Abstract
Aim:
The efficacy of the Akt inhibitor perifosine against chronic myeloid leukemia (CML) cells and its mechanisms of action are unknown. In this study, the cytotoxic effects of perifosine on CML and acute myeloid leukemia (AML) cell lines were compared to elucidate the mechanisms underlying the differences.
Methods:
Human AML cell lines Kasumi-1 and HL-60, and the CML cell line K562 were used. Cell viability was quantitated using MTT assay. Apoptosis was determined using Annexin V-FITC/propidium iodide and Hoechst staining, which were followed by flow cytometry and fluorescence microscopy analysis, respectively. Caspase pathway activation and the expression of autophagy-related genes were examined using Western blot. Autophagy was studied using electron microscopy, the acridine orange staining method, and GFP-LC3 was examined with fluorescence microscopy.
Results:
In contrast to AML cell lines, the CML cell lines K562 and K562/G (an imatinib-insensitive CML cell line) were resistant to perifosine (2.5–20 μmol/L) in respect to inhibiting cell growth and inducing apoptosis. Perifosine (2.5, 5, and 10 μmol/L) inhibited Akt and its phosphorylation in AML cells, but not in CML cells. Treatment with perifosine (20 μmol/L) resulted in autophagy in CML cells as shown by the increased formation of acidic vesicular organelles and the accumulation of LC3-II. Treatment of CML cells with perifosine (5, 10, and 20 μmol/L) dose-dependently upregulated AGT5, but not Beclin 1 at the protein level. Furthermore, inhibition of autophagy by chloroquine (40 nmol/L) significantly suppressed the cell growth and induced apoptosis in CML cells treated with perifosine (20 μmol/L).
Conclusion:
Our results show that CML cell lines were resistant to the Akt inhibitor perifosine in vitro, which is due to perifosine-induced protective autophagy and upregulation of ATG5.
Keywords: Akt inhibitor, perifosine, chronic myeloid leukemia, acute myeloid leukemia, autophagy, apoptosis, beclin 1, ATG5
Introduction
A hallmark of chronic myeloid leukemia (CML) is expression of the BCR/ABL oncoprotein that results from a reciprocal translocation involving chromosomes 9 and 22. This fusion protein has been exploited as a therapeutic target for the treatment of CML because it plays critical and essential roles in leukemogenesis1, 2. The chimeric BCR/ABL protein possesses cellular transforming ability that is ascribed to its elevated tyrosine kinase (TK) activity compared with that of native c-ABL3. Inhibition of BCR/ABL with imatinib mesylate (imatinib), a selective inhibitor of ABL kinase activity, results in long-term remission in CML patients; therefore, imatinib is the first-line therapy for newly diagnosed CML patients4. However, early relapses occur, and imatinib resistance due primarily to BCR/ABL kinase mutations has been documented5. Some resistant cells exhibit genomic amplification of non-mutated BCR/ABL and possess a BCR/ABL independence pathway6. Several signaling pathways are affected by constitutively active BCR/ABL, including increased proliferation through RAS/MAPK activation7, increased transcriptional activity via STAT recruitment8, and decreased apoptosis through the activation of PI3K/Akt9.
PI3K/Akt signaling is activated in numerous cancers types and is a crucial event in tumorigenesis10. Activation of receptor TKs by BCR/ABL results in activation of the PI3K/Akt pathway11. Numerous molecules downstream of Akt have been linked to the leukemogenic effects of BCR/ABL, including the proapoptotic protein BAD, MDM2, mammalian target of rapamycin (mTOR), and the FoxO (forkhead) family of transcription factors12, 13. Activation of Akt may endow CML progenitor cells with the ability to self-renew through deregulation of GSK3β, a critical negative regulator of the Wnt/β-catenin pathway14. Additionally, it was recently reported that imatinib treatment activated the PI3K/Akt/mTOR pathway and that this activation was important in mediating cell survival early in the development of imatinib resistance before the emergence of overt resistance15.
Perifosine is a lipid-based Akt inhibitor that exhibits antitumor activity in a broad range of tumor types. In vitro, perifosine inhibits the translocation of Akt to the cell membrane and suppresses the growth of various types of solid tumor and leukemia cells16, 17, 18. Perifosine induces apoptosis in acute myeloid leukemia (AML) cell lines and reduces the clonogenic activity of AML progenitors, but not of normal CD34+ cells, thereby sensitizing blast cells to etoposide19. Recent preclinical studies showed that perifosine has synergistic effects with chemotherapeutic agents, such as etoposide in leukemia cells19 and doxorubicin in multiple myeloma cells20. Based on these data, Phase II clinical trials of perifosine alone or in combination with dexamethasone for patients with relapsed or refractory multiple myeloma have shown promising antitumor activity21. However, it has been reported that human CML cell lines are unexpectedly resistant to GSK690693 (another Akt inhibitor); the underlying mechanism for this is unclear22. The present study followed up on this interesting observation by investigating the cytotoxic effects of perifosine on human AML cell lines and the CML cell lines K562 and K562/G (a cell line resistant to imatinib). We demonstrated perifosine-induced modulation of different apoptotic and autophagic molecules in an attempt to understand its mechanisms of action. Our data showed that perifosine induced apoptosis and inhibited Akt activation in AML cells, but not in CML cells. Interestingly, treatment of CML cells with perifosine induced autophagy and resulted in the upregulation of ATG5. We also observed that inhibition of the perifosine-mediated autophagic response with the lysosomotropic agent chloroquine led to accelerated apoptotic cell death. These findings support the notion that perifosine-induced autophagy is cytoprotective in CML cells.
Materials and methods
Cell lines and cell culture
The human AML cell lines Kasumi-1 and HL-60 and the CML cell line K562 were obtained from American Type Culture Collection (ATCC, Rockville, MD, USA). K562/G cells were kindly provided by the Institute of Hematology, Chinese Academy of Medical Sciences (Tianjin, China). The K562/G cell line is resistant to imatinib (50% inhibition at 48 h in K562 and K562/G was 71.8 and 261.0 nmol/L, respectively) but does not contain mutations within the TK domain. K562 cells expressing GFP-LC3 were established previously in our laboratory23. Cell lines were maintained in RPMI-1640 medium with 10% fetal bovine serum (Hyclone, Utah, USA) at 37 °C in a 5% CO2 humid atmosphere.
Cellular proliferation assay
Colorimetric assays were performed to evaluate drug activity. Leukemia cell lines were seeded into 96-well plates at a density of 1×105/mL in triplicate and then treated with 1.25–20 μmol/L perifosine (Binxinbio, Tianjin, China) alone or in combination with chloroquine (CQ, Sigma, St Louis, MO, USA) for 24 h or 48 h, respectively. At the end of the drug exposure, 20 μL of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT, Sigma) solution (5 mg/mL) was added into each well and incubated for an additional 4 h at 37 °C, at which time the supernatants were removed and 200 μL DMSO was used to dissolve the formazan crystals. The absorbance was read at 570 nm with a microplate reader (Bio-RAD, Berkeley, USA).
Western blot analysis
Cells were harvested and extracted with lysis buffer (Cell Signaling, Danvers, USA). The cell lysate was collected by centrifugation at 12 000×g for 5 min at 4 °C and protein concentration was determined by the BCA method. Samples containing 50 μg protein lysate were separated on 12% SDS-PAGE gels before transfer to a polyvinylidene difluoride membrane (Millipore, Billerica, MA, USA). The membranes were blocked with TBST containing 5% fat-free milk before overnight incubation with the indicated primary antibodies at 4 °C. The primary antibodies used in this study were as follows: Beclin-1 (Novus Biologicals, Colorado, USA), light chain 3 (LC3, Novus Biologicals), ATG-5 (Sigma), ATG7 (Sigma), JNK (Biovision, CA, USA), and phosphorylated-JNK (p-JNK). Antibodies to BCR/ABL, Akt, phosphorylated-Akt (p-Akt, Ser473), caspase-3, caspase-9, and polyadenosine-5-diphosphate-ribose polymerase (PARP) were purchased from Cell Signaling. The β-actin antibody was obtained from Santa Cruz Biotechnology (Santa Cruz, CA, USA). After incubation with the appropriate secondary antibodies (Multisciences Biotech, Hangzhou, China), antibody binding was detected by enhanced chemiluminescence (ECL) according to the manufacturer's recommendation.
Detection of acidic vesicular organelles
Autophagy is the process of sequestering cytoplasmic proteins into the cellular lytic compartment and is characterized by the development of acidic vesicular organelles (AVOs). Acridine orange (AO) is a widely used method to visualize AVOs. In AO-stained cells, the cytoplasm and nucleolus fluoresce bright green and dim red, respectively, whereas acidic compartments fluoresce bright red. To detect the formation of AVOs, perifosine-treated cells were washed twice with PBS, fixed with 4% paraformaldehyde, stained with AO (Molecular Probes, CA, USA) at 1 μg/mL for 15 min, washed with PBS to remove unbound dye, and subsequently examined under a fluorescence microscope (Olympus, Tokyo, Japan).
Transmission electron microscopy (TEM)
TEM was performed as previously described23. Briefly, cells were harvested, washed twice with PBS, and fixed with ice-cold 2.5% glutaraldehyde overnight. After washing with PBS, the cells were fixed in OsO4 and embedded in Spurr's resin. Ultrathin sections (0.12 μm) were cut and double stained with uranyl acetate and lead citrate. Representative areas were chosen and viewed with a Philips TECNA10 transmission electron microscope.
Assessment of apoptosis
Apoptosis was measured using an annexin V-FITC and propidium iodide (PI) apoptosis detection kit (Biouniquer, Suzhou, China) according to the manufacturer's instructions. Prepared cells were analyzed with a FACScan flow cytometer and CELLQuest software (Becton Dickinson, Franklin Lakes, NJ, USA). Chromatin condensation and nuclear fragmentation in leukemia cells were detected by Hoechst staining. Briefly, cells were harvested, plated on glass slides for fixation with 4% paraformaldehyde, and stained with 5 μg/mL Hoechst 33258 (Sigma) for 15 min in the dark at room temperature. Apoptotic cells were observed under a fluorescence microscope (Olympus).
Statistical analysis
All assays were performed in triplicate, and the results were presented as the mean±SD. Data were analyzed by the Student's t-test and ANOVA for statistical significance. P values <0.05 were considered significant.
Results
Perifosine reduces cell viability and induces apoptosis of AML, but not CML, cell lines
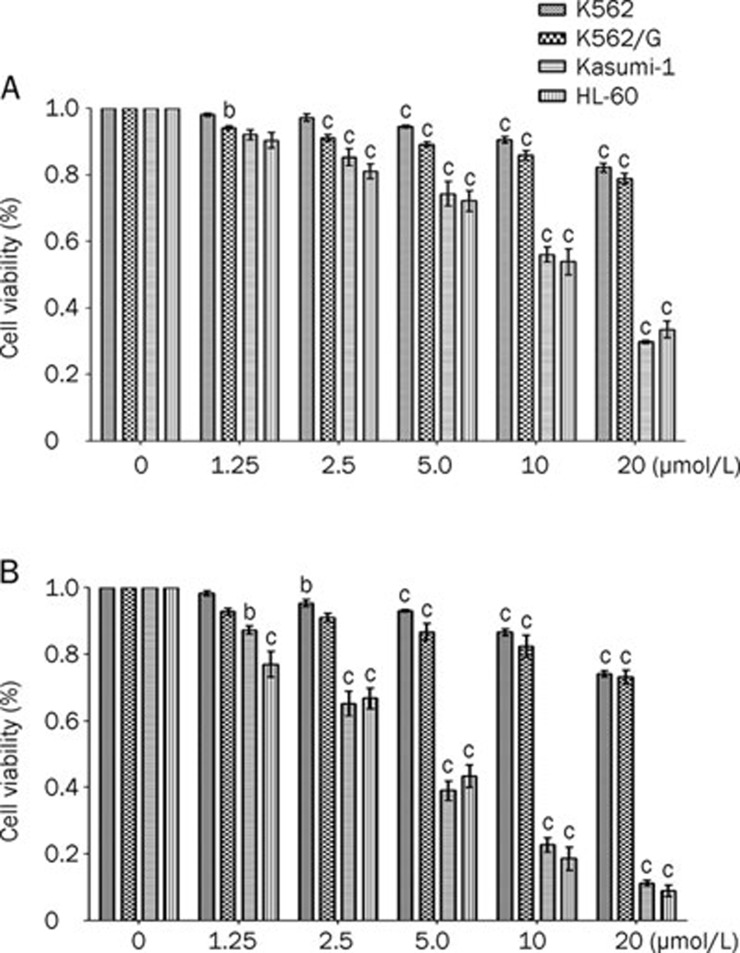
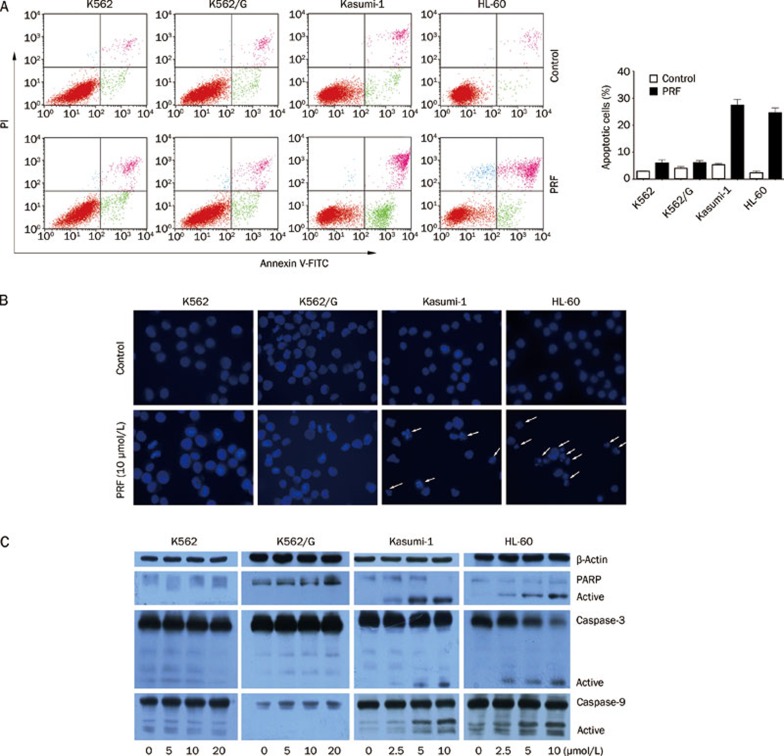
To compare the cytotoxic effects of perifosine on AML and CML cell lines, Kasumi-1, HL-60, K562, and K562/G cells were cultured with the indicated concentrations of perifosine for 24 h or 48 h, respectively. Cell viability was evaluated using an MTT assay. As shown in Figure 1, perifosine inhibited the growth of Kasumi-1 and HL-60 cells with 50% inhibition (IC50) at 48 h of 4.24 and 3.62 μmol/L, respectively. In contrast, 20 μmol/L perifosine did not significantly reduce the viability of the CML cell lines (K562 and K562/G) at 48 h, suggesting that they were resistant to perifosine. In order to characterize the cytotoxicity of perifosine on leukemia cells, we analyzed the induction of apoptosis in AML and CML cells cultured with 10 μmol/L perifosine for 24 h. Upon perifosine treatment, 27.5% and 24.6% of the AML cells were apoptotic, respectively, whereas little apoptosis was observed in the K562 and K562/G cells (Figure 2A). These results were confirmed by fluorescent microscopy analysis of Hoechst staining (Figure 2B). Furthermore, Western blotting analysis demonstrated that dose-dependent cleavage of caspase-9, caspase-3, and PARP was induced by perifosine in the AML cell lines. Neither cleavage of PARP nor activation of caspase-3 or -9 was detected in the CML cell lines (Figure 2C). These data indicated that CML cells were resistant to perifosine-induced apoptosis.
Figure 1.
AML cell lines are much sensitive to perifosine than CML cells. Exponentially growing cells were plated into 96-well plates, and then treated with the indicated concentrations of perifosine for 24 h (A) and 48 h (B), respectively. Growth inhibition in leukemia cell lines by perifosine was assessed by a MTT assay. Data represent mean±SD of three independent experiments. bP<0.05, cP<0.01 compared with untreatment (analyzed by ANOVA and Turkey-Kramer test).
Figure 2.
Apoptosis induced by perifosine in AML cells but not in CML cells. (A) After treatment with perifosine (PRF) at 10 μmol/L for 24 h, leukemia cell lines were harvested and detected by annexin V/propidium (PI)-staining method. The inserted panel shows data from three separate experiments (B) CML and AML cells were stained with Hoechst 33258 from one day after perifosine (10 μmol/L) treatment, and then observed under a fluorescence microscope. Arrows represent the apoptotic nuclei. (C) After incubation of leukemia cell lines for 24 h with the indicated concentrations of perifosine, whole cell extracts were analyzed by Western blot analysis using anti-caspase-3, -9, and PARP antibodies. β-Actin was used as a loading control. The results are representatives of three separate experiments.
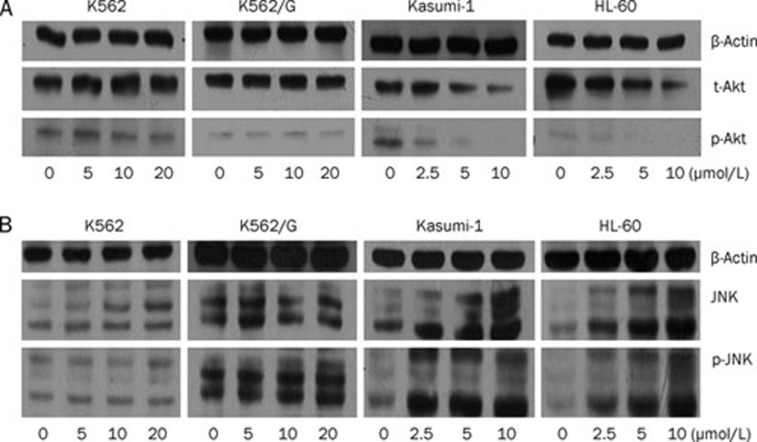
Different effects of perifosine on the phosphorylation of Akt and JNK in leukemia cells
Because the degree of Akt downregulation is correlated with cell sensitivity to perifosine-induced apoptosis24, we examined if perifosine could modulate the expression and phosphorylation of Akt (Ser473) in leukemia cell lines (Figure 3A). Kasumi-1 and HL-60 cells exhibited a dose-dependent decrease in Akt and p-Akt levels when exposed to perifosine for 24 h. As expected, downregulation of Akt was not observed in CML cell lines that are resistant to perifosine. Perifosine has been reported to trigger JNK activation followed by caspase-8, caspase-9, and PARP cleavage in multiple myeloma and AML cells20, 25. We also observed that perifosine strongly induced the phosphorylation of JNK1/2 in AML, but not CML, cells in a dose-dependent manner (Figure 3B). Collectively, these results suggested that the failure of perifosine to inhibit Akt and induce phosphorylation of JNK might play a role in mediating the drug resistance of CML cells.
Figure 3.
Perifosine's effect on phosphorylation and protein expression of Akt and JNK. (A) Leukemia cells were exposed to the indicated concentrations of perifosine for 24 h and then analyzed for expression of total and phosphorylated Akt (Ser473). (B) CML and AML cell lines were treated with varying doses of perifosine for 24 h, after which cells were harvested, and extracted proteins were immunoblotted for the expression of total and phosphorylated JNK, and β-actin. These experiments were repeated once with identical results.
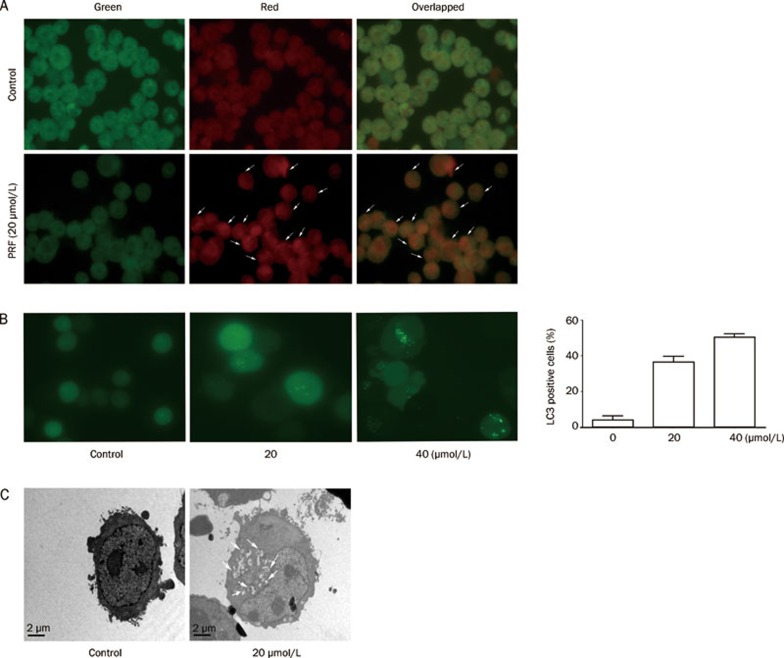
Perifosine induces autophagy in CML cells, but not in AML cells
Autophagy is frequently activated in response to stress and some therapeutic agents and is protective against cell death26, 27, 28. Given these observations, we investigated if perifosine could induce autophagy in K562 cells. An increase in AO-positive acidic vesicular organelles occurs in conjunction with the induction of autophagy in leukemia23, 27. As shown in Figure 4A, AO staining of AVOs was detected in K562 cells treated with perifosine, but not in those cells treated with PBS as a control. Fusing GFP with LC3 provides a fluorescent marker for autophagy, so we transfected this construct into K562 cells. The cells were treated with the indicated dose of perifosine for 24 h and autophagosome formation was visualized by fluorescent microscopy. Perifosine treatment at 20 and 40 μmol/L resulted in 33.3% and 47.1%, respectively, of cells that contained LC3-positive vesicles (Figure 4B). Transmission electron microscopy revealed the formation of autophagic vesicles after treatment with perifosine in K562 cells (Figure 4C). These findings suggested that perifosine induced autophagy in K562 cells.
Figure 4.
Induction of autophagy by perifosine(PRF) in K562 cells. (A) K562 cells were treated with or without 20 μmol/L perifosine for 48 h, and then stained with acridine orange (1 μg/mL), and then visualized under green and red filter microscope; note the presence of numerous autophagical vacuoles (white arrows). All digital micrographs were taken at the same exposure setting and images were overlapped. (B) K562 cells that were transfected with GFP-LC3 were incubated for 24 h without or with perifosine at 20 and 40 μmol/L, respectively, and then examined by a fluorescence microscopy. The cells with LC3-positive vesicles were calculated using ImageJ software, and data from three independent experiments were shown (right panel). (C) Representative TEM photomicrographs (×3700) of the K562 cells treated without or with 20 μmol/L perifosine for 48 h. Arrows, autophagic vacuoles. Scale bars, 2 μm.
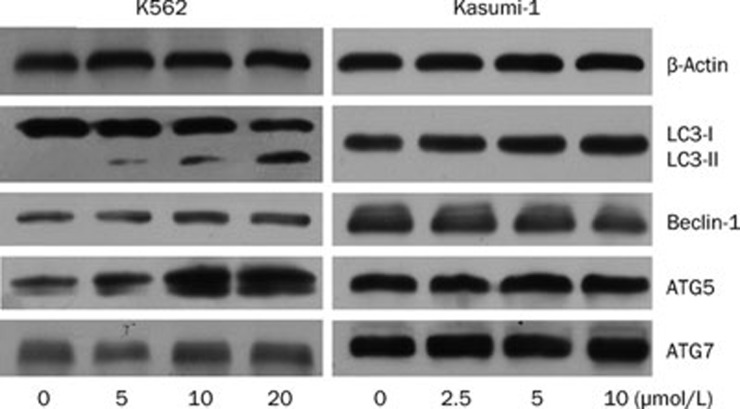
We next examined by Western blot if perifosine could induce the expression of autophagy-related genes. As shown in Figure 5, a dose-dependent increase in the expression of AGT5 was observed in K562 cells treated with perifosine. Meanwhile, a progressive increase in autophagic activity (defined by LC3-I to LC3-II conversion) was detected after exposure to perifosine for 24 h. However, upregulation of ATG7 and Beclin-1, which are required for autophagy29, did not occur. Kasumi-1 cells failed to show this autophagic response or changes in autophagy-related gene expression.
Figure 5.
Effects of perifosine on expression of autophagy-related genes. After treatment with the indicated doses of perifosine for 24 h, K562 and Kasumi-1 cells were harvested. Whole cell lysates were subjected to Western blotting for protein expression of Beclin-1, ATG5, ATG7, and LC3. Anti-β-actin antibody was used as a control for protein loading.
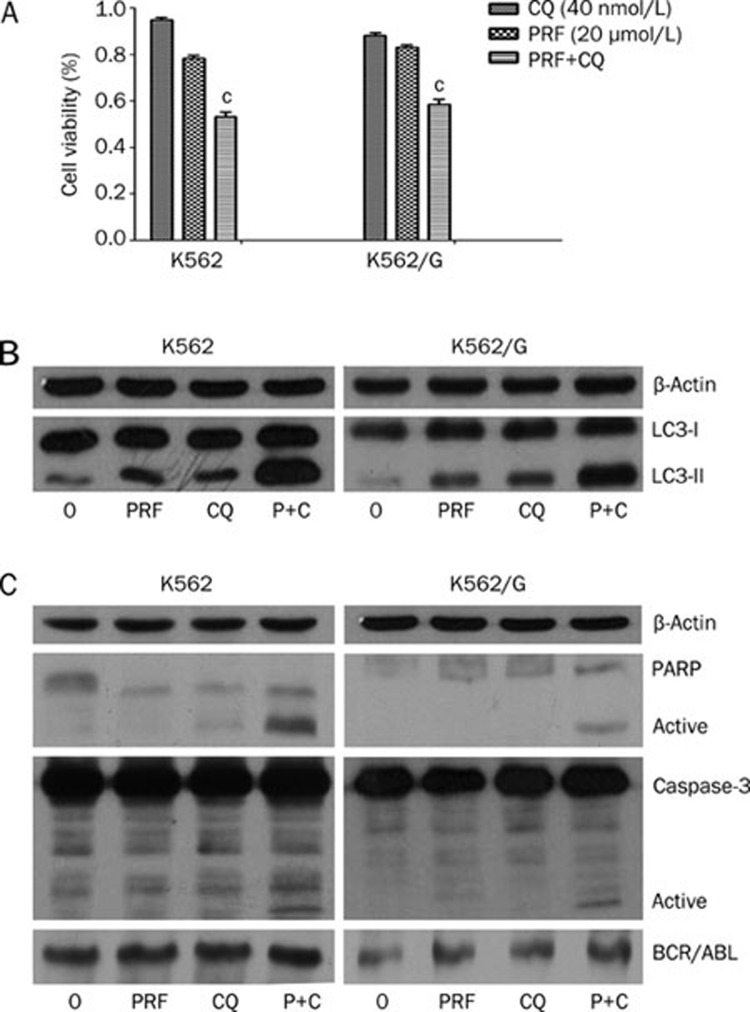
Inhibition of autophagy potentiates perifosine-mediated apoptosis in K562 cells
To examine the significance of perifosine-induced autophagy in CML cells, we inhibited autophagy in K562 and K562/G cells using CQ and analyzed the effect on perifosine-induced cell death. As shown in Figure 6A, cell death, as measured using an MTT assay, significantly increased when perifosine was combined with CQ (from 21.5% to 46.8%; P=0.004). Western blotting showed an enhanced accumulation of LC3-II in CQ- and perifosine-treated K562 cells (Figure 6B) because CQ prevents autophagosome-lysosome fusion and thereby blocks autophagic degradation30. Furthermore, inhibition of autophagy upon co-treatment with perifosine and CQ promoted the apoptosis of K562 cells as evidenced by increased PARP cleavage and caspase-3 activation (Figure 6C). Treatment with perifosine and CQ showed no detectable modulation of the protein level of BCR/ABL (Figure 6C). Similar results were also observed in K562/G cells, an imatinib-resistant cell line (Figure 6). These data indicate that perifosine-induced autophagy plays a prosurvival role in protecting leukemia cells.
Figure 6.
Inhibition of autophagy results in enhanced suppression of cell growth and apoptosis in CML cell lines. (A) K562 and K562/G cells were treated for 48 h with perifosine (PRF, 20 μmol/L), chloroquine (CQ, 40 nmol/L) or two agents combination, respectively. Viability of cells growth was examined by a MTT assay. Mean±SD. n=3. (B) Western blotting analysis was performed for the expression of LC3 and β-actin. (C) The levels of BCR/ABL fusion protein, cleavage of PARP, and activation of caspase-3 were analyzed using western blotting. Anti-β-actin was used as a control for protein loading. cP<0.01 vs perifosine.
Discussion
Akt kinase is reported to be constitutively active in the chronic phase of CML, during blast crisis of CML, and in the K562 cell line11, 31. Activation of Akt may endow CML progenitor cells with the ability to self-renew and could play an important role in mediating imatinib resistance14, 15. Thus, the Akt pathway is an attractive target for the treatment of CML. However, the present study demonstrated that the Akt kinase inhibitor perifosine has activity against AML cells, but not CML cells. This is consistent with a previous report showing that CML cell lines were resistant to GSK690693, another Akt kinase inhibitor22, although the mechanism of this resistance is unknown. Some studies suggest that the downregulation of Akt phosphorylation is associated with perifosine-induced apoptosis and inhibition of tumor growth19,20,22,32. Similarly, our in vitro experiments showed that perifosine inhibited cell growth and Akt phosphorylation and induced apoptosis in AML cells. Inhibition of Akt kinase activity was not observed in the perifosine-insensitive CML cell lines K562 and K562/G, suggesting that the lack of sensitivity was likely due to a failure to inhibit Akt phosphorylation. In contrast to our findings, acute lymphoblastic leukemia cells in which the lack of sensitivity is not related to the inability of perifosine to inhibit Akt signaling have been reported22. Therefore, multiple mechanisms of resistance might exist.
Autophagy is a highly conserved catabolic program for the degradation and recycling of cellular components, including long-lived proteins and organelles, and has been recognized as an important regulatory mechanism in cell fate decisions. This process is activated in cancer cells in response to stress or therapeutic agents23, 26, 27, 33. An emerging role for autophagy has been demonstrated in response to tyrosine kinase inhibitors (TKI) such as imatinib and INNO-406 in CML cells, including the stem cells34, 35, 36. This autophagic response to therapeutic agents in CML cells is dependent on Beclin 1. In the present study, we observed an accumulation of the autophagic protein marker LC3-II and a substantial increase in the formation of AVOs in K562 cells treated with perifosine. Electron microscopy revealed a massive accumulation of autophagic vacuoles after perifosine treatment. Our findings support the previous report in which autophagy was observed in lung cancer cells treated with perifosine37. The same study showed that perifosine inhibited the Akt and mTOR axes, which may contribute to perifosine-induced autophagy. Another study reported that Akt inactivation with small molecule inhibitors did not significantly induce apoptosis but instead increased autophagy38. In our study, perifosine did not inhibit either the Akt or mTOR axes in CML cells (data not shown), suggesting that alternative signaling pathways are involved in autophagy. Interestingly, we found that treatment with perifosine markedly increased ATG5 protein expression, but not that of Beclin 1. Recent publications suggest that non-canonical autophagy is Beclin 1-independent, and this process is emerging as a key regulator of the cell death pathway39, 40, 41, 42. Prior studies have shown that the formation of autophagosomes during Beclin 1-independent autophagy is dependent on the ATG12-ATG5 conjugation system, and that ATG5 is necessary for gossypol-mediated autophagy in cancer cells43, 44, 45. However, in this study we could not successfully transfect ATG5 siRNA into K562 cells using Lipofectamine. Further investigations are needed to elucidate the molecular mechanism by which perifosine-induced non-canonical autophagy in CML cells is associated with the upregulation of ATG5.
It is well established that autophagy functions in a prosurvival role in cancer cells and that the inhibition of autophagy increases the effectiveness of anticancer drugs26, 36. TKIs, the histone deacetylase inhibitor SAHA, and OSI-027 (a drug primarily targeting mTOR) have been reported to initiate protective autophagy in CML cells; disrupting this drug-induced autophagy using CQ, 3-MA, NH4Cl, or bafilomycin A1 significantly augments an agent's antileukemic activity13, 28, 34. Consistent with these findings, we showed that the combined use of the Akt inhibitor perifosine with CQ resulted in an enhanced inhibition of cell growth and induction of apoptosis, even though CML cells are resistant to perifosine alone. Moreover, this therapeutic strategy also effectively killed imatinib-resistant cells (K562/G), indicating that autophagy inhibitors such as CQ, in combination with Akt inhibitors, could be beneficial in overcoming drug resistance. Importantly, it has been shown that the combination of TKIs with inhibitors of autophagy sensitizes the CD34+CD38− subpopulation to TKIs. In a long-term culture-initiating assay that assessed leukemia stem cell functionality, the inhibition of autophagy resulted in a significant elimination of CML stem cells36. These promising results led to a phase II clinical trial that will evaluate the efficacy of imatinib combined with hydroxychloroquine (a lysosomotropic agent) in reducing the population of CML stem cells.
In conclusion, we show for the first time that the Akt inhibitor perifosine induces autophagy in CML cells, which along with the upregulation of ATG5, may contribute to the drug-induced autophagic response. Moreover, the inhibition of perifosine-induced autophagy led to enhanced cell death in CML cells, suggesting that the inhibition of autophagy may improve the therapeutic effects of Akt inhibitors in the treatment of CML.
Author contribution
Wen-bin QIAN designed the research; Yin TONG, Yan-yan LIU, and Liang-shun YOU performed the experiments; Wen-bin QIAN and Yin TONG analyzed the data and wrote the paper.
Acknowledgments
This work was supported by the Zhejiang Provincial Natural Science Foundation of China (R2090392) and Science and the Technology Foundation of Zhejiang Province (2011c23089). We are grateful to Prof Tamotsu YOSHIMORI, PhD, for providing the EGFP-LC3 plasmid and to Li WANG (Zhejiang University) for her help with TEM.
References
- Druker BJ. Translation of the Philadelphia chromosome into therapy for CML. Blood. 2008;112:4808–17. doi: 10.1182/blood-2008-07-077958. [DOI] [PubMed] [Google Scholar]
- Groffen J, Stephenson JR, Heisterkamp N, de Klein A, Bartram CR, Grosveld G. Philadelphia chromosomal breakpoints are clustered within a limited region, bcr, on chromosome 22. Cell. 1984;36:93–9. doi: 10.1016/0092-8674(84)90077-1. [DOI] [PubMed] [Google Scholar]
- Daley GQ, Van Etten RA, Baltimore D. Induction of chronic myelogenous leukemia in mice by the P210 bcr/abl gene of the Philadelphia chromosome. Science. 1990;247:824–30. doi: 10.1126/science.2406902. [DOI] [PubMed] [Google Scholar]
- Deininger M, Buchdunger E, Druker BJ. The development of imatinib as a therapeutic agent for chronic myeloid leukemia. Blood. 2005;105:2640–53. doi: 10.1182/blood-2004-08-3097. [DOI] [PubMed] [Google Scholar]
- Gorre ME, Mohammed M, Ellwood K, Hsu N, Paquette R, Rao PN, et al. Clinical resistance to STI-571 cancer therapy caused by BCR-ABL gene mutation or amplification. Science. 2001;293:876–80. doi: 10.1126/science.1062538. [DOI] [PubMed] [Google Scholar]
- Koptyra M, Falinski R, Nowicki MO, Stoklosa T, Majsterek I, Nieborowska-Skorska M, et al. BCR/ABL kinase induces self-mutagenesis via reactive oxygen species to encode imatinib resistance. Blood. 2006;108:319–27. doi: 10.1182/blood-2005-07-2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puil L, Liu J, Gish G, Mbamalu G, Bowtell D, Pelicci PG, et al. Bcr-Abl oncoproteins bind directly to activators of the Ras signalling pathway. EMBO J. 1994;13:764–73. doi: 10.1002/j.1460-2075.1994.tb06319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warsch W, Kollmann K, Eckelhart E, Fajmann S, Cerny-Reiterer S, Hölbl A, et al. High STAT5 levels mediate imatinib resistance and indicate disease progression in chronic myeloid leukemia. Blood. 2011;117:3409–20. doi: 10.1182/blood-2009-10-248211. [DOI] [PubMed] [Google Scholar]
- Skorski T, Kanakaraj P, Nieborowska-Skorska M, Ratajczak MZ, Wen SC, Zon G, et al. Phosphatidylinositol-3 kinase activity is regulated by BCR/ABL and is required for the growth of Philadelphia chromosome-positive cells. Blood. 1995;86:726–36. [PubMed] [Google Scholar]
- Vivanco I, Sawyers CL. The phosphatidylinositol 3-Kinase AKT pathway in human cancer. Nat Rev Cancer. 2002;2:489–501. doi: 10.1038/nrc839. [DOI] [PubMed] [Google Scholar]
- Quintás-Cardama A, Cortes J. Molecular biology of bcr-abl1-positive chronic myeloid leukemia. Blood. 2009;113:1619–30. doi: 10.1182/blood-2008-03-144790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiter GA, Zerp SF, Bartelink H, van Blitterswijk WJ, Verheij M. Anticancer alkyl-lysophospholipids inhibit the phosphatidylinositol 3-kinase-Akt/PKB survival pathway. Anticancer Drugs. 2003;14:167–73. doi: 10.1097/00001813-200302000-00011. [DOI] [PubMed] [Google Scholar]
- Helgason GV, Karvela M, Holyoake TL. Kill one bird with two stones: potential efficacy of BCR-ABL and autophagy inhibition in CML. Blood. 2011;118:2035–43. doi: 10.1182/blood-2011-01-330621. [DOI] [PubMed] [Google Scholar]
- Jamieson CH. Chronic myeloid leukemia stem cells. Hematology Am Soc Hematol Educ Program. 2008. pp. 436–42. [DOI] [PubMed]
- Burchert A, Wang Y, Cai D, von Bubnoff N, Paschka P, Müller-Brüsselbach S, et al. Compensatory PI3-kinase/Akt/mTor activation regulates imatinib resistance development. Leukemia. 2005;19:1774–82. doi: 10.1038/sj.leu.2403898. [DOI] [PubMed] [Google Scholar]
- Vink SR, Schellens JH, van Blitterswijk WJ, Verheij M. Tumor and normal tissue pharmacokinetics of perifosine, an oral anti-cancer alkylphospholipid. Invest New Drugs. 2005;23:279–86. doi: 10.1007/s10637-005-1436-0. [DOI] [PubMed] [Google Scholar]
- LoPiccolo J, Blumenthal GM, Bernstein WB, Dennis PA. Targeting the PI3K/Akt/mTOR pathway: effective combinations and clinical considerations. Drug Resist Updat. 2008;11:32–50. doi: 10.1016/j.drup.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyåkern M, Cappellini A, Mantovani I, Martelli AM. Synergistic induction of apoptosis in human leukemia T cells by the Akt inhibitor perifosine and etoposide through activation of intrinsic and Fas-mediated extrinsic cell death pathways. Mol Cancer Ther. 2006;5:1559–70. doi: 10.1158/1535-7163.MCT-06-0076. [DOI] [PubMed] [Google Scholar]
- Papa V, Tazzari PL, Chiarini F, Cappellini A, Ricci F, Billi AM, et al. Proapoptotic activity and chemosensitizing effect of the novel Akt inhibitor perifosine in acute myelogenous leukemia cells. Leukemia. 2008;22:147–60. doi: 10.1038/sj.leu.2404980. [DOI] [PubMed] [Google Scholar]
- Hideshima T, Catley L, Yasui H, Ishitsuka K, Raje N, Mitsiades C, et al. Perifosine, an oral bioactive novel alkylphospholipid, inhibits Akt and induces in vitro and in vivo cytotoxicity in human multiple myeloma cells. Blood. 2006;107:4053–62. doi: 10.1182/blood-2005-08-3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson P, Lonial S, Jakubowiak A, Krishnan A, Wolf J, Densmore J, et al. Multi-center phase II study of Perifosine (KRX-0401) alone and in combination with dexamethasone (Dex) for patients with relapsed or relapsed/refractory multiple myeloma (MM): promising activity as combination therapy with manageable toxicity. Blood. 2007;110:1164. [Google Scholar]
- Levy DS, JA Kahana JA, Kumar R. AKT inhibitor, GSK690693, induces growth inhibition and apoptosis in acute lymphoblastic leukemia cell lines. Blood. 2009;113:1723–29. doi: 10.1182/blood-2008-02-137737. [DOI] [PubMed] [Google Scholar]
- Yang C, Tong Y, Ni W, Liu J, Xu W, Li L, et al. Inhibition of autophagy induced by overexpression of MDA/Interleukin-24 using a PI3K inhibitor results in significant enhanced antileukmia activity in vivo. Cancer Gene Ther. 2010;17:109–19. doi: 10.1038/cgt.2009.57. [DOI] [PubMed] [Google Scholar]
- Elrod HA, Lin YD, Yue P, Wang X, Lonial S, Khuri FR, et al. The alkylphospholipid perifosine induces apoptosis of human lung cancer cells requiring inhibition of Akt and activation of the extrinsic apoptotic pathway. Mol Cancer Ther. 2007;6:2029–38. doi: 10.1158/1535-7163.MCT-07-0004. [DOI] [PubMed] [Google Scholar]
- Rahmani M, Reese E, Dai Y, Bauer C, Payne SG, Dent P, et al. Coadministration of histone deacetylase inhibitors and perifosine synergistically induces apoptosis in human leukemia cells through Akt and ERK1/2 inactivation and the generation of ceramide and reactive oxygen species. Cancer Res. 2005;65:2422–32. doi: 10.1158/0008-5472.CAN-04-2440. [DOI] [PubMed] [Google Scholar]
- Mathew R, Karantza-Wadsworth V, White E. Role of autophagy in cancer. Nat Rev Cancer. 2007;7:961–7. doi: 10.1038/nrc2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian W, Liu J, Jin J, Ni W, Xu W. Arsenic trioxide induces not only apoptosis but also autophagic cell death in leukemia cell lines via up-regulation of Beclin-1. Leuk Res. 2007;31:329–39. doi: 10.1016/j.leukres.2006.06.021. [DOI] [PubMed] [Google Scholar]
- Carew JS, Nawrocki ST, Kahue CN, Zhang H, Yang C, Chung L, et al. Targeting autophagy augments the anticancer activity of the histone deacetylase inhibitor SAHA to overcome Bcr-Abl-mediated drug resistance. Blood. 2007;110:313–22. doi: 10.1182/blood-2006-10-050260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Alva A, Su H, Dutt P, Freundt E, Welsh S, et al. Regulation of an ATG7-beclin 1 program of autophagic cell death by caspase-8. Science. 2004;304:1500–2. doi: 10.1126/science.1096645. [DOI] [PubMed] [Google Scholar]
- Levine B, Kroemer G. Autophagy in the pathogenesis of disease. Cell. 2008;132:27–42. doi: 10.1016/j.cell.2007.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawauchi K, Ogasawara T, Yasuyama M, Ohkawa S. Involvement of Akt kinase in the action of STI571 on chronic myelogenous leukemia cells. Blood Cells Mol Dis. 2003;31:11–7. doi: 10.1016/s1079-9796(03)00070-6. [DOI] [PubMed] [Google Scholar]
- Li Z, Tan F, Liewehr DJ, Steinberg SM, Thiele CJ. In vitro and in vivo inhibition of neuroblastoma tumor cell growth by AKT inhibitor perifosine. J Natl Cancer Inst. 2010;102:758–70. doi: 10.1093/jnci/djq125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han J, Hou W, Goldstein LA, Lu C, Stolz DB, Yin XM, et al. Involvement of protective autophagy in TRAIL resistance of apoptosis-defective tumor cells. J Biol Chem. 2008;283:19665–77. doi: 10.1074/jbc.M710169200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ertmer A, Huber V, Gilch S, Yoshimori T, Erfle V, Duyster J, et al. The anticancer drug imatinib induces cellular autophagy. Leukemia. 2007;21:936–42. doi: 10.1038/sj.leu.2404606. [DOI] [PubMed] [Google Scholar]
- Kamitsuji Y, Kuroda J, Kimura S, Toyokuni S, Watanabe K, Ashihara E, et al. The Bcr-Abl kinase inhibitor INNO-406 induces autophagy and different modes of cell death execution in Bcr-Abl-positive leukemias. Cell Death Differ. 2008;15:1712–22. doi: 10.1038/cdd.2008.107. [DOI] [PubMed] [Google Scholar]
- Bellodi C, Lidonnici MR, Hamilton A, Helgason GV, Soliera AR, Ronchetti M, et al. Targeting autophagy potentiates tyrosine kinase inhibitor-induced cell death in Philadelphia chromosome-positive cells, including primary CML stem cells. J Clin Invest. 2009;119:1109–23. doi: 10.1172/JCI35660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu L, Kim YA, Wang X, Wu X, Yue P, Lonial S, et al. Perifosine inhibits mammalian target of rapamycin signaling through facilitating degradation of major components in the mTOR axis and induces autophagy. Cancer Res. 2009;69:8967–76. doi: 10.1158/0008-5472.CAN-09-2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degtyarev M, De Mazière A, Orr C, Lin J, Lee BB, Tien JY, et al. Akt inhibition promotes autophagy and sensitizes PTEN-null tumors to lysosomotropic agents. J Cell Biol. 2008;183:101–16. doi: 10.1083/jcb.200801099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu CT, Zhu J, Dagda R. Beclin 1-independent pathway of damage-induced mitophagy and autophagic stress: implications for neurodegeneration and cell death. Autophagy. 2007;3:663–6. doi: 10.4161/auto.4625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarlatti F, Maffei R, Beau I, Ghidoni R, Codogno P. Non-canonical autophagy: an exception or an underestimated form of autophagy. Autophagy. 2008;4:1083–5. doi: 10.4161/auto.7068. [DOI] [PubMed] [Google Scholar]
- Scarlatti F, Maffei R, Beau I, Codogno P, Ghidoni R. Role of non-canonical Beclin 1-independent autophagy in cell death induced by resveratrol in human breast cancer cells. Cell Death Differ. 2008;15:1318–29. doi: 10.1038/cdd.2008.51. [DOI] [PubMed] [Google Scholar]
- Smith DM, Patel S, Raffoul F, Haller E, Mills GB, Nanjundan M. Arsenic trioxide induces a beclin-1-independent autophagic pathway via modulation of SnoN/SkiL expression in ovarian carcinoma cells. Cell Death Differ. 2010;17:1867–81. doi: 10.1038/cdd.2010.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishida Y, Arakawa S, Fujitani K, Yamaguchi H, Mizuta T, Kanaseki T, et al. Discovery of Atg5/Atg7-independent alternative macroautophagy. Nature. 2009;461:654–8. doi: 10.1038/nature08455. [DOI] [PubMed] [Google Scholar]
- Gao P, Bauvy C, Souquère S, Tonelli G, Liu L, Zhu Y, et al. The Bcl-2 homology domain 3 mimetic gossypol induces both Beclin 1-dependent and Beclin 1-independent cytoprotective autophagy in cancer cells. J Biol Chem. 2010;285:25570–81. doi: 10.1074/jbc.M110.118125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia HG, Zhang L, Chen G, Zhang T, Liu J, Jin M, et al. Control of basal autophagy by calpain1 mediated cleavage of ATG5. Autophagy. 2010;6:61–6. doi: 10.4161/auto.6.1.10326. [DOI] [PMC free article] [PubMed] [Google Scholar]