Abstract
Aim:
The aim of this study was to investigate the protective effect of genistein postconditioning on hypoxia/reoxygenation-induced injury in human gastric epithelial cells and to begin a tentative discussion on the mechanism behind this protection.
Methods:
A model of hypoxia/reoxygenation-induced injury was established in the human gastric epithelial cell line (GES-1). All cells in our present study were randomly divided into five groups: a normal control group (N), a hypoxia/reoxygenation group (H/R), a genistein postconditioning group (GP), a capsazepine+genistein postconditioning group (C+GP) and a DMSO vehicle postconditioning group (DM). The methods used included MTT assays to test cell viability, flow cytometric analyses to quantify the percentage of cell apoptosis, Western blot analyses to measure the protein expression of calcitonin gene-related peptide (CGRP), Bcl-2, and Bax, and immunocytochemistry assays to detect the expression of CGRP in each group.
Results:
The MTT assays indicated that the cell viabilities of the groups were 100.0%±0%, 51.4%±4.1%, 66.7%±2.0%, 56.1%±2.8%, and 50.7%±2.4%, respectively. Compared with the H/R group, the viability of the GP group was significantly increased (P<0.01). Flow cytometric analysis showed that the cell apoptosis percentage of each group was 2.28%±0.44%, 12.17%±2.15%, 5.40%±1.22%, 10.43%±1.37%, and 11.02%±2.19%, respectively. Western blot analysis demonstrated that CGRP, Bcl-2, and Bax were expressed in normal human gastric epithelial cells. Compared with the H/R group, the GP group exhibited increased expression of CGRP and Bcl-2 and decreased expression of Bax. Immunocytochemistry assays indicated that the number of CGRP-positive cells in the GP group was significantly increased.
Conclusion:
Genistein postconditioning has a protective effect on hypoxia/reoxygenation-induced injury in human gastric epithelial cells. The mechanism by which genistein exerts this protection may be via activation of cellular vanilloid receptor subtype 1, resulting in the generation of an endogenous protection substance, CGRP.
Keywords: genistein, pharmacological postconditioning, apoptosis, VR1
Introduction
A number of severe stressors could contribute to gastric ischemia to some degree, leading to gastric mucosal reperfusion injury (GMRI). Clinically, however, few satisfactory treatment methods exist. In 2003, Zhao et al1 first introduced the conception of ischemic postconditioning (IPostC), in which a series of brief mechanical interruptions of reperfusion is applied at the onset of reperfusion following a specific prescribed algorithm; this postconditioning then affords protection in vivo. Pharmacological postconditioning2 involves a modification of the IPostC concept in which a drug is applied to ischemic myocardium or hypoxic cardiomyocytes during the first few minutes of reperfusion or reoxygenation, reducing myocardial death significantly. At present, only a few reports include a discussion of gastric ischemic postconditioning.
Soy isoflavones are naturally occurring plant estrogens derived from soybeans, and genistein is the most important bioactive ingredient of these isoflavones. It can resist oxidation, tumors, and thrombosis and also degrade blood lipids3, 4. Tissier et al5 recently demonstrated that genistein postconditioning could reduce myocardium ischemia/reperfusion (I/R) injury by inhibiting apoptosis in rabbits. Our previous laboratory studies have shown that genistein postconditioning clearly protects rats from gastric I/R injuries.
The aims of the present study were to investigate the protective effect of genistein postconditioning on hypoxia/reoxygenation-induced injury in human gastric epithelial cells and to begin a tentative discussion on the mechanism behind this protection.
Materials and methods
Reagents and cell cultures
Genistein and capsazepine, acquired from the Sigma Company (USA), were dissolved in 100% DMSO and stored at -20 °C. DMEM (Dulbecco's modified Eagle's medium) was purchased from Gibco Corporation (USA). Fetal bovine serum (FBS) was purchased from Tianjin Hao Yang Biological Manufacture Co, Ltd (China). The human gastric epithelial cell line (GES-1) was purchased from Beijing Cancer Hospital. The cells were plated at a density of 1×105 cells/mL in 100-mL culture flasks containing 5 mL DMEM supplemented with 10% FBS and placed in a humidified incubator with 95% air and 5% CO2 at 37 °C.
Experimental protocol
The complete medium was replaced with DMEM containing 1% FBS one day before the experiment to synchronize the cells. The cells were randomly divided into five groups and treated as follows. Cells in the normal control group (N) were kept in normoxic culture for 6 h. In the hypoxia/reoxygenation group (H/R), the DMEM was replaced with Krebs-Ringer bicarbonate buffer prior to hypoxia induction. Cells were transferred into a hypoxic incubator in a humidified atmosphere equilibrated with 94%N2+1%O2+5%CO2 for 2 h (hypoxia). After this phase, the Krebs-Ringer bicarbonate buffer was replaced with DMEM to simulate reperfusion, followed by 4 h in normoxic culture (for reoxygenation). In the genistein postconditioning group (GP), the Krebs-Ringer bicarbonate buffer was replaced with DMEM containing 10, 25, 50, and 100 μmol/L genistein before reoxygenation; other procedures were unchanged from the H/R group. In the capsazepine+genistein postconditioning group (C+GP), the DMEM was replaced with Krebs-Ringer bicarbonate buffer containing 10 μmol/L capsazepine prior to the 2 h hypoxic period. After this phase, the buffer was replaced with DMEM containing 100 μmol/L genistein before reoxygenation; other procedures were unchanged from the H/R group. In the DMSO vehicle postconditioning group (DM), the Krebs-Ringer bicarbonate buffer was replaced with DMEM containing 0.05% DMSO before reoxygenation. Other procedures were unchanged from the H/R group.
MTT assay
Exponentially growing cells were cultured in a 96-well plate at a density of 2000 cells per well. Following each group's experiment, cells in the wells were treated with 10 μL MTT (5 g/L, Amresco, USA) and incubated for 4 h. Afterward, 100 μL DMSO was added to each well for 10 min. A 96-well microplate reader (Thermo, USA) was employed to determine the absorbance, A490 nm. All experiments were performed in triplicate. Viability (%) was determined as (the experimental group A490 nm/the normal control group A490 nm)×100%. There was a positive correlation between absorbance, A, and cell viability. The viability of the cells increased with an increase in the value of absorbance, A.
Flow cytometric analysis
Cells were plated in 100-mL culture flasks and incubated for 48 h. Following each experiment, the cells were digested by 0.2% trypsin (Amresco, USA) and adjusted to a density of 1×106/mL by 0.01 mol/L PBS. Cells were fixed with 95% alcohol at 4 °C for 12 h and then stained by 500 μL pyridine iodide (PI, Sigma) at 4 °C in the dark for 30 min. The apoptosis percentage was analyzed by flow cytometry (Becton Dickinson, USA).
Western blot analysis
Cells were plated in 100-mL culture flasks and incubated for 48 h. Following each experiment, the cells were rinsed with 0.01 mol/L PBS three times; then, 200 μL lysate containing 150 mL/L protease inhibitor was added, followed by a 15 min ice bath. Next, the cells were scraped from the flask, harvested and centrifuged for supernatant collection (total protein). The protein content was determined by Coomassie brilliant blue assay. SDS-PAGE (sodium dodecyl sulfate-polyacrylamide) gel sample buffer was added to the lysates. The lysates were heated to 100 °C for 3 min, and 100 μg protein was loaded into each well of a 12.5% SDS-PAGE gel. Proteins were transferred onto nitrocellulose membrane after electrophoresis. Immunoblotting was performed using the following antibodies: rabbit anti-CGRP (Beijing Biosynthesis Biotechnology Co, Ltd, China), mouse anti-Bcl-2 (Zhongshan Goldenbridge Biotechnology Co, Ltd, China), mouse anti-Bax (ibid), and mouse anti-β-actin (ibid). The secondary antibodies used were alkaline phosphatase goat anti-rabbit IgG (Sigma, USA) and alkaline phosphatase horse anti-mouse IgG (Zhongshan Goldenbridge Biotechnology Co, Ltd, China). Protein expression was quantified by Image J software.
Immunocytochemistry assay
Exponentially growing cells were cultured in a 24-well plate at a density of 1×105 cells per well. Two-step IHC detection reagent (ibid) and a DAB kit were used to examine the expression of CGRP in human gastric epithelial cells. Following each experiment, cells were rinsed three times with 0.01 mol/L PBS and fixed for 30 min with 4% paraformaldehyde at 4 °C. Afterward, cells were incubated with 0.3% Triton X-100 for 20 min and 3% H2O2 for 10 min. Later, cells were blocked with 10% normal goat serum for 1 h at room temperature. The primary antibody (rabbit anti-CGRP) was added and the mixture was incubated at 4 °C overnight. After cells were rinsed with cold PBS three times, the secondary antibody (alkaline phosphatase goat anti-rabbit IgG) was added and the mixture was incubated at room temperature for 3 h. Finally, cells were rinsed with 0.01 mol/L PBS three times and then incubated with DAB complexes for 20 min. Cells were observed and their photos were taken under a phase contrast microscope.
Statistical analysis
All data are expressed as means±SD and were analyzed by one-way ANOVA and t-test. A value of P<0.05 was considered statistically significant.
Results
Cell viability
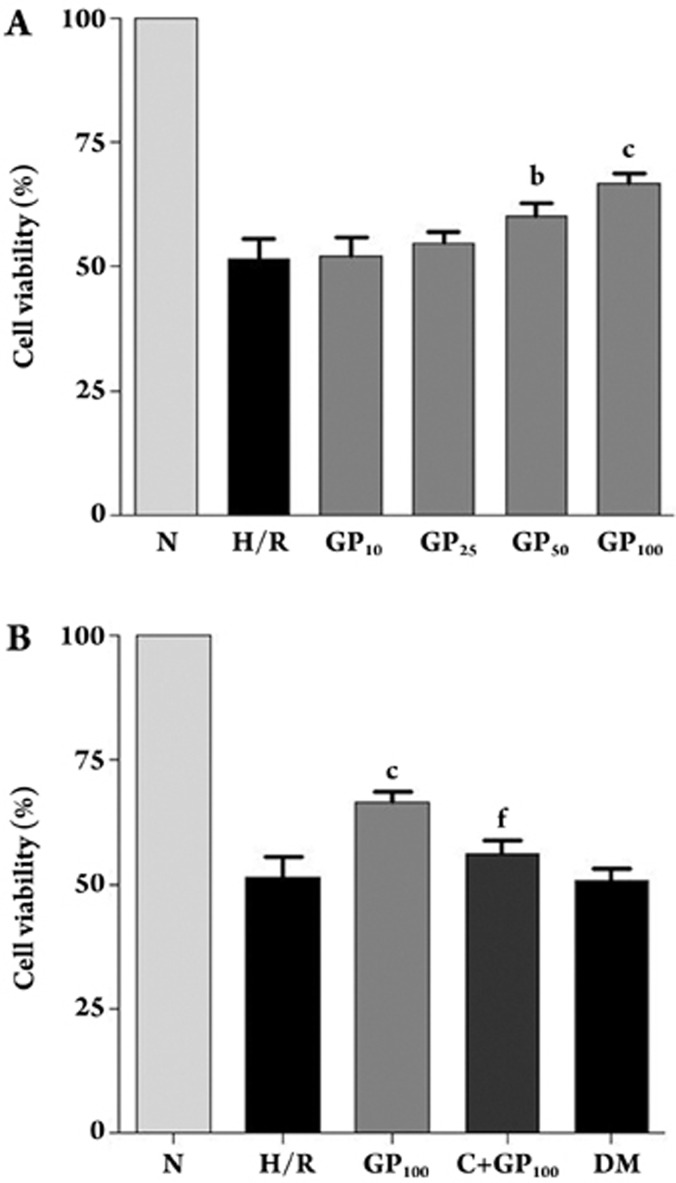
The MTT assay indicated that the cell viability in the GP group (10, 25, 50, and 100 μmol/L) was 52.2%±3.6%, 54.6%±2.5%, 60.0%±2.6%, and 66.7%±2.0%, respectively. The assay also indicated that the cell viability of each group was 100.0%±0%, 51.4%±4.1%, 66.7%±2.0%, 56.1% ±2.8%, and 50.7%±2.4% in a normal control group, H/R group, a GP 100 μmol/L postconditioning group, a capsazepine+genistein postconditioning group (C+GP) and a DMSO vehicle postconditioning group, respectively. Compared with the normal control group, the viability of the H/R group was decreased. Compared with the H/R group, viability of the GP group (50 and 100 μmol/L) was significantly increased (P<0.05). It indicated that capsazepine could reverse the protective effect of genistein postconditioning. In comparison with the GP group (100 μmol/L), the viability of the C+GP group was significantly decreased (P<0.01, Figure 1).
Figure 1.
Effects of genistein postconditioning on cell viability in human gastric epithelial cells. (A) Cells were treated as follows: normoxic culture for 6 h, 2 h hypoxia/4 h reoxygenation and four different concentrations of genistein postconditioning (10, 25, 50, and 100 μmol/L). Cell viability was detected by MTT assay. (B) Cells were treated as follows: normoxic culture for 6 h, 2 h hypoxia/4 h reoxygenation, genistein postconditioning (100 μmol/L), capsazepine+genistein postconditioning (100 μmol/L) and DMSO vehicle postconditioning. Cell viability was detected by MTT assay. Means±SD. bP<0.05, cP<0.01 vs H/R; fP<0.01 vs GP100.
Apoptosis
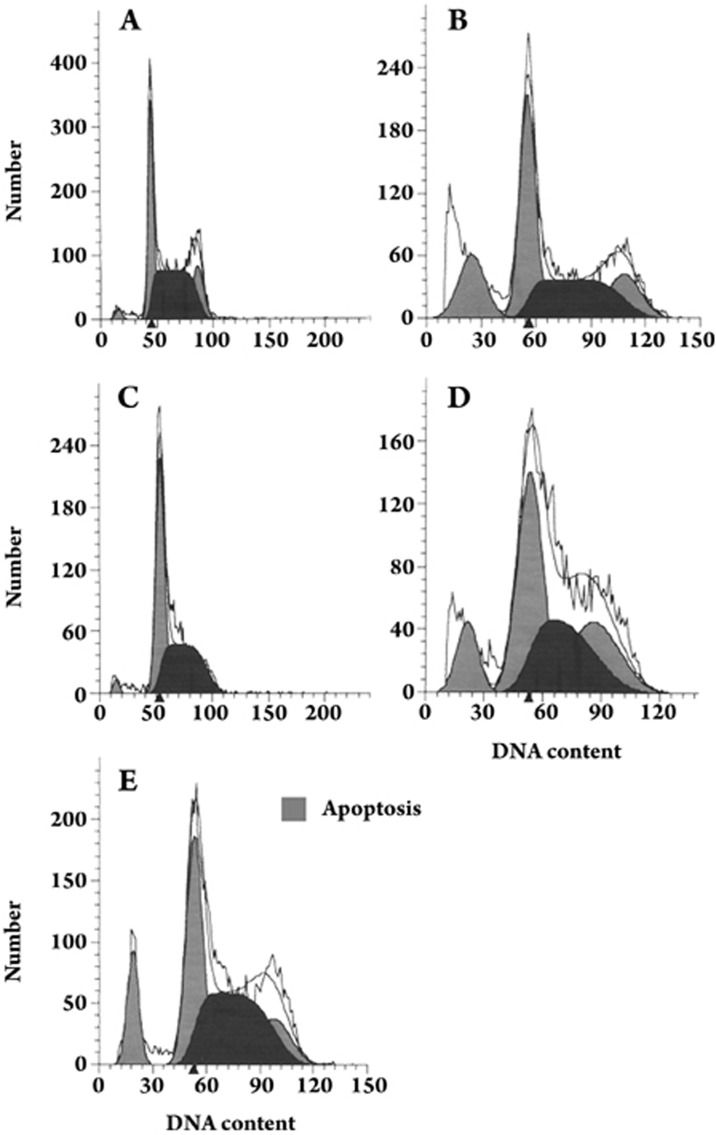
Flow cytometric analysis showed that the apoptosis percentages for the different groups were 2.28%±0.44%, 12.17%±2.15%, 5.40%±1.22%, 10.43%±1.37%, and 11.02%±2.19%, in a normal control group, H/R group, a GP 100 μmol/L postconditioning group, a capsazepine+genistein postconditioning group (C+GP) and a DMSO vehicle postconditioning group, respectively. Compared with the normal control group, the apoptosis percentage of the H/R group was increased, with a visible hypodiploid peak (apoptotic peak). Compared with the H/R group, the apoptosis percentage of the GP group (100 μmol/L) was significantly decreased (P<0.01), and that of the C+GP group was increased (P<0.01) (Figure 2).
Figure 2.
Effect of genistein postconditioning on apoptosis in human gastric epithelial cells. Cells were treated as follows: normoxic culture for 6 h (A), 2 h hypoxia/4 h reoxygenation (B), genistein postconditioning (100 μmol/L) (C), capsazepine+genistein postconditioning (100 μmol/L) (D), and DMSO vehicle postconditioning (E). Subsequently, cells were fixed with 95% alcohol at 4 °C for 12 h and then stained with 500 μL pyridine iodide (PI) at 4 °C in the dark for 30 min. Percentages of cell apoptosis were detected by flow cytometry.
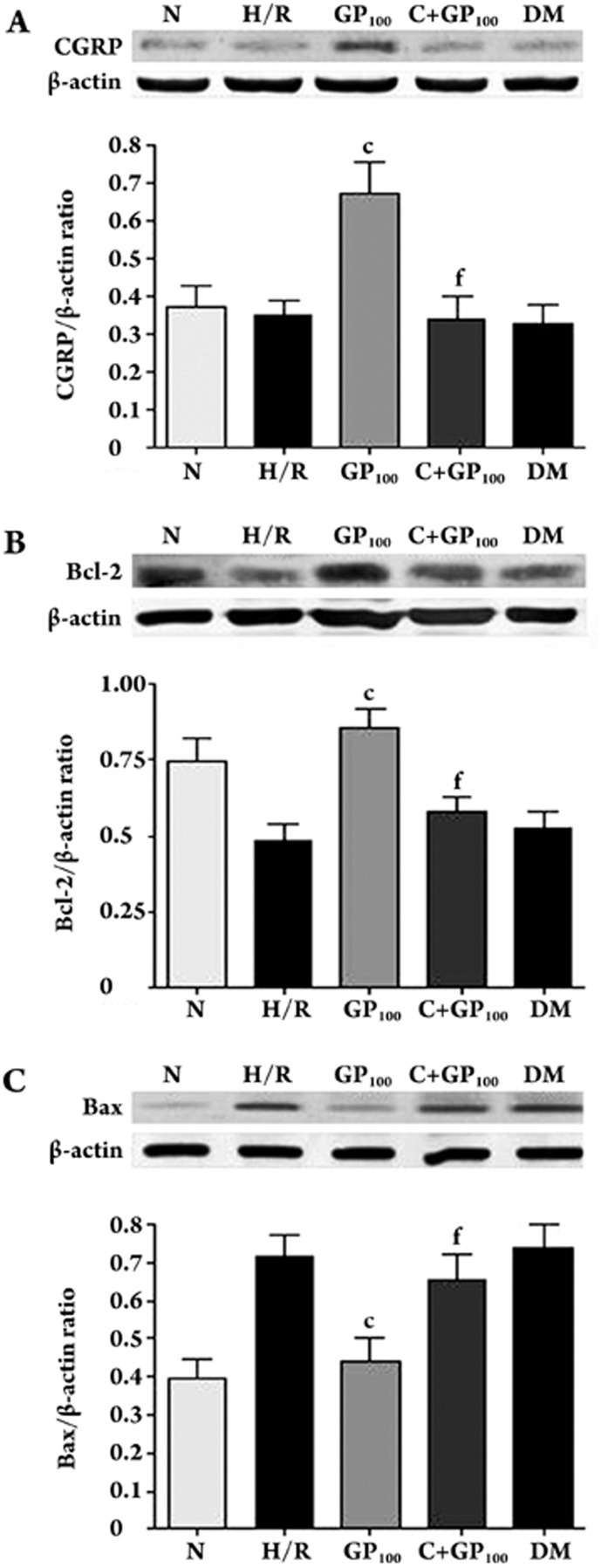
Expression of CGRP, Bcl-2 and Bax
Western blot analysis demonstrated that calcitonin gene-related peptide (CGRP) was expressed in normal gastric epithelial cells. There was no significant difference among the normal control, H/R and DM groups. Compared with the H/R group, the expression of CGRP was increased in the GP group (100 μmol/L) (P<0.01) and decreased in the C+GP group (P<0.01). Bcl-2 and Bax were also expressed in normal human gastric epithelial cells. Compared with the H/R group, the expression of Bcl-2 was increased in the GP group (100 μmol/L), while whereas the expression of Bax was decreased (P<0.01). On the other hand, in comparison with the GP group, the expression of Bcl-2 was decreased in the C+GP group, while whereas the expression of Bax was increased (P<0.01) (Figure 3).
Figure 3.
Effect of genistein postconditioning on the expression of CGRP, Bcl-2, and Bax in human gastric epithelial cells. Cells were treated as follows: normoxic culture for 6 h, 2 h hypoxia/ 4 h reoxygenation, genistein postconditioning (100 μmol/L), capsazepine+genistein postconditioning (100 μmol/L) and DMSO vehicle postconditioning. Afterward, cells were harvested and lysed, and the total protein was obtained as described in the text. The protein was isolated by 12.5% SDS-PAGE and then transferred to a nitrocellulose membrane. The expression of CGRP, Bcl-2, and Bax was analyzed by Western blot with rabbit anti-CGRP, mouse anti-Bcl-2, mouse anti-Bax, and mouse anti-β-actin antibodies. Protein expression was quantified by Image J software. (A) CGRP expression; (B) Bcl-2 expression; (C) Bax expression. cP<0.01 vs H/R, fP<0.01 vs GP100.
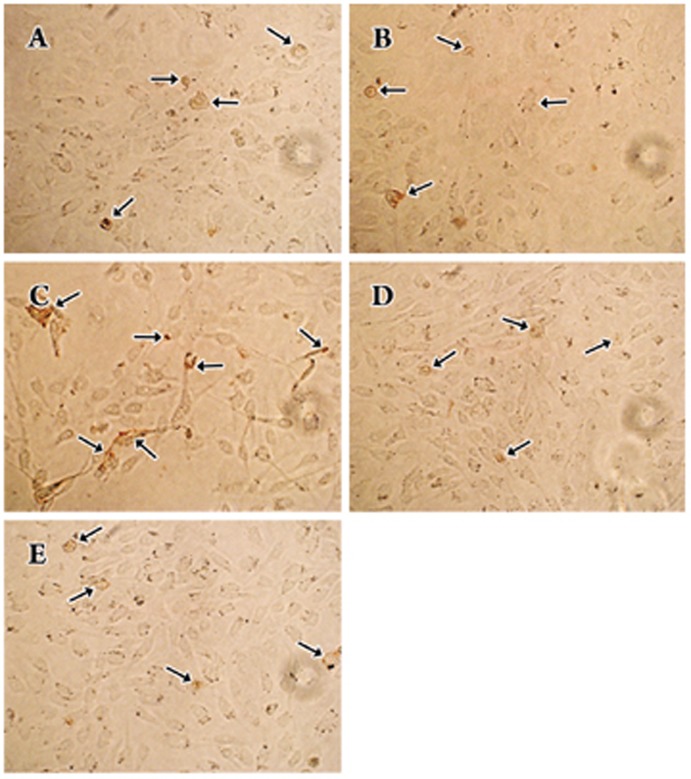
CGRP-positive cells
The immunocytochemistry assay confirmed the expression of CGRP in normal human gastric epithelial cells (Figure 4A). There were no significant differences among the normal control, H/R (Figure 4B) and DM groups (Figure 4E). The number of CGRP-positive cells in the GP group (100 μmol/L) was significantly increased (Figure 4C), whereas it was decreased in the C+GP group (Figure 4D).
Figure 4.
Effect of genistein postconditioning on the expression of CGRP in human gastric epithelial cells. Cells were treated as follows: normoxic culture for 6 h (A), 2 h hypoxia/4 h reoxygenation (B), genistein postconditioning (100 μmol/L) (C), capsazepine+genistein postconditioning (100 μmol/L) (D), and DMSO vehicle postconditioning (E). The two-step IHC detection reagent and the DAB kit were used to examine the expression of CGRP in human gastric epithelial cells. Cells were observed and their photos were taken under a phase contrast microscope (×400).
Discussion
Gastric ischemia/reperfusion injury is a complicated issue, related to such factors as excessive generation of oxygen free radicals (OFR) in gastric mucosa, intracellular calcium overload, increased gastric acid secretion and gastric microcirculation disturbance6. Excessive generation of OFRs and intracellular calcium overload may lead to apoptosis7. Bcl-2 and Bax belong to the Bcl-2 family and are considered the key factors in apoptosis8. Ji et al9 reported that genistein preconditioning reduced I/R injury in rabbit myocardium by decreasing Fas and Bax expression and by increasing the Bcl-2/Bax ratio. In our study, MTT assays, flow cytometric analysis and Western blot were used to test cell viability, apoptosis percentages and apoptosis-related protein expression. Our results indicate that cell viability is significantly decreased and apoptosis percentage is increased in the model of 2 h hypoxia/4 h reoxygenation. They also show that, in the same model, the expression of anti-apoptotic protein (Bcl-2) was decreased and the expression of pro-apoptotic protein (Bax) was increased. Our experiment has demonstrated that postconditioning with 50 and 100 μmol/L of genistein can reduce H/R-induced injury in human gastric epithelial cells.
Vanilloid receptor subtype 1 (VR1), a non-selective cation channel, is widely distributed in capsaicin-sensitive primary sensory neurons of the dorsal root ganglion, trigeminal ganglion and vagus ganglion and the sensory nerve terminals responsive to mechanical, thermal and chemical stimuli10, 11. Therefore, VR1 is regarded as a new target for drug therapy12. Activation of VR1 induces Ca2+ influx into sensory nerve terminals, resulting in the exocytosis of neuropeptides, such as calcitonin gene-related peptide (CGRP)13. Previous research has shown that CGRP has a protective effect on ischemic/reperfused myocardial and endothelial cells14, 15. It has been suggested that rutaecarpine may protect the myocardium from ischemia/reperfusion injury by activating the vanilloid receptor and generating an endogenous protection substance, CGRP16.
Conventionally, VR1 is recognized as a nervous system-specific receptor. Recent research, however, has indicated that VR1 is also distributed in some non-nervous tissues, such as liver, lungs, gastric epithelial cells17, bronchi18, bladder epithelium19, mast cells, skin cells20, and macrophages21. This finding suggests that VR1 might be involved in regulating a variety of physiological functions of different tissues and organs. We thus speculated that the protective effect of genistein postconditioning on I/R (or H/R-induced) injury to the stomach was modulated via the direct activation of VR1 in gastric epithelial cells, leading to the generation of an endogenous protection substance, CGRP.
In the present study, the results of Western blot analysis and immunocytochemistry assays have shown that normal human gastric epithelial cells express a certain amount of CGRP and that genistein postconditioning significantly increases this expression. Capsazepine is a specific and competitive antagonist of the vanilloid receptor. Liu et al22 confirmed that 10 μmol/L of capsazepine blocked the vanilloid receptor of trigeminal ganglion neurons. Our experiment showed that capsazepine at this dose could reverse the protective effect of genistein postconditioning, suggesting that this protective effect might be attributed to the activation of VR1.
Genistein is a safe, naturally occurring drug. However, genistein does exhibit toxic side effects on retinal function when used at the optimal therapeutic concentrations without any protective agents23. The need to consider the potential for genistein neurotoxicity has been previously reported24. The dose of genistein is critical in the induction of tissue-dependent biological actions. Finally, it is important to emphasize that we observed no significant side effects in our study.
In conclusion, we have identified a novel therapeutic strategy for gastric ischemia/reperfusion injury. We have confirmed that genistein-induced pharmacological postconditioning exerts its effect in vitro through direct activation of the vanilloid receptor subtype 1, resulting in the generation of an endogenous protection substance (CGRP) and a decrease in apoptosis in human gastric epithelial cells.
Author contribution
Jian-fu ZHANG designed research; Yu LI performed research; Yong-mei ZHANG contributed new analytical tools and reagents; Yu LI and Xiao-bo MA analyzed data; Yu LI wrote the paper.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No 30570671).
References
- Zhao ZQ, Corvera JS, Halkos ME, Kerendi F, Wang NP, Guyton RA, et al. Inhibition of myocardial injury by ischemic postconditioning during reperfusion: comparison with ischemic preconditioning. Am J Physiol Heart Circ Physiol. 2003;285:H579–88. doi: 10.1152/ajpheart.01064.2002. [DOI] [PubMed] [Google Scholar]
- Hausenloy DJ, Yellon DM. New directions for protecting the heart against ischemia-reperfusion injury: targeting the reperfusion injury salvage kinase (RISK)-pathway. Cardiovasc Res. 2004;61:448–60. doi: 10.1016/j.cardiores.2003.09.024. [DOI] [PubMed] [Google Scholar]
- Rishi RK. Phytoestrogens in health and illness. Indian J Pharmacol. 2002;34:311–20. [Google Scholar]
- Jiang F, Jones GT, Husband AJ, Dusting GJ. Cardiovascular protective effects of synthetic isoflavone derivatives in apolipoprotein E-deficient mice. J Vasc Res. 2003;40:276–84. doi: 10.1159/000071891. [DOI] [PubMed] [Google Scholar]
- Tissier R, Waintraub X, Couvreur N, Gervais M, Bruneval P, Mandet C, et al. Pharmacological postconditioning with the phytoestrogen genistein. J Mol Cell Cardiol. 2007;42:79–87. doi: 10.1016/j.yjmcc.2006.10.007. [DOI] [PubMed] [Google Scholar]
- Nakamoto K, Wada K, Kitano M, Kishimoto Y, Ashida K, Kamisaki Y, et al. The role of endogenous acid in the development of acute gastric ulcer induced by ischemia-reperfusion in the rat. Life Sci. 1998;62:PL63–9. doi: 10.1016/s0024-3205(97)01119-3. [DOI] [PubMed] [Google Scholar]
- Thompson CB. Apoptosis in the pathogenesis and treatment of disease. Science. 1995;267:1456–62. doi: 10.1126/science.7878464. [DOI] [PubMed] [Google Scholar]
- Carambula SF, Matikainen T, Lynch MP, Flavell RA, Goncalves PB, Tilly JL, et al. Caspase-3 is a pivotal mediator of apoptosis during regression of the ovarian corpus luteum. Endocrinology. 2002;143:1495–501. doi: 10.1210/endo.143.4.8726. [DOI] [PubMed] [Google Scholar]
- Ji ES, Yue H, Wu YM, He RR. Effects of phytoestrogen genistein on myocardial ischemia/reperfusion injury and apoptosis in rabbits. Acta Pharmacol Sin. 2004;25:306–12. [PubMed] [Google Scholar]
- Sasamura T, Kuraishi Y. Peripheral and central actions of capsaicin and VR1 receptor. Jpn J Pharmacol. 1999;80:275–80. doi: 10.1254/jjp.80.275. [DOI] [PubMed] [Google Scholar]
- Holzer P. Capsaicin: cellular targets, mechanisms of action, and selectivity for thin sensory neurons. Pharmacol Rev. 1991;43:143–201. [PubMed] [Google Scholar]
- Sterner O, Szallasi A. Novel natural vanilloid receptor agonists: new therapeutic targets for drug development. Trends Pharmacol Sci. 1999;20:459–65. doi: 10.1016/s0165-6147(99)01393-0. [DOI] [PubMed] [Google Scholar]
- Wardle KA, Ranson J, Sanger GJ. Pharmacological characterization of the vanilloid receptor in the rat dorsal spinal cord. Br J Pharmacol. 1997;121:1012–6. doi: 10.1038/sj.bjp.0701199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren YS, Ma TG, Wang HB, Yu SQ. Protective effects of calcitonin gene-related peptide (CGRP) on myocardial cell injury and calcium and magnesium contents following severe hypoxia and simulated reperfusion. Med Sci Res. 1993;21:177–8. [Google Scholar]
- Li YJ, Peng CF, Li NS, You JM, Deng HW. Calcitonin gene-related peptide protects against endothelial cell damage due to oxidized low-density lipoprotein. Med Sci Res. 1995;23:253–4. [Google Scholar]
- Hu CP, Li NS, Xiao L, Deng HW, Li YJ. Involvement of capsaicin-sensitive nerves in cardioprotection of rutaecarpine in rats. Regul Pept. 2003;114:45–9. doi: 10.1016/s0167-0115(03)00087-9. [DOI] [PubMed] [Google Scholar]
- Kechagias S, Botella S, Petersson F, Borch K, Ericson AC. Expression of vanilloid receptor-1 in epithelial cells of human antral gastric mucosa. Scand J Gastroenterol. 2005;40:775–82. doi: 10.1080/00365520510015782. [DOI] [PubMed] [Google Scholar]
- Reilly CA, Taylor JL, Lanza DL, Carr BA, Crouch DJ, Yost GS. Capsaicinoids cause inflammation and epithelial cell death through activation of vanilloid receptors. Toxicol Sci. 2003;73:170–81. doi: 10.1093/toxsci/kfg044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birder LA, Kanai AJ, de Groat WC, Kiss S, Nealen ML, Burke NE, et al. Vanilloid receptor expression suggests a sensory role for urinary bladder epithelial cells. Proc Natl Acad Sci USA. 2001;98:13396–401. doi: 10.1073/pnas.231243698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southall MD, Li T, Gharibova LS, Pei Y, Nicol GD, Travers JB. Activation of epidermal vanilloid receptor-1 induces release of proinflammatory mediators in human keratinocytes. J Pharmacol Exp Ther. 2003;304:217–22. doi: 10.1124/jpet.102.040675. [DOI] [PubMed] [Google Scholar]
- Chen CW, Lee ST, Wu WT, Fu WM, Ho FM, Lin WW. Signal transduction for inhibition of inducible nitric oxide synthase and cyclooxygenase-2 induction by capsaicin and related analogs in macrophages. Br J Pharmacol. 2003;140:1077–87. doi: 10.1038/sj.bjp.0705533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L, Oortgiesen M, Li L, Simon SA. Capsaicin inhibits activation of voltage-gated sodium currents in capsaicin-sensitive trigeminal ganglion neurons. J Neurophysiol. 2001;85:745–58. doi: 10.1152/jn.2001.85.2.745. [DOI] [PubMed] [Google Scholar]
- Lüke C, Krott R, Lüke M, Lebek J, Walter P, Brunner R, et al. Effects of protein tyrosine kinase inhibitor genistein on retinal function in superfused vertebrate retina. J Ocul Pharmacol Ther. 2001;17:151–8. doi: 10.1089/10807680151125474. [DOI] [PubMed] [Google Scholar]
- Linford NJ, Yang Y, Cook DG, Dorsa DM. Neuronal apoptosis resulting from high doses of the isoflavone genistein: role for calcium and p42/44 mitogen-activated protein kinase. J Pharmacol Exp Ther. 2001;299:67–75. [PubMed] [Google Scholar]