Abstract
AIM
To evaluate differences in flap thickness resulting from use of an Alcon Wavelight FS200 femtosecond laser and a MORIA SBK microkeratome when making a 110-µm-thick corneal flap and to identify the potential factors that affect corneal flap thickness.
METHODS
A prospective case study was performed on 120 eyes of 60 patients who were divided into two groups for LASIK, each group consisting of 60 eyes (30 patients). The corneal flaps were created using an Alcon Wavelight FS200 femtosecond laser or a MORIA SBK microkeratome. The central corneal flap thickness was calculated by subtraction pachymetry. Age, central corneal thickness (CCT), spherical equivalent refraction, mean keratometry, and corneal diameter were recorded preoperatively for analysis.
RESULTS
Cutting of all flaps was easily performed without intraoperative complications. In the Alcon Wavelight FS200 femtosecond laser group, the mean right and left corneal flap thicknesses were 114.0±6.6 µm (range: 98-126) and 111.4±7.6 µm (range: 98-122), respectively. The difference (2.6±9.1 µm) in the corneal flap thickness between the right and left eyes was not significant (t=1.59, P=0.12). Stepwise regression analysis indicated that the resulting corneal flap thickness was unrelated to the patient's age, preoperative CCT, spherical equivalent refraction, mean keratometry, or corneal diameter. In the MORIA SBK microkeratome group, the mean right and left corneal flap thicknesses were 110.6±7.4 µm (range: 97-125 µm) and 108.2±6.1 µm (range: 78-123 µm), respectively. The difference in the corneal flap thickness between the right and left eyes (2.4±6.5µm) was not significant (t=2.039, P=0.0506). The corneal flap thickness was positively correlated with the preoperative CCT through stepwise regression analysis (r=0.297, P=0.021). The corneal flap thickness was not related to age, spherical equivalent refraction, mean keratometry, or corneal diameter. The corneal flap thickness was estimated using the following equation: Tflap=67.77+0.076 CCT (F=5.63, P=0.021).
CONCLUSION
Both the Alcon Wavelight FS200 femtosecond laser and the MORIA SBK microkeratome produced 110-µm-thick corneal flaps. The central corneal flap thickness was positively correlated with the preoperative CCT in MORIA SBK microkeratome surgery.
Keywords: corneal flap thickness, femtosecond laser, laser in situ keratomileusis, microkeratome
INTRODUCTION
Over the past decades, laser in situ keratomileusis (LASIK) has become the most common refractive procedure for the correction of refractive errors[1]-[3]. Creating a successful corneal flap is the first critical procedure during LASIK surgery. Two techniques are used to produce corneal flaps during LASIK surgery: a microkeratome and a femtosecond laser[4],[5]. The consistency and predictability of the corneal flap thickness is crucial in producing successful LASIK outcomes. The corneal flap thickness is directly related to LASIK predictability and safety; therefore, methods that improve the predictability and minimize the degree of variation in corneal flap thickness are worthy of attention[6]-[8]. In this study, we compared the corneal flap thickness resulting from two myopic LASIK surgery procedures, one using an Alcon Wavelight FS200 femtosecond laser and the other using a MORIA SBK microkeratome, in 120 eyes of 60 patients. This study evaluated the predictability and comparability of the corneal flap thickness made by the two methods, which was measured using A-type ultrasonic pachymeter. The average thickness of the corneal flap was recorded, and factors related to corneal flap thickness were evaluated.
SUBJECTS AND METHODS
Subjects
General information
This prospective study included 120 eyes of 60 patients (28 males, 32 females), ranging in age from 18 to 48y. All patients had LASIK surgery between January and March of 2012 at the Ruijin Hospital affiliated with Shanghai Jiaotong University School of Medicine. The corneal flaps were created using an Alcon Wavelight FS200 femtosecond laser or a MORIA SBK microkeratome. Patients were divided into two groups depending on the type of surgery received: femtosecond laser surgery or microkeratome surgery. The patients were equally divided between these two groups, i.e. 30 cases for each surgery type.
Inclusion criteria included the following: age 18-50y, preoperative spherical refraction of -2.00 to -12.00D, refractive cylinder of less than -3.00D, a stable refractive state for 2y, an intraocular pressure (IOP) of <21 mm Hg (where 1 mm Hg=0.133 kPa), and at least 2 or 4wk without soft or hard contact lenses respectively. Exclusion criteria included the following: a history of systemic autoimmune diseases, a history of diabetes, other ophthalmic disorders, a history of ocular trauma, and surgical history.
Methods
Prior approval by ethic committee of Ruijin Hospital (Shanghai Jiaotong University School of Medicine) was obtained according to the Declaration of Helsinki. The participants were informed about the purpose of the study and gave informed consent before inclusion. Patients underwent a full eye examination before LASIK surgery, including evaluations of their uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), IOP, corneal curvature, corneal diameter, corneal thickness, anterior and posterior corneal surface height, corneal topography, refraction and slit-lamp anterior segment, and fundus examination. Preoperative and intraoperative corneal thickness measurements were performed using a DGH 550 A-type ultrasonic pachymeter (DGH). The corneal center point was selected for the measurements. The corneal thickness measurements were performed 10 times, and the mean value was recorded. The data of corneal diameter could be obtained from examining corneal topography with Pentacam.
Patients were divided into two groups based on the type of surgery they received to create the corneal flap: the FS200 femtosecond laser group and the SBK microkeratome group. The femtosecond laser had a bad energy of 0.65 mJ, with a side-cut energy of 0.8 mJ and a repetition frequency of 200 kHz. Myopia stromal ablations were performed using an Allegretto Wave Eye-Q excimer laser (Wavelight Company, Germany). The wavelength and energy intensity of the excimer laser were 193 nm and 180 mJ cm−2, respectively.
The surgery procedure was as follows. Topical anesthesia and 2% propoxyphene tetracaine eye drops were applied, along with routine disinfection and shop towels. An eyelid holder was used to open the eye. A suction ring was applied to the eye to hold it in place and a aluminium cone was moved to contact and fasten to it. Surgery using the femtosecond laser or microkeratome was used to create the corneal flap.
For microkeratome surgery, the pedicle position was set to the nasal pedicle width. The flap was opened with the microkeratome, and the central corneal stromal bed thickness was measured. This was subtracted from the preoperative corneal thickness to calculate the thickness of the corneal flap.
For surgery using the FS200 femtosecond laser, the first measurement of the corneal thickness and the corneal flap design parameters were entered into the computer. The thickness of the corneal flap was set to 110 µm. The pedicle position was set to the nasal pedicle width settings (3.5 mm), and the flap diameter was set to 8.5 mm, with a 70° angled side cut. The suction ring was applied for eye fixation. Once the flap was created and opened, the central corneal stromal bed thickness was measured and compared with the preoperative corneal thickness to calculate the thickness of the corneal flap.
The corneal stroma was then ablated by the excimer laser. The corneal bed was rinsed, and the corneal flap reset. Antibiotic anti-inflammatory saline eye drops were used during recovery.
Statistical Analysis
Levene's test was used to determine the consistency of the preoperative data with a normal distribution. All results showed normal distributions by the Kolmogorov-Smirnov method. Preoperative baseline data were compared using one-way analysis of variance (ANOVA). The corneal flap thickness for the left and right eyes of patients in each group were compared using a paired t -test. The correlation between the corneal flap thickness, flap-creation method, and other relevant factors were analyzed using stepwise regression. The data were analyzed using Microsoft Excel (Microsoft Corp., Redmond, WA, USA) and SPSS Version 11.5 (SPSS Inc., Chicago, IL, USA) statistical software. A P-value of 0.05 was considered statistically significant.
RESULTS
The preoperative characteristics of the patients in both groups are summarized in Table 1.
Table 1. Preoperative demographic baseline characteristics of the two groups of patients.
| Group | Age (a) | Refraction (D) | CT (µm) | CHD (mm) | CC (D) |
| FS200 | 27.9±5.9 | -6.31±2.13 | 552.3±28.8 | 11.68±0.36 | 42.75±2.71 |
| SBK | 28.7±8.0 | -5.83±2.27 | 547.1±26.7 | 11.69±0.32 | 43.50±1.18 |
| F | 0.3826 | 1.2019 | 1.0370 | 0.2145 | 1.980 |
| P | 0.7034 | 0.2318 | 0.3018 | 0.8305 | 0.051 |
(One-way ANOVA). CT: Corneal thickness; CHD: Corneal horizontal diameter; CC: Corneal curvature.
Average Thickness Range of the Corneal Flap Center
FS200 group
The average thickness of the right corneal flap center was 114.0±6.6 µm (range: 98-126 µm). The average thickness of the left cornea flap center was 111.4±7.6 µm (range: 98-122 µm). The binocular average corneal flap thickness was 112.7±7.2 µm. The difference in corneal flap thickness between the eyes was 2.6±9.1 µm, which was not statistically significant (t=1.59, P=0.12). The average thickness of the corneal flap center and the range of corneal flap thickness are given in Tables 2 and 3, respectively.
Table 2. Comparison of corneal flap thickness of FS200 and SBK procedures between bilateral eyes µm.
| Group | Flap thickness value in both eyes |
t | P | |
| Right eyes | Left eyes | |||
| FS200 | 114.0±6.6 | 111.4±7.6 | 1.59 | 0.12 |
| SBK | 110.6±7.4 | 108.2±6.1 | 2.039 | 0.0506 |
(Paired t-test).
Table 3. Variation in corneal flap thickness of FS200 and SBK Moria microkeratome procedures µm.
| Group | Maximum |
Minimum |
Difference | ||
| Right eye | Left eye | Right eye | Left eye | ||
| FS200 | 126 | 122 | 98 | 98 | 28 |
| SBK | 125 | 123 | 97 | 98 | 28 |
Group SBK
The average thickness of the right corneal flap center was 110.6±7.4 µm (range: 97-125 µm). The average thickness of the left cornea flap center was 108.2±6.1 µm (range: 98-123 µm). The average corneal flap thickness was 109.4±6.8 µm. The difference in corneal flap thickness between eyes was 2.4±6.5 µm, which was not statistically significant (t=2.039, P=0.0506). The average thickness of the corneal flap center and the range of corneal flap thickness are given in Tables 2 and 3, respectively.
Stepwise Regression and Correlation Analysis
FS200 corneal flap thickness and factor analysis
Stepwise regression revealed that factors including the pre-operative corneal thickness, age, curvature, corneal diameter, diameter of the corneal flap, and refraction were unrelated to thickness of the corneal flap.
SBK corneal flap thickness and factor analysis
In stepwise regression analysis of the SBK corneal flap thickness, only the pre-operative corneal thickness significantly predicted corneal flap thickness; age, curvature, corneal diameter, and diameter of the corneal flap were unrelated. The resulting equation was as follows: Tflap=67.77+0.076 CCT (F=5.63, P=0.021). Correlation analysis showed that the corneal flap thickness and the pre-operative corneal thickness were positively correlated (r=0. 297, P=0.021) (Figure 1).
Figure 1. Correlation analysis of the corneal thickness (µm) and corneal flap thickness (µm) using SBK microkeratome surgery.
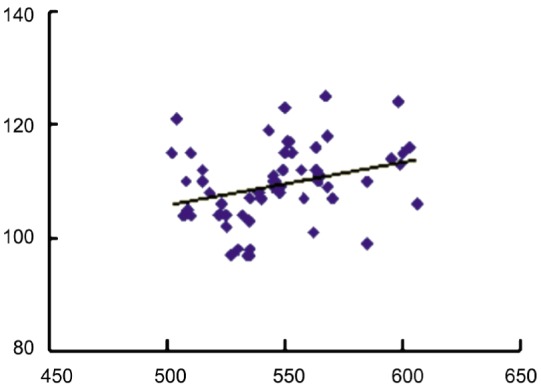
(r=0.297, P=0.021; stepwise regression).
DISCUSSION
Production of a moderate-sized corneal flap with uniform thickness is important during LASIK surgery. In recent years, there has been a tendency to create thinner corneal flaps ranged from 100 to110 µm[9]-[11]. The thin corneal flap has the advantage of preserving more of the corneal stroma, which avoids the onset of ectasia after surgery, and it also allows for treatment of a relatively high degree of myopia. At present, there are two methods used to produce the thin corneal flap; one method uses a femtosecond laser, and the other uses a microkeratome. Each approach has advantages and disadvantages.
The femtosecond laser corneal flap has the advantage of producing a corneal flap in which the thickness is thin and uniform, the flap diameter is adjustable, the pedicle position width and side cut angle can be arbitrarily set, and there are relatively few complications. The disadvantages to this technique are the high cost of surgery, the development of bubbles during the procedure in the corneal layer and anterior chamber, which may affect pupil tracking, and the requirement of a slightly longer suction time (20-30s) which may cause damage to the retina[12],[13].
Microkeratome corneal flap surgery has the advantage of low cost, short suction times (<10s), and the absence of bubbles in the anterior corneal layer. However, the disadvantages include poor corneal flap thickness uniformity, greater variation in thickness, and the inability to arbitrarily set the flap diameter, pedicle location, pedicle width, or side cut angle, which may increase the risk of epithelial cell ingrowth and the probability of complications associated with the corneal flap such as irregularities, astigmatism, buttonholes, and free caps[14].
Several articles have examined the femtosecond laser versus mechanical microkeratome in creating thin corneal flaps. Gil-Cazorla et al[15] compared the Intralase FS60 with MORIA M2 microkeratome flap creation. Although, there was no difference in safety, the refractive outcomes with FS60 were better at 3mo after surgery. The previous two studies also used an Intralase FS60 femtosecond laser and a MORIA M2 microkeratome to do a comparison using an anterior section OCT examination[16],[17]. In 1440 measurements points of 72 eyes, the maximum error for the femtosecond laser and microkeratome were 7 µm and 26 µm, respectively, a difference of nearly 20 µm. With the femtosecond laser, the thickness varied by 0.42%, whereas with the microkeratome, it varied by 15%. Thus, femtosecond laser flap creation was more uniform and accurate. Cummings' study provided an evidence of the predictability and lower variability of LASIK flaps created using a 200 kHz femtosecond laser[18].
Chen et al[19] performed a meta-analysis with an Intralase femtosecond laser and mechanical microkeratome. No difference was observed in the safety or efficacy of the two techniques; however, the corneal flap thickness was more predictable with the femtosecond laser and might induce fewer aberrations[20]-[22]. Although many corneal epithelial cells were damaged by the microkeratome during the operation, there were no statistically significant difference in dry-eye between a microkeratome and a femtosecond laser[23]; however, more diffuse lamellar keratitis (DLK) and corneal haze occurred after femtosecond laser-assisted LASIK[24]-[26].
In this study, for both the FS200 and SBK groups, the differences in the average thickness of the cornea flap center, the binocular average corneal flap thickness, and the corneal flap thickness between eyes were not statistically significant. Both methods produced 110-µm-thick corneal flaps, and both methods were safe and effective, without significant complications after surgery. However, the results of the study have some limitations. Only the central corneal flap thickness was measured and not the peripheral corneal flap thickness. Because the measurement of corneal stromal bed thickness was carried out during surgery, we could not measure the number of points. If we did it would inevitably bring the risk of infection. Von Jagow and Kohnen[27] reported that the thickness of the flaps produced by the Intralase femtosecond laser and Zyoptix XP microkeratome were not significantly different from anterior segment OCT measurements of the corneal flap thickness at various points. However, measurements of the peripheral corneal flap thickness found that the femtosecond laser was more accurate and more predictable.
Kim et al[28] analyzed the impact of various factors on the femtosecond laser corneal flap thickness including the patient's age, refractive error, corneal curvature, and central corneal thickness. However, the results indicated that these parameters were not related to flap thickness. Measurements of the radial area 1.5 mm from the cornea's center were more accurate than were those in the peripheral areas, at a 3-4 mm radius.
In the present study, following FS200 surgery, correlational analysis showed that corneal flap thickness was not related to the preoperative corneal flap thickness, age, refractive error, corneal thickness, curvature, diameter, or flap diameter. However, correlation analysis on the SBK results indicated that corneal flap thickness was positively associated with preoperative corneal thickness (r=0.297, P=0.021), although age, preoperative spherical-equivalent refraction, corneal curvature, diameter, and flap diameter were unrelated to clap thickness. Thus, preoperative corneal thickness must be considered before microkeratome surgery, but this is not a concern for femtosecond laser-assisted LASIK[4].
In conclusion, the introduction of femtosecond lasers for the production of corneal flaps has brought significant improvement to the accuracy of corneal flap production. Vaddavalli and Yoo[29] summarized this by stating that the femtosecond laser was capable of creating uniform, predictable corneal flaps that could be personalized in design; additionally, the side-cut angle could be varied at the operator's discretion. Obvious advantages were that thicker flaps resulted in decreased stromal-bed thickness, which increased the risk for interlayer cloudiness and iatrogenic corneal ectasia. Therefore, patients should be carefully evaluated for proper design of the corneal flap to minimize post-operative complications and the need for additional surgery.
Acknowledgments
Conflicts of Interest: Zhang J, None; Zhang SS, None; Yu Q, None; Wu JX, None; Lian JC, None.
REFERENCES
- 1.Solomon KD, Fernández de Castro LE, Sandoval HP, Biber JM, Groat B, Neff KD, Ying MS, French JW, Donnenfeld ED, Lindstrom RL, Joint LASIK study task force LASIK world literature review: quality of life and patient satisfaction. Ophthalmology. 2009;116(4):691–701. doi: 10.1016/j.ophtha.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 2.Carr JD, Stulting RD, Thompson KP, Waring GO., 3rd Laser in situ keratomileusis: surgical technique. Ophthalmol Clin North Am. 2001;14(2):285–294. [PubMed] [Google Scholar]
- 3.Sugar A, Rapuano CJ, Culbertson WW, Huang D, Varley GA, Agapitos PJ, de Luise VP, Koch DD. Laser in situ keratomileusis for myopia and astigmatism: safety and efficacy: a report by the American academy of ophthalmology. Ophthalmology. 2002;109(1):175–187. doi: 10.1016/s0161-6420(01)00966-6. [DOI] [PubMed] [Google Scholar]
- 4.Salomão MQ, Ambrósio R, Jr, Wilson SE. Dry eye associated with laser in situ keratomileusis: mechanical microkeratome versus femtosecond laser. J Cataract Refract Surg. 2009;35(10):1756–1760. doi: 10.1016/j.jcrs.2009.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanna M, Schallhorn SC, Hettinger KA. Femtosecond laser versus mechanical microkeratome: a retrospective comparison of visual outcomes at 3mo. J Refract Surg. 2009;25(7):668–671. doi: 10.3928/1081597X-20090611-08. [DOI] [PubMed] [Google Scholar]
- 6.Hsu SY, Chen HY, Chung CP. Analysis of actual corneal flap thickness and confounding factors between first and second operated eyes. Ophthalmic Surg Lasers Imag. 2009;40(5):448–452. doi: 10.3928/15428877-20090901-02. [DOI] [PubMed] [Google Scholar]
- 7.Zhou Y, Zhang J, Tian L, Zhai C. Comparison of the Ziemer FEMTO LDV femtosecond laser and Moria M2 mechanical microkeratome. J Refract Surg. 2012;28(3):189–194. doi: 10.3928/1081597X-20120208-01. [DOI] [PubMed] [Google Scholar]
- 8.Ortiz D, Alió JL, Piñero D. Measurement of corneal curvature change after mechanical laser in situ keratomileusis flap creation and femtosecond laser flap creation. J Cataract Refract Surg. 2008;34(2):238–242. doi: 10.1016/j.jcrs.2007.09.023. [DOI] [PubMed] [Google Scholar]
- 9.Slade SG, Durrie DS, Binder PS. A prospective, contralateral eye study comparing thin-flap LASIK (sub-Bowman keratomileusis) with photorefractive keratectomy. Ophthalmology. 2009;116(6):1075–1082. doi: 10.1016/j.ophtha.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Salomão MQ, Wilson SE. Femtosecond laser in laser in situ keratomileusis. J Cataract Refract Surg. 2010;36(6):1024–1032. doi: 10.1016/j.jcrs.2010.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slade SG. The use of the femtosecond laser in the customization of corneal flaps in laser in situ keratomileusis. Curr Opin Ophthalmol. 2007;18(4):314–317. doi: 10.1097/ICU.0b013e3281bd88a0. [DOI] [PubMed] [Google Scholar]
- 12.Slade SG. Thin-flap laser-assisted in situ keratomileusis. Curr Opin Ophthalmol. 2008;19(4):325–329. doi: 10.1097/ICU.0b013e328302cc77. [DOI] [PubMed] [Google Scholar]
- 13.Barequet IS, Hirsh A, Levinger S. Effect of thin femtosecond LASIK flaps on corneal sensitivity and tear function. J Refract Surg. 2008;24(9):897–902. doi: 10.3928/1081597X-20081101-08. [DOI] [PubMed] [Google Scholar]
- 14.Kymionis GD, Portaliou DM, Tsiklis NS, Panagopoulou SI, Pallikaris IG. Thin LASIK flap creation using the SCHWIND Carriazo-Pendular microkeratome. J Refract Surg. 2009;25(1):33–36. doi: 10.3928/1081597X-20090101-06. [DOI] [PubMed] [Google Scholar]
- 15.Gil-Cazorla R, Teus MA, de Benito-Llopis L, Mikropoulos DG. Femtosecond laser vs mechanical microkeratome for hyperopic laser in situ keratomileusis. Am J Ophthalmol. 2011;152(1):16–21. doi: 10.1016/j.ajo.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 16.Zhou Y, Tian L, Wang N, Dougherty PJ. Anterior segment optical coherence tomography measurement of LASIK flaps: femtosecond laser vs microkeratome. J Refract Surg. 2011;27(6):408–416. doi: 10.3928/1081597X-20101029-01. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Y, Chen YG, Xia YJ. Comparison of corneal flap morphology using AS-OCT in LASIK with the WaveLight FS200 femtosecond laser versus a mechanical microkeratome. J Refract Surg. 2013;29(5):320–324. doi: 10.3928/1081597X-20130415-03. [DOI] [PubMed] [Google Scholar]
- 18.Cummings AB, Cummings BK, Kelly GE. Predictability of corneal flap thickness in laser in situ keratomileusis using a 200 kHz femtosecond laser. J Cataract Refract Surg. 2013;39(3):378–385. doi: 10.1016/j.jcrs.2012.10.041. [DOI] [PubMed] [Google Scholar]
- 19.Chen S, Feng Y, Stojanovic A, Jankov MR, 2nd, Wang Q. IntraLase femtosecond laser vs mechanical microkeratomes in LASIK for myopia: a systematic review and meta-analysis. J Refract Surg. 2012;28(1):15–24. doi: 10.3928/1081597X-20111228-02. [DOI] [PubMed] [Google Scholar]
- 20.Zhang ZH, Jin HY, Suo Y, Patel SV, Montés-Micó R, Manche EE, Xu X. Femtosecond laser versus mechanical microkeratome laser in situ keratomileusis for myopia: metaanalysis of randomized controlled trials. J Cataract Refract Surg. 2011;37(12):2151–2159. doi: 10.1016/j.jcrs.2011.05.043. [DOI] [PubMed] [Google Scholar]
- 21.Montés-Micó R, Rodríguez-Galietero A, Alió JL. Femtosecond laser versus mechanical keratome LASIK for myopia. Ophthalmology. 2007;114(1):62–68. doi: 10.1016/j.ophtha.2006.07.019. [DOI] [PubMed] [Google Scholar]
- 22.Li H, Sun T, Wang M, Zhao J. Safety and effectiveness of thin-flap LASIK using a femtosecond laser and microkeratome in the correction of high myopia in Chinese patients. J Refract Surg. 2010;26(2):99–106. doi: 10.3928/1081597X-20100121-05. [DOI] [PubMed] [Google Scholar]
- 23.Golas L, Manche EE. Dry eye after laser in situ keratomileusis with femtosecond laser and mechanical keratome. J Cataract Refract Surg. 2011;37(8):1476–1480. doi: 10.1016/j.jcrs.2011.03.035. [DOI] [PubMed] [Google Scholar]
- 24.Moshirfar M, Gardiner JP, Schliesser JA, Espandar L, Feiz V, Mifflin MD, Chang JC. Laser in situ keratomileusis flap complications using mechanical microkeratome versus femtosecond laser: retrospective comparison. J Cataract Refract Surg. 2010;36(11):1925–1933. doi: 10.1016/j.jcrs.2010.05.027. [DOI] [PubMed] [Google Scholar]
- 25.Haft P, Yoo SH, Kymionis GD, Ide T, O'Brien TP, Culbertson WW. Complications of LASIK flaps made by the IntraLase 15- and 30-kHz femtosecond lasers. J Refract Surg. 2009;25(11):979–984. doi: 10.3928/1081597X-20091016-02. [DOI] [PubMed] [Google Scholar]
- 26.Ibrahim AI, Sharif KW. Evaluation of haze formation after thin-flap microkeratome LASIK for myopia. J Refract Surg. 2012;28(11):749–750. doi: 10.3928/1081597X-20121011-10. [DOI] [PubMed] [Google Scholar]
- 27.Von Jagow B, Kohnen T. Corneal architecture of femtosecond laser and microkeratome flaps imaged by anterior segment optical coherence tomography. J Cataract Refract Surg. 2009;35(1):35–41. doi: 10.1016/j.jcrs.2008.09.013. [DOI] [PubMed] [Google Scholar]
- 28.Kim CY, Song JH, Na KS, Chung SH, Joo CK. Factors influencing corneal flap thickness in laser in situ keratomileusis with a femtosecond laser. Korean J Ophthalmol. 2011;25(1):8–14. doi: 10.3341/kjo.2011.25.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vaddavalli PK, Yoo SH. Femtosecond laser in-situ keratomileusis flap configurations. Curr Opin Ophthalmol. 2011;22(4):245–250. doi: 10.1097/ICU.0b013e3283479ebd. [DOI] [PubMed] [Google Scholar]


