Abstract
Aim:
To investigate the anti-hyperprolactinemia activity of casticin, a flavonoid isolated from Vitex rotundifolia, and elucidate its molecular mechanism.
Methods:
Hyperprolactinemia (MIHP) was induced by administration of metoclopramide dihydrochloride (50 mg/kg, tid, ip, for 10 d) in SD rats and the primary pituitary cells were prepared from the pituitary glands of the SD rats. Prolactin concentrations were measured using a radioimmunoassay. Cell viability was measured using an MTT assay. The mRNA expression of estrogen receptor alpha and beta in rat pituitary cells was measured using semi-quantitative RT-PCR analysis.
Results:
The level of serum prolactin in the MIHP model group was 2.1 fold higher than that in the untreated control group (P<0.01). Casticin (10, 20, and 40 mg/kg, ip, for 7 d) reduced serum prolactin levels by 33.9%, 54.3%, and 64.7%, respectively (P<0.01). The positive control drug bromocriptine 1 mg/kg decreased the serum prolactin concentration in MIHP rats by 44.9%. 17β-Estradiol (E2) significantly increased the proliferation of pituitary cells and casticin (1 and 10 μmol/L) markedly inhibited E2-induced pituitary cell proliferation by 27.7% and 42.1%, respectively. Stimulation of pituitary cells with E2 increased prolactin secretion into the cell culture supernatants, and casticin (0.1, 1, and 10 μmol/L) significantly inhibited the prolactin release stimulated by E2 in a concentration-dependent manner. Casticin (1 and 10 μmol/L) significantly inhibited ERα mRNA expression in pituitary cells stimulated with E2 (P<0.01) but increased ERβ mRNA expression at a concentration of 10 μmol/L (P<0.01). However, casticin had no effects on proliferation and prolectin release of the unstimulated primary pituitary cells in vitro.
Conclusion:
Casticin inhibited the release of prolactin from pituitary cells of SD rats stimulated with E2 in vivo and in vitro. These effects might be related with inhibiting the ERα mRNA expression and increasing the ERβ mRNA expression.
Keywords: casticin, premenstrual syndrome, prolactin, estrogen, estrogen receptors
Introduction
Premenstrual syndrome (PMS) involves physical, psychological and behavioral symptoms and occurs during the luteal phase of the menstrual cycle and disappears at the onset of menstruation1, 2. At least one premenstrual symptom occurs in 95% of women of reproductive age3. The main treatment strategies involve ovulation suppression or targeting the central nervous system components that are thought to be involved in the etiology of PMS4. As demonstrated by several clinical studies, PMS patients hypersecrete prolactin in response to the pressures of daily life, which leads to an unphysiological stimulation of the mammary gland, thereby causing mastodynia5. The release of prolactin is associated with a variety of factors such as estrogens, thyroid-releasing factor, vasoactive intestinal peptides, opioids, surgery, illness, and mental or physical stress6. In the pituitary, estrogen promotes the proliferation of several pituitary cell types and the production of prolactin7. It has been shown that prolactin synthesis is increased by 17β-estradiol (E2) through direct binding to the promoter region of the prolactin gene8. Studies suggest that changes in follicular or periovulatory estradiol secretion may be critical to the onset of symptoms of PMS9, 10. It has been widely accepted that the action of E2 is mediated by the nuclear estrogen receptors (ER), ERα and ERβ11, 12, which function as ligand-dependent transcription factors and regulate the transcription of target genes. ERα plays the major role in estrogen responsiveness in the female rat pituitary13 due it having a higher affinity to estrogen than ERβ does. However, ERβ decreases the sensitivity of ERα to estrogen, thereby acting as a physiological regulator of the effects of ERα14.
Vitex rotundifolia, which belongs to the same genus as V agnus-castus, belongs to the family Verbenaceae. V agnus-castus has been proved to be effective in treating patients with PMS15. In our previous study, we found that the flavone-enriched fraction extracted from V rotundifolia decreases serum prolactin levels in metoclopramide dihydrochloride-induced hyperprolactinemia (MIHP) mice, and casticin is the active component of this extract2. In order to understand the inhibitory effects of casticin on prolactin release in rats, we used both in vivo and in vitro models to investigate the effects of casticin on prolactin release and the mechanisms of regulation of estrogen and estrogen receptors.
Materials and methods
Materials
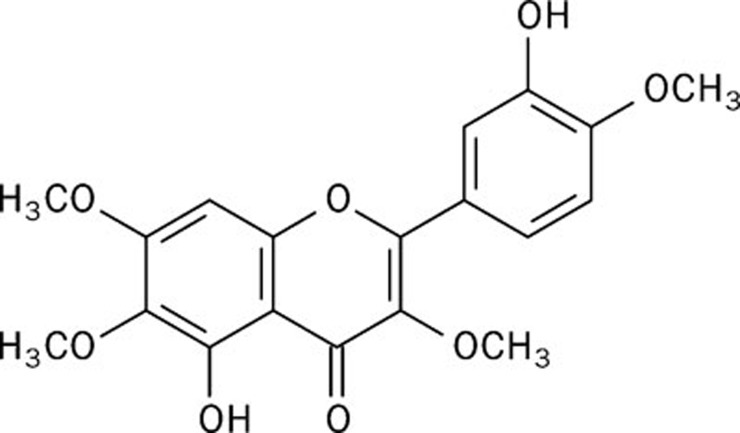
Casticin (3',5-dihydroxy-3,4',6,7-tetramethoxyflavone, Figure 1) was isolated from the methanol extract of fruits of Vitex rotundifolia L, and its chemical structure was identified by spectrum analysis. Phenol red-free Dulbecco's modified Eagle's medium (DMEM) and fetal bovine serum (FBS) were purchased from Gibco (USA). Bovine serum albumin (BSA) was purchased from Sigma (USA). Bromocriptine was purchased from Novartis Pharma SPA (Italy). Metoclopramide dihydrochloride was obtained from Harvest Pharmaceutical CO. The other chemicals were domestic AR grade.
Figure 1.
Chemical structure of casticin.
Animal model and drug treatment
Sixty adult female Sprague Dawley (SD) rats (180–220 g) were purchased from the Experimental Animal Center of the Second Military Medical University. These animals had free access to food and water and were housed in a room with a 12-h light/dark cycle. Animal experiments were performed in accordance with the guidelines of the Institutional Animal Ethics Committee of the Second Military Medical University.
Animals were grouped randomly into six groups (n=10). Ten rats were not treated and served as the normal control. Hyperprolactinemia was induced in 50 rats using metoclopramide dihydrochloride (50 mg/kg, tid×10 d, ip)16. The hyperprolactinemia SD rats were then treated daily with saline (vehicle control), bromocriptine (1 mg/kg) or different doses of casticin (10, 20, and 40 mg/kg, ip) for 1 week. Blood samples were collected from the orbit vein without anesthesia. The sera were obtained by centrifugation at 2500×g for 15 min and were stored at −20 °C until the prolactin assay was performed16, 17.
Pituitary cell proliferation in vitro
Primary pituitary cells were prepared from the pituitary glands of the SD rats as described18. In brief, the pituitaries from five rats were cut into small pieces and incubated at 37 °C with 2.5% trypsin for 15 min, then treated with 2 mg/L DNase and trypsin inhibitor. Cells were dispersed, seeded into 96-well culture plates at a density of 2×105 cells/well and cultured in phenol red-free DMEM supplemented with 10% fetal bovine serum, 0.1 mmol/L nonessential amino acids, 25 μmol/L dexamethasone, 5 g/L insulin, 1 μg/L fibroblast growth factor, 100 000 U/L penicillin, 100 mg/L streptomycin and 60 pmol/L triiodothyronine for 24 h at 37 °C in a humidified atmosphere of 5% CO2.
To determine the effect of casticin on cell proliferation, the culture medium was replaced with the above phenol red-free conditioned DMEM supplemented as above except for the use of 0.1% BSA instead of 10% fetal bovine serum. Casticin was then added, and the cells were incubated for an additional 72 h. The numbers of metabolically active mitochondria and viable cells were determined colorimetrically at 550 nm using an ELx800 universal microplate reader (Bio-Tek) and MTT [3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide] as described. To analyze the effect of casticin on E2-driven proliferation, cells were pretreated with E2 (0.01 μmol/L) for 4 h and then thoroughly washed with phosphate buffered saline. Casticin was then added, and the cells were incubated for an additional 72 h.
Prolactin release from pituitary cells in vitro
To test the effect of casticin on E2-induced prolactin release, primary pituitary cells were seeded into 96-well culture plates at a density of 2×105 cells/well, pretreated with E2 (0.01 μmol/L) for 4 h, then treated with casticin at final concentrations of 0.01, 0.1, 1, and 10 μmol/L for 48 h. The supernatants were collected and stored at −20 °C for measurement of the concentration of prolactin.
Prolactin radioimmunoassay
The prolactin concentration was measured using a double-antibody radioimmunoassay method as previously described17. The assay used human prolactin as a standard, and anti-human prolactin antiserum from rabbits (UCB-Bioproducts, Brussels, Belgium) that interacted with the 125I-labeled human prolactin (Dupont New England Nuclear, Boston, MA, USA) served as a tracer. A sheep anti-rabbit gamma-globulin (UCB-Bioproducts) was used as the second antibody. The immuno-titration curve for common rat serum prolactin was found to be parallel to the human prolactin standard curve17. The assay sensitivity was 0.5 μg/L, and the inter- and intra-assay coefficients of variation were 10% and 4%, respectively.
ERα and ERβ mRNA expression analysis using RT-PCR
Pituitary cells were seeded into 6-well tissue culture plates at a density of 2×106 cells/well. Cells were primed with 0.01 μmol/L E2 for 4 h at 37 °C and then treated with casticin at final concentrations of 0.01, 0.1, 1, and 10 μmol/L for 48 h. Total RNA was isolated using a TRIzol reagent kit and was reverse transcribed to form cDNA with a Revert Ace-α-R kit (TOYOBO, Osaka, Japan) according to the manufacturer's recommendations. The primer sequences were as follows: ERα sense primer: 5′-AATTCTGACAATCGACGCCAG-3′ ERα antisense primer: 5′-GTGCTTCAACATTCTCCCTCCTC-3′ ERβ sense primer: 5′-AAAGCCAAGAGAAACGGTGGGCAT-3′ ERβ antisense primer: 5′-GCCAATCATGTGCACCAGTTCCTT-3′ β-actin sense primer: 5′-TTGTAACCA ACTGGGACGATATGG-3′ and β-actin antisense primer: 5′-GATCTTGATCTTCATGGTTGCTAGG-3′. The PCR reaction mixture, in a total volume of 25 μL, contained 2.5 μL 10×buffer, 2 μL dNTPs (0.2 mmol/L each), 2 μL forward primer (2.5 mmol/L), 2 μL reverse primer (2.5 mmol/L), 0.5 μL rTaq polymerase, 2 μL cDNA template and 14 μL dH2O. The PCR conditions used for ERα and ERβ were as follows: initial denaturation at 94 °C for 4 min; 32–33 cycles of 94 °C for 45 s, 63 °C for 45 s, and 72 °C for 60 s; and a final extension at 72 °C for 7 min. The expression of β-actin was used as an internal standard. The PCR products were electrophoresed on a 1.5% agarose gel and visualized with ethidium bromide staining. The densities of the bands were determined using a bio-imagine analyzer (Bio-Rad), and quantification of the products was performed using Quantity One version 4.2.2 software (Bio-Rad).
Statistical analysis
Data were evaluated for statistical significance using the Student's t-test. A value of P<0.05 was considered significant. All data were expressed as the mean±SD of triplicate independent experiments, and representative experiments are shown.
Results
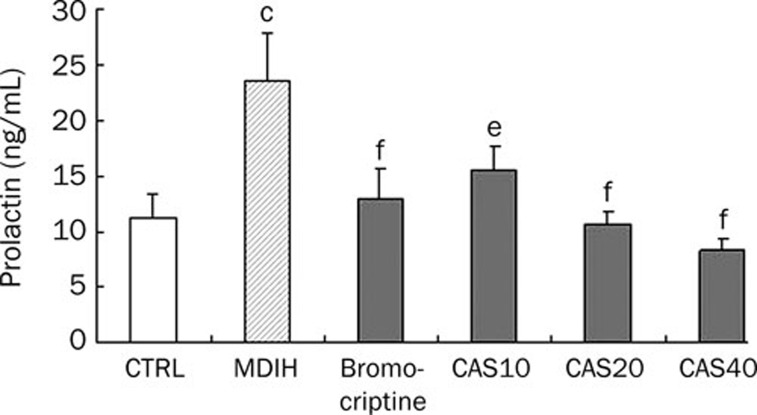
Anti-hyperprolactinemia activity in vivo
The animals were either left untreated or were given metoclopramide dihydrochloride (50 mg/kg, tid×10 d, ip) to induce hyperprolactinemia (MIHP). The level of serum prolactin in the MIHP model group was 2.1 fold higher than in the untreated control group (P<0.01). The elevated serum prolactin levels were reduced by 33.9%, 54.3%, and 64.7% with casticin at doses of 10, 20, and 40 mg/kg, respectively, and by 44.9% with bromocriptine at a dose of 1 mg/kg (Figure 2).
Figure 2.
Effects of casticin on MDIH rats. CAS10, CAS20, and CAS40 represent the prolactin levels, expressed as the percentage of production by the controls, of pituitary cells treated with casticin at doses of 10, 20, and 40 mg/kg, respectively. The data are represented as the mean±SD (n=10). cP<0.01 vs CTRL group, eP<0.05, fP<0.01 vs MDIH group.
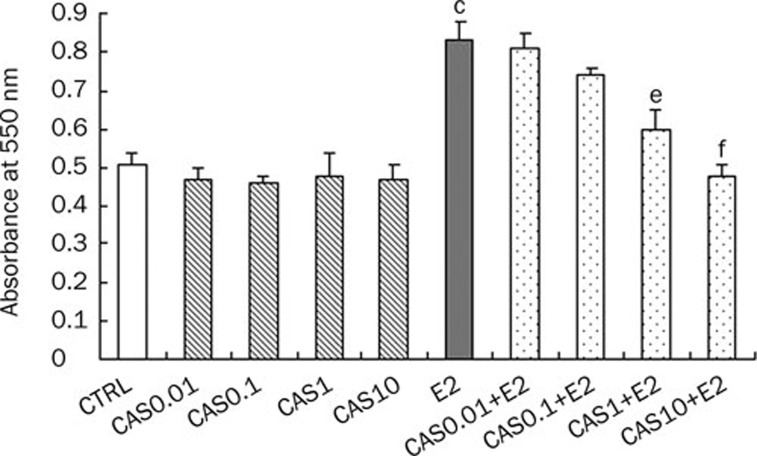
Effects on pituitary cell proliferation
To assess whether casticin affects pituitary cell proliferation, we first analyzed the effect of casticin on unstimulated pituitary cells. Casticin did not show any effect on the proliferation of pituitary cells at the tested concentrations. However, E2 significantly increased the proliferation of pituitary cells and casticin (1 and 10 μmol/L) markedly inhibited E2-driven pituitary cell proliferation by 27.7% and 42.1%, respectively. These results indicate that casticin could counteract the stimulatory effects of E2 on pituitary cell proliferation (Figure 3).
Figure 3.
Effects of casticin on pituitary cell proliferation. CAS0.01, CAS0.1, CAS1, and CAS10 represents the prolactin levels, expressed as the percentage of production by the controls, of pituitary cells treated with casticin for 48 h at doses of 0.01, 0.1, 1, and 10 μmol/L, respectively; E2 represents the prolactin level, expressed as the percentage of production by the controls, of pituitary cells stimulated with E2 (0.01 μmol/L) for 4 h; E2+CAS0.01, E2+CAS0.1, E2+CAS1, and E2+CAS10 represent prolactin levels, expressed as the percentage of production by the controls, of pituitary cells stimulated with E2 (0.01 μmol/L) for 4 h and then treated with casticin for 48 h at doses of 0.01, 0.1, 1, and 10 μmol/L, respectively. The data are represented as the mean±SD (n=10). cP<0.01 vs CTRL group, eP<0.05, fP<0.01 vs E2-treated group.
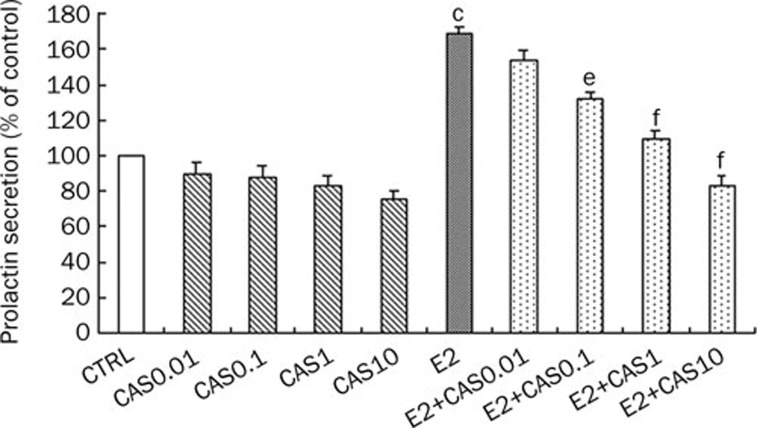
Effect on prolactin release from pituitary cells in vitro
Because casticin decreased the serum levels of prolactin in the MIHP model, we investigated whether this decrease was due to a direct effect of casticin on the pituitary cells. Casticin did not decrease prolactin release from unstimulated pituitary cells at the tested concentrations. We then explored the effect of casticin on prolactin secretion by the pituitary cells induced by E2. Stimulation of pituitary cells with E2 resulted in an increase in prolactin secretion into the cell culture supernatants, and casticin (0.1, 1, and 10 μmol/L) significantly inhibited prolactin release from E2-stimulated pituitary cells in a concentration-dependent manner (Figure 4). These results indicate that casticin attenuated the stimulatory effects of E2 and regulated prolactin release from pituitary cells.
Figure 4.
Effects of casticin on prolactin secretion of normal and E2-treated pituitary cells. CAS0.01, CAS0.1, CAS1, and CAS10 represent the prolactin levels, expressed as the percentage of production by the controls, of pituitary cells treated with casticin for 48 h at doses of 0.01, 0.1, 1, and 10 μmol/L, respectively; E2 represents the prolactin level, expressed as the percentage of production by the controls, of pituitary cells stimulated with E2 (0.01 μmol/L) for 4 h; E2+CAS0.01, E2+CAS0.1, E2+CAS1, and E2+CAS10 represents the prolactin levels, expressed as the percentage of production by the controls, of pituitary cells stimulated with E2 (0.01 μmol/L) for 4 h and then treated with casticin for 48 h at doses of 0.01, 0.1, 1, and 10 μmol/L, respectively. The data are represented as the mean±SD (n=10). cP<0.01 vs CTRL group, eP<0.05, fP<0.01 vs E2-treated group.
ERα and ERβ mRNA expression
To further understand the underlying mechanism of casticin's effects on prolactin secretion, we evaluated the effects of casticin on the expression of ER genes in rat pituitary cells. Stimulation of pituitary cells with E2 resulted in an increase in ERα and ERβ mRNA expression. Casticin (1 and 10 μmol/L) significantly inhibited ERα mRNA expression in pituitary cells stimulated with E2 (P<0.01) but increased ERβ mRNA expression at a concentration of 10 μmol/L (P<0.01, Figure 5).
Figure 5.
Effects of casticin on the mRNA expression of ERα and ERβ in pituitary cells stimulated with E2. Pituitary cells were stimulated with E2 (0.01 μmol/L) for 4 h and then treated with casticin for 48 h. E2+CAS0.1, E2+CAS1, and E2+CAS10 represent the expression of ERα or ERβ mRNA, expressed as the percentage of expression by the controls, in pituitary cells treated with casticin at doses of 0.1, 1, and 10 μmol/L, respectively. cP<0.01 vs CTRL group, fP<0.01 vs E2-treated group.
Discussion
It has been reported that women with very severe PMS have higher mid-cycle estrogen levels10 and that the symptom severity is strongly associated with high luteal-phase estradiol levels19. PMS patients experience significant symptom relief after administration of the gonadotropin-releasing hormone agonist leuprolide; in contrast, the addition of either estrogen or progesterone results in the recurrence of symptoms9. Estrogenic stimulation of prolactin secretion is the primary cause of higher serum prolactin concentrations in women20, 21. In our study, casticin significantly inhibited E2-stimulated pituitary cell proliferation and prolactin production in vitro, but casticin did not affect either the proliferation or the prolactin production of normal pituitary cells. These results suggest that casticin decreased prolactin production by counteracting the stimulatory effects of estrogen.
Other investigations have shown that the actions of estrogen on pituitary cells during the estrous cycle are probably mediated by ERα, and prolactin can stimulate estrogen receptor expression and increase the number of estradiol-binding sites22. In our study, casticin inhibited the mRNA expression of ERα in pituitary cells stimulated with E2. Hence, the prolactin-reducing effect of casticin might be due to its inhibition of ERα expression in pituitary cells. Further, the stimulatory effect of E2 decreased in the casticin-treated pituitary cells and led to a reduction in the proliferation and prolactin production of these pituitary cells. In addition, inhibition of pituitary cell proliferation by casticin might also contribute to the observed decrease of ER transcription and the reduced prolactin production.
Many premenstrual syndromes, particularly premenstrual mastalgia (mastodynia), are associated with latent hyperprolactinemia23, 24, 25. In addition, casticin has been demonstrated to reduce abnormally high serum prolactin levels in vivo (Figure 2). The level of prolactin in vivo is controlled not only by prolactin-releasing factor (PRF) and prolactin-inhibiting factors (PIF) such as dopamine but also by several possible stimulatory pathways that respond to serotonin reuptake, opiates, cocaine, and antihypertensive medications26. In previous studies on extracts of V agnus-castus using the corpus striatum membrane dopamine (DA) receptor binding assay in vitro, however, diterpenes (not casticin) were reported to be the active constituents, acting as DA agonists and inhibiting the release of prolactin15, 24. Therefore, the prolactin-reducing effect of casticin described in the hyperprolactinemia model in vivo may be due to other compounds counteracting the stimulatory effects of estrogen on pituitary cells. Unfortunately, we did not provide in vivo evidence for E2 involvement in the mechanism of action of casticin. Further studies should focus on these effects of casticin. Despite this limitation, our in vitro data provide deeper insight into the mechanisms underlying casticin-reduced prolactin production. In summary, in the fruits of Vitex rotundifolia and V agnus-castus, diterpenes inhibit the release of prolactin by acting as DA agonists, and the current study indicated that casticin counteracted the stimulatory effects of estrogen to reduce the production of prolactin.
In this study, we observed the effects of casticin on the release of prolactin in vivo and in vitro. Casticin inhibited the release of prolactin from pituitary cells stimulated with E2. These results further support the hypothesis that casticin might be the active constitute in Vitex rotundifolia extracts. This plant could be the source of an efficient alternative phytotherapeutic drug in the treatment of PMS.
Author contribution
Lu-ping QIN designed research; Qi YE performed research; Cheng-jian ZHENG and Yang WANG contributed new analytical tools and reagents; Qiao-yan ZHANG analyzed data; Qi YE wrote the paper.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (No 30772783).
References
- Reid RL, Yen SS. The premenstrual syndrome. Clin Obstet Gynecol. 1983;26:710–8. [PubMed] [Google Scholar]
- Hu Y, Xin HL, Zhang QY, Zheng HC, Rahman K, Qin LP. Anti-nociceptive and anti-hyperprolactinemia activities of Fructus Viticis and its effective fractions and chemical constituents. Phytomedicine. 2007;14:668–74. doi: 10.1016/j.phymed.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Dickerson LM, Mazyck PJ, Hunter MH. Premenstrual syndrome. Am Fam Physician. 2003;67:1743–52. [PubMed] [Google Scholar]
- Usman SB, Indusekhar R, O'Brien S. Hormonal management of premenstrual syndrome. Best Pract Res Clin Obstet Gynaecol. 2008;22:251–60. doi: 10.1016/j.bpobgyn.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Lurie S, Borenstein R. The premenstrual syndrome. Obstet Gynecol Surv. 1990;45:220–8. doi: 10.1097/00006254-199004000-00003. [DOI] [PubMed] [Google Scholar]
- Nagy I, MacLeod RM. Metabolic changes in the rat anterior pituitary and prolactin production following estradiol treatment. Metabolism. 1980;29:429–34. doi: 10.1016/0026-0495(80)90167-5. [DOI] [PubMed] [Google Scholar]
- Sarkar DK, Hentges ST, De A, Reddy RH. Hormonal control of pituitary prolactin-secreting tumors. Front Biosci. 1998;3:d934–43. doi: 10.2741/a334. [DOI] [PubMed] [Google Scholar]
- Freeman ME, Kanyicska B, Lerant A, Nagy G. Prolactin: structure, function, and regulation of secretion. Physiol Rev. 2000;80:1523–631. doi: 10.1152/physrev.2000.80.4.1523. [DOI] [PubMed] [Google Scholar]
- Schmidt PJ, Nieman LK, Danaceau MA, Adams LF, Rubinow DR. Differential behavioral effects of gonadal steroids in women with and in those without premenstrual syndrome. N Engl J Med. 1998;338:209–16. doi: 10.1056/NEJM199801223380401. [DOI] [PubMed] [Google Scholar]
- Redei E, Freeman EW. Daily plasma estradiol and progesterone levels over the menstrual cycle and their relation to premenstrual symptoms. Psychoneuroendocrinology. 1995;20:259–67. doi: 10.1016/0306-4530(94)00057-h. [DOI] [PubMed] [Google Scholar]
- Green S, Walter P, Greene G, Krust A, Goffin C, Jensen E, et al. Cloning of the human oestrogen receptor cDNA. J Steroid Biochem. 1986;24:77–83. doi: 10.1016/0022-4731(86)90035-x. [DOI] [PubMed] [Google Scholar]
- Green S, Walter P, Kumar V, Krust A, Bornert JM, Argos P, et al. Human oestrogen receptor cDNA: sequence, expression and homology to v-erb-A. Nature. 1986;320:134–9. doi: 10.1038/320134a0. [DOI] [PubMed] [Google Scholar]
- Tena-Sempere M, Navarro VM, Mayen A, Bellido C, Sanchez-Criado JE. Regulation of estrogen receptor (ER) isoform messenger RNA expression by different ER ligands in female rat pituitary. Biol Reprod. 2004;70:671–8. doi: 10.1095/biolreprod.103.021378. [DOI] [PubMed] [Google Scholar]
- Hall JM, McDonnell DP. The estrogen receptor beta-isoform (ERbeta) of the human estrogen receptor modulates ERalpha transcriptional activity and is a key regulator of the cellular response to estrogens and antiestrogens. Endocrinology. 1999;140:5566–78. doi: 10.1210/endo.140.12.7179. [DOI] [PubMed] [Google Scholar]
- Berger D, Schaffner W, Schrader E, Meier B, Brattstrom A. Efficacy of Vitex agnus castus L extract Ze 440 in patients with pre-menstrual syndrome (PMS) Arch Gynecol Obstet. 2000;264:150–3. doi: 10.1007/s004040000123. [DOI] [PubMed] [Google Scholar]
- Lin KC, Kawamura N, Okamura H, Mori T. Inhibition of ovulation, steroidogenesis and collagenolytic activity in rabbits by sulpiride-induced hyperprolactinaemia. J Reprod Fertil. 1988;83:611–8. doi: 10.1530/jrf.0.0830611. [DOI] [PubMed] [Google Scholar]
- Moro M, Inada Y, Kojima M, Miyata H, Komatsu H, Torii R. New hyperprolactinemia and anovulation model in common marmoset (Callithrix jacchus) and effect of cabergoline. Eur J Pharmacol. 1999;368:57–66. doi: 10.1016/s0014-2999(98)00940-6. [DOI] [PubMed] [Google Scholar]
- Smith RE, Dean PN. A study of acid phosphatase and dipeptidyl aminopeptidase II in monodispersed anterior pituitary cells using flow cytometry and electron microscopy. J Histochem Cytochem. 1979;27:1499–504. doi: 10.1177/27.11.512332. [DOI] [PubMed] [Google Scholar]
- Seippel L, Backstrom T. Luteal-phase estradiol relates to symptom severity in patients with premenstrual syndrome. J Clin Endocrinol Metab. 1998;83:1988–92. doi: 10.1210/jcem.83.6.4899. [DOI] [PubMed] [Google Scholar]
- Frantz AG. Prolactin. N Engl J Med. 1978;298:201–7. doi: 10.1056/NEJM197801262980408. [DOI] [PubMed] [Google Scholar]
- Franks S. Regulation of prolactin secretion by oestrogens: physiological and pathological significance. Clin Sci (Lond) 1983;65:457–62. doi: 10.1042/cs0650457. [DOI] [PubMed] [Google Scholar]
- Frasor J, Gibori G. Prolactin regulation of estrogen receptor expression. Trends Endocrinol Metab. 2003;14:118–23. doi: 10.1016/s1043-2760(03)00030-4. [DOI] [PubMed] [Google Scholar]
- Jarry H, Leonhardt S, Wuttke W, Spengler B, Christoffel V. Auf der Suche nach dopaminergen Substanzen in Agni-casti-fructus-Präparaten: Warum eigentlich. Z Phytother. 1999;20:150–2. [Google Scholar]
- Jarry H, Leonhardt S, Gorkow C, Wuttke W. In vitro prolactin but not LH and FSH release is inhibited by compounds in extracts of Agnus castus: direct evidence for a dopaminergic principle by the dopamine receptor assay. Exp Clin Endocrinol. 1994;102:448–54. doi: 10.1055/s-0029-1211317. [DOI] [PubMed] [Google Scholar]
- Wuttke W, Jarry H, Christoffel V, Spengler B, Seidlova-Wuttke D. Chaste tree (Vitex agnus-castus) — pharmacology and clinical indications. Phytomedicine. 2003;10:348–57. doi: 10.1078/094471103322004866. [DOI] [PubMed] [Google Scholar]
- Molitch ME. Medical management of prolactin-secreting pituitary adenomas. Pituitary. 2002;5:55–65. doi: 10.1023/a:1022375429083. [DOI] [PubMed] [Google Scholar]