Abstract
Expression of Toll-like receptors (TLRs) in B cells provides a cell-intrinsic mechanism for innate signals regulating adaptive immune responses. In combination with other signaling pathways in B cells, including through the B-cell receptor (BCR), TLR signaling plays multiple roles in B-cell differentiation and activation. The outcome of TLR signaling in B cells is largely context-dependent, which partly explains discrepancies among in vitro and in vivo studies, or studies using different immunogens. We focus on recent findings on how B-cell-intrinsic TLR signaling regulates antibody responses, including germinal center formation and autoantibody production in autoimmune disease models. In addition, TLR signaling also acts on the precursors of B cells, which could influence the immune response of animals by shaping the composition of the immune system. With TLR signaling modulating immune responses at these different levels, much more needs to be understood before we can depict the complete functions of innate signaling in host defense.
Keywords: autoimmunity, B-cell development, germinal center, Toll-like receptor
Introduction
As one of the most important families of pattern recognition receptors, the Toll-like receptor (TLR) family plays critical roles in initiating innate inflammatory responses and promoting adaptive immune responses.1 In humans and mice, there are 10–13 TLRs that recognize different components of bacteria and viruses, such as lipopolysaccharide (LPS), ssRNA and CpG-containing DNA. Most TLRs signal via an adaptor protein called myeloid differentiation factor 88 (MyD88), except for TLR3, which signals through TIR domain-containing adaptor-inducing interferon-β (TRIF), and TLR4, which signals through both. Both MyD88 and TRIF pathways elicit transcriptional alterations through the activation of nuclear factor-κB and other transcription factors.2 Interestingly, not all TLRs are expressed on the cell surface. TLR3, 7 and 9, which recognize bacterial and viral nucleic acids, are localized to intracellular membranes and are activated in phagolysosomes or endosomes.3 The restricted access to these TLRs may be important to prevent their aberrant activation by self-nucleic acids released from apoptotic cells, which could lead to autoimmune diseases.
Antibody production by B cells is a major adaptive immune mechanism in host defense against infectious agents. Both human and murine B cells express several different types of TLRs.4 Purified TLR agonists are known to act on their own as effective adjuvants for antibody responses in both mice and humans.4,5,6 Over the last few years, research on TLR signaling in B cells has generated enormous interest due to its potential application in vaccine design and other B cell-related diseases. However, we are just beginning to understand the full scope of how the role of TLR signaling in antibody responses can be applied to health and disease conditions. This review will highlight some recent findings on the roles of TLR signaling in B-cell development and activation.
TLR signaling in B-cell development
B cells originate from hematopoietic stem cells (HSCs), and undergo several developmental stages including early lymphoid progenitor, common lymphoid progenitor (CLP), pro-B and pre-B cells within the bone marrow, and transitional B cells in the peripheral lymphoid organs, before developing into mature B cells.7 Lack of overt defect in peripheral and bone marrow B cell numbers in the absence of TLR signaling makes its role in B-cell development less obvious. However, emerging evidence suggests that TLR signaling is involved in B-cell lymphopoiesis, as well as in shaping the composition of the B-cell repertoire.
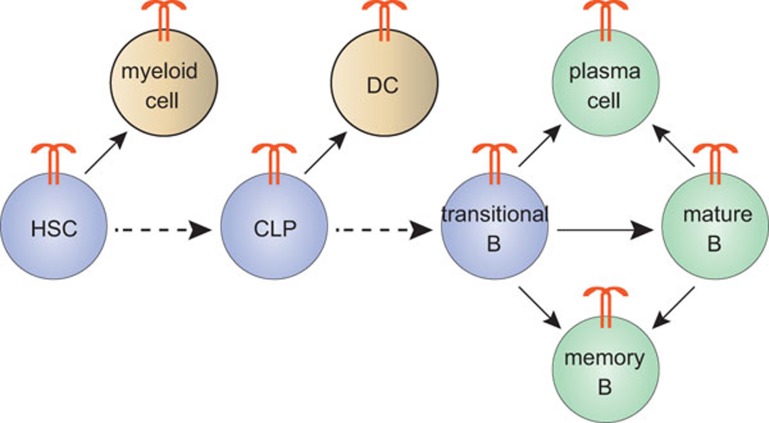
Surprisingly, it was revealed that HSCs could recognize pathogen, when Kincade and colleagues found functional TLR expression in early hematopoietic progenitors.8 TLR signaling in these cells shifts their development potential towards myelopoiesis rather than lymphopoiesis (Figure 1).8 Further studies showed that CLPs from mice infected with herpes simplex virus differentiated into dendritic cells (DCs) instead of B cells (Figure 1) and that this phenomenon was mainly mediated by TLR9 signaling.9 Dynamic change of hematopoiesis upon environmental stress might provide an evolutionary advantage for rapid adaptation to microbial infections but might also be responsible for reduced lymphopoiesis during the normal aging process. Indeed, chronic exposure to low doses of LPS, a TLR4 ligand, causes HSCs to lose their ability to maintain quiescence, a phenomenon that also occurs in aging.10
Figure 1.
Functions of TLR signaling in B-cell development and differentiation. TLRs are expressed through most stages of B-cell development, including HSCs and CLPs. Activation of TLR signaling in HSCs shifts their developmental potential towards myeloid cells. TLR signaling in CLPs causes cell differentiation into DCs instead of B cells. Transitional B cells can differentiate into mature B cells, plasma cells and IgM memory B cells upon TLR activation. The roles of TLR signaling in mature B cells are simplified here and are described in more detail elsewhere. Arrows with solid or dashed lines indicate that the processes respectively promoted or inhibited by TLR signaling. Abbreviations: CLP, common lymphoid progenitor; DC, dendritic cell; HSC, hematopoietic stem cell; TLR, Toll-like receptor.
In addition to B-cell lineage determination, TLR signaling may play a role in the process of negative selection. Meffre and colleagues11 found an increased ratio of autoreactive B cells to naive B cells in patients deficient in MyD88 or IRAK4 (a kinase downstream of MyD88 signaling) compared to healthy controls, suggesting a defect in negative selection. The underlying mechanism is not clear, but based on recent findings of synergy between TLR and B-cell receptor (BCR) signaling,12 a possible explanation is that reduced TLR signaling may grant B cells a higher threshold to be eliminated during negative selection. On the other hand, studies using BCR transgenic mice suggested a positive role for TLR signaling in cell survival during negative selection. In mice deficient in Lyn kinase, a negative regulator of BCR signaling in vivo, B cell numbers decreased dramatically due to increased negative selection.13 Consistently, in lyn−/− mice that expressed an anti-hen-egg lysozyme BCR transgene, the majority of anti-hen-egg lysozyme transgenic B cells were eliminated in the presence of soluble hen-egg lysozyme. In contrast, in lyn−/− mice that expressed an anti-dsDNA BCR transgene, the anti-dsDNA transgenic B cells survived,14 suggesting the possibility that TLR signaling activated by endogenous DNA might counteract the apoptotic process. Further study is required to clarify these opposing roles of TLR signaling in B-cell negative selection.
Interestingly, TLR activation in transitional B cells (T1 and T2), which is also the stage for negative selection, might change cell differentiation routes. For example, one study found that T1 B cells could be activated by LPS or CpG to secrete IgM and class-switched Igs.15 Another study found that CpG stimulated T1 and T2 B cells to secrete proinflammatory cytokines.16 Carsetti and colleagues reported that CpG induced transitional B cells isolated from human cord blood to differentiate into plasma cells with both class switch and somatic hypermutations.17 A recent study from the same group demonstrated the differentiation of transitional B cells into phenotypic IgM memory B cells (Figure 1).18 These works suggest the possibility for a role of TLR signaling in regulating B-cell sub-populations and in BCR repertoire adjustment. In line with the in vitro data, it was found that IgM+IgD+CD27+ cells (mostly likely human IgM memory B cells) are significantly reduced in MyD88- and IRAK4-deficient patients.19
TLR signaling in antibody response to immunization
It has long been known that stimulation of mature B cells in vitro with TLR ligands leads to B-cell proliferation and differentiation into plasma cells. Therefore, TLR signaling in B cells has been generally assumed to account for the adjuvant effect in any immunization regimen. However, Nemazee and colleagues tested four typical adjuvants (alum, Freund's complete adjuvant, Freund's incomplete adjuvant, and monophosphoryl-lipid A adjuvant) with both T cell-dependent (TD) and T cell-independent (TI) antigens in MyD88−/−Trif−/− mice and found no significant change in antibody response compared to wild-type mice.20 This may not be a surprise because other innate signaling pathways may mediate the effect of these adjuvants. In cases of antigens containing defined TLR ligands, TLR signaling does play important roles in many aspects of antibody response. Many TI antigens themselves exist as, or contain, TLR ligands, such as LPS. For these types of antigens, it is thought that engagement of both BCR and TLR signaling provides a strong signal for B-cell activation. In vivo, there is a clear dependence on B-cell TLR signaling for the IgM response to these antigens.21 Interestingly, for proteins conjugated with TLR ligands, which are typical TD type antigens, the antigen-specific IgM response is also dependent on B-cell TLR signaling to some degree, consistent with most findings of B-cell responses to TLR ligands in vitro.22,23
A TD type IgG response is much more complicated because other immune cells, especially DCs, also express TLRs and contribute to antibody responses. Earlier work using adoptive transfer of MyD88−/− B cells into B cell-deficient mice demonstrated a requirement of MyD88 for a proper TD antibody response.24 Subsequent studies have either provided evidence for a role of TLRs in promoting antibody responses or failed to do so, depending on the circumstances examined.23,25 Various reasons have been proposed to explain the discrepancy in these studies, including the types of antigens used.26 To address this question, we used a conditional MyD88-deficient model.27 We immunized mice with several soluble protein antigens with variable levels of immunogenicity mixed or directly conjugated to a TLR ligand and found that the magnitude of the IgG responses was comparable between B cell MyD88-deficient mice and wild-type controls.22 However, MyD88 signaling in DCs accounted for most of the effect of TLR stimulation,22 presumably because TLR signaling in DCs is required for activation of CD4+ T follicular helper cells, which could provide sufficient stimulation to B cells.
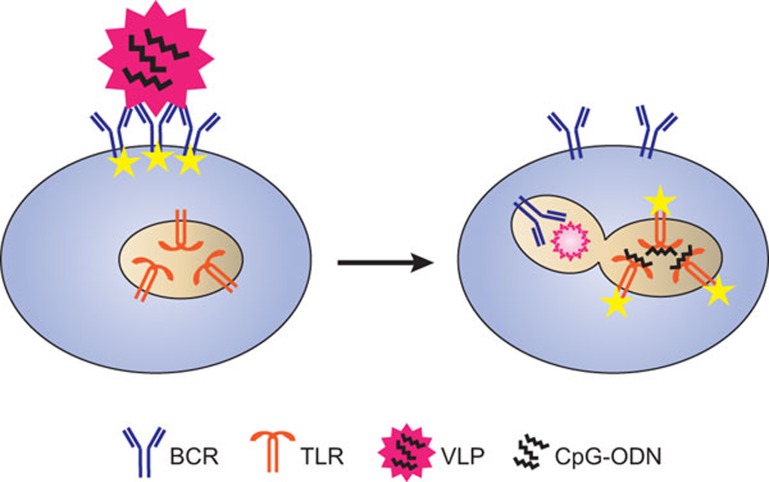
Intriguingly, when we immunized mice with virus-like particles (VLPs) containing CpG-oligodeoxynucleotides (a TLR9 ligand), we found that the deficiency of MyD88 in B cells caused a 30-fold decrease in IgG response. Moreover, the requirement of B cell MyD88 signaling strongly depends on the antigen epitope density on the surface of VLPs, suggesting a synergistic effect between BCR and TLR signaling.22 Because TLR9 is localized in endosomes, the CpG contained within the VLPs might reach TLR9 through BCR-mediated binding and internalization of VLPs (Figure 2). Whether the BCR signaling and TLR signaling are simply sequential events linked by membrane trafficking or they have crosstalk at a molecular level needs to be further examined. In addition, it is clear that B-cell TLR signaling promotes VLP antibody production through germinal center (GC) response,22 a unique mechanism markedly distinct from that in TI type responses. A similar study using the model retrovirus, Friend virus, also observed a similar requirement for B-cell TLR signaling in GC-mediated antibody responses.28 GC formation requires clonal expansion of B cells, migration and clustering of several other cell types as well as differentiation of T follicular helper cell.29 The requirements of B-cell TLR signaling within this complicated event remains to be elucidated.
Figure 2.
Working model of how VLPs induce B-cell TLR signaling. A VLP containing CpG-ODN binds to an antigen-specific B cell and elicits BCR signaling by crosslinking surface BCRs (indicated by yellow stars). TLR9 is localized to endosomes and is only activated following VLP internalization. Abbreviations: BCR, B-cell receptor; ODN, oligodeoxynucleotide; TLR, Toll-like receptor; VLP, virus-like particle.
TLR signaling in autoantibody production
Marshak-Rothstein's group first demonstrated that a synergistic engagement of BCR and TLR9 signaling could effectively activate autoreactive B cells in vitro.30 They tested B cells from AM14 transgenic mice (AM14 RF+ B cells), which express BCR that recognizes a specific IgG (IgG2aa). Upon adding IgG2aa isolated from the sera of autoimmune mice, AM14 RF+ B cells were activated and proliferated in vitro. However, when DNase was added to the assay medium, the proliferative response disappeared, suggesting that DNA is required to activate B cells. They further confirmed that chromatin-IgG complexes could access TLRs in B cells through BCR binding and, in addition to BCR signaling, TLR stimulation was essential for the activation of autoreactive B cells.30
The above in vitro data seem to be consistent with the in vivo study using a variety of different mouse models of autoimmune diseases. Genetic deficiency of TLR7, TLR9 or MyD88 often leads to reduced production of autoantibody, and increased expression of TLR7 causes susceptibility to autoimmune diseases.31 However, it is difficult to ascertain in vivo whether TLR signaling in B cells directly contributes to the pathogenesis of autoimmune diseases, especially when considering that DCs or plasmacytoid DCs are also activated by similar TLR ligands and play essential roles in propagating the diseases.32 Another question to consider is whether direct B-cell TLR signaling involves the TI or TD type response or other mechanisms.
It is known that autoantibodies bear somatic hypermutations, a sign of GC response. However, when Shlomchick's group crossed the AM14 transgenic mouse strain onto the MRL/lpr lupus-prone mouse strain to generate a model of systemic lupus erythematosus, they found that the autoreactive B cells actually proliferate and undergo somatic hypermutation in the so-called ‘extrafollicular' sites, not in GCs.33 Further study indicated that the extrafollicular TLR-dependent autoantibody response is independent of T cell help, although T cells can enhance this response.34 The roles of B-cell TLR signaling in autoantibody production thus might resemble those for the TI response discussed earlier, at least in this mouse model. Indeed, there are only a few studies thus far that have attempted to answer whether B cell intrinsic TLR signaling is required for the autoantibody production in vivo, and these studies did generate supporting evidence for it.35,36,37 We have used B cell MyD88-deficient mice crossed to a different systemic lupus erythematosus mouse model (lyn−/−) and found a strong dependence on B-cell TLR signaling for autoantibody level and associated pathological change. Surprisingly, the autoantibody production in this model mainly depends on GC response, in a similar manner as that in TD response to VLPs as mentioned previously (manuscript in preparation).
Conclusion
TLR signaling plays a variety of roles in B-cell development and activation. In addition to its functions in promoting antibody responses, TLR signaling is also involved in B-cell cytokine secretion, antigen presentation, Ig isotype switching and cell survival for long-lived plasma cells and memory B cells, which are beyond the scope of this review. Although B cell-intrinsic TLR signaling is important in all the aspects mentioned above, it is noteworthy that many other cell types express TLRs and can regulate B-cell functions when their TLRs are activated. Understanding the mechanisms of how innate signaling contributes to humoral responses will provide a platform for developing applications, including vaccines, for human diseases.
Acknowledgments
This work was supported by research grants from the National Natural Science Foundation of China to BH (31170848) and to ZH (31200669).
References
- Iwasaki A, Medzhitov R. Regulation of adaptive immunity by the innate immune system. Science. 2010;327:291–295. doi: 10.1126/science.1183021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akira S. Toll-like receptors and innate immunity. Adv Immunol. 2001;78:1–56. doi: 10.1016/s0065-2776(01)78001-7. [DOI] [PubMed] [Google Scholar]
- Barton GM, Kagan JC. A cell biological view of Toll-like receptor function: regulation through compartmentalization. Nat Rev Immunol. 2009;9:535–542. doi: 10.1038/nri2587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekeredjian-Ding I, Jego G. Toll-like receptors—sentries in the B-cell response. Immunology. 2009;128:311–323. doi: 10.1111/j.1365-2567.2009.03173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halperin SA, Dobson S, McNeil S, Langley JM, Smith B, McCall-Sani R, et al. Comparison of the safety and immunogenicity of hepatitis B virus surface antigen co-administered with an immunostimulatory phosphorothioate oligonucleotide and a licensed hepatitis B vaccine in healthy young adults. Vaccine. 2006;24:20–26. doi: 10.1016/j.vaccine.2005.08.095. [DOI] [PubMed] [Google Scholar]
- Jennings GT, Bachmann MF. The coming of age of virus-like particle vaccines. Biol Chem. 2008;389:521–536. doi: 10.1515/bc.2008.064. [DOI] [PubMed] [Google Scholar]
- Hardy RR, Kincade PW, Dorshkind K. The protean nature of cells in the B lymphocyte lineage. Immunity. 2007;26:703–714. doi: 10.1016/j.immuni.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Nagai Y, Garrett KP, Ohta S, Bahrun U, Kouro T, Akira S, et al. Toll-like receptors on hematopoietic progenitor cells stimulate innate immune system replenishment. Immunity. 2006;24:801–812. doi: 10.1016/j.immuni.2006.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welner RS, Pelayo R, Nagai Y, Garrett KP, Wuest TR, Carr DJ, et al. Lymphoid precursors are directed to produce dendritic cells as a result of TLR9 ligation during herpes infection. Blood. 2008;112:3753–3761. doi: 10.1182/blood-2008-04-151506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esplin BL, Shimazu T, Welner RS, Garrett KP, Nie L, Zhang Q, et al. Chronic exposure to a TLR ligand injures hematopoietic stem cells. J Immunol. 2011;186:5367–5375. doi: 10.4049/jimmunol.1003438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meffre E. The establishment of early B cell tolerance in humans: lessons from primary immunodeficiency diseases. Ann N Y Acad Sci. 2011;1246:1–10. doi: 10.1111/j.1749-6632.2011.06347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawlings DJ, Schwartz MA, Jackson SW, Meyer-Bahlburg A. Integration of B cell responses through Toll-like receptors and antigen receptors. Nat Rev Immunol. 2012;12:282–294. doi: 10.1038/nri3190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross AJ, Lyandres JR, Panigrahi AK, Prak ET, DeFranco AL. Developmental acquisition of the Lyn-CD22-SHP-1 inhibitory pathway promotes B cell tolerance. J Immunol. 2009;182:5382–5392. doi: 10.4049/jimmunol.0803941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo S, Buckler J, Erikson J. Novel roles for Lyn in B cell migration and lipopolysaccharide responsiveness revealed using anti-double-stranded DNA Ig transgenic mice. J Immunol. 2001;166:3710–3716. doi: 10.4049/jimmunol.166.6.3710. [DOI] [PubMed] [Google Scholar]
- Ueda Y, Liao D, Yang K, Patel A, Kelsoe G. T-independent activation-induced cytidine deaminase expression, class-switch recombination, and antibody production by immature/transitional 1 B cells. J Immunol. 2007;178:3593–3601. doi: 10.4049/jimmunol.178.6.3593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan M, Lopez-Herrera G, Blomberg KE, Lindvall JM, Berglof A, Smith CI, et al. Defective Toll-like receptor 9-mediated cytokine production in B cells from Bruton's tyrosine kinase-deficient mice. Immunology. 2008;123:239–249. doi: 10.1111/j.1365-2567.2007.02693.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capolunghi F, Cascioli S, Giorda E, Rosado MM, Plebani A, Auriti C, et al. CpG drives human transitional B cells to terminal differentiation and production of natural antibodies. J Immunol. 2008;180:800–808. doi: 10.4049/jimmunol.180.2.800. [DOI] [PubMed] [Google Scholar]
- Aranburu A, Ceccarelli S, Giorda E, Lasorella R, Ballatore G, Carsetti R. TLR ligation triggers somatic hypermutation in transitional B cells inducing the generation of IgM memory B cells. J Immunol. 2010;185:7293–7301. doi: 10.4049/jimmunol.1002722. [DOI] [PubMed] [Google Scholar]
- Weller S, Bonnet M, Delagreverie H, Israel L, Chrabieh M, Marodi L, et al. IgM+IgD+CD27+ B cells are markedly reduced in IRAK-4-, MyD88- and TIRAP- but not UNC-93B-deficient patients. Bloode-pub ahead of print 21 September 2012; doi: 10.1182/blood-2012-07-440776 [DOI] [PMC free article] [PubMed]
- Gavin AL, Hoebe K, Duong B, Ota T, Martin C, Beutler B, et al. Adjuvant-enhanced antibody responses in the absence of toll-like receptor signaling. Science. 2006;314:1936–1938. doi: 10.1126/science.1135299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alugupalli KR, Akira S, Lien E, Leong JM. MyD88- and Bruton's tyrosine kinase-mediated signals are essential for T cell-independent pathogen-specific IgM responses. J Immunol. 2007;178:3740–3749. doi: 10.4049/jimmunol.178.6.3740. [DOI] [PubMed] [Google Scholar]
- Hou B, Saudan P, Ott G, Wheeler ML, Ji M, Kuzmich L, et al. Selective utilization of Toll-like receptor and MyD88 signaling in B cells for enhancement of the antiviral germinal center response. Immunity. 2011;34:375–384. doi: 10.1016/j.immuni.2011.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer-Bahlburg A, Khim S, Rawlings DJ. B cell intrinsic TLR signals amplify but are not required for humoral immunity. J Exp Med. 2007;204:3095–3101. doi: 10.1084/jem.20071250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasare C, Medzhitov R. Control of B-cell responses by Toll-like receptors. Nature. 2005;438:364–368. doi: 10.1038/nature04267. [DOI] [PubMed] [Google Scholar]
- Jegerlehner A, Maurer P, Bessa J, Hinton HJ, Kopf M, Bachmann MF. TLR9 signaling in B cells determines class switch recombination to IgG2a. J Immunol. 2007;178:2415–2420. doi: 10.4049/jimmunol.178.4.2415. [DOI] [PubMed] [Google Scholar]
- Lanzavecchia A, Sallusto F. Toll-like receptors and innate immunity in B-cell activation and antibody responses. Curr Opin Immunol. 2007;19:268–274. doi: 10.1016/j.coi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Hou B, Reizis B, DeFranco AL. Toll-like receptors activate innate and adaptive immunity by using dendritic cell-intrinsic and -extrinsic mechanisms. Immunity. 2008;29:272–282. doi: 10.1016/j.immuni.2008.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne EP. Toll-like receptor 7 controls the anti-retroviral germinal center response. PLoS Pathog. 2011;7:e1002293. doi: 10.1371/journal.ppat.1002293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora GD, Nussenzweig MC. Germinal Centers. Annu Rev Immunol. 2012;30:429–457. doi: 10.1146/annurev-immunol-020711-075032. [DOI] [PubMed] [Google Scholar]
- Leadbetter EA, Rifkin IR, Hohlbaum AM, Beaudette BC, Shlomchik MJ, Marshak-Rothstein A. Chromatin-IgG complexes activate B cells by dual engagement of IgM and Toll-like receptors. Nature. 2002;416:603–607. doi: 10.1038/416603a. [DOI] [PubMed] [Google Scholar]
- Green NM, Marshak-Rothstein A. Toll-like receptor driven B cell activation in the induction of systemic autoimmunity. Semin Immunol. 2011;23:106–112. doi: 10.1016/j.smim.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshak-Rothstein A. Toll-like receptors in systemic autoimmune disease. Nat Rev Immunol. 2006;6:823–835. doi: 10.1038/nri1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- William J, Euler C, Christensen S, Shlomchik MJ. Evolution of autoantibody responses via somatic hypermutation outside of germinal centers. Science. 2002;297:2066–2070. doi: 10.1126/science.1073924. [DOI] [PubMed] [Google Scholar]
- Herlands RA, Christensen SR, Sweet RA, Hershberg U, Shlomchik MJ. T cell-independent and toll-like receptor-dependent antigen-driven activation of autoreactive B cells. Immunity. 2008;29:249–260. doi: 10.1016/j.immuni.2008.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers M, Fukuyama H, McGaha TL, Aderem A, Ravetch JV. TLR9/MyD88 signaling is required for class switching to pathogenic IgG2a and 2b autoantibodies in SLE. J Exp Med. 2006;203:553–561. doi: 10.1084/jem.20052438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groom JR, Fletcher CA, Walters SN, Grey ST, Watt SV, Sweet MJ, et al. BAFF and MyD88 signals promote a lupuslike disease independent of T cells. J Exp Med. 2007;204:1959–1971. doi: 10.1084/jem.20062567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker-Herman S, Meyer-Bahlburg A, Schwartz MA, Jackson SW, Hudkins KL, Liu C, et al. WASp-deficient B cells play a critical, cell-intrinsic role in triggering autoimmunity. J Exp Med. 2011;208:2033–2042. doi: 10.1084/jem.20110200. [DOI] [PMC free article] [PubMed] [Google Scholar]