Abstract
Pulmonary arterial hypertension (PAH) is characterized by a persistent elevation of pulmonary arterial pressure and pulmonary arterial remodeling with unknown etiology. Current therapeutics available for PAH are primarily directed at reducing the pulmonary blood pressure through their effects on the endothelium. It is well accepted that pulmonary arterial remodeling is primarily due to excessive pulmonary arterial smooth muscle cell (PASMC) proliferation that leads to narrowing or occlusion of the pulmonary vessels. Future effective therapeutics will be successful in reversing the vascular remodeling in the pulmonary arteries and arterioles. The purpose of this review is to provide updated information on molecular mechanisms involved in pulmonary arterial remodeling with a focus on growth factors, transcription factors, and epigenetic pathways in PASMC proliferation. In addition, this review will highlight novel therapeutic strategies for potentially reversing PASMC proliferation.
INTRODUCTION
Pulmonary arterial hypertension (PAH) is characterized by a persistent elevation of pulmonary artery pressure accompanied by right ventricular hypertrophy (RVH). Left untreated, PAH can result in right heart failure and death. Our current understanding of the pathogenesis of PAH has expanded significantly in recent years which have resulted in an increase of available treatments and an improved prognosis, but, unfortunately, there is no cure. The exact molecular mechanism of PAH has yet to be resolved. Median survival rates have improved with the recent introduction of endothelin receptor antagonists (ERAs) and phosphodiesterase (PDE)-5 inhibitors, but a recent estimate of survival of 3.6 years is still discouraging (1). To manage PAH successfully, the reversal or inhibition of pulmonary vascular remodeling must be achieved. This review will highlight the molecular mechanisms involved in pulmonary arterial remodeling and recent advancements in potential therapeutics.
ENDOTHELIAL DYSFUNCTION AND PAH
Endothelial dysfunction is a term applied when the balance between vasoconstrictors and vasodilators in the endothelium is disturbed and is well established in PAH (2). In PAH patients, the endogenous production of pulmonary vasodilators is low, including endothelial nitric oxide synthase (eNOS), the enzyme responsible for producing the vasodilator nitric oxide (3). The levels of prostanoids, another class of vasodilators, are decreased in PAH patients and the administration of prostaglandin I2 (prostacyclin) can improve symptoms and decrease pulmonary arterial pressure in PAH patients (4). Today, prostacyclin analogues remain a vital source of treatment for PAH patients through their ability to decrease pulmonary arterial blood pressure and inhibit vascular smooth muscle cell (SMC) proliferation. Further studies demonstrated an increase in vasoconstrictors including endothelin-1 (ET-1), thromboxane and serotonin (5–6). ET-1 in particular is a potent vasoconstrictor that can constrict blood vessels and contribute to vascular remodeling. Serotonin, or 5-hydroxytryptamine (5-HT) also can increase vasoconstriction and trigger abnormal endothelial-SMC cross-talk. Mouse models of PAH with enhanced 5-HT expression and transport have established a link between 5-HT and PAH (7–8). Certain drugs that alter 5-HT levels, including anorexigenics, are associated with an increased risk of developing PAH (9).
Chronic low grade inflammation is another factor that can contribute to endothelial dysfunction in cardiovascular disease. Conditions such as shear stress or vascular injury can induce upregulation of cell adhesion molecules (Vascular cell adhesion molecule-1 [VCAM-1], Intracellular adhesion molecule-1 [ICAM-1]) that can attract inflammatory mediators (monocytes/macrophages, lymphocytes) to endothelial cells which can contribute to remodeling of the vascular wall (10). Various chemokines (fraktalkine, chemokine ligand 2 [CCL2; also called monocyte chemotactic protein-1 {MCP-1}] and regulated on activation, normal T-cell expressed and secreted [RANTES; also called chemokine ligand 5 {CCL5}]) and receptors (CX3CR1) also are known to be upregulated in the endothelium of PAH patients (11–12). In fact, the monocrotaline (MCT) rodent model is used widely to study PAH because it triggers severe vascular inflammation, remodeling, and increases pulmonary blood pressure (13).
Today, therapies to improve the endothelial dysfunction in PAH patients are available which include the endothelin receptor antagonists, phosphodiesterase-5 inhibitors and prostacyclin analogues. Recent investigations between endothelial cells and SMCs revealed that endothelial dysfunction contributes to vascular remodeling through the proliferative effects of some vasoconstrictors (14–15). In addition, the loss of vasodilators can promote cell proliferation (14). When abnormal proliferation of vascular SMCs occurs, the end result is hyperplasia of the arterial medial layer and occlusion of the lumen. In PAH, significant occlusion of the distal pulmonary arteries increases both pulmonary arterial pressure and vascular resistance, eventually leading to right heart failure and death. Thus, the focus of PAH research has evolved in recent years to incorporate the knowledge that the endothelial and smooth muscle cells both have an effect on the mechanisms that regulate the extensive vascular remodeling observed in patients. Therefore, reversing the vascular remodeling along with improving endothelial function would provide a significant clinical improvement for patients.
MOLECULAR MECHANISMS OF PULMONARY ARTERIAL SMOOTH MUSCLE CELL (PASMC) PROLIFERATION
The categories of PAH differ in their underlying causes, but one feature common to almost all forms is the excessive proliferation of vascular cells in the distal pulmonary arteries (16). All vessel layers (intima, media and adventitia) are affected which results in severe loss of cross-sectional lumen area and increases the right ventricular afterload (15). Perhaps the most prominent feature of PAH is the extensive proliferation of the SMCs in the medial layer. The changes in vascular structure suggest a switch from a quiescent state to a proliferative and antiapoptotic state in the progression of PAH. Unfortunately the cellular mechanisms underlying the remodeling process are incompletely understood. This section will provide an overview of several key molecular pathways regulating PASMC proliferation (Figure 1).
Figure 1.
Summary of molecular mechanisms involved in pulmonary remodeling. In pulmonary artery smooth muscle cells, inhibition of the potassium channels leads to cell depolarization and calcium entry, stimulating excess calcium release from the sarcoplasmic reticulum leading to calcium-calmodulin–regulated cell proliferation. When growth factors (PDGF, VEGF, TGF-β) and mitogens (ET-1) bind to their receptors, various signaling pathways are activated which increase cytosolic calcium levels and activate the MAPK signaling pathway–stimulating transcription factors (c-fos, c-jun, c-myc, and so on) and increase cell proliferation. Prostacyclin’s antagonistic effects act by increasing cAMP concentration, which simultaneously inhibits MAPK signaling and activates the PKA/MLCK growth-suppressive pathway. The vasodilator nitric oxide diffuses into the cell and stimulates cGMP production via guanylyl cyclase that results in MLCK dephosphorylation that inhibits cell growth and relaxes the SMC, leading to vasodilation. Finally, depolarization of the mitochondrial membrane by the mitoKATP channels (see mitoKATP above) delays apoptosis by inhibiting cytochrome c release and generates hydrogen peroxide (H2O2), stimulating transcription factors that drive cell proliferation. Cyto-C, cytochrome c; CaM: calcium-calmodulin complex; S.R, sarcoplasmic reticulum; RyR, ryanodine receptor; PKA, protein kinase A; AC, adenylyl cyclase; GC, guanylyl cyclase; N.O., nitric oxide. Lightning bolt indicates hyperpolarization.
ET-1
The ET system may be involved in the pathogenesis of PAH. Blockade of ETA and ETB receptors are effective treatments for PAH. ET-1 is a potent mitogen and exerts its effects in PASMCs through binding to either the ETA or ETB receptor, depending on the location of the cell. For example, when ET-1 binds to ETA, a rapid increase in intracellular calcium levels and sustained protein kinase C activation result (16). Early induction of the mitogen-activated protein kinase (MAPK) pathway and activation of the c-fos and c-jun genes also are reported as a result of ET-1 stimulation (see Figure 1) (17). ET-1 therefore contributes to the abnormal proliferation of PASMCs in PAH. When ET-1 binds its receptor, vasoconstriction and cell proliferation results in response to activation of phospholipase-C β and the second messengers diacylglycerol and Ins(1,4,5)P3 by activating calcium channels (18). ET-1 binding also stimulates MAPK family signaling events by first activating the small guanosine triphosphates (GTPases) Ras and Raf, leading to phosphorylation of downstream MAP kinases followed by phosphorylation of extracellular signal-regulated kinase (ERK) 1/2 (see Figure 1). Phosphorylation of ERK 1/2 results in p38MAPK and c-Jun terminal kinase activation that promotes growth signaling and controls cell survival and differentiation (18).
Prostacyclin
Prostacyclin, along with prostaglandins and thromboxanes, form a subclass of the eicosanoids called the prostanoids. Prostacyclin is a potent pulmonary vasodilator and platelet inhibitor that exerts its effects through the cyclic adenosine monophosphate (cAMP)-dependent pathways. Acting as a paracrine agent, prostacyclin is released by endothelial cells and binds G-protein–coupled receptors on nearby smooth muscle cells causing adenylyl cyclase to generate cAMP (see Figure 1). Elevated cAMP levels activate protein kinase A which results in inhibition of myosin light chain kinase (MLCK) leading to SMC relaxation. In addition to its vasodilatory properties, prostacyclin also inhibits SMC proliferation by activation of cell surface prostanoid receptors, leading to activation of G-protein–coupled receptors and increasing cAMP production (see Figure 1) (19). The antiproliferative effects of cAMP have been demonstrated in many different cell types (20–22). Prostacyclin has been studied extensively in PAH and remains a cornerstone for therapeutic management in patients with severe PAH. Several FDA approved drugs taking advantage of prostacyclin biology are available for use in PAH patients today. On the other hand, a clinical study showed that chronic treatment with epoprostenol (a prostacyclin analog) increased the survival in a patient with idiopathic PAH, but it did not prevent progression of the underlying PASMC proliferation (23). Remarkably, the RV was able to sustain a normal cardiac output in the face of advanced PA pathology with the mechanism to be explored (23). However, this observation is based on a case report. A clinical trial with a large cohort is needed before a conclusion can be made regarding the therapeutic potential of prostacyclin.
Transforming Growth Factor β (TGF-β) Family
One of the most important discoveries in PH research includes the identification of germ line mutations occurring in the gene coding for bone morphogenetic proteins (BMPs) of the TGF-β superfamily. Roughly 60% of familial PH cases and 10% to 30% of idiopathic PH patients are estimated to have the mutation (24–25). Other genes in the BMP/TGF-β signaling pathway are expected to be involved in the pathogenesis of PAH and evidence supporting this include the additional discoveries of mutations on TGF-β receptors and endoglins identified in PH patients with a family history of hereditary hemorrhagic telangiectasia (26–27).
The BMP receptor (BMP-R) is a constitutively active serine/theronine kinase receptor and is activated by binding of several specific ligands including BMP2, BMP4, BMP7 and others. Activation of the BMP-R initiates phosphorylation of signaling via the Smad1, Smad5 and Smad8 proteins that eventually allow translocation of a signaling complex into the nucleus and gene transcription regulation to occur (16). Human PASMCs and PA endothelial cells both express several TGF-β family receptors on their surface. Increasing evidence also suggests that MAPKs including ERK, p38 and Janus kinases are activated by TGF-β and BMP receptors (see Figure 1) (28). Research into BMP-R expression in human PAH patients revealed that BMP-RII and BMP-RIA are both downregulated (29–30). TGF-β1 also was shown to induce ET-1 production in human PASMCs through the protein kinase A pathway (31). Taken together, the TGF-β family plays a vital role in the control of vascular tone and growth but, due to the large family and complex downstream interactions, much has yet to be learned.
Nitric Oxide (NO)
NO is an important molecule that plays a vital role in vascular function. NO is produced in the endothelium but, when released, it diffuses into SMCs where it acts as a vasodilator by stimulating production of the second messenger cyclic guanosine monophosphate (cGMP) from guanylyl cyclase, leading to dilation of blood vessels by dephosphorylation of myosin light chain (see Figure 1) (32). NO also has the ability to inhibit SMC proliferation through the ERK pathway (33). The ERK pathway can be pro-or antiproliferative depending upon the activation status of the small GTPase RhoA; where inactivation of RhoA inhibits proliferation of smooth muscle cells. NO has been shown to decrease Rho activation and inhibit proliferation of SMCs (33). NO is an important mediator in PAH because the lack of NO availability in patients contributes to decreases in pulmonary vasodilation and promotes SMC proliferation.
Calcium Channels
In addition to promoting cell contraction by binding to calmodulin and stimulating MLCK, calcium is a critical second messenger that can regulate proliferation and gene expression within the smooth muscle cell (34). Calcium exerts its proproliferative effects by binding the calmodulin complex which then stimulates production of c-fos and c-jun causing quiescent cells to enter cell cycle which drives proliferating cells through mitosis (see Figure 1) (34–35). In addition, the magnitude, duration, amplitude and frequency of mitogen-induced calcium increase can influence what set of genes are activated (34). For example, PDGF stimulates signal transducer and activator of transcription 3 (STAT3) phosphorylation, leading to the upregulation of c-jun which activates transcription of the transient receptor protein-canonical (TRPC) genes (36). TRPC genes encode for large cation channels responsible for many voltage independent calcium pathways in vascular cells (34). TRPC1,3,4 and 6 have all shown to be expressed in PASMCs and are suggested to mediate proliferation. Preliminary results suggest TRPC6 is highly expressed in lung tissue and proliferating PASMCs of PH patients and was shown to increase agonist-induced calcium entry through the STAT3/c-jun pathway (37). Most importantly, inhibition of TRPC6 with antisense was demonstrated to inhibit agonist-induced PASMC proliferation and to improve vascular tone (36,38). Understanding the abnormal calcium signaling in PH therefore remains an attractive therapeutic approach and is an area of active investigation.
Potassium Channels
Hypoxic pulmonary vasoconstriction results in the closing of voltage-gated potassium (Kv) channels and the resulting membrane depolarization triggers opening of voltage-gated calcium channels. In PASMCs from PH patients, Kv1.5 was downregulated compared with cells from normal patients (39). Also, microarray studies of lungs from PAH patients have shown suppression of Kv channel genes (40). In rats with chronic hypoxia-induced PAH, Kv1.5 and Kv2.1 are both downregulated. The loss of Kv channels in PASMCs leads to depolarization of the cell and a subsequent influx of cytosolic calcium that ultimately initiates vasoconstriction and proliferation of the SMCs (16).
Recent evidence suggests that Kv1.5 and Kv2.1 are not the only Kv channels involved in regulating the membrane potential in PASMCs. Further investigation into potassium channels showed that the PASMC resting potential depends on background K+ currents comprising voltage-dependent and -independent components (41). Members of the KCNQ (Kv7) potassium channels, notably KCNQ4, were shown to regulate, in part, the intrinsic tone of pulmonary arteries and may provide alternative routes for treating PH (41). Reports indicate that KCNQ channels effect pulmonary artery tone by preventing voltage-gated Ca2+ channels from opening, so it is reasonable to suggest that they are also directly affecting PASMC growth and proliferation via Ca2+ release as well.
Potassium channels located on mitochondria can affect PASMC growth and proliferation. By use of the hypoxia model, mitochondrial ATP-sensitive potassium (mitoKATP) channels were demonstrated to depolarize the mitochondrial membrane potential, leading to inhibition of cytochrome c release and an increase in hydrogen peroxide levels. Increased hydrogen peroxide can promote proliferative and antiapoptotic responses in the cell. The mitoKATP channel blocker, 5-hydroxydeconoate (5-HD), partly reduced the hypoxia-induced responses through increasing cytochrome c release causing an increase in apoptosis. Hydrogen peroxide stimulates cell proliferation by increasing expression of early response genes belonging to the AP-1 family including c-myc, c-jun and egr-1 (42). Hydrogen peroxide levels were reduced by 5-HD administration and prevented the proliferation response. The exact mechanism of how mitoKATP channels affect the production of hydrogen peroxide is unclear at this time.
Apoptosis
One method for potentially reversing the proliferation of PASMCs would be through manipulating apoptosis. The idea that apoptotic-resistant endothelial or smooth muscle cells may be contributing to or initiating the progression of PH has been suggested (43). Dichloroacetate, a metabolic modulator, was shown to increase expression of voltage-gated potassium channels that depolarize PASMC mitochondria, causing release of cy-tochrome c, thereby enhancing apoptosis (44). Apoptosis signal-regulating kinase-(Ask-1) is a member of the MAPK-kinase family that, when activated, stimulates JNK and p38, inducing apoptosis and has been demonstrated to play a central role in proliferation of SMCs due to injury (45). These are some examples of how apoptosis pathways could be targeted to reverse the in vivo PASMC proliferation and pulmonary remodeling that occurs in PH patients.
Epigenetics
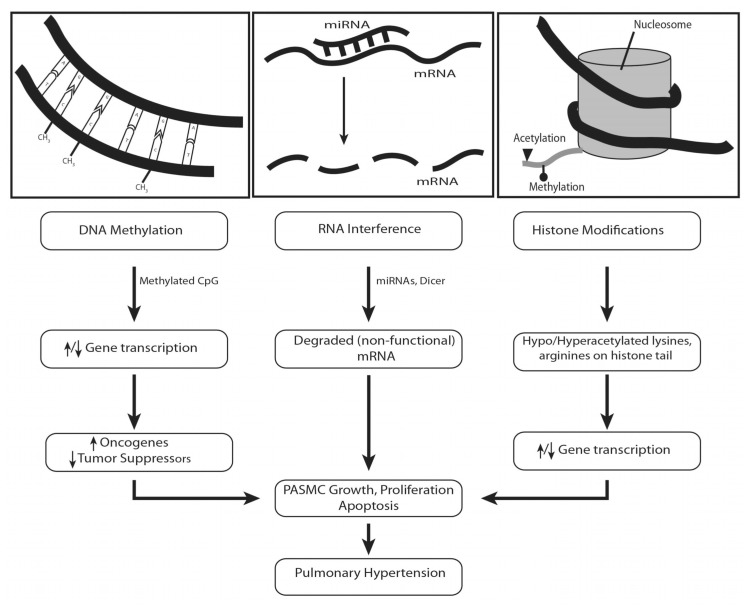
Heritable changes in phenotype or in gene expression states that are not involved in the DNA sequence itself describe epigenetic modifications. Examples of epigenetic modifications include histone modifications, DNA methylation, and RNA interference (Figure 2). DNA methylation and histone modification are the major epigenetic events that selectively activate or inactivate cell growth, proliferation and apoptosis-controlling genes. Epigenetic mechanisms can either be acquired or inherited, and provide a means for gene and environment interactions to take place. There is substantial evidence that supports a role for epigenetic involvement in the mechanism of several diseases including cancer, asthma and heritable disorders (46–47).
Figure 2.
Epigenetics and pulmonary hypertension. Methylation of CpG islands in the promoter region of genes can lead to either hypo- or hyperacetylated promoters. This, in turn, can lead to increased or decreased gene transcription. While the pathways are not clearly defined, it is expected that an increase in oncogenes and/or a decrease in tumor suppressor genes can promote the abnormal cell proliferation of PASMCs. RNA interference is a well-described mechanism where miRNAs target specific mRNA and lead to degradation, preventing translation into mature protein. Lastly, histone modifications (either acetylated or methylated lysines and arginines) can promote or prevent transcription factor-mediated gene transcription and lead to increased cell proliferation or apoptosis resistance. These epigenetic mechanisms provide an alternative route for PH development besides mutations associated with the DNA sequence itself. ↑, Increase or upregulation; ↓ decrease or downregulation.
Recent evidence suggests that epigenetic factors may play a role in PAH. Archer et al. described a tissue-specific, epigenetic deficiency in superoxide dismutase (SOD) that initiates and sustains a heritable form of PAH by impairing redox signaling in PASMCs (48). The impaired redox signaling created a proliferative and apoptosis-resistant condition in cells. Specifically, they observed a decrease in Kv1.5 channels and a rise in cytosolic calcium that increased cell proliferation while SOD augmentation reversed the proliferation of the PASMCs (48). Xu et al. reported that changes in the chromatin structure of the eNOS gene increased its expression in a model of newborn pulmonary hypertension (49). They suggest that these changes allowed for the binding of transcription factors that increased gene transcription of eNOS and contributed to endothelial dysfunction. These results provide further evidence that epigenetics may contribute to the disease pathogenesis of PAH. The early investigations into epigenetics and PH are exciting because they could provide a link to risk factors for developing the disease and may even contribute to overall disease development. The works by Archer et al. and Xu et al. clearly provide evidence for a direct link between epigenetic modifications in PAH that alter the vascular biology which may contribute to endothelial dysfunction, SMC proliferation and apoptosis resistance, three mechanisms that are critically involved in pulmonary vascular remodeling.
Recently, conserved and noncoding RNAs such as microRNAs (miRNAs, miRs) have been identified as essential mediators of a variety of genes and cellular processes (50–51). Interestingly, miRs regulate cell survival, differentiation and proliferation, suggesting that miRs may be involved in pulmonary arterial remodeling. The miR-21 expression is increased in remodeled pulmonary vessels of animal models of PAH and human PAH (51–52); miR-21 regulates hypoxia-associated PASMC proliferation and PA remodeling (53–54). Parikh et al. (52) found that hypoxia and BMP receptor type 2 signaling independently upregulate miR-21 in cultured PA endothelial cells. Targeted deletion of miR-21 increases Rho-kinase activity and exacerbated PAH and PA remodeling (51). The nuclear factor of activated T cells (NFAT) signaling pathway is linked to PASMC proliferation and PAH (55). Kang et al. found that miR-124 inhibited NFAT receptor activity and decreased both the dephosphorylation and the nuclear translocation of NFAT (55). Hypoxia downregulated miR-124 in human PASMCs; consistent with the activation of NFAT during this process. Overexpression of miR-124 not only inhibited human PASMC proliferation, but also maintained its differentiated phenotype by repressing the NFAT pathway (55). It was reported that miR-206 regulates PASMC proliferation and differentiation (56) and that miR-210 has antiapoptotic effects in PASMCs during hypoxia (57). Courboulin et al. reported that miR-204 plays a role in human PAH and PA remodeling (58). This group also demonstrated that the role of miR-204 and NFAT in PAH may be mediated by the DNA damage/PARP-1 signaling pathway (59). Drake et al. reported that heritable pulmonary arterial hypertension (HPAP)-associated mutation engender a primary defect in noncanonical miR processing, where bone morphogenetic protein (BMP) signaling is partially maintained (60). Smad-8 is responsible for this miR pathway. Induction of miR-21 and miR-27a is a critical component of BMP-induced growth suppression, loss of which likely contributes to PASMC proliferation in HPAP (60). Kim et al. reported that an endothelial apelin-FGF link mediated by miR-424 and miR-503 is disrupted in PAH (61), suggesting that these miRs may be involved in PA remodeling. It should be emphasized that the role of miRs in PASMC proliferation and PA remodeling is still largely unknown although recent data is emerging quickly (62). It will be interesting to investigate if modulation of miRs could serve as a new therapeutic strategy for reversing pulmonary vascular remodeling (63–64).
GROWTH FACTORS AND PASMC PROLIFERATION
Growth factors regulate a wide variety of physiological processes including cell migration, differentiation, proliferation and survival (65). There are a variety of growth factors including epidermal growth factor, fibroblast growth factor, vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF) and others. Growth factors bind to specific receptors with receptor tyro-sine kinase activity and, among them, the PDGF receptors are the most intensively studied systems.
PDGF
Identified more than 30 years ago, PDGF biology has evolved into a major player in therapeutic research encompassing many fields including embryonic development, angiogenesis, cancer biology and cardiovascular disease. The PDGF family consists of four ligands (PDGF A-D) that combine to form five homo- and heterodimeric isoforms. The dimers exert their effects on two receptors (platelet-derived growth factor receptors [PDGFR]-α or -β) with varying affinities for the five ligands (65). Upon ligand binding, autophosphorylation of the PDGFR occurs and creates docking sites for signal transduction molecules containing SH2 domains including but not limited to phosphatidylinositol 3 kinase, phospholipase C γ, Src family kinases, SHP-2 phosphatases, GTPase and a variety of other molecules lacking enzymatic activity (which are able to bind through adaptor proteins) (65). After receptor activation, downstream signaling pathways are initiated, including the MAPK pathway (ERKs, JNKs, p38) and early response genes (c-fos, JunB, c-myc) that mediate cellular processes including apoptosis, cell cycle progression and cell migration (66–67).
Early studies investigating the role of PDGF in PAH pathogenesis generated the idea that cell proliferation in PAH patients was similar to various forms of cancer (65). More recently, evidence supports the hypothesis that molecular mechanisms involved in tumor cell proliferation play a vital role in chronic vascular changes observed in PH (68). Early reports identified increased PDGF receptor expression in the lungs of PAH patients (69). PDGF also was found to be an extremely potent mitogen and chemoattractant for PASMCs (70). In PAH animal models, PDGF ligand and receptor expression was elevated in PASMCs (71–72).
With the strong evidence supporting a role for PDGF in the pathogenesis of PAH, investigations then focused on the potential for treating PAH patients by inhibition of PDGF. Initially developed for the treatment of chronic myelogenous leukemia by inhibiting the kinase activity of the proto-oncogene ABL, imatinib (or Gleevec) also was shown to inhibit receptor tyrosine kinase activity. Shermuly et al. first demonstrated that imatinib was able to reverse pulmonary hypertension in two different PH animal models (68). Pulmonary arterial hypertension, right ventricular hypertrophy and cardiac output were all improved and animal survival increased with the administration of imatinib. Ghofrani et al. then reported preliminary results indicating that imatinib reversed SMC proliferation and neointima formation in a human PAH patient (73). Drawing on these and other data suggesting the potential application for PDGF therapy in PH patients, a multinational, randomized, placebo-controlled clinical trial was initiated where imatinib was administered concomitantly with ongoing conventional PH treatments in patients (74). The IMPRES study (imatinib in pulmonary arterial hypertension, a randomized, efficacy study) showed that imatinib improved exercise capacity and hemodynamics in patients with advanced PAH who remained symptomatic on at least two drugs of the currently available three drug classes (74–75). However, discontinuations of study medication and serious side effects, including surgical hematomas, were more common in the imatinib group, and further studies are required to assess the risk-benefit profile of imatinib in patients with advanced PAH (74). It should be emphasized that the results of the IMPRES study were very disappointing and ended up with increased morbidity in the treatment group on imatinib. Therefore, imatinib was not approved for clinical use in PAH. The off-label use of imatinib for this indication is strongly discouraged until further data are available. Clearly, new and specific PDGF receptor antagonists with no or minimum side effects should be developed and tested.
VEGF
The VEGF family is actually a subfamily of the PDGF family of cystine-knot growth factors. Currently, there are five families in the mammalian VEGFs including VEGF A-D and placental growth factor (76). VEGF plays a central role in embryogenic vasculogenesis and angiogenesis and is essential for wound healing and endometrium regeneration in adults (76). Unfortunately, VEGF’s role in the pathogenesis of PAH remains under debate. Evidence of increased VEGF expression was reported in plexiform lesions of PAH patients including one of its receptors, VEGF receptor 2 (77). By using the hypoxia model to induce PAH, VEGF has consistently been shown to increase and is likely to modulate hypoxia-induced vascular remodeling (78). In the MCT model, however, VEGF levels appear to be decreased (78). In fact, it was reported that VEGF attenuated PAH through viral- and cell-based transfer studies in the MCT and hypoxia-induced PAH models, possibly by protecting endothelial cells from injury and apoptosis (79–80).
While the role for VEGF in endothelial cells remains to be elucidated, emerging evidence suggests that VEGF may play a significant role in PAH through its effects on PASMCs. Using an in vivo blood flow model, one group demonstrated that VEGF levels in PASMCs were elevated and regulated through a TGF-β/NADPH oxidase pathway that may contribute significantly to vascular remodeling in pulmonary vasculature through increased reactive oxygen species production (81,82). In addition, Steiner et al. used an IL-6 overexpression model to show that IL-6 administration increased VEGF levels in PASMCs that led to significant remodeling of the vasculature (52). The IL-6/VEGF-induced remodeling was accompanied by the observation of increased ERK activation, increased c-myc production and an increase in antiapoptotic proteins survivin and Bcl-2 in PASMCs which created a state of pro-proliferation and antiapoptosis.
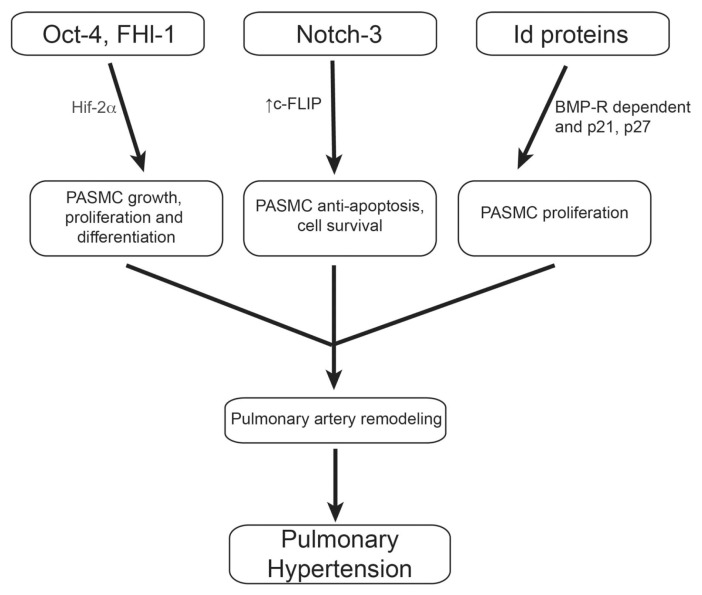
TRANSCRIPTION FACTORS AND PASMC PROLIFERATION
Transcription factors are sequence specific elements that bind to DNA promoter regions, usually in a complex with other proteins, that regulate the transcription of DNA into messenger RNA. Transcription factors including hypoxia inducible factor 1α (Hif-1α), suppressor of cytokine signaling 3 (SOCS3) and nuclear factor kappa B (NF-κB) are known regulators of PASMC proliferation, but research so far has not yielded effective therapeutics (83). Thus, there remains a need for the discovery of novel transcription factors involved in PASMC proliferation and migration. Several novel transcription factors that may play a role in PASMC proliferation will be discussed (Figure 3).
Figure 3.
Novel transcription factors and pulmonary hypertension. Oct-4, normally associated with embryonic stem cell differentiation, has been suggested to play a role in hypoxia-mediated proliferation of PASMCs through the ability of Hif-2α to bind the Oct-4 promoter and trigger cell growth. Similar to Oct-4, Fhl-1 also was demonstrated to promote PASMC growth and proliferation through activation of the Hif-1/2 factors in response to hypoxia. Increased levels of Notch-3 were shown to induce c-FLIP, an antiapoptotic mediator, in PASMCs, and results in increased apoptosis resistance. Notch-3 also may interact with upstream regulators of the MAPK signaling pathway (including Src and Ras) to promote cell proliferation. Lastly, the Id protein family may act cooperatively to regulate BMP-R-dependent PASMC proliferation via their effects on the cyclin-dependent kinases and have been shown to be affected by prostacyclin therapy, a vital treatment resource for PH patients.
Octamer-binding transcription factor 4 (Oct-4)
A novel transcription factor, Oct-4 is also referenced as POU51, OCT-3/4 and OTF3/4 in the literature. Originally shown to be a critical mediator in maintaining human embryonic stem cells in an undifferentiated state, Oct-4 is suggested to play important roles in the induction of stem cells, tumor growth and, most recently, in the proliferation of PASMCs (83). Oct-4 expression was suggested to be limited only to germ cells, but evidence supports the presence of Oct-4 in other cell populations including multipotent adult progenitor cells and mesenchymal stem cells (84). A study conducted by Firth et al. showed that Oct-4 isoforms were upregulated in PASMCs from human PAH patients compared with control cell lines (83). They also demonstrated increased expression of Hif-2α, a transcription factor known to bind and regulate the Oct-4 promoter in PASMCs from PAH patients. Finally, they showed that hypoxia-exposed PASMCs had increased levels of both Oct-4 and Hif-2α compared with nonhypoxic cells. While molecular investigations of Oct-4 regulation are lacking, early evidence suggests that c-myc and Kruppel-like factor-4 may be involved, two genes associated with cell proliferation and anti-apoptosis (52,85). The increased Oct-4 expression in hypoxic cells and PASMCs from PAH patients suggests a functional role for Oct-4 in the development and progression of vascular remodeling in PAH patients (83). This evidence identifies a potential new therapeutic target for vascular remodeling in PAH patients.
Four and a Half LIM Domains Protein 1 (Fhl-1)
Fhl-1 is a protein that belongs to the family of proteins containing LIM domains that are cysteine-rich double zinc finger motifs and mediate protein-protein interactions of transcription factors (86). Recently, it was shown that in hypoxia-induced PAH, Fhl-1 expression was increased (87). Interestingly, Fhl-1 expression was increased as early as 1 d after hypoxia exposure and remained elevated for the duration of the 21 d experiment (87). Expression was limited to the pulmonary vasculature with the strongest localization of Fhl-1 in the SMCs of pulmonary arteries and arterioles, key sites of vascular remodeling. Using the siRNA approach, Fhl-1 knockdown decreased PASMC migration and proliferation while Fhl-1 overexpression had the opposite effect (87). Lastly, Fhl-1 expression is elevated in the MCT rat model as well. Similar to Oct-4, Fhl-1 expression is known to be regulated by hypoxia-nducible factors (Hif-1α and Hif-2α) and, importantly, Hif is known to be involved in hypoxia- and nonhypoxia- induced forms of PAH (88–89). These early investigations theorize that Fhl-1 might be an early response element involved in PASMC proliferation.
Notch-3
The Notch receptors are single trans-membrane spanning proteins that, after ligand binding, lead to the release of intracellular domains that translocate to the nucleus and form active transcriptional complexes with various proteins that can regulate cell fate and differentiation (90). Notch-3 is strongly suggested to regulate arterial SMC identity, proliferation and apoptosis. Since PAH is a disease characterized by SMC proliferation, the study of Notch-3 has garnered attention (91–92). Notch-3 has been demonstrated to induce c-FLIP expression, an antiapoptotic mediator (93). While the mechanism remains unclear, it is suggested to exert antiapoptotic effects through cross-talk with the MAPK pathway (93). Evidence supporting this hypothesis includes the ability of Notch-3 to interact with Src and Ras but again the mechanisms are still under investigation and remain unclear at this time (94).
In human PAH patients, Notch-3 mRNA and protein is overexpressed (90). Li et al. demonstrated that human PAH vasculopathy is characterized by high levels of Notch-3 and its downstream effectors in PA arterioles (90). Disease severity also correlated with Notch-3 levels in humans and rodents and showed PASMC proliferation induced by constitutive Notch-3 intracellular domain expression. Finally, Notch3−/− mice demonstrated a resistance to the development of PAH. Their results suggest the possibility that Notch signaling may mediate pulmonary vessel remodeling by affecting proliferation and homeostasis of PASMCs.
Inhibitors of DNA Binding
DNA-binding protein inhibitors (Id) are another group of transcription factors identified to regulate PASMC proliferation and differentiation. BMP receptor mutations lead to decreased Id expression in human PAH patients and Id1−/− mice present with PAH identical to hypoxia-induced PAH. In opposition to these findings, Id3 was elevated in response to hypoxia. The different Id3 expression suggests that this family of transcription factors may act cooperatively in regulating BMP-dependent SMC proliferation due to chronic hypoxia (95). While the molecular signaling events are still unclear, the cyclin-dependent kinase inhibitor proteins, p21 and p27, appear to be the targets for Id proteins (96). Both p21 and p27 have been shown to be inhibited by Ids, resulting in cell cycle progression and proliferation in various cell types (96). Interestingly, in vitro and in vivo results have demonstrated that prostacyclins are effective in enhancing Id1 expression through a cAMP–protein kinase A–dependent mechanism (97). These insights may provide new strategies for managing PASMC proliferation in PAH patients.
CONCLUSION
Understanding the molecular mechanisms that regulate vascular proliferation remains a key challenge to developing effective therapeutics for managing PAH. Our insight into the vascular biology in PAH has evolved rapidly in the last decade to incorporate the idea that successful strategies for managing PAH will include both restoring pulmonary endothelial function and preventing or reversing remodeling of the arteries due to smooth muscle cell proliferation. Resolving how endothelial dysfunction and the increased production of vasoconstrictors, including ET-1 and thromboxane, activate signaling mechanisms that promote proliferation in SMCs will greatly improve current treatment strategies for patients. However, PAH patients are widely considered to vary greatly in response to treatment and it is more likely that future treatments will focus on individualized therapeutic strategies for patients that hopefully will prove more successful than broad application-based treatments. Furthermore, while high rates of BMP receptor mutations have been observed in PAH patients, only 20% of BMP receptor carriers will actually develop the disease and that, along with the observation that individual patients vary greatly in response to identical treatment regimens, underscores the importance for an epigenetic factor in disease development and progression (46). Only lately have we begun to understand the potential for processes that can alter gene expression outside of changes in the DNA sequence itself and how this applies to disease mechanisms. DNA methylation and histone modifications are the predominant epigenetic factors that can activate or inactivate genes which regulate cell growth and proliferation, and these have yet to fully be explored in the field of PAH. Future experiments to understand epigenetic factors and their contribution, if any, to proliferation of SMCs in PAH are needed.
ACKNOWLEDGMENTS
Funding was received from NIH R01 HL116863, HL102074 and HL105302 and AHA 11PRE7830040.
Footnotes
Online address: http://www.molmed.org
DISCLOSURE
The authors declare that they have no competing interests as defined by Molecular Medicine, or other interests that might be perceived to influence the results and discussion reported in this paper.
REFERENCES
- 1.Anderson JR, Nawarskas JJ. Pharmacotherapeutic management of pulmonary arterial hypertension. Cardiol Rev. 2010;18:148–62. doi: 10.1097/CRD.0b013e3181d4e921. [DOI] [PubMed] [Google Scholar]
- 2.Morrell NW, et al. Cellular and molecular basis of pulmonary arterial hypertension. J Am Coll Cardiol. 2009;54:S20–31. doi: 10.1016/j.jacc.2009.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giaid A, Saleh D. Reduced expression of endothelial nitric oxide synthase in the lungs of patients with pulmonary hypertension. N Engl J Med. 1995;333:214–21. doi: 10.1056/NEJM199507273330403. [DOI] [PubMed] [Google Scholar]
- 4.Szczeklik J, et al. Effects of prostaglandin E1 on pulmonary circulation in patients with pulmonary hypertension. Br Heart J. 1978;40:1397–401. doi: 10.1136/hrt.40.12.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christman BW, et al. An imbalance between the excretion of thromboxane and prostacyclin metabolites in pulmonary hypertension. N Engl J Med. 1992;327:70–5. doi: 10.1056/NEJM199207093270202. [DOI] [PubMed] [Google Scholar]
- 6.Stewart DJ, Levy RD, Cernacek P, Langleben D. Increased plasma endothelin-1 in pulmonary hypertension: marker or mediator of disease? Ann Intern Med. 1991;114:464–9. doi: 10.7326/0003-4819-114-6-464. [DOI] [PubMed] [Google Scholar]
- 7.Launay JM, et al. Function of the serotonin 5-hydroxytryptamine 2B receptor in pulmonary hypertension. Nat Med. 2002;8:1129–35. doi: 10.1038/nm764. [DOI] [PubMed] [Google Scholar]
- 8.Eddahibi S, et al. Cross talk between endothelial and smooth muscle cells in pulmonary hypertension: critical role for serotonin-induced smooth muscle hyperplasia. Circulation. 2006;113:1857–64. doi: 10.1161/CIRCULATIONAHA.105.591321. [DOI] [PubMed] [Google Scholar]
- 9.Uchida S, et al. An integrated approach for the systematic identification and characterization of heart-enriched genes with unknown functions. BMC Genomics. 2009;10:100. doi: 10.1186/1471-2164-10-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Savoia C, et al. Vascular inflammation and endothelial dysfunction in experimental hypertension. Int J Hypertens. 2011;2011;281240 doi: 10.4061/2011/281240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crosswhite P, Sun Z. Nitric oxide, oxidative stress and inflammation in pulmonary arterial hypertension. J Hypertens. 2010;28:201–12. doi: 10.1097/HJH.0b013e328332bcdb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Balabanian K, et al. CX(3)C chemokine fractalkine in pulmonary arterial hypertension. Am J Respir Crit Care Med. 2002;165:1419–25. doi: 10.1164/rccm.2106007. [DOI] [PubMed] [Google Scholar]
- 13.Gomez-Arroyo JG, et al. The monocrotaline model of pulmonary hypertension in perspective. Am J Physiol Lung Cell Mol Physiol. 2011;302:L363–9. doi: 10.1152/ajplung.00212.2011. [DOI] [PubMed] [Google Scholar]
- 14.Ghamra ZW, Dweik RA. Primary pulmonary hypertension: an overview of epidemiology and pathogenesis. Cleve Clin. J. Med. 2003;70(Suppl 1):S2–8. doi: 10.3949/ccjm.70.suppl_1.s2. [DOI] [PubMed] [Google Scholar]
- 15.Schermuly RT, Ghofrani HA, Wilkins MR, Grimminger F. Mechanisms of disease: pulmonary arterial hypertension. Nat Rev Cardiol. 2011;8:443–55. doi: 10.1038/nrcardio.2011.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Humbert M, et al. Cellular and molecular pathobiology of pulmonary arterial hypertension. J Am Coll Cardiol. 2004;43:13S–24S. doi: 10.1016/j.jacc.2004.02.029. [DOI] [PubMed] [Google Scholar]
- 17.Jeffery TK, Morrell NW. Molecular and cellular basis of pulmonary vascular remodeling in pulmonary hypertension. Prog Cardiovasc Dis. 2002;45:173–202. doi: 10.1053/pcad.2002.130041. [DOI] [PubMed] [Google Scholar]
- 18.Bouallegue A, Daou GB, Srivastava AK. Endothelin-1-induced signaling pathways in vascular smooth muscle cells. Curr Vasc Pharmacol. 2007;5:45–52. doi: 10.2174/157016107779317161. [DOI] [PubMed] [Google Scholar]
- 19.Clapp LH, et al. Differential effects of stable prostacyclin analogs on smooth muscle proliferation and cyclic AMP generation in human pulmonary artery. Am J Respir Cell Moll Biol. 2002;26:194–201. doi: 10.1165/ajrcmb.26.2.4695. [DOI] [PubMed] [Google Scholar]
- 20.Owen NE. Effect of prostaglandin E1 on DNA synthesis in vascular smooth muscle cells. Am J Physiol. 1986;250:C584–8. doi: 10.1152/ajpcell.1986.250.4.C584. [DOI] [PubMed] [Google Scholar]
- 21.Nilsson J, Olsson AG. Prostaglandin E1 inhibits DNA synthesis in arterial smooth muscle cells stimulated with platelet-derived growth factor. Atherosclerosis. 1984;53:77–82. doi: 10.1016/0021-9150(84)90107-2. [DOI] [PubMed] [Google Scholar]
- 22.Jourdan KB, Evans TW, Lamb NJ, Goldstraw P, Mitchell JA. Autocrine function of inducible nitric oxide synthase and cyclooxygenase-2 in proliferation of human and rat pulmonary artery smooth-muscle cells: species variation. Am J Respir Cell Mol Biol. 1999;21:105–10. doi: 10.1165/ajrcmb.21.1.3502. [DOI] [PubMed] [Google Scholar]
- 23.Rich S, et al. Long-term effects of epoprostenol on the pulmonary vasculature in idiopathic pulmonary arterial hypertension. Chest. 2010;138:1234–9. doi: 10.1378/chest.09-2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deng Z, et al. Familial primary pulmonary hypertension (gene PPH1) is caused by mutations in the bone morphogenetic protein receptor-II gene. Am J Hum Genet. 2000;67:737–44. doi: 10.1086/303059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lane KB, et al. Heterozygous germline mutations in BMPR2, encoding a TGF-beta receptor, cause familial primary pulmonary hypertension. Nat Genet. 2000;26:81–4. doi: 10.1038/79226. [DOI] [PubMed] [Google Scholar]
- 26.Trembath RC, et al. Clinical and molecular genetic features of pulmonary hypertension in patients with hereditary hemorrhagic telangiectasia. N Engl J Med. 2001;345:325–34. doi: 10.1056/NEJM200108023450503. [DOI] [PubMed] [Google Scholar]
- 27.Chaouat A, et al. Endoglin germline mutation in a patient with hereditary haemorrhagic telangiectasia and dexfenfluramine associated pulmonary arterial hypertension. Thorax. 2004;59:446–8. doi: 10.1136/thx.2003.11890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Massague J, Chen YG. Controlling TGF-beta signaling. Genes Dev. 2000;14:627–44. [PubMed] [Google Scholar]
- 29.Beppu H, et al. BMP type II receptor is required for gastrulation and early development of mouse embryos. Dev Biol. 2000;221:249–58. doi: 10.1006/dbio.2000.9670. [DOI] [PubMed] [Google Scholar]
- 30.Du L, et al. Signaling molecules in nonfamilial pulmonary hypertension. N Engl J Med. 2003;348:500–9. doi: 10.1056/NEJMoa021650. [DOI] [PubMed] [Google Scholar]
- 31.Markewitz BA, Farrukh IS, Chen Y, Li Y, Michael JR. Regulation of endothelin-1 synthesis in human pulmonary arterial smooth muscle cells. Effects of transforming growth factor-beta and hypoxia. Cardiovasc Res. 2001;49:200–6. doi: 10.1016/s0008-6363(00)00221-2. [DOI] [PubMed] [Google Scholar]
- 32.Barst RJ. A review of pulmonary arterial hypertension: role of ambrisentan. Vasc Health Risk Manag. 2007;3:11–22. [PMC free article] [PubMed] [Google Scholar]
- 33.Zuckerbraun BS, et al. Nitric oxide-induced inhibition of smooth muscle cell proliferation involves S-nitrosation and inactivation of RhoA. Am J Physiol Cell Physiol. 2007;292:C824–31. doi: 10.1152/ajpcell.00592.2005. [DOI] [PubMed] [Google Scholar]
- 34.Landsberg JW, Yuan JX. Calcium and TRP channels in pulmonary vascular smooth muscle cell proliferation. News Physiol Sci. 2004;19:44–50. doi: 10.1152/nips.01457.2003. [DOI] [PubMed] [Google Scholar]
- 35.Berridge MJ. Inositol trisphosphate and calcium signalling. Nature. 1993;361:315–25. doi: 10.1038/361315a0. [DOI] [PubMed] [Google Scholar]
- 36.Yang XR, Lin MJ, Sham JS. Physiological functions of transient receptor potential channels in pulmonary arterial smooth muscle cells. Adv Exp Med Biol. 2010;661:109–22. doi: 10.1007/978-1-60761-500-2_7. [DOI] [PubMed] [Google Scholar]
- 37.Inoue R, et al. The transient receptor potential protein homologue TRP6 is the essential component of vascular alpha(1)-adrenoceptor-activated Ca(2+)-permeable cation channel. Circ Res. 2001;88:325–32. doi: 10.1161/01.res.88.3.325. [DOI] [PubMed] [Google Scholar]
- 38.Slish DF, Welsh DG, Brayden JE. Diacyl-glycerol and protein kinase C activate cation channels involved in myogenic tone. Am J Physiol Heart Circ Physiol. 2002;283:H2196–201. doi: 10.1152/ajpheart.00605.2002. [DOI] [PubMed] [Google Scholar]
- 39.Yuan JX, et al. Dysfunctional voltage-gated K+ channels in pulmonary artery smooth muscle cells of patients with primary pulmonary hypertension. Circulation. 1998;98:1400–6. doi: 10.1161/01.cir.98.14.1400. [DOI] [PubMed] [Google Scholar]
- 40.Geraci MW, et al. Gene expression patterns in the lungs of patients with primary pulmonary hypertension: a gene microarray analysis. Circ Res. 2001;88:555–62. doi: 10.1161/01.res.88.6.555. [DOI] [PubMed] [Google Scholar]
- 41.Joshi S, Sedivy V, Hodyc D, Herget J, Gurney AM. KCNQ modulators reveal a key role for KCNQ potassium channels in regulating the tone of rat pulmonary artery smooth muscle. J Pharmacol Exp Ther. 2009;329:368–76. doi: 10.1124/jpet.108.147785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang RP, et al. Tumor promotion by hydrogen peroxide in rat liver epithelial cells. Carcinogenesis. 1999;20:485–92. doi: 10.1093/carcin/20.3.485. [DOI] [PubMed] [Google Scholar]
- 43.Zhang S, et al. Bone morphogenetic proteins induce apoptosis in human pulmonary vascular smooth muscle cells. Am J Physiol Lung Cell Mol Physiol. 2003;285:L740–54. doi: 10.1152/ajplung.00284.2002. [DOI] [PubMed] [Google Scholar]
- 44.McMurtry MS, et al. Dichloroacetate prevents and reverses pulmonary hypertension by inducing pulmonary artery smooth muscle cell apoptosis. Circ Res. 2004;95:830–40. doi: 10.1161/01.RES.0000145360.16770.9f. [DOI] [PubMed] [Google Scholar]
- 45.Liu H, Nishitoh H, Ichijo H, Kyriakis JM. Activation of apoptosis signal-regulating kinase 1 (ASK1) by tumor necrosis factor receptor-associated factor 2 requires prior dissociation of the ASK1 inhibitor thioredoxin. Mol Cell Biol. 2000;20:2198–208. doi: 10.1128/mcb.20.6.2198-2208.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim GH, Ryan JJ, Marsboom G, Archer SL. Epigenetic mechanisms of pulmonary hypertension. Pulm Circ. 2011;1:347–56. doi: 10.4103/2045-8932.87300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xu XF, Cheng F, Du LZ. Epigenetic regulation of pulmonary arterial hypertension. Hypertens Res. 2011;34:981–6. doi: 10.1038/hr.2011.79. [DOI] [PubMed] [Google Scholar]
- 48.Archer SL, et al. Epigenetic attenuation of mitochondrial superoxide dismutase 2 in pulmonary arterial hypertension: a basis for excessive cell proliferation and a new therapeutic target. Circulation. 2010;121:2661–71. doi: 10.1161/CIRCULATIONAHA.109.916098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Xu XF, et al. Epigenetic regulation of the endothelial nitric oxide synthase gene in persistent pulmonary hypertension of the newborn rat. J Hypertens. 2011;28:2227–35. doi: 10.1097/HJH.0b013e32833e08f1. [DOI] [PubMed] [Google Scholar]
- 50.White K, Loscalzo J, Chan SY. Holding our breath: The emerging and anticipated roles of microRNA in pulmonary hypertension. Pulm Circ. 2012;2:278–90. doi: 10.4103/2045-8932.101395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Parikh VN, et al. MicroRNA-21 integrates pathogenic signaling to control pulmonary hypertension: results of a network bioinformatics approach. Circulation. 2012;125:1520–32. doi: 10.1161/CIRCULATIONAHA.111.060269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Steiner MK, et al. Interleukin-6 overexpression induces pulmonary hypertension. Circ Res. 2009;104:236–44. doi: 10.1161/CIRCRESAHA.108.182014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yang S, et al. miR-21 regulates chronic hypoxia-induced pulmonary vascular remodeling. Am J Physiol Lung Cell Mol Physiol. 2012;302:L521–9. doi: 10.1152/ajplung.00316.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sarkar J, et al. MicroRNA-21 plays a role in hypoxia-mediated pulmonary artery smooth muscle cell proliferation and migration. Am J Physiol Lung Cell Mol Physiol. 2010;299:L861–71. doi: 10.1152/ajplung.00201.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kang K, et al. MicroRNA-124 suppresses the transactivation of nuclear factor of activated T cells by targeting multiple genes and inhibits the proliferation of pulmonary artery smooth muscle cells. J Biol Chem. 2013;288:25414–27. doi: 10.1074/jbc.M113.460287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jalali S, et al. Mir-206 regulates pulmonary artery smooth muscle cell proliferation and differentiation. PLoS One. 2012;7:e46808. doi: 10.1371/journal.pone.0046808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gou D, et al. miR-210 has an antiapoptotic effect in pulmonary artery smooth muscle cells during hypoxia. Am J Physiol Lung Cell Mol Physiol. 2012;303:L682–91. doi: 10.1152/ajplung.00344.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Courboulin A, et al. Role for miR-204 in human pulmonary arterial hypertension. J Exp Med. 2011;208:535–48. doi: 10.1084/jem.20101812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Meloche J, et al. Role for DNA damage signaling in pulmonary arterial hypertension. Circulation. 2014;129:786–97. doi: 10.1161/CIRCULATIONAHA.113.006167. [DOI] [PubMed] [Google Scholar]
- 60.Drake KM, et al. Altered microRNA processing in heritable pulmonary arterial hypertension: an important role for Smad-8. Am J Respir Crit Care Med. 2011;184:1400–8. doi: 10.1164/rccm.201106-1130OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim J, et al. An endothelial apelin-FGF link mediated by miR-424 and miR-503 is disrupted in pulmonary arterial hypertension. Nat Med. 2013;19:74–82. doi: 10.1038/nm.3040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Grant JS, White K, MacLean MR, Baker AH. MicroRNAs in pulmonary arterial remodeling. Cell Mol Life Sci. 2013;70:4479–94. doi: 10.1007/s00018-013-1382-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Meloche J, Paulin R, Provencher S, Bonnet S. Therapeutic potential of microRNA modulation in pulmonary arterial hypertension. Curr Vasc Pharmacol. 2013 2013 May 13; doi: 10.2174/15701611113119990010. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 64.Paulin R, Courboulin A, Barrier M, Bonnet S. From oncoproteins/tumor suppressors to microRNAs, the newest therapeutic targets for pulmonary arterial hypertension. J Mol Med (Berl) 2011;89:1089–101. doi: 10.1007/s00109-011-0788-5. [DOI] [PubMed] [Google Scholar]
- 65.Grimminger F, Schermuly RT. PDGF receptor and its antagonists: role in treatment of PAH. Adv Exp Med Biol. 2010;661:435–46. doi: 10.1007/978-1-60761-500-2_28. [DOI] [PubMed] [Google Scholar]
- 66.Grotendorst GR, Chang T, Seppa HE, Kleinman HK, Martin GR. Platelet-derived growth factor is a chemoattractant for vascular smooth muscle cells. J Cell Physiol. 1982;113:261–6. doi: 10.1002/jcp.1041130213. [DOI] [PubMed] [Google Scholar]
- 67.Ross R, Glomset J, Kariya B, Harker L. A platelet-dependent serum factor that stimulates the proliferation of arterial smooth muscle cells in vitro. Proc Natl Acad Sci U S A. 1974;71:1207–10. doi: 10.1073/pnas.71.4.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schermuly RT, et al. Reversal of experimental pulmonary hypertension by PDGF inhibition. J Clin Invest. 2005;115:2811–21. doi: 10.1172/JCI24838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Humbert M, et al. Platelet-derived growth factor expression in primary pulmonary hypertension: comparison of HIV seropositive and HIV seronegative patients. Eur Respir J. 1998;11:554–9. [PubMed] [Google Scholar]
- 70.Yu Y, et al. PDGF stimulates pulmonary vascular smooth muscle cell proliferation by up-regulating TRPC6 expression. Am J Physiol Cell Physiol. 2003;284:C316–30. doi: 10.1152/ajpcell.00125.2002. [DOI] [PubMed] [Google Scholar]
- 71.Balasubramaniam V, et al. Role of platelet-derived growth factor in vascular remodeling during pulmonary hypertension in the ovine fetus. Am J Physiol Lung Cell Mol Physiol. 2003;284:L826–33. doi: 10.1152/ajplung.00199.2002. [DOI] [PubMed] [Google Scholar]
- 72.Jankov RP, et al. A role for platelet-derived growth factor beta-receptor in a newborn rat model of endothelin-mediated pulmonary vascular remodeling. Am J Physiol Lung Cell Mol Physiol. 2005;288:L1162–70. doi: 10.1152/ajplung.00180.2004. [DOI] [PubMed] [Google Scholar]
- 73.Ghofrani HA, Seeger W, Grimminger F. Imatinib for the treatment of pulmonary arterial hypertension. N Engl J Med. 2005;353:1412–3. doi: 10.1056/NEJMc051946. [DOI] [PubMed] [Google Scholar]
- 74.Hoeper MM, et al. Imatinib mesylate as add-on therapy for pulmonary arterial hypertension: results of the randomized IMPRES study. Circulation. 2013;127:1128–38. doi: 10.1161/CIRCULATIONAHA.112.000765. [DOI] [PubMed] [Google Scholar]
- 75.Mucke H. The role of imatinib in the treatment of pulmonary hypertension. Drugs Today (Barc) 2013;49:203–11. doi: 10.1358/dot.2013.49.3.1937430. [DOI] [PubMed] [Google Scholar]
- 76.Clifford RL, Deacon K, Knox AJ. Novel regulation of vascular endothelial growth factor-A (VEGF-A) by transforming growth factor (beta)1: requirement for Smads, (beta)-CATENIN, AND GSK3(beta) J Biol Chem. 2008;283:35337–53. doi: 10.1074/jbc.M803342200. [DOI] [PubMed] [Google Scholar]
- 77.Hassoun PM, et al. Inflammation, growth factors, and pulmonary vascular remodeling. J Am Coll Cardiol. 2009;54:S10–9. doi: 10.1016/j.jacc.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 78.Partovian C, et al. Heart and lung VEGF mRNA expression in rats with monocrotaline- or hypoxia-induced pulmonary hypertension. Am J Physiol. 1998;275:H1948–56. doi: 10.1152/ajpheart.1998.275.6.H1948. [DOI] [PubMed] [Google Scholar]
- 79.Campbell AI, Zhao Y, Sandhu R, Stewart DJ. Cell-based gene transfer of vascular endothelial growth factor attenuates monocrotaline-induced pulmonary hypertension. Circulation. 2001;104:2242–8. doi: 10.1161/hc4201.097838. [DOI] [PubMed] [Google Scholar]
- 80.Partovian C, et al. Adenovirus-mediated lung vascular endothelial growth factor overexpression protects against hypoxic pulmonary hypertension in rats. Am J Respir Cell Mol Biol. 2000;23:762–71. doi: 10.1165/ajrcmb.23.6.4106. [DOI] [PubMed] [Google Scholar]
- 81.Mata-Greenwood E, Grobe A, Kumar S, Noskina Y, Black SM. Cyclic stretch increases VEGF expression in pulmonary arterial smooth muscle cells via TGF-beta1 and reactive oxygen species: a requirement for NAD(P)H oxidase. Am J Physiol Lung Cell Mol Physiol. 2005;289:L288–9. doi: 10.1152/ajplung.00417.2004. [DOI] [PubMed] [Google Scholar]
- 82.Mata-Greenwood E, Meyrick B, Soifer SJ, Fineman JR, Black SM. Expression of VEGF and its receptors Flt-1 and Flk-1/KDR is altered in lambs with increased pulmonary blood flow and pulmonary hypertension. Am. J. Physiol. Lung Cell. Mol. Physiol. 2003;285:L222–31. doi: 10.1152/ajplung.00388.2002. [DOI] [PubMed] [Google Scholar]
- 83.Firth AL, Yao W, Remillard CV, Ogawa A, Yuan JX. Upregulation of Oct-4 isoforms in pulmonary artery smooth muscle cells from patients with pulmonary arterial hypertension. Am J Physiol Lung Cell Mol Physiol. 2010;298:L548–57. doi: 10.1152/ajplung.00314.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Greco SJ, Liu K, Rameshwar P. Functional similarities among genes regulated by OCT4 in human mesenchymal and embryonic stem cells. Stem Cells. 2007;25:3143–54. doi: 10.1634/stemcells.2007-0351. [DOI] [PubMed] [Google Scholar]
- 85.Yoshida T, Kaestner KH, Owens GK. Conditional deletion of Kruppel-like factor 4 delays downregulation of smooth muscle cell differentiation markers but accelerates neointimal formation following vascular injury. Circ Res. 2008;102:1548–57. doi: 10.1161/CIRCRESAHA.108.176974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Freyd G, Kim SK, Horvitz HR. Novel cysteine-rich motif and homeodomain in the product of the Caenorhabditis elegans cell lineage gene lin-11. Nature. 1990;344:876–9. doi: 10.1038/344876a0. [DOI] [PubMed] [Google Scholar]
- 87.Kwapiszewska G, et al. Fhl-1, a new key protein in pulmonary hypertension. Circulation. 2008;118:1183–94. doi: 10.1161/CIRCULATIONAHA.107.761916. [DOI] [PubMed] [Google Scholar]
- 88.Bonnet S, et al. An abnormal mitochondrial-hypoxia inducible factor-1alpha-Kv channel pathway disrupts oxygen sensing and triggers pulmonary arterial hypertension in fawn hooded rats: similarities to human pulmonary arterial hypertension. Circulation. 2006;113:2630–41. doi: 10.1161/CIRCULATIONAHA.105.609008. [DOI] [PubMed] [Google Scholar]
- 89.Semenza GL. Pulmonary vascular responses to chronic hypoxia mediated by hypoxia-inducible factor 1. Proc Am Thorac Soc. 2005;2:68–70. doi: 10.1513/pats.200404-029MS. [DOI] [PubMed] [Google Scholar]
- 90.Li X, et al. Notch3 signaling promotes the development of pulmonary arterial hypertension. Nature Med. 2009;15:1289–97. doi: 10.1038/nm.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Campos AH, Wang W, Pollman MJ, Gibbons GH. Determinants of Notch-3 receptor expression and signaling in vascular smooth muscle cells: implications in cell-cycle regulation. Circ Res. 2002;91:999–1006. doi: 10.1161/01.res.0000044944.99984.25. [DOI] [PubMed] [Google Scholar]
- 92.Morrow D, et al. Notch-mediated CBF-1/RBP-J{kappa}-dependent regulation of human vascular smooth muscle cell phenotype in vitro. Am J Physiol Cell Physiol. 2005;289:C1188–96. doi: 10.1152/ajpcell.00198.2005. [DOI] [PubMed] [Google Scholar]
- 93.Wang W, Prince CZ, Mou Y, Pollman MJ. Notch3 signaling in vascular smooth muscle cells induces c-FLIP expression via ERK/MAPK activation. Resistance to Fas ligand-induced apoptosis. J Biol Chem. 2002;277:21723–9. doi: 10.1074/jbc.M202224200. [DOI] [PubMed] [Google Scholar]
- 94.Berset T, Hoier EF, Battu G, Canevascini S, Hajnal A. Notch inhibition of RAS signaling through MAP kinase phosphatase LIP-1 during C. elegans vulval development. Science. 2001;291:1055–8. doi: 10.1126/science.1055642. [DOI] [PubMed] [Google Scholar]
- 95.Lowery JW, et al. ID family protein expression and regulation in hypoxic pulmonary hypertension. Am J Physiol Regul Integr Comp Physiol. 2010;299:R1463–77. doi: 10.1152/ajpregu.00866.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Perk J, Iavarone A, Benezra R. Id family of helix-loop-helix proteins in cancer. Nat Rev Cancer. 2005;5:603–14. doi: 10.1038/nrc1673. [DOI] [PubMed] [Google Scholar]
- 97.Yang J, et al. Smad-dependent and smad-independent induction of id1 by prostacyclin analogues inhibits proliferation of pulmonary artery smooth muscle cells in vitro and in vivo. Circ Res. 2010;107:252–62. doi: 10.1161/CIRCRESAHA.109.209940. [DOI] [PubMed] [Google Scholar]