Abstract
Aim:
To evaluate single-dose and multiple-dose pharmacokinetics of panaxatrol disuccinate sodium in healthy volunteers and patients with advanced solid tumors.
Methods:
In the single-dose pharmacokinetic study, 27 healthy volunteers received panaxatrol disuccinate sodium in three doses (70, 100, and 140 mg·m−2). In the multiple-dose pharmacokinetic study, Panaxatrol disuccinate sodium was administered to 8 patients at 100 mg·m−2 daily in a 30-day continuous intravenous injection. Determination of the panaxatrol disuccinate sodium plasma concentration was performed by an LC-MS method. The pharmacokinetic analysis system — Drug and Statistics (DAS) — was applied to assess plasma panaxatrol disuccinate sodium concentration-time data.
Results:
After a single intravenous dose of 70, 100, or 140 mg·m−2 was administered to subjects, panaxatrol disuccinate sodium distributed broadly, and the plasma concentration of panaxatrol disuccinate sodium declined rapidly. No significant differences were observed in the main pharmacokinetic parameters among the three dosing groups, including AUC0–t, MRT0–t, VRT0–t, t1/2Z, CLz/F, Vz/F, and C0 (P>0.05). In the multiple-dose pharmacokinetic study, the mean steady-state peak concentration (Cmax), trough concentration (Cmin), average concentration (Cav), mean steady state AUC (AUCss) and the degree of fluctuation were 13.96±15.48 mg·L−1, 0.18±0.29 mg·L−1, 0.15±0.29 mg·L−1, 3.58±6.94 mg·L−1·h, and 148.00±117.18, respectively. At any given dose of panaxatrol disuccinate sodium, interindividual variability in the pharmacokinetic parameters was obvious.
Conclusion:
The effect of the dose level on single-dose pharmacokinetics of panaxatrol disuccinate sodium was not significant. No accumulation was observed with exposure to 100 mg·m−2 panaxatrol disuccinate sodium in the 30-day continuous intravenous injection. All subjects were evaluated for tolerability throughout the study. Thus, the phase II dose of panaxatrol disuccinate sodium may be considered to be 100 mg·m−2 for a 30-day continuous intravenous injection to treat patients with advanced solid tumors.
Keywords: panaxatrol disuccinate sodium, pharmacokinetics, liquid chromatography-mass spectrometry, anti-cancer
Introduction
Ginseng has long been known to be multifunctional as both a tonic and a sedative agent. Ginsenosides, the main bioactive components of Ginseng, have become a major focus in cancer research.
Based on the properties of different sapogenins, ginsenosides are divided into 3 groups, 20(S)-protopanaxadiol, 20(S)-protopanaxatriol and oleanolic acid glycoside. Many ginsenosides have been found to have anti-cancer activity1 and are involved in several anti-cancer mechanisms, such as inhibition of cell proliferation2, invasion3, induction of cell apoptosis4 and anti-angiogenesis5. However, the antitumor mechanism of ginsenoside is not fully clear. Nakata H et al reported that ginsenoside Rh2 inhibited the growth of human ovarian cancer cells cultured in nude mice6. Quasipanaxatriol may reverse daunomycin resistance in P388/ADM cells by effectively blocking daunomycin efflux, leading to the accumulation of the drug in the cells7. Ginsenoside has been implicated in several signaling pathways, such as MAPK8, caspase9, NF-kappaB, and JNK pathways10. Furthermore, ginsenoside Rg3 (“Shenyi” Capsule) has shown effects on improving body immunity, decreasing toxic effects induced by chemotherapy and increasing sensitivity to chemotherapy11. Recently, ginsenoside Rg3 has been produced as an anti-angiogenic and anti-cancer drug in China. Despite the prosperity of mechanistic research, current literature shows limited data on the pharmacokinetics of ginsenoside in biological systems. Pang reported the first pharmacokinetic study of ginsenoside Rg3 in humans, which was performed by an HPLC–UV method12. The results showed that Rg3 had low bioavailability after oral administration. Xie presented a report mainly concerning the development of a liquid chromatography/mass spectrometry (LC/MS) method using solid-phase extraction for a pharmacokinetic study of Rg3 and its metabolites in rats13. Recently, a pharmacokinetic study of ginsenoside Rh2 in rats and dogs showed that Rh2 distributed mainly to the liver and gastrointestinal tissues in rats after oral dosing, and multiple dosing (7 days, 1 mg/kg bid) did not affect its pharmacokinetics in dogs14.
San-chi Ginseng (P notoginseng Burk), grown in Yunnan Province in China, has also been used for similar purposes. The major bioactive saponins of Panax notoginseng (PNS) are ginsenoside Rg1, ginsenoside Rb1, notoginsenoside R1 and notoginsenoside R2. The content of ginsenoside in PNS is 50% higher than that in ginseng. Many studies have shown that PNS extracts have anti-cancer activity1, 15.
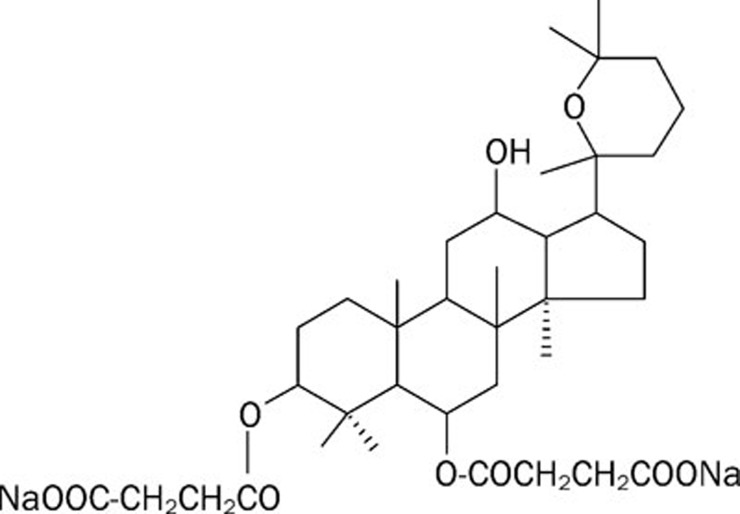
Panaxatrol disuccinate sodium (Figure 1), a notoginsenoside derivative, has been newly synthesized by Kunming Medical College and Kunming Pharmaceuticals Ltd. Preclinical pharmacologic and toxicologic studies have indicated that this dammarane-type tetracyclic triterpenoid saponin effectively inhibited the growth of nude mice xenografts and improved animal immunity. Further study has shown that panaxatrol disuccinate sodium induces minimal toxic effects even with long-term application. The antitumor activities and minimal toxic effects observed in preclinical trials indicate the need to initiate clinical trials of panaxatrol disuccinate sodium in human subjects. Thus, a pharmacokinetic study on panaxatrol disuccinate sodium was initiated by the Tianjin Medical University Cancer Institute and Hospital.
Figure 1.
Chemical structure of panaxatrol disuccinate sodium.
The aim of this study was to determine the pharmacokinetic profile of panaxatrol disuccinate sodium in healthy volunteers and patients with advanced solid tumors and to observe its toxicity as well as the tolerability of the subjects after panaxatrol disuccinate sodium administration.
Materials and methods
Drug and reagents
Panaxatrol disuccinate sodium for injection and panaxatrol disuccinate sodium standard were obtained from Tianzhijiao Life Science and Technology, Ltd (Guangdong, China). The panaxatrol disuccinate sodium for injection was made as a freeze-dried powder. Each vial contained 25 mg of panaxatrol disuccinate sodium powder. Indapamide standard was obtained from National Institution for the Control of Pharmaceutical and Biological Products (Beijing, China). Acetonitrile was an HPLC-grade reagent and was purchased from Concord Technology Co Ltd (Tianjin, China). HPLC-grade water was prepared in a Milli-Q system (Millipore Corporation Billerica, Massachusetts, USA). All other reagents were analytical grade.
Instruments
The instrument system consisted of a LCMS-2010A Liquid Chromatograph-Mass Spectrometer with electrospray ionization (ESI), an LCMS Solution 3.0 data processing system (Shimadzu Corporation, Kyoto, Japan), a C18 column (150×2.0 mm, 5 μm, Shimadzu Corporation, Kyoto, Japan) and a RTX-5MS capillary column (30 m×0.25 mm, id×0.25 μm, Restek).
Selection of healthy volunteers and patients
The study was approved by the Ethics Committee at Tianjin Medical University Cancer Institute and Hospital. All subjects were informed about the program of the study and signed informed consent forms before entering the study. Healthy volunteers in the single-dose pharmacokinetic study were required to meet the following criteria: normal function in all organs of the body; no drug administration for 2 weeks before participating in the study; good living habits; no cigarette or alcohol consumption allowed during the entire treatment period; and good compliance. Patients who had solid tumors confirmed after histologic examination that had proven intractable to standard therapy (or no standard therapy applied) were eligible for the multiple-dose pharmacokinetic study. The patients had not received any chemotherapy, biotherapy, radiotherapy or had an operation for 4 weeks before participating in the study. Other inclusion criteria were as follows: age of 18–70 years; Karnofsky performance status scale ≥70; survival expectancy over 3 months; efficient bone marrow function (WBC count ≥3.0×109/L, absolute neutrophil count≥1.5×109/L, platelet count ≥100.0×109/L, hemoglobin ≥100.0 g/L); efficient renal function (serum creatine ≤1.5×the upper limit of normal[ULN]); efficient hepatic function (ALT, AST and total bilirubin level ≤1.5×ULN); and no obvious cardiac, pneumonic, or psychiatric disorders. Patients with an active infection, hemorrhagic diathesis, serious brain tumor, or brain metastases were excluded from the study. All patients who could possibly become pregnant were required to use adequate contraception during the entire study.
Study design
The study was designed as an open-label, dose escalation study. Preclinical pharmacology studies demonstrated that panaxatrol disuccinate sodium was effective against cancer cells over a broad dose range. Based on the outcomes of preclinical pharmacological and toxicological studies, the initial dose of panaxatrol disuccinate sodium for the single-dose pharmacokinetic study was 70 mg·m−2. The dosage was sequentially increased twice to 100 mg·m−2 and 140 mg·m−2. In the multiple-dose pharmacokinetic study, eight patients were enrolled. Patients were continuously given a dose of 100 mg·m−2 daily through intravenous injection for 30 days.
Pharmacokinetic sample collection
Single-dose pharmacokinetic blood samples (5 mL) were taken respectively 10 min before drug injection and immediately after drug injection. In addition, blood samples were taken respectively 5 min, 10 min, 15 min, 30 min, 1 h, 2 h, 4 h, 8 h, and 12 h after drug injection. In the multiple-dose pharmacokinetic study, on the 1st and 30th days, blood samples (5 mL each time) were collected 10 min before drug injection and 5 min, 10 min, 15 min, 30 min, 1 h, 2 h, 4 h, 8 h, and 12 h after the injection. On the 2nd, 3rd, and 4th days, blood specimens (5 mL) were taken 10 min before drug injection and after injection. Blood samples were collected in heparinization tubes and then centrifuged at 3000 rpm (4 °C) for 10 min to obtain plasma, which was stored at -80 °C for determination.
Chromatographic conditions
The mobile phase consisted of acetonitrile: 10 mmol/L ammonium acetate (55:45, v/v), pH 6.5, pumped at a flow rate of 0.3 mL·min−1. The column temperature was set at 40 °C. During the analysis, 10 μL of sample was injected by the autosampler and carried to the analysis column.
Mass spectrometer conditions
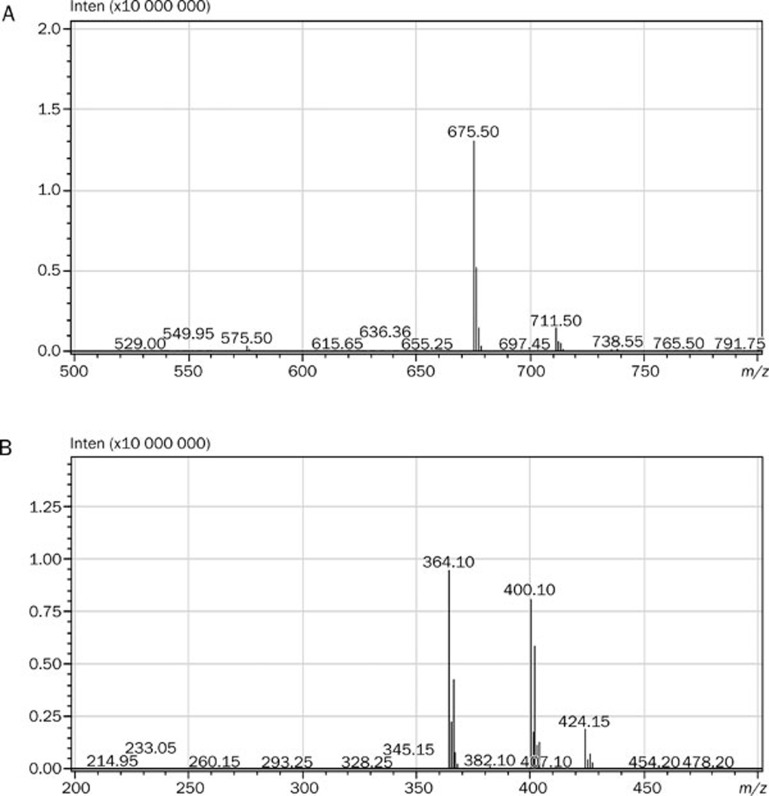
The LCMS-2010A Liquid Chromatograph-Mass Spectrometer was operated in negative ion mode. It was operated with a voltage at 1.50 kV, a heat block temperature of 200 °C and a nebulized gas (nitrogen, N2) flow rate of 1.5 L·min−1. Quantitative analysis was performed in SIM mode. The mass spectrometer was tuned to monitor m/z 675.50 for panaxatrol disuccinate sodium and m/z 364.10 for indapamide. The production mass spectra of panaxatrol disuccinate sodium and indapamide are presented in Figure 2. Quantitation calculations were performed using the internal standard method using LCMS solution, Ver 3.0 (Shimadzu) as the analytical software.
Figure 2.
(A) Production of mass spectra of panaxatrol disuccinate sodium. (B) Production of mass spectra of indapamide.
Stock solutions, calibration standards, and quality control samples preparation
Stock solution of panaxatrol disuccinate sodium at a concentration of 1.013 mg/mL was prepared in methanol. Working solutions of panaxatrol disuccinate sodium were prepared by serially diluting the stock solution with methanol. The internal standard (indapamide) solution at a concentration of 414.4 μg/mL was prepared in methanol and was further diluted with methanol to obtain a concentration of 4.144 μg/mL. Serial calibration standards at concentrations of 0.03039, 0.1013, 0.2026, 5.065, 10.13, 20.26, 50.65, and 101.3 μg/mL were prepared by adding 50 μL of appropriate working solutions to 1 mL of blank plasma. The calibration curves were established by determining the peak area ratio [panaxatrol disuccinate sodium/internal standard (Y) versus panaxatrol disuccinate sodium concentration (X)]. Quality control samples were prepared in the same way to obtain concentrations of 0.1013 μg/mL (low), 10.13 μg/mL(medium) and 50.65 μg/mL (high).
Blood sample processing
All frozen plasma samples were thawed at room temperature. For sample extraction, 1.0 mL of sample was added into a 10 mL centrifuge tube, and 0.2 mL of 10% phosphoric acid and 25 μL of the 4.144 μg/mL internal standard solution were added. After vortex mixing for 30 s, 5 mL of acetic ether was added to the mixture. After vortex mixing for 3 min, the mixture was centrifuged at 5000 r/min for 10 min, and then 4 mL of the organic phase was placed into another centrifuge tube and evaporated to dryness under a stream of nitrogen. The residue was reconstituted in 100 μL of the mobile phase. The mixture was centrifuged at 13000 r/min for 15 min, and 10 μL of the supernatant was injected into the LC-MS system.
Sensitivity
The low limit of quantification (LLOQ) values were measured using a series of diluted standard plasma samples. For the concentration to be accepted as the LLOQ, the signal-to-noise ratio had to be greater than or equal to 3, and the percent deviation for the analyte concentration and the relative standard deviation had to be within 20%.
Precision and accuracy
Batches of quality control (QC) samples were analyzed on three different days to validate the method. In each batch, QC samples were assayed in sets of five replicates to evaluate the accuracy and intra- and interday precision. The accuracy (relative recovery) was determined by comparing the concentration calculated from the calibration curve to the known concentration.
Extraction recovery
Extraction recovery of panaxatrol disuccinate sodium and the internal standard was determined by comparing the absolute peak areas of the QC samples in human plasma before extraction to blank plasma extracted in the same manner then spiked post-extraction with the same concentration of panaxatrol disuccinate sodium and the internal standard.
Stability
Sample stability was assessed by serial experiments, including processed sample stability, unprocessed sample stability, frozen sample stability and freeze-thaw stability.
Pharmacokinetic data analysis and statistical analysis
The plasma concentration-time data were analyzed using noncompartmental methods. The pharmacokinetic analysis system—DAS 2.1(Anhui, China)—was applied to assess pharmacokinetic parameters. The peak plasma concentration (Cmax) and time to peak plasma concentration (Tmax) were obtained by experimental observations. The elimination half-life (t1/2) was calculated as 0.693×mean retention time (MRT). The AUC from zero to infinity (AUC0–∞) was equivalent to the sum of the areas from time zero to the time of the last measured concentration, calculated using the linear trapezoidal method (until Cmax), the log-trapezoidal method (until the last measurable concentration), and the extrapolated area. The extrapolated area was determined by dividing the final measured concentration by the slope of the terminal log-linear phase. Trough values on days 2, 3, and 4 were averaged on each day for each dose level. All statistical tests were 2-tailed and significance was set at the 0.05 level. Differences in the mean values of physical examinations and pharmacokinetic parameters among the three groups were compared by analysis of variance (ANOVA) or Kruskal-Wallis test (K–W H test). For differences between two groups, t-test or Wilcoxon's test was employed.
Results
Representative chromatogram and validation of the analytical method
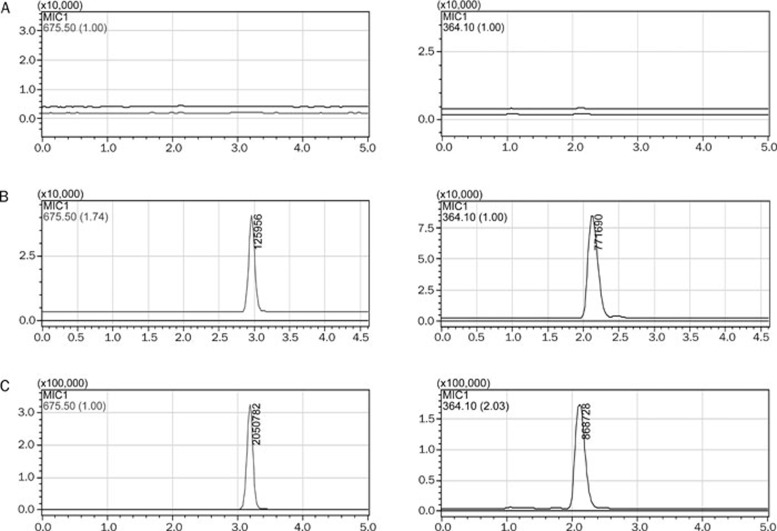
Representative chromatograms of a control blank sample, a standard sample containing 20.26 and 4.144 μg/mL internal standard, and a subject sample are shown in Figures 3A–3C, respectively. Panaxatrol disuccinate sodium and the internal standard in plasma were completely separated without significant interference. The retention times of panaxatrol disuccinate sodium and the internal standard were 3.0 min and 2.1 min, respectively.
Figure 3.
(A) Representative chromatogram of control blank plasma. (B) Representative chromatogram of a standard sample containing 20.26 μg/mL panaxatrol disuccinate sodium and 4.144 μg/mL internal standard. (C) Representative chromatogram of a subject sample collected 30 min after administration of 70 mg·m−2 panaxatrol disuccinate sodium.
The calibration curve is linear over the concentration range from 0.03039 μg/mL to 101.3 μg/mL. The equation of calibration curve is Y=0.08444X+0.03585 (r=0.9998, n=5). The LLOQ is 0.03039 μg/mL.
The precision and accuracy results are presented in Table 1. The relative standard deviation of the method was less than 8.0%. Extraction recoveries for three gradient concentrations of panaxatrol disuccinate sodium were 58.47%±6.49%, 64.06%±2.94% and 55.51%±7.25%, respectively. Extraction recovery for internal standard was 73.66%±7.0%. Panaxatrol disuccinate sodium was stable in human plasma after two freeze-thaw cycles, at room temperature for 2 h and at −80 °C for 40 days prior to extraction. Panaxatrol disuccinate sodium was also stable in processed samples at room temperature for 24 h. The differences between stored and freshly prepared solutions were within 15%.
Table 1. Precision and accuracy (n=5).
| Concerntration (μg/mL) | Presion, RSD% |
Accuracy |
||
|---|---|---|---|---|
| Intra-day | Inter-day | Mean/% | RSD/% | |
| 0.1013 | 7.26 | 7.23 | 99.58 | 7.26 |
| 10.13 | 2.96 | 5.50 | 104.92 | 2.96 |
| 50.65 | 2.91 | 2.94 | 94.85 | 2.91 |
Subject characteristic
Thirty-five individuals were enrolled in this pharmacokinetic study in which twenty-seven healthy volunteers and eight patients were studied for the single-dose pharmacokinetic study and multiple-dose pharmacokinetic study, respectively. The characteristics of healthy volunteers and patients and planned dose levels are shown in Table 2. All healthy subjects had normal physical and laboratory examinations. No statistically significant differences were found in age, height, weight, body surface area and BMI among the 3 groups via analysis of variance (ANOVA). The mean age of the 8 patients was 53.4±8.1 years. There were 3 male and 5 female patients, all of whom had Karnofsky performance status scores ≥70. Three patients had non-Hodgkin lymphoma, two had non-small-cell lung cancer, and one each had hepatoma, malignant melanoma and testis carcinoma.
Table 2. Subjects characteristics. Data are expressed as Mean±SD.
| Single dose | Multiple-dose | |||
|---|---|---|---|---|
| 70 mg·m−2 (n=8) | 100 mg·m−2 (n=14) | 140 mg·m−2 (n=5) | 100 mg·m−2 (n=8) | |
| Sex | ||||
| Male | 3 | 8 | 4 | 3 |
| Female | 5 | 6 | 1 | 5 |
| Age (years) | 42.1±12.7 | 47.4±12.5 | 34.2±15.2 | 53.4±8.1 |
| Height (cm) | 165±5 | 170±6 | 164±4 | 168±5 |
| Weight (kg) | 60.6±5.2 | 69.8±8.8 | 54.6±6.7 | 73.1±9.5 |
| Body surface area (m2) | 1.65±0.10 | 1.78±0.12 | 1.57±0.09 | 1.81±0.13 |
| BMI (kg·m−2) | 22.3±0.7 | 24.3±2.8 | 20.4±2.7 | 25.9±2.6 |
Single-dose pharmacokinetics in healthy volunteers
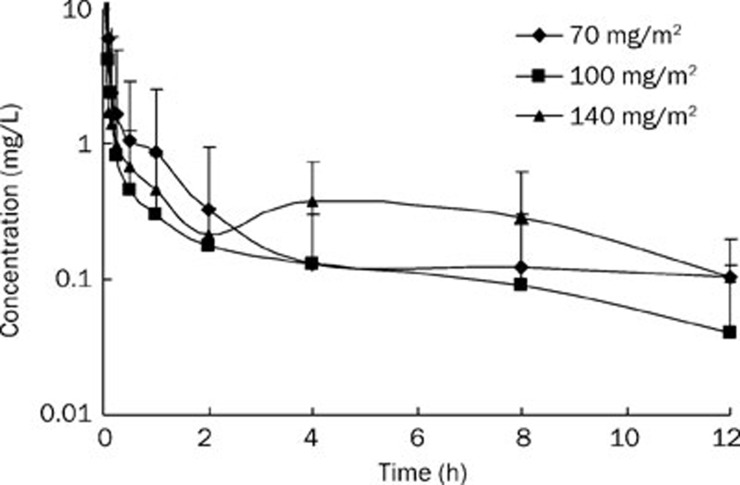
Mean plasma concentration-time profiles of the healthy volunteers at each dose level are shown in Figure 4. The main pharmacokinetic variables are summarized in Table 3. Following a single intravenous dose of 70 mg·m−2, 100 mg·m−2 or 140 mg·m−2 in healthy volunteers, panaxatrol disuccinate sodium distributed broadly, and the plasma concentration declined rapidly after the injection. No significant differences were observed in the main pharmacokinetic parameters among the three dosing groups (P>0.05).
Figure 4.
Mean logarithmic concentration versus time plot after administration of 70 mg·m−2 (♦, n=8), 100 mg·m−2 (▪, n=14) or 140 mg·m−2 (▴, n=5) panaxatrol disuccinate sodium intravenously.
Table 3. Single dose pharmacokinetics parameters of the three dose level groups. Data are expressed as Mean±SD. aP>0.05 vs 70 mg·m−2 group. dP>0.05 vs 100 mg·m−2 group.
| Parameters | Dose lever (mg·m−2) | P | ||
|---|---|---|---|---|
| 70 (n=8) | 100 (n=14) | 140 (n=5) | ||
| C0/mg·L−1 | 27.32±24.75 | 29.36±39.38a | 37.12±21.75ad | 0.867 (ANOVA) |
| t1/2z/h | 8.99±17.75 | 4.48±4.77a | 4.17±1.45ad | 0.573 (ANOVA) |
| AUC(0–t)/mg·L−1·h | 4.19±5.56 | 3.41±3.66a | 5.03±3.70ad | 0.757 (ANOVA) |
| AUC(0–∞)/mg·L−1·h | 4.98±5.62 | 3.89±4.09a | 5.58±3.66ad | 0.734 (ANOVA) |
| MRT(0–t)/h | 1.24±1.44 | 1.66±1.41a | 2.15±1.71ad | 0.562 (ANOVA) |
| MRT(0–∞)/h | 10.44±25.12 | 3.32±4.38a | 3.85±2.47ad | 0.504 (K-W H test) |
| VRT(0–t)/h2 | 4.56±5.75 | 5.31±4.75a | 7.44±6.09ad | 0.632 (ANOVA) |
| VRT(0–∞)/h2 | 733.27±2035.59 | 45.66±92.89a | 33.26±26.60ad | 0.603 (K-W H test) |
| CLz/L·h−1 | 51.94±88.80 | 83.49±82.84a | 33.64±19.62ad | 0.416 (ANOVA) |
| Vz/L | 243.31±441.20 | 267.97±155.62a | 213.10±155.81ad | 0.924 (ANOVA) |
Multiple-dose pharmacokinetics in patients with advanced solid tumors
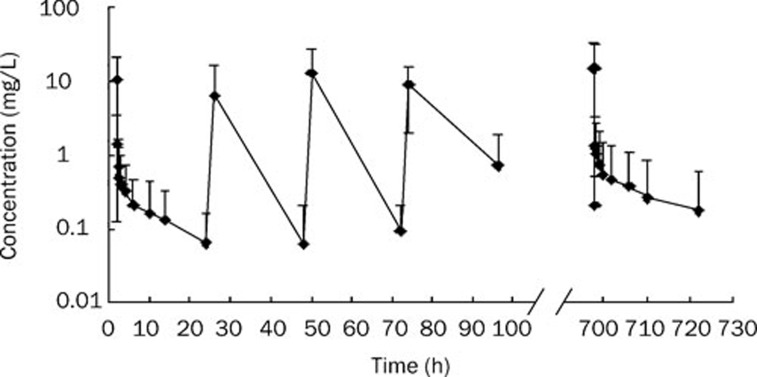
Figure 5 demonstrates a mean plasma concentration versus time plot for the eight patients obtained after receiving 100 mg·m−2 panaxatrol disuccinate sodium for the 30-day continuous intravenous injection. Steady-state pharmacokinetic parameters are summarized in Table 4. Cmax, trough concentration (Cmin) and average concentration (Cav) were 13.96±15.48, 0.18±0.29, and 0.15±0.29 mg·L−1, respectively. No accumulation was observed with continuous administration of panaxatrol disuccinate sodium. The mean steady state AUC (AUCss) and the degree of fluctuation were 3.58±6.94 mg·L−1 and 148.00±117.18, respectively. Comparing the groups that received single and multiple dose of 100 mg·m−2, no significant difference was observed in C0, AUC0–t, AUC0–∞, t1/2z, CLz/F, and Vz/F (P>0.05, t-test).
Figure 5.
Mean logarithmic concentration versus time after receiving 100 mg·m−2 panaxatrol disuccinate sodium for the 30-day continuous intravenous injection (n=8). Data are expressed as means±SD.
Table 4. Steady-state pharmacokinetics parameters after receiving panaxatrol disuccinate sodium 100 mg·m−2 for the 30-day continuous intravenous injection.
| Parameters | AUCss (mg·L−1·h) | Cmax (mg·L−1) | Cmin (mg·L−1) | Cav (mg·L−1) | DF |
|---|---|---|---|---|---|
| No 1 | 0.432 | 1.909 | 0.575 | 0.018 | 74.06 |
| No 2 | 0.527 | 2.169 | 0 | 0.022 | 98.76 |
| No 3 | 2.445 | 35.97 | 0 | 0.102 | 353.12 |
| No 4 | 0.253 | 2.539 | 0.704 | 0.011 | 173.91 |
| No 5 | 0.497 | 0.318 | 0.128 | 0.021 | 9.18 |
| No 6 | 20.582 | 29.623 | 0 | 0.858 | 34.54 |
| No 7 | 1.008 | 7.649 | 0 | 0.042 | 182.06 |
| No 8 | 2.926 | 31.496 | 0 | 0.122 | 258.33 |
| Mean | 3.584 | 13.959 | 0.176 | 0.15 | 148.00 |
| SD | 6.941 | 15.482 | 0.292 | 0.289 | 117.18 |
Toxic effects
Intravenous injection of panaxatrol disuccinate sodium was well tolerated in healthy volunteers and patients with advanced tumors. All subjects were evaluated for tolerability, and no toxic effects were observed throughout the study.
Discussion
Panaxatrol disuccinate sodium, a novel anti-cancer drug, is synthesized by structure reconstitution of notoginsenoside. In this present study, we determine the concentration of panaxatrol disuccinate sodium in human plasma by LC-MS. The LLOQ under the present condition was 0.03039 μg·mL−1. The results indicated that the method was specific, sensitive and convenient for determination of panaxatrol disuccinate sodium levels in biological samples. Then, we investigated the pharmacokinetics and safety of panaxatrol disuccinate sodium in healthy volunteers and patients with advanced solid tumors.
Following a single dose intravenous administration, the plasma concentration of panaxatrol disuccinate sodium declined rapidly after the end of the intravenous injection to a level that was ten-fold lower on average than Cmax within 10 min. However, Cmax and AUC did not increase proportionally to the dose ranging from 70 mg·m−2 to 140 mg·m−2. No significant differences were observed in the main pharmacokinetic parameters among the three dosing groups, indicating that the effect of dose level on single dose pharmacokinetics of panaxatrol disuccinate sodium is not significant. Non-clinical pharmacokinetic studies in rats16, 17 showed that the concentration-time profile of active saponins from PNS were similar. The distribution and elimination of saponins were rapid after oral administration of PNS. In the multiple-dose pharmacokinetic study, Cmin and Cav remained low. No significant differences were observed in pharmacokinetic parameters between single-dose 100 mg·m−2 group and multiple-dose 100 mg·m−2 group, indicating that no accumulation was observed with repeated doses of panaxatrol disuccinate sodium.
Moreover, we found obvious intragroup variability in pharmacokinetic parameters. At any given dose of panaxatrol disuccinate sodium, there was 5–28-fold variability in panaxatrol disuccinate sodium exposure. It is presently unclear whether the pharmacokinetic variability of panaxatrol disuccinate sodium is relevant to hepatic metabolic enzymes and/or other catabolic enzymes. Attention should be given to the interindividual variability in future study.
No intolerable side effects were observed in the entire study period. A previous tolerability study18 had similar results, suggesting that this product had minimal toxic effects. In the tolerability study, the major side effects after the 30-day continuous injection included low-grade fatigue, pharyngalgia and sensation of heat. This result is consistent with the suggestion that ginsenoside has tonic effects in humans.
In conclusion, the effect of dose level on single-dose pharmacokinetics of panaxatrol disuccinate sodium was not significant. No accumulation was observed with exposure to 100 mg·m−2 panaxatrol disuccinate sodium in a 30-day continuous intravenous injection. All subjects had high tolerance throughout the study. Thus, the phase II dose of panaxatrol disuccinate sodium may be considered to be 100 mg·m−2 for a 30-day continuous intravenous injection to treat patients with advanced solid tumors. Further evaluation of the efficacy and safety of panaxatrol disuccinate sodium versus placebo should be done in pivotal phase II/III clinical trials.
Author contribution
Zhao YAN and Chang-xiao LIU designed the research; Zhao YAN, Zhong-ling ZHU, Hua-qing WANG, Wei LI, and Ya-xian MI performed the research; Zhao YAN and Zhong-ling ZHU analyzed data; Zhao YAN, Zhong-ling ZHU, and Chang-xiao LIU wrote the paper.
References
- Wang W, Rayburn ER, Hang J, Zhao Y, Wang H, Zhang R. Anti-lung cancer effects of novel ginsenoside 25-OCH(3)-PPD. Lung Cancer. 2009;65:306–11. doi: 10.1016/j.lungcan.2008.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yun TK, Choi SY. Preventive effect of ginseng intake against various human cancers: a case-control study on 1987 pairs. Cancer Epidemiol Biomarkers Prev. 1995;4:401–8. [PubMed] [Google Scholar]
- Shinkai K, Akedo H, Mukai M, Imamura F, Isoai A, Kobayashi M, et al. Inhibition of in vitro tumor cell invasion by ginsenoside Rg3. Jpn J Cancer Res. 1996;87:357–62. doi: 10.1111/j.1349-7006.1996.tb00230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park JA, Lee KY, Oh YJ, Kim KW, Lee SK. Activation of caspase-3 protease via a Bcl-2-insensitive pathway during the process of ginsenoside Rh2-induced apoptosis. Cancer Lett. 1997;121:73–81. doi: 10.1016/s0304-3835(97)00333-9. [DOI] [PubMed] [Google Scholar]
- Sato K, Mochizuki M, Saiki I, Yoo YC, Samukawa K, Azuma I. Inhibition of tumor angiogenesis and metastasis by a saponin of Panax ginseng, ginsenoside-Rb2. Biol Pharm Bull. 1994;17:635–9. doi: 10.1248/bpb.17.635. [DOI] [PubMed] [Google Scholar]
- Nakata H, Kikuchi Y, Tode T, Hirata J, Kita T, Ishii K, et al. Inhibitory effects of ginsenoside Rh2 on tumor growth in nude mice bearing human ovarian cancer cells. Jpn J Cancer Res. 1998;89:733–40. doi: 10.1111/j.1349-7006.1998.tb03278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasegawa H, Sung JH, Matsumiya S, Uchiyama M, Inouye Y, Kasai R, et al. Reversal of daunomycin and vinblastine resistance in multidrug-resistant P388 leukemia in vitro through enhanced cytotoxicity by triterpenoids. Planta Med. 1995;61:409–13. doi: 10.1055/s-2006-958126. [DOI] [PubMed] [Google Scholar]
- Lau WS, Chen WF, Chan RY, Guo DA, Wong MS. Mitogen-activated protein kinase (MAPK) pathway mediates the oestrogen-like activities of ginsenoside Rg1 in human breast cancer (MCF-7) cells. Br J Pharmacol. 2009;156:1136–46. doi: 10.1111/j.1476-5381.2009.00123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang TH, Tran VH, Roufogalis BD, Li Y. Gypenoside XLIX, a naturally occurring gynosaponin, PPAR-alpha dependently inhibits LPS-induced tissue factor expression and activity in human THP-1 monocytic cells. Toxicol Appl Pharmacol. 2007;218:30–6. doi: 10.1016/j.taap.2006.10.013. [DOI] [PubMed] [Google Scholar]
- Choi K, Kim M, Ryu J, Choi C. Ginsenosides compound K and Rh(2) inhibit tumor necrosis factor-alpha-induced activation of the NF-kappaB and JNK pathways in human astroglial cells. Neurosci Lett. 2007;421:37–41. doi: 10.1016/j.neulet.2007.05.017. [DOI] [PubMed] [Google Scholar]
- Lin HS, Piao BK. Phase II clinical trial report of treating lung cancer with capsule. Chin J Clin Oncol. 2002;29:276–9. [Google Scholar]
- Pang H, Wang HL, Fu L, Su CY. Pharmacokinetic studies of 20(R)-ginsenoside Rg3 in human volunteers. Yao Xue Xue Bao. 2001;36:170–3. [PubMed] [Google Scholar]
- Xie HT, Wang GJ, Sun JG, Tucker I, Zhao XC, Xie YY, et al. High performance liquid chromatographic-mass spectrometric determination of ginsenoside Rg3 and its metabolites in rat plasma using solid-phase extraction for pharmacokinetic studies. J Chromatogr B Analyt Technol Biomed Life Sci. 2005;818:167–73. doi: 10.1016/j.jchromb.2004.12.028. [DOI] [PubMed] [Google Scholar]
- Gu Y, Wang GJ, Sun JG, Jia YW, Wang W, Xu MJ, et al. Pharmacokinetic characterization of ginsenoside Rh2, an anticancer nutrient from ginseng, in rats and dogs. Food Chem Toxicol. 2009;47:2257–68. doi: 10.1016/j.fct.2009.06.013. [DOI] [PubMed] [Google Scholar]
- Konoshima T, Takasaki M, Tokuda H. Anti-carcinogenic activity of the roots of Panax notoginseng. II. Biol Pharm Bull. 1999;22:1150–2. doi: 10.1248/bpb.22.1150. [DOI] [PubMed] [Google Scholar]
- Li L, Sheng Y, Zhang J, Wang C, Guo D. HPLC determination of four active saponins from Panax notoginseng in rat serum and its application to pharmacokinetic studies. Biomed Chromatogr. 2004;18:849–56. doi: 10.1002/bmc.400. [DOI] [PubMed] [Google Scholar]
- Xu QF, Fang XL, Chen DF. Pharmacokinetics and bioavailability of ginsenoside Rb1 and Rg1 from Panax notoginseng in rats. J Ethnopharmacol. 2003;84:187–92. doi: 10.1016/s0378-8741(02)00317-3. [DOI] [PubMed] [Google Scholar]
- Sun Y, Wang HQ, Yan Z, Song Z, Zhang HL, Liu XM, et al. A phase I trial for evaluating the tolerance of disodium panaxatriol 3,6-succinate. Chin J New Drugs. 2008;17:241–3. [Google Scholar]