NF-κB p65 | 5′-AGGCTTCTGGGCCTTATGTG-3′ | 5′-TGCTTCTCTCGCCAGGAATAC-3′ |
| IκB-α | 5′-TGAAGGACGAGGAGTACGAGC-3′ | 5′-TTCGTGGATGATTGCCAAGTG-3′ |
| IKK-β | 5′-ACAGCCAGGAGATGGTACG-3′ | 5′-CAGGGTGACTGAGTCGAGAC-3′ |
| TNF-α | 5′-CCCTCACACTCAGATCATCTTCT-3′ | 5′-GCTACGACGTGGGCTACAG-3′ |
| IL-6 | 5′-TAGTCCTTCCTACCCCAATTTCC-3′ | 5′-TTGGTCCTTAGCCACTCCTTC-3′ |
Adipose tissue homogenization and Western analysis
Adipose tissue samples were homogenized in ice-cold buffer containing 50 mmol/L HEPES (pH 7.6), 150 mmol/L sodium chloride, 20 mmol/L beta-glycerophosphate, 10 mmol/L sodium fluoride, 2 mmol/L EDTA, 10% glycerol, 1 mmol/L magnesium chloride, 1 mmol/L calcium chloride, 10 μg/mL leupeptin, and 10 μg/mL aprotinin. Tissue homogenates were clarified by centrifugation at 14 000×g for 15 min, and protein concentrations in the supernatant were determined with a Bradford assay. Proteins in the supernatants of the tissue homogenates were resolved by SDS-PAGE and transferred to PVDF membrane. Bound proteins were blocked with 1% nonfat dry milk in Tris-buffered saline with 0.1% Tween 20, and probed with specific primary antibodies (NF-κB p65 and IκB-α from Santa Cruz). The membranes were washed with Tris-buffered saline with 0.5% Tween 20, then incubated with horseradish peroxidase-conjugated secondary antibody (Promega Corp, Madison, WI). Proteins were visualized by chemiluminescence reactions, and the intensity of the corresponding bands was analyzed with a Kodak image station 440CF and 1D image analysis software (Eastman Kodak). The expression of proteins was normalized to that of GAPDH14.
Statistical analysis
Results are presented as means±SEM. Statistical significance of differences was assessed by ANOVA, followed by the t-test. P<0.05 was considered statistically significant. All analyses were performed using SPSS version 13.0.
Results
Insulin tolerance
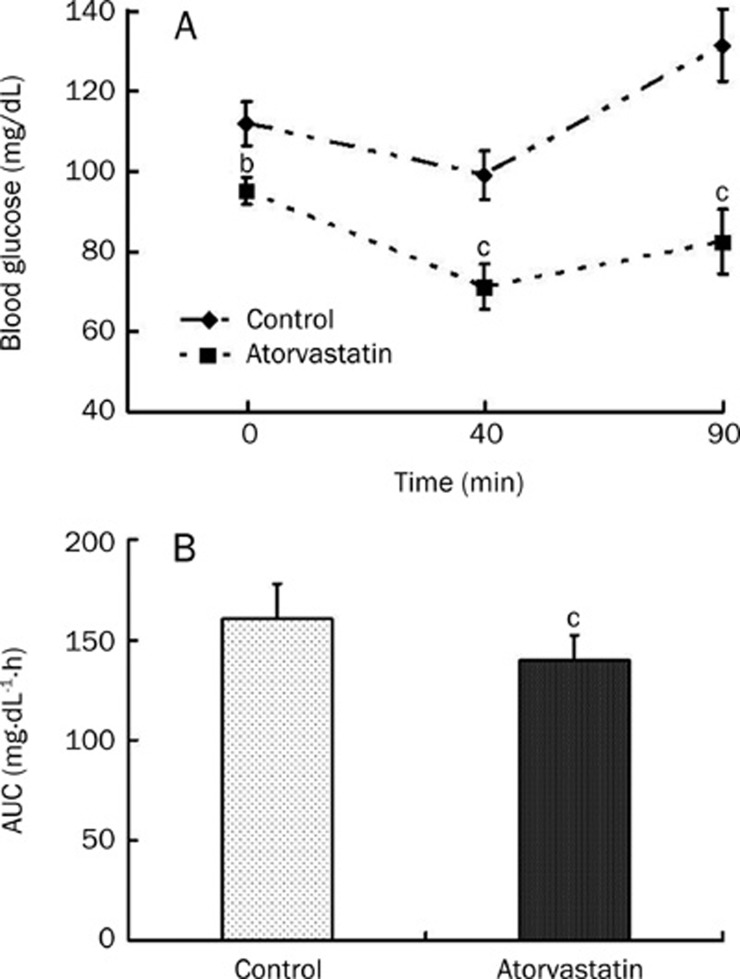
Plasma glucose levels after insulin injection were significantly lower in the obese mice treated with atorvastatin (80 mg/kg) than those in the vehicle-treated control obese mice at all times tested. As shown in Figure 1B the mean AUC for glucose was significantly reduced after atorvastatin treatment, compared to the control treatment (n=8, P<0.01, Figure 1).
Figure 1.
Effect of atorvastatin on insulin tolerance in MSG-induced obese mice with insulin resistance. (A) Mean blood glucose; (B) Mean area under the curve (AUC) by insulin tolerance test (ITT). Obese mice were challenged with oral glucose as described in the materials and methods, and blood glucose measured at the indicated times by tail blood sampling. Obese mice (n=8 /per group) were treated and untreated with atorvastatin (80 mg·kg−1·d−1) for 20 d. Results show means±SEM. bP<0.05, cP<0.01 compared with groups untreated with atorvastatin.
Oral glucose tolerance
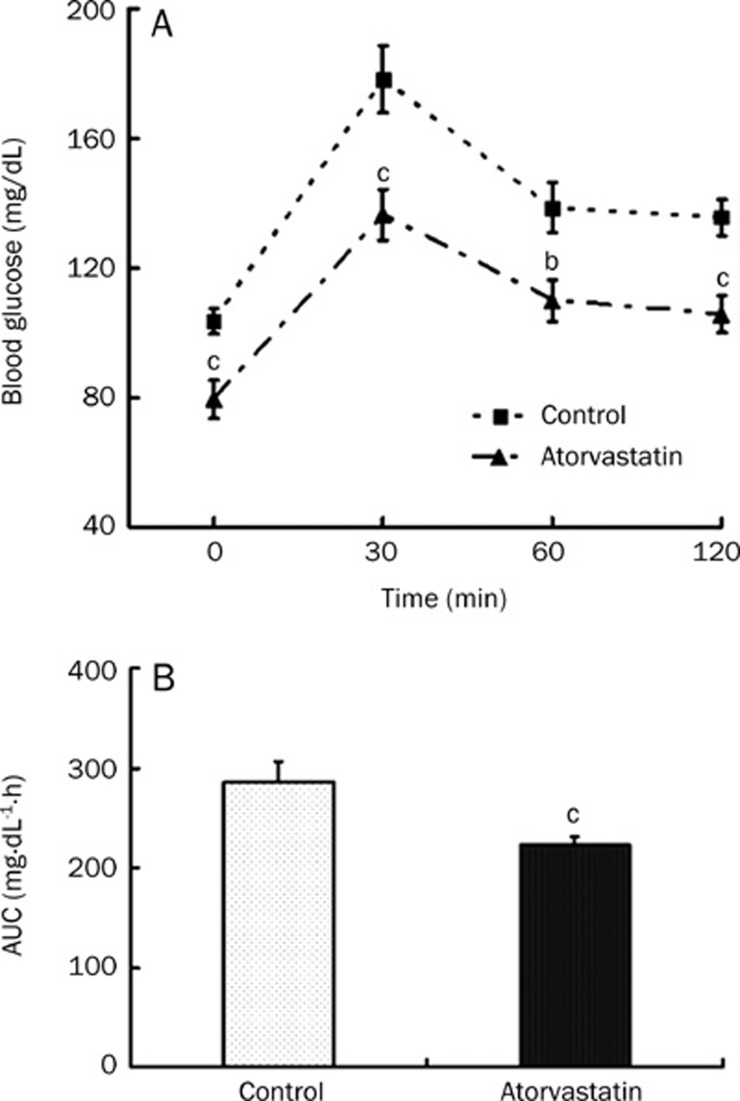
Compared to the control treatment, atorvastatin treatment produced lower blood glucose concentrations before and 30, 60 and 120 min after glucose loading (Figure 2A), and reduced the mean glucose AUC (Figure 2B).
Figure 2.
Effect of atorvastatin on glucose tolerance in MSG-induced obese mice with insulin resistance. (A) Mean blood glucose; (B) Mean area under the curve (AUC) by oral glucose tolerance test (OGTT). Mice (n=8/per group) were treated with atorvastatin (80 mg·kg−1·d−1) for 10 d. n=8. All data are represented by means±SEM. bP<0.05, cP<0.01 vs control group.
Effect of atorvastatin on plasma lipid profile
On day 12, obese mice treated with atorvastatin showed significantly lower plasma levels of total cholesterol, LDL-C and HDL-C than the control obese mice (P<0.01). The atorvastatin treated mice also had markedly lower levels of triglycerides and FFAs (P<0.05, Table 2).
Table 2. Effect of atorvastatin on lipid metabolism in MSG-induced obese mice with insulin resistance. All data are represented by mean ±SEM. Mice were treated with atorvastatin for 30 d. n=8 mice/group. bP<0.05, cP<0.01 vs control-treated obese mice.
| Group | Triglycerides (mg/dL) | Total cholesterol (mg/dL) | LDL-C (mg/dL) | HDL-C (mg/dL) | Free fatty acids (μEq/L) |
|---|---|---|---|---|---|
| Control | 79.9±5.1 | 103.9±7.8 | 16.7±1.0 | 77.7±6.4 | 415.7±15.9 |
| Atorvastatin (80 mg/kg) | 63.8±4.1b | 59.3±5.4c | 10.4±0.8c | 37.5±2.9c | 352.0±24.3b |
LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol.
Characteristics of MSG-induced obese mice
The physical characteristics of the normal non-obese mice and the obese mice treated with either atorvastatin or vehicle control are shown in Table 3. Normal non-obese mice were lean and had a smaller waistline circumstance, body weight and smaller waistline index than MSG-induced obese mice treated with vehicle control (P<0.01). Vehicle control-treated obese mice had more intraperitoneal fat and a greater intraperitoneal fat index than did non-obese mice (P<0.01). Atorvastatin treatment had no effect on body weight, body length, waistline, or intraperitoneal fat weight and index as compared with vehicle control treatment in obese mice.
Table 3. Effect of atorvastatin on body characteristics of MSG-induced obese mice with insulin resistance. Data are mean±SEM. Mice were treated with atorvastatin for 30 d. n=8 mice/group. bP<0.05, cP<0.01 vs control obese mice.
| Group | Body weight (g) | Body length (cm) | Waistline (cm) | Intraperitoneal fat (g) | Waistline index | Intraperitoneal fat index |
|---|---|---|---|---|---|---|
| Normal non-obese | 30.7±2.4 | 10.1±0.3b | 8.73±0.42c | 0.600±0.100c | 0.86±0.062c | 0.02±0.003c |
| Control | 63.0±7.5 | 10.9±0.5 | 13.24±0.77 | 6.650±1.753 | 1.21±0.090 | 10.54±2.416 |
| Atorvastatin (80 mg/kg) | 59.7±6.2 | 10.5±0.3 | 12.80±0.85 | 6.600±1.125 | 1.22±0.077 | 11.05±1.413 |
Waistline index=waistline circumference/body length. Intraperitoneal fat index is intraperitoneal fat/body weight.
Effect of atorvastatin on inflammatory factors in plasma and adipose tissue
The concentrations of IL-6 and TNF- α in serum and adipose tissue are shown in Table 4. The serum concentration of IL-6 and TNF-α in vehicle control-treated obese mice was similar to that in normal non-obese mice. The atorvastatin-treated obese mice showed no difference in content from the vehicle-control treated obese mice. The adipose-tissue concentrations of IL-6 and TNF-α were significantly greater in vehicle-treated control obese mice than in normal non-obese mice (n=8, P<0.01). Thirty-day atrovastatin treatment produced significantly lower adipose-tissue concentrations of IL-6 and TNF-α compared to vehicle control treatment in the obese mice (n=8, P<0.05).
Table 4. Effect of atorvastatin on levels of TNF-α and IL-6 in MSG-induced obese mice with insulin resistance. Data are mean±SEM. Mice were treated with atorvastatin for 30 days. n=8 mice/group. aP>0.05, bP<0.05, cP<0.01 vs control-treated obese mice.
| Group | Serum IL-6 (ng/mL) | IL-6 in adipose tissue (ng/mg protein) | Serum TNF-α (ng/mL) | TNF-α in adipose tissue (ng/mg protein) |
|---|---|---|---|---|
| Normal non-obese | 0.096±0.007 | 0.127±0.025c | 1.21±0.071 | 1.44±0.029c |
| Control | 0.091±0.007 | 0.341±0.039 | 1.19±0.039 | 3.79±0.062 |
| Atorvastatin (80 mg/kg) | 0.069±0.007a | 0.232±0.032b | 1.34±0.025 | 2.20±0.021b |
Homeostasis model assessment of insulin resistance (HOMA-IR) index and insulin sensitivity index (ISI)
The calculated values for the insulin resistance index and insulin sensitivity index are shown in Table 5. Fasting serum insulin levels were significant higher in vehicle treated control obese mice than in normal non-obese mice. The HOMA-IR index was also higher in vehicle treated control mice than in normal non-obese mice (n=8, P<0.001). The ISI for vehicle treated control mice was lower than that for normal non-obese mice (n=8, P<0.001). Atorvastatin treatment decreased the HOMA-IR index and increased the ISI compared to vehicle control treatment in obese mice (P<0.05, P<0.01, respectively) (Table 5).
Table 5. Effect of atorvastatin on homeostasis model assessment of insulin resistance (HOMA-IR) index and insulin sensitivity index (ISI) in MSG-induced obese mice with insulin resistance. Data are mean±SEM. Mice were treated with atorvastatin for 30 days. n=8 mice/group. bP<0.05, cP<0.01 vs control-treated obese mice.
| Group | Fasting blood glucose (mg/dL) | Serum insulin (mIU/L) | ISI (×10−4) | HOMA-IR |
|---|---|---|---|---|
| Normal non-obese | 101.8±4.0c | 39.6±2.1c | 2.6±0.18c | 178.8±10.5c |
| Control | 135.6±6.1 | 177.3±34.2 | 0.6±0.11 | 1071.3±225.7 |
| Atorvastatin (80 mg/kg) | 116.8±4.8b | 85.0±10.4b | 1.2±0.20c | 429.0±55.5b |
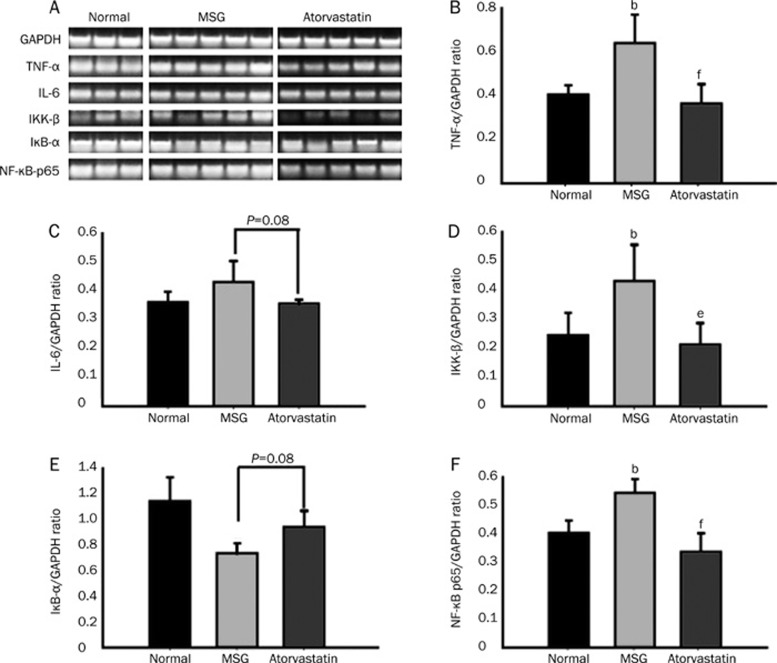
Semi-quantitative RT-PCR analysis of inflammatory factors
A semi-quantitative analysis of the expression of factors involved in inflammation pathways are shown in Figure 3. The expression of TNF-α and IL-6 was higher in the vehicle-treated control obese mice than in normal non-obese mice (Figure 3B, 3C), and the expression of IκB was lower in vehicle treated obese controls than in normal non-obese mice (Figure 3E). Atorvastatin treatment decreased the expression of TNF-α, IL-6, NF-κB, and IKK-β (P<0.01, P=0.08, P<0.05, P<0.01, respectively) and enhanced of the expression of IκB (P=0.08) compared to vehicle control treatment in obese mice (Figure 3).
Figure 3.
Effect of atorvastatin on inflammatory factors gene expressions at transcriptional levels in adipose tissue of MSG-induced obese mice with insulin resistance. Mice (n=5) were treated with atorvastatin (80 mg·kg−1·d−1) for 30 days. Non-obese mice (n=3) and vehicle control-treated obese mice (n=5) were normal and MSG respectively. (A) The products of semi-quantitative PCR were run on 2.0% agarose gels and stained with ethidium bromide. The expression level of each inflammatory factors mRNA was normalized to that of GAPDH shown in panel A. Atorvastatin inhibited the expression of TNF-α and IL-6 in the adipose tissue (B, C), meantime atorvastatin decreased the expression of IKK-β and NF-κB p65 (D, F). Futhermore, atorvastatin increased the IκB-α expression in adipose tissue (E). Values show means±SEM as ratio. bP<0.05 vs normal non-obese mice; eP<0.05, fP<0.01 vs control-treated obese mice.
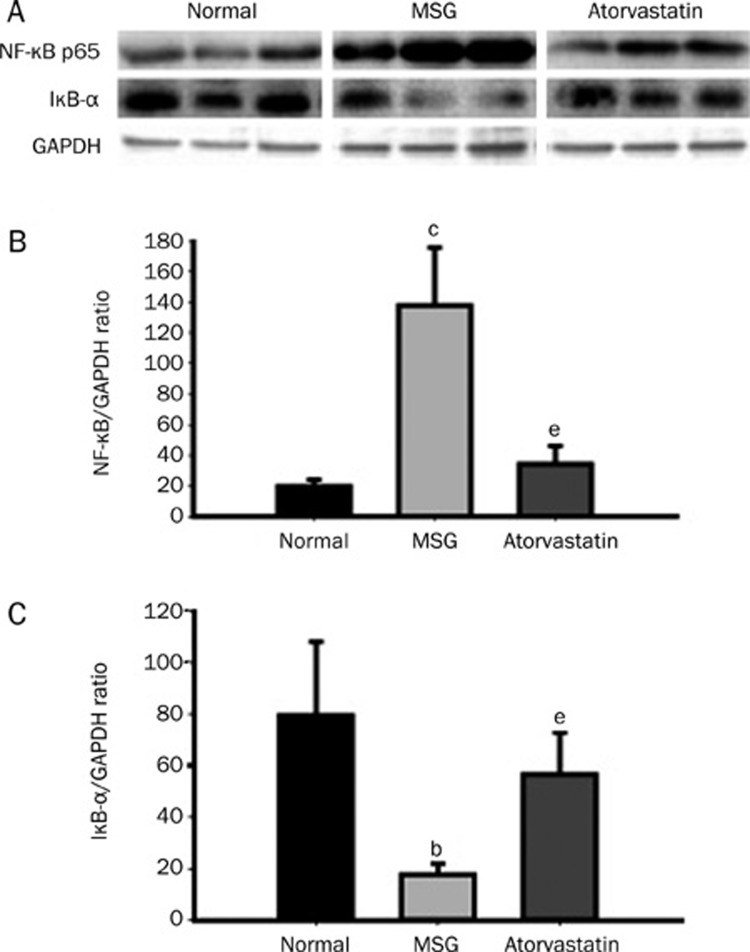
Western blot analysis of NF-κB p65 and IκB-α
The level of NF-κB p65 and IκB-α proteins were analyzed by Western blot analysis, and the results shown in Figure 4. The protein level of NF-κB was higher in vehicle treated control obese mice than in normal non-obese mice. Atorvastatin treatment reduced the protein level of NF-κB in obese mice compared to vehicle-treated control mice (P<0.05, Figure 4A, 4B). The level of IκB-α protein was lower in vehicle treated controls than in normal non-obese mice, and atorvastatin treatment enhanced the protein expression of IκB-α in obese mice (P<0.05, Figure 4A, 4C).
Figure 4.
Effect of atorvastatin on the expression of NF-κB p65 and IκB-α at translational levels in adipose tissue of MSG-induced obese mice with insulin resistance. Mice were treated with atorvastatin (80 mg·kg−1·d−1) for 30 days. Normal: non-obese control mice; MSG: vehicle control-treated obese mice; Atorvastatin: atorvastatin-treated obese mice. The protein expressions of NF-κB p65, IκB-α, and GAPDH were analyzed by Western blot assay (A), the expressional levels of NF-κB p65, IκB-α, and GAPDH were normalized to that of GAPDH, respectively. Atorvastatin significantly reduced the expression of NF-κB p65 in adipose tissue compared to MSG group (B), but induced the expression of IκB-α (C). Values are means±SEM as ratio. bP<0.05, cP<0.01 vs normal mice; eP<0.05 vs MSG mice.
Discussion
Insulin resistance is the critical pathological feature of type 2 diabetes mellitus, obesity, metabolic syndrome, and aging15. Although the precise pathogenesis of insulin resistance remains ill-defined, several factors have been proposed to have a role in this process, such as adipokines, defects in the insulin signaling pathway, mitochondrial dysfunction and inflammation16, 17. In the past few years it has been shown clearly that obesity, along with diabetes, is characterized by a state of chronic low-grade inflammation18, 19, 20 implying that approaches designed to improve state of chronic low-grade inflammation should be useful in attenuating insulin resistance with obesity.
The effects of statins on insulin sensitivity had been reported in the past years, simvastatin and atorvastatin may improve insulin sensitivity in diabetic patients21; however, others have reported that simvastatin either did not change or worsened insulin sensitivity in diabetic patients22, 23. And there are no reports exist of their mechanism of action in insulin resistance, obesity animal models. We investigated the effect of atorvastatin on glucose metabolism and insulin resistance and the mechanism of action in MSG-induced obese mice, a model of T2DM with obesity, hyperinsulinemia, insulin resistance, hyperlipidemia and hyperglycemia24. Atorvastatin significantly inhibited the plasma glucose and decreased the plasma insulin level and the HOMA-IR index but increased the ISI in obese mice. These findings suggest that atorvastatin may improve insulin resistance in MSG-induced obese mice.
As mentioned before, mounting evidence indicates that adipose tissue is an important cytokines-secretory organ25 and that adiposity contributes to a chronic state of systemic inflammation26. Actually, the molecular connection between obesity and inflammation was documented in 1993, after the demonstration of enhanced expression of TNF-α in adipose tissue of obese rodents, and more importantly, the amelioration of insulin sensitivity after neutralization of this multi-potent inflammatory cytokine. Inflammatory mediators derived from adipose tissue and increased in level in obesity include IL-6, IL-1β, and monocyte MCP-127, 28. Further, growing evidence suggests that, similar to TNF-α, these and other inflammatory molecules negatively affect insulin sensitivity through activation of NF-κB, a transcription factor, which triggers the production of numerous inflammatory mediators such as TNF-α and IL-6. These factors can sustain and heighten inflammatory activation, thus leading to local and systemic insulin resistance29. In our study, atorvastatin significantly decreased the secretory level of TNF-α and IL-6 in adipose tissue. This finding suggests that atorvastatin may inhibit the generation of inflammatory factors, thereby improving insulin resistance in MSG-induced obese mice.
Furthermore, atorvastatin decreased the mRNA level of TNF-α and IL-6 but not significantly (P=0.08) in adipose tissue, which is consistent with the results of their secretory levels in adipose tissue. In addition, atorvastatin significantly decreased the expression of IKK-β and NF-κB and increased that the expression of the inhibitor of NF-κB, IκB-α. IKK-β is an important kinase that can affect insulin signaling through serine phosphorylation of IRS-1 and by phosphorylation of IκB-α, which leads to stimulation of the NF-κB pathway. IκB -α inhibits the transcriptional activity of NF-κB in the cytoplasm by preventing the nuclear translocation of NF-κB. In the nucleus, it dissociates NF-κB from DNA and transports it back to the cytoplasm30. To further support the mechanism of atorvastatin action through inflammatory factors, we analyzed the protein level of NF-κB and IκB-α and found that atorvastatin significantly reduced the level of NF-κB protein and increased protein levels of IκB-α. These findings support our hypothesis that atorvastatin inhibits the activity of IKK-β and NF-κB, and increases that of IκB-α, which inhibits the activity of NF-κB. Thus, atorvastatin reduced inflammatory factor activation and improved insulin resistance in MSG-induced obese mice.
Results from our study and that of others raise questions about the effects in humans being treated with approved doses of atorvastatin. We chose doses of atorvastatin comparable to those used for treatment of hypercholesterolemia in humans. The dose of 80 mg·kg−1·d−1 for mice is estimated to be slightly higher than the maximal approved dose for humans. Atorvastatin has a high LD50 (5000 mg/kg) in the mice31 so the dose used was safe for the mice in our study. Atorvastatin can adversely affect liver function in some patients with liver dysfunction32. In our study, we also assayed AST and ALT levels in serum and found the liver function of MSG-induced obese mice with atorvastatin treatment had no difference from that of the treated control mice (data not shown). Interesting, we found a decrease in plasma HDL-cholesterol after atorvastatin treatment. This result seems to be conflicting with other reports about the role of increasing HDL with atorvastatin. However, compared to humans, mice and rats transport most of their serum cholesterol in the HDL-C fraction, not the LDL-C fraction33. In this mouse model, when atorvastatin decreased the plasma level of total cholesterol, the plasma level of HDL was decreased. However, we have used the mice with MSG-induced obesity as a model of obesity-associated insulin resistance for many years, and many characteristics of this animal model have a striking resemblance to human disease. The most important characteristic of such mice is abdominal obesity. A large amount of abdominal fat in MSG-induced obese mice with insulin resistance could be related to chronic inflammation, so MSG-induced obese mice are suitable for study of the effect of atorvastatin on improving insulin resistance to ameliorate the state of chronic inflammation and inhibit the activity of proteins in the inflammatory pathway.
In conclusion, atorvastatin treatment decreased lipid levels, improved glucose metabolism after glucose loading, and improved insulin resistance in MSG-induced obese mice. Possible mechanisms of the improved glucose metabolism with atorvastatin treatment may include ameliorating the state of chronic inflammation by inhibiting synthesis of inflammatory factors through inhibiting the expression of NF-κB and IKK-β, as well as increasing the expression of IκB-α in adipose tissue.
Author contribution
Ning ZHANG and Zhu-fang SHEN designed research; Ning ZHANG, Yi HUAN, Hui HUANG, Guang-ming SONG and Su-juan SUN performed research; Ning ZHANG analyzed data; Ning ZHANG and Zhu-fang SHEN wrote the paper.
Acknowledgments
We thank Prof Ming-zhi XIE for her suggestions about this experimental design.
References
- Bosello O, Zamboni M. Visceral obesity and metabolic syndrome. Obes Rev. 2000;1:47–56. doi: 10.1046/j.1467-789x.2000.00008.x. [DOI] [PubMed] [Google Scholar]
- Christian H, Sophie S, Wolfgang R, Burkhard H, Heiko S, Horst W, et al. Low-grade inflammation, obesity, and insulin resistance in adolescents. J Clin Endocrinol Metab. 2007;92:4569–74. doi: 10.1210/jc.2007-0955. [DOI] [PubMed] [Google Scholar]
- Koistinen HA, Forsgren M, Wallberg HH, Zierath JR. Insulin action on expression of novel adipose genes in healthy and type 2 diabetic subjects. Obes Res. 2004;12:25–31. doi: 10.1038/oby.2004.5. [DOI] [PubMed] [Google Scholar]
- Kahn BB, Flier JS. Obesity and insulin resistance. J Clin Invest. 2000;106:473–81. doi: 10.1172/JCI10842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paz K, Hemi R, LeRaith D, Karasik A, Elhanany E, Kanety H, et al. A molecular basis for insulin resistance: elevated serine/threonine phosphorylation of IRS-1 and IRS-2 inhibits their binding to the juxta membrane region of the insulin receptor and impairs their ability to undergo insulin-induced tyrosine phosphorylation. J Biol Chem. 1997;272:29911–8. doi: 10.1074/jbc.272.47.29911. [DOI] [PubMed] [Google Scholar]
- Hotamisligil GS, Peraldi P, Budavari A, Ellis R, White MF, Spiegelman BM. IRS-1-mediated inhibition of insulin receptor tyrosine kinase activity in TNF-α and obesity induced insulin resistance. Science. 1996;271:665–8. doi: 10.1126/science.271.5249.665. [DOI] [PubMed] [Google Scholar]
- Tanti JF, Grémeaux T, van Obberghen E, Le Marchand-Brustel Y. Serine/threonine phosphorylation of insulin receptor substrate 1 modulates insulin receptor signaling. J Biol Chem. 1994;269:6051–7. [PubMed] [Google Scholar]
- Hong R, Nir H, Todd RG, Luk VP, Harvey FL. Tumor necrosis factor-α suppresses adipocyte-specific genes and activates expression of preadipocyte genes in 3T3-L1 adipocytes: nuclear factor-kappaB activation by TNF-α is obligatory. Diabetes. 2002;51:1319–36. doi: 10.2337/diabetes.51.5.1319. [DOI] [PubMed] [Google Scholar]
- Prigent M, Barlat I, Langen H, Dargemont C. IκBα and IκBα/NF-κB complexes are retained in the cytoplasm through interaction with a novel partner, RasGAP SH3-binding protein 2. J Biol Chem. 2000;275:36441–9. doi: 10.1074/jbc.M004751200. [DOI] [PubMed] [Google Scholar]
- Esther L, Mat D. HMG-CoA reductase inhibitors: lipid-lowering and beyond. Drug Discov Today Ther Strateg. 2004;1:189–94. [Google Scholar]
- Wolfgang D, Jozef D, Matthias F, Hannes FA, Severin PS, Mikko A, et al. HMG-CoA reductase inhibitors regulate inflammatory transcription factors in human endothelial and vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 2003;23:58–63. doi: 10.1161/01.atv.0000043456.48735.20. [DOI] [PubMed] [Google Scholar]
- Macho L, Ficková M, Jezová D, Zórad S. Late effects of postnatal administration of monosodium glutamate on insulin action in adult rats. Physiol Res. 2000;49:S79–85. [PubMed] [Google Scholar]
- Tokushi K, Fumiaki I, Satoshi M, Koichi H. Gene expression of resistin in adipose tissue and mammary gland of lactating and non-lactating cows. J Endocrinol. 2003;178:R1–R5. doi: 10.1677/joe.0.178r001. [DOI] [PubMed] [Google Scholar]
- Shana S, Zhao BP, Yang JZ. Enhanced muscle by myostatin propeptide increases adipose tissue adiponectin, PPAR-α and PPAR- γ expressions. Biochem Biophys Res Commun. 2008;369:767–73. doi: 10.1016/j.bbrc.2008.02.092. [DOI] [PubMed] [Google Scholar]
- Newsholme P, Haber EP, Hirabara SM, Rebelato EL, Procopio J, Morgan D, et al. Diabetes associated cell stress and dysfunction: role of mitochondrial and non-mitochondrial ROS production and activity. J Physiol. 2007;583:92–4. doi: 10.1113/jphysiol.2007.135871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muoio DM, Newgard CB. Mechanisms of disease: molecular and metabolic mechanisms of insulin resistance and beta-cell failure in type 2 diabetes. Nat Rev Mol Cell Biol. 2008;9:193–205. doi: 10.1038/nrm2327. [DOI] [PubMed] [Google Scholar]
- Kim JA, Wei Y, Sowers JR. Role of mitochondrial dysfunction in insulin resistance. Circ Res. 2008;102:401–14. doi: 10.1161/CIRCRESAHA.107.165472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engstrom G, Stavenow L, Hedblad B, Lind P, Eriksson KF, Janzon L, et al. Inflammation-sensitive plasma proteins, diabetes, and mortality and incidence of myocardial infarction and stroke: a population-based study. Diabetes. 2003;52:442–7. doi: 10.2337/diabetes.52.2.442. [DOI] [PubMed] [Google Scholar]
- Festa A, D'Agostino R, Jr, Williams K, Karter AJ, Mayer-Davis EJ, Tracy RP, et al. The relation of body fat mass and distribution to markers of chronic inflammation. Int J Obes Relat Metab Disord. 2001;25:1407–15. doi: 10.1038/sj.ijo.0801792. [DOI] [PubMed] [Google Scholar]
- Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW. C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue. Arterioscler Thromb Vasc Biol. 1999;19:972–8. doi: 10.1161/01.atv.19.4.972. [DOI] [PubMed] [Google Scholar]
- Paolisso G, Barbagallo M, Petrella G, Ragno E, Barbieri M, Giordano M, et al. Effects of simvastatin and atorvastatin administration on insulin resistance and respiratory quotient in aged dyslipidemic non-insulin dependent diabetic patients. Atherosclerosis. 2000;150:121–7. doi: 10.1016/s0021-9150(99)00352-4. [DOI] [PubMed] [Google Scholar]
- Farrer M, Winocour PH, Evans K, Neil HA, Laker MF, Kesteven P, et al. Simvastatin in non-insulin-dependent diabetes mellitus: effect on serum lipids, lipoproteins and haemostatic measures. Diabetes Res Clin Pract. 1994;23:111–9. doi: 10.1016/0168-8227(94)90018-3. [DOI] [PubMed] [Google Scholar]
- Ohrvall M, Lithell H, Johansson J, Vessby B. A comparison between the effects of gemfibrozil and simvastatin on insulin sensitivity in patients with non-insulin-dependent diabetes mellitus and hyperlipoproteinemia. Metabolism. 1995;44:212–7. doi: 10.1016/0026-0495(95)90267-8. [DOI] [PubMed] [Google Scholar]
- Hirata AE, Andrade IS, Vaskevicius P, Dolnikoff MS. Monosodium glutamate (MSG)-obese rats develop glucose intolerance and insulin resistance to peripheral glucose uptake. Braz J Med Biol Res. 1997;30:671–4. doi: 10.1590/s0100-879x1997000500016. [DOI] [PubMed] [Google Scholar]
- Ahima RS, Flier JS. Adipose tissue as an endocrine organ. Trends Endocrinol Metab. 2000;11:327–32. doi: 10.1016/s1043-2760(00)00301-5. [DOI] [PubMed] [Google Scholar]
- Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW. C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue. Arterioscler Thromb Vasc Biol. 1999;19:972–8. doi: 10.1161/01.atv.19.4.972. [DOI] [PubMed] [Google Scholar]
- Kern PA, Ranganathan S, Li C, Wood L, Ranganathan G. Adipose tissue tumor necrosis factor and interleukin-6 expression in human obesity and insulin resistance. Am J Physiol Endocrinol Metab. 2001;280:E745–51. doi: 10.1152/ajpendo.2001.280.5.E745. [DOI] [PubMed] [Google Scholar]
- Peter S, David JL. Monocyte chemoattractant protein 1 in obesity and insulin resistance. Proc Natl Acad Sci. 2003;100:7265–70. doi: 10.1073/pnas.1133870100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilg H, Moschen AR. Inflammatory mechanisms in the regulation of insulin resistance. Mol Med. 2008;14:222–31. doi: 10.2119/2007-00119.Tilg. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoelson SE, Lee J, Yuan M. Inflammation and the IKKβ/IκB/NF-κB axis in obesity- and diet-induced insulin resistance. Int J Obes. 2003;27:49–52. doi: 10.1038/sj.ijo.0802501. [DOI] [PubMed] [Google Scholar]
- Victor C, Melvin K, Charles R, Cheryl H, Jeffrey T. The genotoxicity profile of atorvastatin, a new drug in the treatment of hypercholesterolemia. Mutat Res. 1995;343:95–107. doi: 10.1016/0165-1218(95)90076-4. [DOI] [PubMed] [Google Scholar]
- Clarke AT, Mills PR. Atorvastatin associated liver disease. Dig Liver Dis. 2006;38:772–7. doi: 10.1016/j.dld.2006.04.013. [DOI] [PubMed] [Google Scholar]
- Harris WS. n-3 Fatty acids and serum lipoproteins: animal studies. Am J Clin Nutr. 1997;65:1611S–1616S. doi: 10.1093/ajcn/65.5.1611S. [DOI] [PubMed] [Google Scholar]