Abstract
Purpose
The goal of this study was to determine the dose contributions from image guided adaptive brachytherapy (IGABT) to individual suspicious pelvic lymph nodes (pLNN) in cervical cancer patients. Data were collected in two cancer centers, University of Pittsburgh Cancer Institute (UPCI) and University Medical Center Utrecht (UMCU).
Material and methods
27 and 15 patients with node positive cervical cancer treated with HDR (high dose rate) or PDR (pulsed dose rate)-IGABT were analyzed. HDR-IGABT (UPCI) was delivered with CT/MRI compatible tandem-ring applicators with 5.0-6.0 Gy × five fractions. PDR-IGABT (UMCU) dose was delivered with Utrecht tandem-ovoid applicators with 32 × 0.6 Gy × two fractions. Pelvic lymph nodes with short axis diameter of ≥ 5 mm on pre-treatment MRI or PET-CT were contoured for all BT-plans. Dose contributions to individual pLNN expressed as D90 (dose to 90% of the volume) were calculated from dose-volume histograms as absolute and relative physical dose (% of the reference dose) for each fraction. For each node, the total dose from all fractions was calculated, expressed in EQD2 (equivalent total dose in 2 Gy fractions).
Results
Fifty-seven (UPCI) and 40 (UMCU) individual pLNN were contoured. The mean D90 pLNN was 10.8% (range 5.7-25.1%) and 20.5% (range 6.8-93.3%), respectively, and therefore different in the two centers. These values translate into 2.7 Gy (1.3-6.6 Gy) EQD2 and 7.1 Gy (2.2-36.7 Gy) EQD2, respectively. Differences are caused by the location of the individual nodes in relation to the spatial dose distribution of IGABT, differences in total dose administered and radiobiology (HDR versus PDR).
Conclusions
The IGABT dose contribution to individual pelvic nodes depends on patient and treatment related factors, and varies considerably.
Keywords: brachytherapy, cervical cancer, dosimetry, HDR, MRI-guidance, PDR
Purpose
The combination of external beam radiotherapy (EBRT), chemotherapy and brachytherapy (BT) is the standard treatment of locally advanced cervical cancer. Image-guided adaptive brachytherapy (IGABT) has been widely adopted during the last years [1, 2] and guidelines have been published for treatment planning and dose reporting [3, 4]. The main advantage is dose-volume optimization, allowing adjustments to the classical pear-shaped isodose patterns according to tumor regression during treatment and residual disease at the time of BT. Literature shows that combined EBRT and BT (especially IGABT) is curative for many patients with especially high local control rates [5–7]. However, regional recurrences do occur in the pelvic lymph nodes (pLNN) within and adjacent to radiotherapy fields [8]. Most regional recurrences include a component of marginal failure, suggesting a deficit in target volume coverage and dose delivered to suspicious nodes [9]. From earlier publications we know that brachytherapy contributes to the pelvic nodal dose [10, 11], but so far there is no data reported for MRI guided IGABT.
The purpose of this study was to determine the dose contributions from image guided adaptive brachytherapy (IGABT) to individual suspicious pLNN in cervical cancer patients. Data was collected in two cancer centers, University of Pittsburgh Cancer Institute (UPCI) and University Medical Center Utrecht (UMCU).
Material and methods
We performed a combined analysis of IGABT data in two institutes; University of Pittsburgh Cancer Institute (UPCI, USA) and University Medical Center Utrecht (UMCU, The Netherlands).
Patients and treatment
University of Pittsburgh Cancer Institute
Twenty-seven patients with International Federation of Gynecology and Obstetrics (FIGO) stage IB to IIIB cervical cancer and enlarged pLNN were treated between January 2007 and December 2010 with IGABT high dose rate (HDR) applications. The patients received EBRT to the pelvis or combined pelvic and para-aortic region to 45 Gy in 25 fractions. The dose to suspicious pLNN was delivered with simultaneous integrated boosts (55 Gy in 25 fractions). Brachytherapy was scheduled once a week during the fourth or fifth week of treatment, and twice a week after completion of the EBRT. Computed tomography (CT)/magnetic resonance imaging (MRI) compatible tandem-ring applicators (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden) were used with MRI-based planning for the first BT fraction followed by CT-based planning for subsequent treatments [6, 12]. The tandem length ranged from 40 to 60 mm, the ring- tandem angle was 45° to 60°, and ring diameter was 26-34 mm. All patients were treated with 5 HDR fractions of 5.0-6.0 Gy per fraction (reference dose) depending on the stage of disease and response to treatment. Planning aim was to cover 90% of the HR-CTV volume with the reference dose. Treatment planning optimization was performed using a combination of graphical and manual tools. For every patient, body mass index (BMI) was calculated.
University Medical Center Utrecht
Fifteen patients with FIGO stage IBI to IVA cervical cancer and enlarged pLNN were treated between May 2009 and September 2011. Treatment consisted of EBRT to the clinical target volume as described by van de Bunt et al. [13] combined with 3D image-guided intracavitary or combined intracavitary/interstitial pulsed dose rate (PDR) BT applications. The EBRT dose was 45 Gy in 25 fractions. Brachytherapy consisted of two PDR applications of 32 pulses of 0.6 Gy (2 × 19.2 Gy planning aim) with the first insertion after 22 EBRT fractions, and the second one after completion of EBRT. Pulsed dose rate was delivered in a 24-hour schedule, one pulse per hour. Dose was prescribed to 90% of the HR-CTV volume. Treatment planning optimization was performed using a combination of graphical and manual tools. Brachytherapy was performed using the Utrecht Interstitial Applicator, a CT/MR compatible tandem-ovoid applicator that allows additional interstitial needle placement (Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden). For the first BT fraction, only the intracavitary part of the applicator was used. In six of the fifteen patients, the dose to 90% of the HR-CTV (D90 HR-CTV) of the first application did not meet the planning aim. In this group the second application was performed with 1-6 additional interstitial needles. The number of needles and their position and depth of insertion were based on dosimetric and spatial shortcomings of the first application. After BT, all patients received an additional 3D-conformal EBRT boost of 10 to 14 Gy in 5 to 7 fractions to suspicious pLNN, taking into account the dose contribution of BT. Also for these patients, BMI was calculated.
Imaging and contouring
University of Pittsburgh Cancer Institute
At UPCI, all 27 patients had MRI examination (GE SIGNA HD excite 1.5T, GE Health Care, Milwaukee, WI, USA); T2-weighted sequences with 3.5 mm slice thickness for the first BT fraction. For the following four fractions, a CT examination was performed (GE LightSpeed Ultra-64 slice per rotation, GE Health Care, Milwaukee, WI, USA) with 2.5 mm slice thickness. CT images were acquired without intravenous contrast, but with 60 ml diluted contrast injected into the bladder. HR-CTV and organs at risk (OAR) were contoured on an Eclipse™ workstation for each fraction, according to the GEC ESTRO recommendations [3, 4]. Thereafter, they were transferred to the Nucletron Plato Brachytherapy Planning system (version 14.3, Nucletron, an Elekta company, Elekta AB, Stockholm, Sweden) for three-dimensional planning.
University Medical Center Utrecht
At UMCU, all fifteen patients had MRI examination for each application (Gyroscan NT Intera 1.5 T, Philips Medical Systems, Best, The Netherlands) based on the institutional protocol, which includes T2-weighted turbo spin-echo images with 3 or 4.5 mm slice thickness, and a balanced steady-state free precession scan with a slice thickness of 1.5 mm for applicator reconstruction purposes [14]. HR-CTV and OAR were contoured in VolumeTool [15] according to GEC ESTRO recommendations [3, 4]. Contours were transferred into the Plato Brachytherapy Planning System, and applicator reconstruction and treatment planning was performed.
Node contouring
Gross nodal volume for each pLNN was contoured based on imaging information. Individual pLNN were contoured on the images performed for each BT fraction. Pre-treatment MRI or PET-CT information was used to guide identification of residual pLNN on BT scans. In case of complete response of the enlarged pLNN, the areas previously occupied by the individual nodes were contoured. Pelvic lymph nodes contours were generated by a specifically trained resident and verified by a radiation oncologist experienced in gynecological tumors in UPCI and UMCU, respectively.
Analysis
The dose contributions (D90) to each individual pLNN were calculated from dose-volume histograms (DVH) for each fraction; both as absolute physical dose and as percentage of the reference dose. The doses were expressed as biologically equivalent dose in 2 Gy fractions (EQD2) using LQ-model (with α/β = 10 for tumor, α/β = 3 for OAR and half time of repair of 1.5 hours) [16] and were added for all fractions. Furthermore, the D90 for the HR-CTVs were determined in EQD2. In order to get an estimate of the influence of radiobiology, the PDR data were recalculated as if given by HDR in 4 fractions of 7 Gy and scaled for OAR constraints (clinically used HDR schedule in our institute).
For every patient, we determined the total reference air kerma (TRAK). Total reference air kerma divided by the reference dose was considered as an indicator of the volume encompassed by the 100% isodose.
Anatomical nodal regions
The contoured pLNN were grouped by three physicians into anatomical nodal regions, based on Radiation Therapy Oncology Group (RTOG) definitions of pelvic nodal groups for intensity-modulated radiation therapy (IMRT) [17] and other published literature [18–20]. The common iliac region (CI) covers the area around the common iliac vessels from the aortic to iliac bifurcation. The internal iliac region (II) is defined as an area of 7 mm around and along the internal iliac vessels, excluding pLNN ventrally to external iliac vessels. From the point where the internal and external iliac vessels spread to a distance of more than 7 mm, the space around and along external iliac artery is called external iliac region (EI). The obturator region (OB) encompasses the space bordered by internal and external iliac regions.
Results
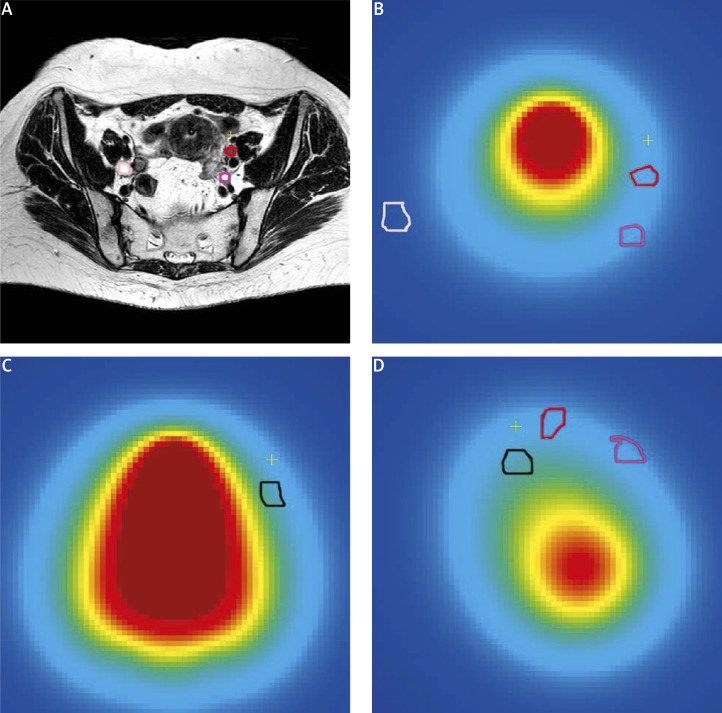
For patients characteristics see Table 1. In UPCI, 27 patients underwent 135 tandem-ring based HDR applications in total. Fifty-seven pLNN were detected with a minimum of 1 and a maximum of 9 per patient. The mean HR-CTV of these patients was 36.9 cm3 (range 21.0-59.8 cm3), and the mean BT D90 HR-CTV was 39.3 Gy (range 34.9-63.3 Gy) EQD2. The mean D90 received by the suspicious pLNN was 10.8% (range 5.7-25.1%) of the reference dose, corresponding to 2.7 Gy (range 1.3-6.6 Gy) EQD2. In UMCU, 15 patients underwent 30 PDR applications in total. Forty pLNN were detected with a minimum of 1 and a maximum of 5 per patient. The mean HR-CTV was 39.4 cm3 (range 15.9-115 cm3), and the mean BT D90 HR-CTV was 47.1 Gy (range 0.3-52.4 Gy) EQD2. The mean D90 of the pLNN was 20.5% (range 6.8-93.3%) resulting in 7.1 Gy (range 2.2-36.7 Gy) EQD2 (Table 2). Figure 1 shows an illustration of the 3D EQD2 distribution of a BT PDR fraction displaying pLNN with different locations and different dose contributions.
Table 1.
Patient characteristics
| UPCI | UMCU | |
| Patients (n) | 27 | 15 |
| Age (years) | ||
| Mean | 49 | 53 |
| Range | 29-83 | 27-79 |
| FIGO stage | ||
| IB1 | 1 | 1 |
| IB2 | 2 | 3 |
| IIA | 1 | 1 |
| IIB | 17 | 4 |
| IIIA | 0 | 0 |
| IIIB | 6 | 5 |
| IVA | 0 | 1 |
| Nodes (n) | 57 | 40 |
| BMI | ||
| Mean | 30 | 25 |
| Range | 18-41 | 19-32 |
UPCI – University of Pittsburgh Cancer Institute, UMCU – University Medical Center Utrecht, BMI – body mass index
Table 2.
Results
| UPCI | UMCU | |||||||
|---|---|---|---|---|---|---|---|---|
| HDR | PDR | Recalculated for HDR** | ||||||
| 57 pLNN | All 40 pLNN | Selection 35 pLNN | Selection 35 pLNN | |||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Volume HR-CTV (cm3) | 36.9 | 10 | 39.4 | 28 | 39.4 | 28 | 39.4 | 28 |
| D90 HR-CTV (Gy EQD2) | 39.3 | 5.2 | 47.1 | 3 | 47.1 | 3.1 | 41.2 | 4.9 |
| D90 pLNN/Ref. dose (%) | 10.8 | 5.1 | 20.5 | 15 | 16.7 | 7.2 | 16.7 | 7.2 |
| D90 pLNN (Gy EQD2) | 2.7 | 1.4 | 7.1 | 5.9 | 5.6 | 2.5 | 3.9 | 1.9 |
UPCI – University of Pittsburgh Cancer Institute, UMCU – University Medical Center Utrecht, HDR – high dose-rate, PDR – pulsed dose-rate, pLNN – pathologically enlarged pelvic lymph-nodes, SD – standard deviation, HR-CTV – high risk-CTV, D90 – dose to 90% of the volume, ref. dose – reference dose, EQD2 – biologically equivalent dose in 2-Gy fractions
PDR data were recalculated as if given by HDR in 4 fractions of 7 Gy and scaled for OAR constraints
Fig. 1.
Illustration of a transversal T2 weighted MR image (A) and corresponding 3D dose distribution in EQD2 of a brachytherapy pulsed dose rate fraction presented in three slices: (B) transversal, (C) coronal and (D) sagittal view. Four pelvic lymph nodes are delineated (colored contours). Blue = 0 and Red > 20 Gy EQD2, yellow cross indicates common point for all images
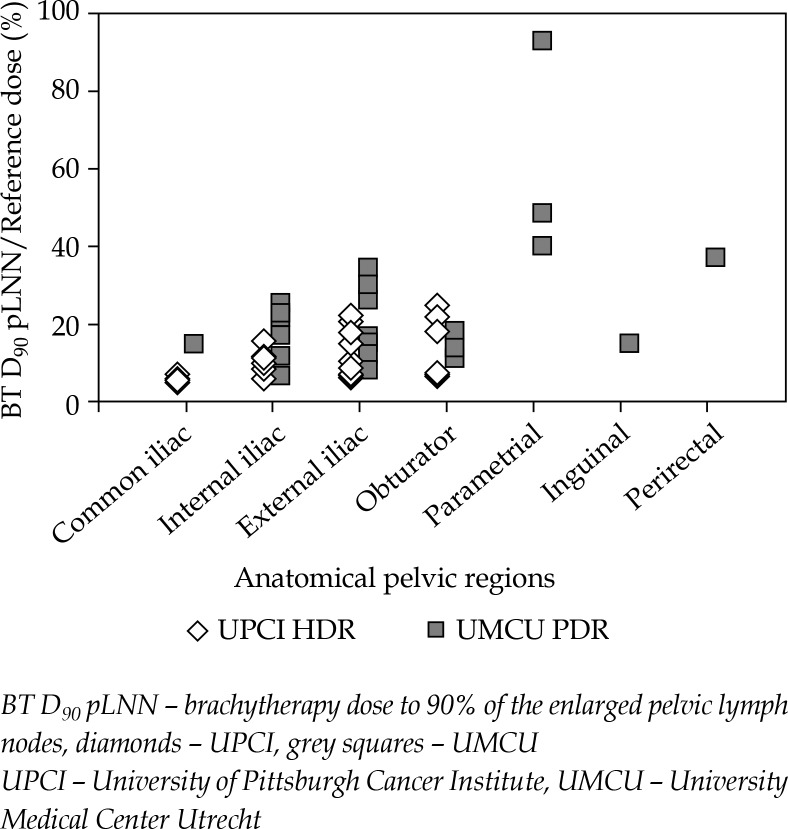
Table 3 and Figure 2 show the dose contributions of IGABT to the different nodal regions. In UPCI, but not in UMCU we saw a tendency that dose decreases from obturator to external, internal and common iliac nodes. The dose contributions of IGABT to individual pLNN varied impressively in both centers (range ∼5 to > 90% of the reference dose). After having excluded the few parametrial, inguinal and peri-rectal nodes from the UMCU data set (leaving 35 pLNN for the comparison; see Table 2), the nodes received on average 16.7% (range 6.8-34.7%) of the reference dose, corresponding to 5.6 Gy (range 2.2-12.0 Gy) EQD2. Furthermore, recalculating the UMCU PDR into HDR values, resulted in a reduced mean D90 of 3.9 Gy (range 1.5-8.2 Gy) EQD2, and a smaller difference with UPCI values.
Table 3.
Results for different nodal regions
| Nodal region | UPCI | UMCU | ||||||
|---|---|---|---|---|---|---|---|---|
| D90 pLNN (Gy EQD2) | D90 pLNN (Gy EQD2) | |||||||
| n | Mean | SD | Range | n | Mean | SD | Range | |
| Common ililac | 4 | 1.6 | 0.2 | 1.4-2.5 | 1 | 5 | ||
| Internal iliac | 14 | 2.4 | 0.8 | 1.3-6.6 | 11 | 4.7 | 2.3 | 2.2-8.7 |
| External iliac | 32 | 2.8 | 1.4 | 1.3-6.0 | 18 | 6.2 | 2.9 | 2.7-12.0 |
| Obturator | 7 | 3.4 | 2.2 | 1.7-5.7 | 5 | 5.3 | 1.1 | 3.7-6.3 |
| Parametrial | 0 | 3 | 22.8 | 12.2 | 14.2-36.7 | |||
| Inguinal | 0 | 1 | 5.1 | |||||
| Perirectal | 0 | 1 | 13 | |||||
UPCI – University of Pittsburgh Cancer Institute, UMCU – University Medical University Utrecht, pLNN – pathologically enlarged pelvic lymph-nodes, D90 – dose to 90% of the volume, EQD2 – biologically equivalent dose in 2-Gy fractions, SD – standard deviation
Fig. 2.
Relative dose contributions of PDR and HDR treatments to individual lymph nodes in the different pelvic regions; dose variations indicated between and within anatomical regions
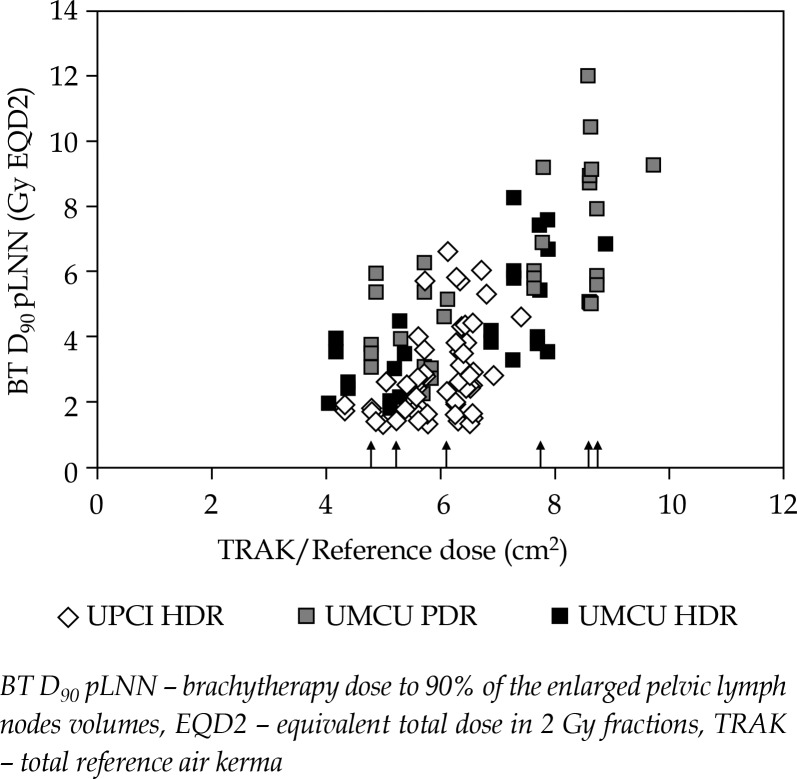
Figure 3 shows the D90 pLNN as function of TRAK per reference dose (as surrogate of the 100% isodose volume). The irradiated volumes of UMCU are in general larger than the ones of UPCI. This overall results in higher dose contributions to the pLNN in UMCU, irrespective of PDR or HDR calculations. The addition of interstitial needles for the second BT fractions in six of the UMCU patients did not influence the D90 pLNN systematically; see wide range of values for those cases in Figure 3.
Fig. 3.
Dose contributions to individual lymph nodes as function of TRAK/Reference Dose; TRAK/Reference Dose is considered an indicator for the volume encompassed by the 100% isodose. Arrows indicate cases treated with a combined intracavitary/interstitial approach. Diamonds – UPCI (HDR). Grey squares – UMCU (PDR). Black squares – UMCU recalculated for HDR. The differences between black and grey squares show that the BT dose contribution (in EQD2) to pLNN is influenced by dose rate
Body mass index was 25 (range 19-32) in UMCU patients and 30 (range 18-41) in UPCI patients, respectively, without a relation between physical D90 dose to the nodes and BMI.
Discussion
To our knowledge, this retrospective inter-institutional study represents the first dosimetric analysis of MRI based IGABT dose-contributions to pelvic lymph nodes in patients with advanced cervical cancer. Since the introduction of image guided BT, local control in cervical cancer has increased [5, 7], but regional control is still a matter of concern [6, 9]. Additionally, modern imaging modalities allow a better visualization of pLNN [21] and help to consider them suspicious or not, which influences our intentions to treat nodal disease.
For accurate dose reporting and for our understanding of nodal dose response relations it is essential to learn how EBRT and BT contribute to the treatment of individual affected lymph nodes. More detailed information on the dose administered per node will also help us to further optimize nodal boosting.
Isodose patterns of traditional Manchester system BT are pear shaped and symmetrical. Point B in this system was thought to give an estimate of the dose contribution to the lateral parametrium and the regional nodes. It is located at the level of point A, 5 cm lateral from the center of the tandem and gets approximately 15% to 25% of the point A dose. Lee et al. [10] already showed that the point B dose is not a good surrogate for the dose to pelvic nodes. In that study, the nodal regions defined on CT scans were overlaid with the BT dose distributions showing significantly lower dose to nodal groups than to point B (on average 5 vs. 7 Gy). Additionally, it was documented that there is some variation in dose delivered to the different nodal groups, defined as internal iliac, external iliac, and obturator nodes.
In our study, we investigated the contribution of individualized IGABT to the pLNN. We computed the BT dose to individual nodes located in the different groups by using the images at time of BT and the optimized BT treatment plans. We found a variety of dose levels in individual nodes and patients, but no general dose level differences when comparing the earlier defined nodal groups. This finding might be due to the fact that the spatial dose distributions of IGABT in the central pelvis can be quite asymmetric as they follow the target and OAR locations and shapes. It can therefore be expected that individualized IGABT also individually contributes to different pLNN with the highest values to nodes in the vicinity of the HR-CTV and high dose regions. Based on the data presented here, we consider to calculate the IGABT dose for the individual nodes, especially when EBRT boosting is part of the treatment schedule. Dose calculation for the different nodal regions is a rougher estimate and might still be used if individual node dose calculation is not possible.
We found astonishing pLNN dose level differences in and between the two cancer centers. The IGABT dose contributions to pLNN in UPCI were on average lower than the ones in UMCU. Several factors were investigated in order to explain these findings. Part of the difference was caused by the fact that in some UMCU patients, different from UPCI, pLNN were identified in the vicinity of the HR-CTV, especially in parametrium and perirectally. After excluding these nodes and their corresponding high D90 values, the dose level difference was smaller. Another part of the difference is accounted for radiobiology. After having recalculated the UMCU PDR contributions to pLNN into HDR values, the difference in dose again was smaller, but still remained. This lasting difference is due to the fact that the prescribed and administered tumor dose in UMCU is in principal higher, irrespective of the underlying radiobiology. The on average higher D90 HR-CTV values in UMCU are corresponding to higher totally administered doses and larger BT volumes irradiated to the reference dose.
.
Conclusions
The IGABT dose contribution to individual pLNN depends on patient and treatment related factors and varies considerably. The difference is caused by the positions of the individual nodes in relation to the radiation source, by differences in radiobiology and by individual treatment planning, and spatial dose delivery to specific HR-CTV and OAR locations and shapes. Based on the data presented here, calculation of the BT dose to the individual pLNN for nodal dose reporting and individual node boost planning should be considered. Dose calculations for the different nodal regions is a rougher estimate and can be used as alternative if individual node dose calculation is not possible.
Acknowledgements
Research conducted at: Department of Radiation Oncology, University Medical Center Utrecht, The Netherlands.
Disclosure
Authors report no conflict of interest.
References
- 1.Dimopoulos JC, De Vos V, Berger D, et al. Inter-observer comparison of target delineation for MRI-assisted cervical cancer brachytherapy: application of the GYN GEC-ESTRO recommendations. Radiother Oncol. 2009;91:166–172. doi: 10.1016/j.radonc.2008.10.023. [DOI] [PubMed] [Google Scholar]
- 2.Viswanathan AN, Erickson BA. Three-dimensional imaging in gynecologic brachytherapy: a survey of the American Brachytherapy Society. Int J Radiat Oncol Biol Phys. 2010;76:104–109. doi: 10.1016/j.ijrobp.2009.01.043. [DOI] [PubMed] [Google Scholar]
- 3.Haie-Meder C, Pötter R, Van Limbergen E, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2005;74:235–245. doi: 10.1016/j.radonc.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 4.Pötter R, Haie-Meder C, Van Limbergen E, et al. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol. 2006;78:67–77. doi: 10.1016/j.radonc.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Pötter R, Georg P, Dimopoulos JC, et al. Clinical outcome of protocol based image (MRI) guided adaptive brachytherapy combined with 3D conformal radiotherapy with or without chemotherapy in patients with locally advanced cervical cancer. Radiother Oncol. 2011;100:116–123. doi: 10.1016/j.radonc.2011.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beriwal S, Kannan N, Kim H, et al. Three-dimensional high dose rate intracavitary image-guided brachytherapy for the treatment of cervical cancer using a hybrid magnetic resonance imaging/computed tomography approach: feasibility and early results. Clin Oncol (R Coll Radiol) 2011;23:685–690. doi: 10.1016/j.clon.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Nomden CN, de Leeuw AA, Roesink JM, et al. Clinical outcome and dosimetric parameters of chemo-radiation including MRI guided adaptive brachytherapy with tandem-ovoid applicators for cervical cancer patients: a single institution experience. Radiother Oncol. 2013;107:69–74. doi: 10.1016/j.radonc.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 8.Eifel PJ, Winter K, Morris M, et al. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: an update of radiation therapy oncology group trial (RTOG) 90-01. J Clin Oncol. 2004;22:872–880. doi: 10.1200/JCO.2004.07.197. [DOI] [PubMed] [Google Scholar]
- 9.Beadle BM, Jhingran A, Yom SS, et al. Patterns of regional recurrence after definitive radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2010;76:1396–1403. doi: 10.1016/j.ijrobp.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 10.Lee LJ, Sadow CA, Russell A, et al. Correlation of point B and lymph node dose in 3D-planned high-dose-rate cervical cancer brachytherapy. Int J Radiat Oncol Biol Phys. 2009;75:803–809. doi: 10.1016/j.ijrobp.2008.11.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee YC, Rash DL, Stern RL, et al. The equivalent dose contribution from high-dose-rate brachytherapy to positive pelvic lymph nodes in locally advanced cervical cancer. Brachytherapy. 2013;12:555–559. doi: 10.1016/j.brachy.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Nag S, Erickson B, Thomadsen B, et al. The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2000;48:201–211. doi: 10.1016/s0360-3016(00)00497-1. [DOI] [PubMed] [Google Scholar]
- 13.van de Bunt L, van der Heide UA, Ketelaars M, et al. Conventional, conformal, and intensity-modulated radiation therapy treatment planning of external beam radiotherapy for cervical cancer: The impact of tumor regression. Int J Radiat Oncol Biol Phys. 2006;64:189–196. doi: 10.1016/j.ijrobp.2005.04.025. [DOI] [PubMed] [Google Scholar]
- 14.De Leeuw AA, Moerland MA, Nomden C, et al. Applicator reconstruction and applicator shifts in 3D MR-based PDR brachytherapy of cervical cancer. Radiother Oncol. 2009;93:341–346. doi: 10.1016/j.radonc.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Bol GH, Kotte AN, van der Heide UA, et al. Simultaneous multi-modality ROI delineation in clinical practice. Comput Methods Programs Biomed. 2009;96:133–140. doi: 10.1016/j.cmpb.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 16.Lang S, Kirisits C, Dimopoulos J, et al. Treatment planning for MRI assisted brachytherapy of gynecologic malignancies based on total dose constraints. Int J Radiat Oncol Biol Phys. 2007;69:619–627. doi: 10.1016/j.ijrobp.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 17.Small W, Jr, Mell LK, Anderson P, et al. Consensus guidelines for delineation of clinical target volume for intensity-modulated pelvic radiotherapy in postoperative treatment of endometrial and cervical cancer. Int J Radiat Oncol Biol Phys. 2008;71:428–434. doi: 10.1016/j.ijrobp.2007.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taylor A, Rockall AG, Reznek RH, et al. Mapping pelvic lymph nodes: guidelines for delineation in intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys. 2005;63:1604–1612. doi: 10.1016/j.ijrobp.2005.05.062. [DOI] [PubMed] [Google Scholar]
- 19.Toita T, Ohno T, Kaneyasu Y, et al. A consensus-based guideline defining the clinical target volume for pelvic lymph nodes in external beam radiotherapy for uterine cervical cancer. Jpn J Clin Oncol. 2010;40:456–463. doi: 10.1093/jjco/hyp191. [DOI] [PubMed] [Google Scholar]
- 20.Taylor A, Rockall AG, Powell ME. An atlas of the pelvic lymph node regions to aid radiotherapy target volume definition. Clin Oncol (R Coll Radiol) 2007;19:542–550. doi: 10.1016/j.clon.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 21.Havrilesky LJ, Kulasingam SL, Matchar DB, et al. FDG-PET for management of cervical and ovarian cancer. Gynecol Oncol. 2005;97:183–191. doi: 10.1016/j.ygyno.2004.12.007. [DOI] [PubMed] [Google Scholar]