Abstract
In cells of Old World and some New World monkeys, dominant factors restrict human immunodeficiency virus type 1 (HIV-1) infections after virus entry. The simian immunodeficiency virus SIVmac is less susceptible to these restrictions, a property that is determined largely by the viral capsid protein. For this study, we altered exposed amino acid residues on the surface of the HIV-1 capsid, changing them to the corresponding residues found on the SIVmac capsid. We identified two distinct pathways of escape from early, postentry restriction in monkey cells. One set of mutants that were altered near the base of the cyclophilin A-binding loop of the N-terminal capsid domain or in the interdomain linker exhibited a decreased ability to bind the restricting factor(s). Consistent with the location of this putative factor-binding site, cyclophilin A and the restricting factor(s) cooperated to achieve the postentry block. A second set of mutants that were altered in the ridge formed by helices 3 and 6 of the N-terminal capsid domain efficiently bound the restricting factor(s) but were resistant to the consequences of factor binding. These results imply that binding of the simian restricting factor(s) is not sufficient to mediate the postentry block to HIV-1 and that SIVmac capsids escape the block by decreases in both factor binding and susceptibility to the effects of the factor(s).
The Gag proteins of the lentiviruses human immunodeficiency virus type 1 (HIV-1) and simian immunodeficiency virus (SIV) are essential for critical steps in the viral life cycle, including virion assembly and uncoating. The Gag precursor protein is synthesized as a 55-kDa polyprotein which is myristylated and subsequently localized to the plasma membrane, where it recruits other viral components that are important for infectivity (26). In addition, a number of host factors appropriated by the virus (Tsg101, ubiquitin, ERK2, cyclophilin A [CypA], and topoisomerase I) interact specifically with elements of the HIV-1 Gag polyprotein and contribute to assembly, release, and subsequent postentry events in the viral life cycle (11, 19, 24, 27, 41-43, 47). After the release of viral particles, virions undergo a maturation process during which the viral protease cleaves the HIV-1 Gag polyprotein into four mature proteins: p17 matrix (MA), p24 capsid (CA), p7 nucleocapsid (NC), and p6 (20). This late cleavage event triggers a structural rearrangement in which the matrix protein remains associated with the viral envelope and the viral CA protein ultimately condenses into a conical structure that encapsulates the viral RNA genome, which is complexed with NC. Maturation is required for the subsequent infectivity of virions and negotiation of the early steps of retroviral replication in the target cell after infection (48).
The early events in the HIV-1 life cycle immediately following virus entry are poorly understood. Presumably, the HIV-1 CA core is released into the cytoplasm of the target cell, where uncoating releases the reverse transcription complex. Recent evidence suggests that HIV-1 reverse transcription begins in an intact viral core but that core disassembly is necessary for the process to continue (38). Disassembly of the core must occur rapidly, as very little CA protein can be found associated with the reverse transcription complex (17). Uncoating events are likely to be relevant to HIV-1 tropism restrictions in cells of some nonhuman primate species, given the substantial reduction in reverse transcription products detected in newly infected cells (2, 15, 29). Thus, although HIV-1 entry into cells of several Old World monkey species is efficiently supported by simian CD4 and chemokine coreceptors (14, 35), HIV-1 infection of these cells is restricted at a postentry step (2, 3, 15, 28, 31, 45). Old World monkeys are natural hosts for SIVmac, which is not susceptible to postentry restrictions in these cells (16, 30, 31). However, SIVmac encounters postentry restrictions in most New World monkey cells (31). Similar restrictions for some murine leukemia viruses have been observed with human cells (44). By examining the infection of heterokaryons and by performing infections in the presence of competitor viruses, the cellular factors responsible for retroviral restriction have been demonstrated to be dominant and saturable (2, 3, 15, 28, 37). A chimeric HIV-1 reporter virus in which the HIV-1 CA protein was largely replaced with the SIVmac CA sequence escaped the monkey cell restrictions, demonstrating that the CA protein of HIV-1 is an important viral determinant for susceptibility to postentry restriction (39). Conversely, an SIVmac chimera expressing the CA-p2 domain of HIV-1 was susceptible to postentry cellular restrictions in cells that were otherwise permissive for SIVmac (15, 39).
Recent studies have suggested that CypA interactions with the HIV-1 CA protein can increase the sensitivity of HIV-1 to postentry restrictions in the cells of owl monkeys, a New World species (32, 46). This effect could contribute to the ability of SIVmac to escape restriction in Old World monkey cells, as CypA does not bind to the SIVmac CA protein (7). However, replacement of the CypA-binding loop in HIV-1 CA with the corresponding SIVmac sequence does not result in escape from restriction in Old World monkey cell lines, even though CypA binding is eliminated by this substitution (32). Thus, although CypA binding can influence the degree of HIV-1 restriction in some monkey cells, it is not required for the observed postentry blocks. The treatment of some human target cells with cyclosporine (CspA), which binds CypA and blocks its interaction with the incoming HIV-1 capsids, results in decreases in infection (32, 46). These decreases have been suggested to be due to the interaction of the HIV-1 capsid with Ref-1, an early restriction factor for murine leukemia viruses in human cells (46). Thus, CypA can positively or negatively influence the action of restriction factors on HIV-1.
High-resolution X-ray crystal structures of the HIV-1 CA protein have been determined (1, 21, 22, 25). The CA protein is composed of distinct N- and C-terminal domains (NTD and CTD, respectively) separated by a short flexible linker. The prolyl isomerase CypA is incorporated into viral particles at a stoichiometry of approximately 1 molecule per 10 CA monomers by binding to an exposed proline-rich loop formed by residues 85 to 93 in the NTD (21). In permissive human cells, a disruption of CypA incorporation during assembly has been shown to be detrimental to the subsequent infectivity of viral particles (5-8, 19). CypA has been shown to catalyze the cis-trans isomerization of the G89/P90 peptide bond in the CypA-binding loop of the HIV-1 CA protein in vitro (4); however, the relevance of this activity to viral infectivity is uncertain in light of the finding that the bond is primarily trans both in the free protein and when complexed with CypA (21, 25).
HIV-1 assembly, budding, and maturation require the organization of CA proteins into much larger structures. The dimerization of purified CA protein occurs spontaneously in solution and is mediated by the CTD (22). Three-dimensional reconstructions of cryoelectron microscopy images of conical CA cores have revealed that the quaternary structure of the core is composed of CA hexamers (23, 34). Dimeric contacts between adjacent hexamers are formed between the CTDs of the CA protein and contribute to the stability of the conical core structure. These models predict that the surface of the NTD is exposed to the cytoplasm of the infected cell. This surface would be an attractive target for cellular restriction factors that may modulate the dissociation of the CA core. For example, the diameter of the holes formed at the center of the hexameric rings (∼25 Å) or between hexamers (∼107 Å) could potentially accommodate soluble host factors that may perturb the ability of the CA core to uncoat (34). Such a model is consistent with the observation that the block to HIV-1 infection in monkey cells occurs at a step prior to reverse transcription (15, 29, 37).
To understand the contribution of the HIV-1 CA protein to susceptibility to postentry restriction, we sought to mutagenize the solvent-accessible surface residues and determine the impact of these changes on postentry events in cells of various monkey species. In most cases, we altered the HIV-1HXBc2 sequence to that of SIVmac. Analyses of the phenotypes of the mutants revealed the existence of different pathways of escape from the early blocks to HIV-1 infection in monkey cells.
MATERIALS AND METHODS
Cell lines and primary cell cultures.
Adherent cells used for this study were grown in Dulbecco's modified Eagle medium supplemented with 10% fetal bovine serum and 1% penicillin-streptomycin at 37°C. Suspension cells were cultured in RPMI 1640 medium containing 10% fetal bovine serum and 1% penicillin-streptomycin. All cell lines used for this study, with the exception of primary macrophages, are described elsewhere (31, 39) or were obtained from the American Type Culture Collection. HeLa, C8166, and CEMx174 cells are of human origin; MK2D and Vero cells and primary rhesus lung (PRL) fibroblasts are derived from Old World monkeys; and owl monkey kidney (OMK) and Pindak cells are derived from New World monkeys.
Monocyte-derived primary macrophages were isolated from rhesus macaque whole blood on a Ficoll-Paque gradient, washed three times with phosphate-buffered saline (PBS), and seeded in each well of a 12-well plate in macrophage-driving medium (75% RPMI, 10% human AB serum, 15% conditioned medium from L929 fibroblasts, 10 mM HEPES, 10 μM β-mercaptoethanol, 12.5 ng of macrophage colony-stimulating factor/ml, 1 ng of granulocyte-macrophage colony-stimulating factor/ml, and antibiotics). Cultures were washed every 3 days for 2 weeks to remove nonadherent cells, and fresh medium was added back to each well.
Viral constructs.
The HIV-1HXBc2 nucleotide sequence 667 to 2048 was PCR amplified and blunt ligated into cloning vector pPCR-Script Amp (Stratagene). The resulting vector, pHgag1, was sequenced to verify the accuracy of the amplified region. Mutations were introduced into pHgag1 by the QuikChange protocol (Stratagene). The DNAs of the mutant constructs were subsequently sequenced to confirm the presence of mutations and to exclude the introduction of unwanted additional mutations. The mutated regions in pHgag1 encoding the HIV-1 capsid were subcloned by the insertion of BssHII-PspOMI fragments into pCMVΔP1ΔenvpA, a previously described HIV-1 Gag/Pol expression vector (40). The G89A mutant has been described previously (10) and was included here as a control.
The efficiency of a single round of HIV-1 infection was measured by using recombinant reporter viruses expressing green fluorescent protein (GFP) in place of Nef and pseudotyped with the vesicular stomatitis virus G glycoprotein (VSV-G). These HIV-GFP viruses were generated by cotransfecting 293T cells by calcium phosphate precipitation (13) with pHIvec2.GFP, wild-type (wt) or mutant pCMVΔP1ΔenvpA, pHCMV-G, and a Rev-expressing plasmid, as described previously (31, 39). Alternatively, virus-like particles (VLPs) lacking a reporter were generated by cotransfecting 293T cells with all of the above plasmids, except pHIvec2.GFP. All virus- and VLP-containing supernatants were cleared of cell debris by low-speed centrifugation and were quantitated by measurement of the reverse transcriptase (RT) activity as described previously (33). Supernatants were stored in aliquots at −80°C.
Infection assays.
HeLa, MK2D, OMK, Vero, PRL, and Pindak cells were plated at a density of 3 × 104 cells/well in 24-well plates the day before inoculation. C8166 and CEMx174 cells were plated at a density of 5 × 104 cells/well in a similar manner. Thawed medium containing recombinant HIV-1 was normalized on the basis of RT activity and was added to cells directly or in threefold serial dilutions in a total volume of 0.5 ml. In some experiments, target cells were treated with CspA (1 μg/ml; Sigma) 30 min prior to inoculation. To test the ability of the generated mutants to compete for restricting factors, we inoculated target cells simultaneously with VSV-G-pseudotyped wt or mutant VLPs in addition to the HIV-GFP reporter virus. Cells were incubated with recombinant viruses at 37°C for approximately 6 h before removal of the supernatants and the addition of 1.0 ml of fresh medium. Cells were subsequently incubated at 37°C for 3 days before being trypsinized if necessary and fixed in PBS containing 4% formaldehyde. The percentage of infected cells was determined by fluorescence-activated cell sorting (FACS; Becton Dickinson FACScan). The average vector infectivities and standard deviations were derived from at least two independent experiments.
Fluorescence microscopy of primary rhesus macaque macrophages and PRL cells was performed by using a fluorescein isothiocyanate filter set on a Nikon TE300 inverted microscope. Cells were infected with recombinant HIV-1 vectors and analyzed 3 days later by microscopy before being trypsinized and prepared for FACS.
Viral protein analysis and Western blotting.
Recombinant wt and mutant HIV-1 Gag/Pol expression vectors (pCMVΔP1ΔenvpA) were transfected into 293T cells as described above, without the addition of the pHCMV-G plasmid expressing the VSV-G envelope glycoprotein. Cells were cotransfected with or without 10 μg of SRα-CypA-HA, an expression vector for human cyclophilin A (CypA) containing an epitope tag derived from influenza virus hemagglutinin (HA) (9). Cells were washed 12 h after transfection and metabolically labeled with [35S]methionine (50 μCi/ml) for 24 h. Virions released into the supernatant were filtered (0.45-μm pore size) and pelleted through a 20% sucrose cushion (in PBS) for 90 min at 4°C and 27,000 rpm in a Beckman SW28 rotor. Pelleted viral particles were lysed in RIPA buffer (1× PBS-1% NP-40-0.5% sodium deoxycholate-0.05% sodium dodecyl sulfate [SDS]), normalized for 35S counts in a Beckman LS6500 scintillation counter, and either directly analyzed by SDS-polyacrylamide gel electrophoresis (PAGE) (12.5% resolving gel) and autoradiography or separated by SDS-PAGE (4 to 12% acrylamide) for Western blotting. Proteins were transferred, blotted with antisera, and detected by enhanced chemiluminescence (ECL; NEN). The primary antibody used for the detection of CypA-HA was a high-affinity rat anti-HA antibody (3F10) directly conjugated with horseradish peroxidase at a 1:500 dilution (Roche).
RESULTS
Mutagenesis strategy.
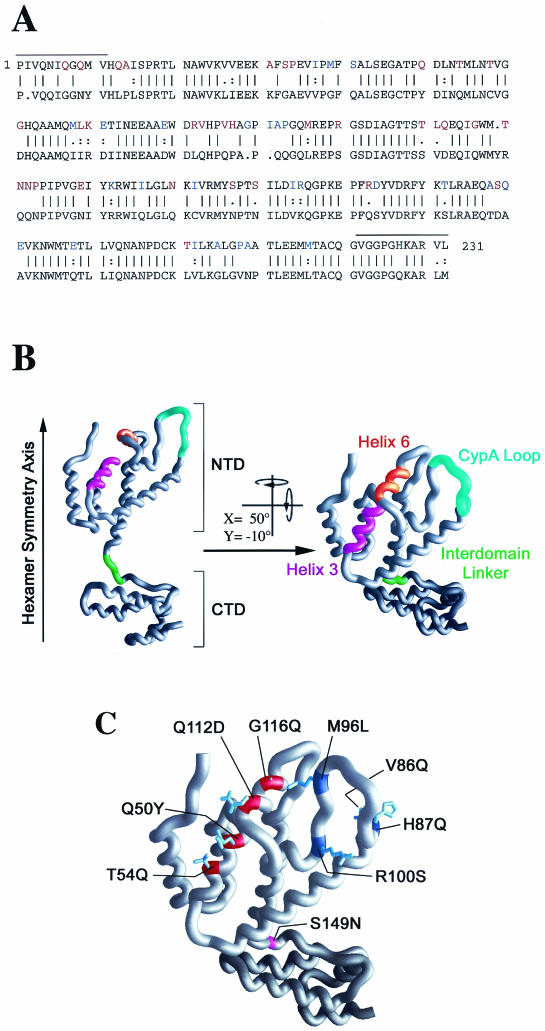
The CA proteins of HIV-1 and SIVmac have been identified as important viral determinants of susceptibility to postentry restrictions observed in Old World and New World monkeys, respectively (15, 39). We sought to characterize the region of the HIV-1 CA protein that is important for the susceptibility of HIV-1 to restriction in Old World monkey cells and OMK cells. Given that SIVmac is resistant to postentry restriction in these cells, we compared the amino acid sequences of the HIV-1HXBc2 and SIVmac CA proteins (Fig. 1A). The X-ray crystal structure of the HIV-1 CA protein (1, 21, 25) suggests that approximately 80% of the amino acid differences between the two proteins are solvent accessible in the HIV-1 CA (Fig. 1A, blue and red residues). We altered the residues in the HIV-1 CA protein that are shown in red in Fig. 1A; approximately 70% of the surface-accessible residues in the CA amino-terminal domain that exhibited differences between HIV-1 and SIVmac were altered in this study. Residues in the HIV-1HXBc2 sequence were changed to those found in the SIVmac capsid in most cases. Two exceptions were mutants L1 and L4, in which the HIV-1 CA residues were changed to the corresponding sequences of SIVCPZ and HIV-1MVP, respectively (Table 1). Residues were altered singly or in a variety of double and multiple combinations. For comparison purposes, the G89A mutant, which is deficient in CypA binding (10), was included in the study.
FIG. 1.
HIV-1 CA sequences. (A) The amino acid sequences of HIV-1HXBc2 (top) and SIVmac (bottom) CA proteins were aligned. Vertical lines indicate sequence identity and dots represent related residues. Differences between the two proteins in solvent-accessible residues were determined through the analysis of GRASP computer models of the molecular surface of the HIV-1 CA protein and are colored in the HIV-1 CA sequence (top). Residues that were changed in this study from the HIV-1 sequence to the SIVmac sequence are shown in red in the HIV-1 CA sequence. Horizontal lines above the HIV-1 sequence designate structurally indeterminate regions. (B) Structural model of the HIV-1 CA protein (1). The N- and C-terminal domains are designated NTD and CTD, respectively. The hexamer symmetry axis is indicated, with the arrow pointing towards the exterior of the viral core (34). With respect to the figure on the left, the right-hand figure was rotated 50° about the x axis and −10° about the y axis. From this perspective, the ridge formed at the interface of helices 3 (magenta) and 6 (orange) is evident. Also highlighted are the CypA-binding loop (cyan) and the interdomain linker (green). (C) Structure of the HIV-1 CA protein in the same orientation as that of the model at the right side of panel B. The three regions in which changes result in escape from postentry restrictions in monkey cells are highlighted as follows: the helix 3/6 ridge is red, the CypA-binding loop is blue, and the interdomain linker is magenta. The side chains of residues associated with the indicated changes are shown.
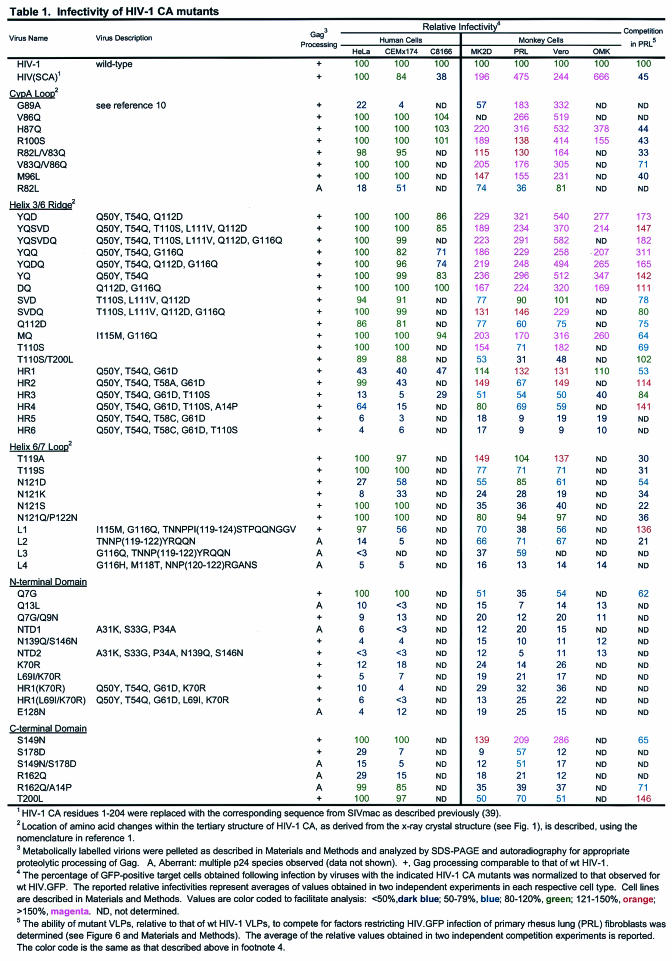
TABLE 1.
Three distinct regions of the CA protein contribute to escape from restriction in monkey cells.
The infectivities of recombinant viruses with mutant CA proteins were examined in a variety of human and monkey cell lines. To measure infection, we used HIV-1 reporter viruses expressing GFP and pseudotyped with VSV-G, as described previously (31, 39). Cells were infected with either wt or mutant reporter virus preparations normalized according to RT units (see Materials and Methods) and added either at the lowest concentration previously determined with wt HIV-1 to infect 100% of human cells or at a concentration that resulted in infection of approximately 20% of monkey cells. This protocol allowed us to determine which, if any, of the CA changes deleteriously affected the function of the CA protein during infection in permissive human cells while facilitating the identification of mutants that were less sensitive to postentry restrictions in monkey cells. The infectivities of viruses with selected CA mutants were also studied over a range of virus concentrations. All of the HIV-1 CA mutants used in this study were capable of producing virion particles (Table 1). The infectivities of the mutant virions, relative to those observed for wt HIV-1 in each cell type, are presented in Table 1. For convenience, values in blue represent relative infectivities of <80% of the wt HIV-1 value, whereas those in green represent viral infectivities of 80 to 120% that of wt HIV-1. Relative infectivities of >120% but <150% of the wt HIV-1 values are represented in orange. Magenta is used to identify relative infectivities of >150% that of wt HIV-1.
We identified three distinct regions within the CA protein that, when altered, allowed efficient HIV-1 infection of human cells and conferred on HIV-1 a level of infectivity in monkey cells comparable to that seen with the HIV(SCA) mutant reported previously (39). The HIV(SCA) mutant has most of the HIV-1 CA replaced with that of SIVmac and was included here as a positive control (Table 1; Fig. 2). Two CA regions associated with increased relative infectivities in monkey cells involved the base of the CypA-binding loop and a ridge formed at the interface of helices 3 and 6 (Fig. 1B and C). Additionally, a single amino acid change at Ser 149 in the interdomain linker, which results in the loss of a phosphorylation site (12), was found to confer an approximately two- to threefold increase in infectivity in simian cells. Notably, although the alteration of this amino acid to alanine has been reported to eliminate viral infectivity in permissive cells (12), a change to asparagine, the residue found in the SIVmac CA, is functionally tolerated. The G89A mutant, which is deficient in CypA binding, infected PRL and Vero cells more efficiently than wt HIV-1 (Table 1). However, unlike the other mutants with changes in the CypA-binding loop and increased relative infectivities in monkey cells, the G89A mutant infected human cells with an efficiency that was significantly lower than that of wt HIV-1.
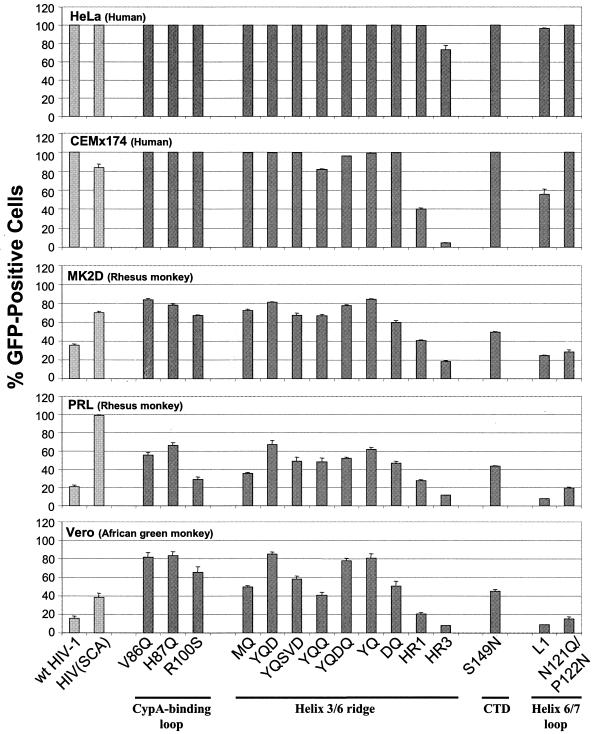
FIG. 2.
Infectivities of recombinant viruses with HIV-1 capsid changes. Cell supernatants containing recombinant wt HIV-GFP or HIV-GFP with the indicated capsid changes were assessed for RT activity. Then 5 × 104 RT units of virus was added to human, MK2D, and Vero cells, and 1 × 105 RT units of virus was added to PRL cells. Cells were incubated for 3 days prior to FACS analysis for GFP expression. The average percentages of GFP-expressing cells and the standard deviations were calculated from at least two independent experiments.
The infectivities of viruses with representative CA mutants involving the CypA loop and the helix 3/6 ridge, as well as the Ser 149 mutant, are compared in Fig. 2. Mutants L1 and N121Q/P122N are located in a loop between helices 6 and 7 which makes hydrogen bonding contacts with the CypA loop (1, 25). Although these mutants were infectious in human cells, they remained restricted in monkey cells and were thus included as internal negative controls. A titration of viruses with selected CA mutants is shown in Fig. 3.
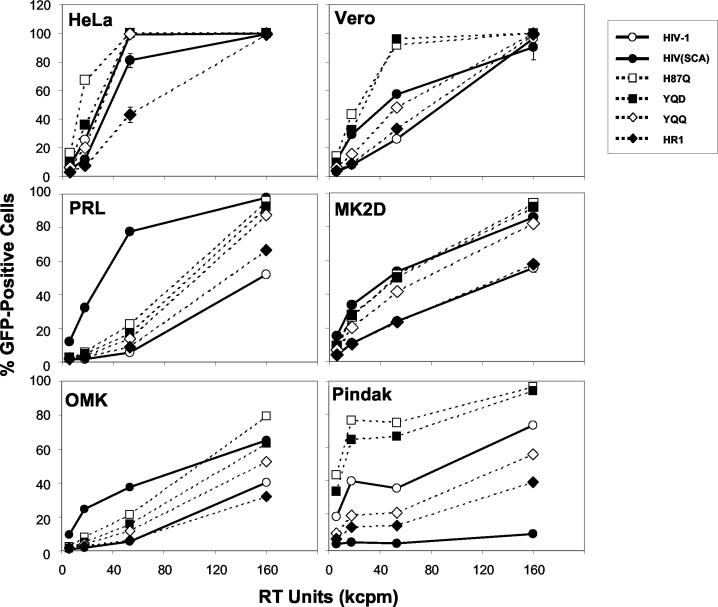
FIG. 3.
Infection of cells by recombinant viruses with changes in HIV-1 capsid. Cell supernatants containing the indicated GFP-expressing viruses were assayed for RT activity. Viruses were added to cells at 1.6 × 104 RT units/well or threefold serial dilutions thereof. Samples were incubated for 3 days and assayed for GFP expression by FACS analysis. The mean percentages of GFP-positive cells and standard deviations were calculated from two independent experiments. The cell lines used originated from the following species: HeLa, human; Vero, African green monkey; PRL, rhesus macaque; MK2D, rhesus macaque; OMK, owl monkey; and Pindak, squirrel monkey. The control wt HIV-1 and HIV(SCA) viruses are indicated by solid lines, and the mutant viruses are indicated by broken lines.
In general, the infectivities of the mutants were comparable in HeLa (human) cells. The HR1 and HR3 mutants contained the Q50Y and T54Q substitutions common to the YQD and YQQ mutants affecting the helix 3/6 ridge, but additional changes in glycine 61 and/or threonine 110 rendered these mutants more defective than the wt virus in most human cell lines examined (Fig. 2; Table 1).
The abilities of selected mutants to infect Old World monkey cells (MK2D, PRL, and Vero cells) and OMK cells, which are derived from the atypical New World monkey species owl monkeys, are compared in Fig. 2 and 3. The degree to which the substitution of the SIVmac capsid region in the HIV(SCA) mutant relieved the restriction to infection varied for the different cell types. The HIV(SCA) mutant exhibited a much higher level of infectivity than wt HIV-1 in PRL cells compared to other cell types. This probably reflects the fact that the chimeric nature of the HIV(SCA) construct results in some defectiveness in replication (39), and the relative impact of this property is less significant in cell lines such as PRL cells, in which the block to HIV-1 infection is stronger. The pattern of infectivities of the selected mutants in MK2D, PRL, Vero, and OMK cells was similar, suggesting that the HIV-1-restricting factors in these cells, and in the diverse monkey species from which they were derived, are related. Except in PRL cells, in which the infectivity of the HIV(SCA) mutant was particularly efficient, several mutants containing alterations in the CypA-binding loop, the helix 3/6 ridge, and Ser 149 exhibited infectivities that were comparable to or at a higher level than that of the HIV(SCA) mutant. We conclude that changes in distinct regions of the HIV-1 CA can decrease the susceptibility of HIV-1 to postentry restrictions in Old World and owl monkey cells.
We also examined the infectivities of selected HIV-1 CA mutants in Pindak cells, which are derived from a New World monkey (Bolivian squirrel monkey) that exhibits restrictions against SIVmac infection (31). With the exception of the HIV(SCA) mutant, which as expected (39) did not infect Pindak cells efficiently due to the presence of the SIVmac CA, the other mutants tested infected Pindak cells. The YQQ and HR1 mutants infected Pindak cells less efficiently than wt HIV-1, but they were not as restricted as the HIV(SCA) mutant. Thus, none of the introduced changes in the surface of HIV-1 CA was sufficient to confer complete susceptibility to the SIVmac-specific restriction factor(s) present in New World monkey cells.
Infectivity of HIV-1 capsid mutants in primary target cells restricted for HIV-1.
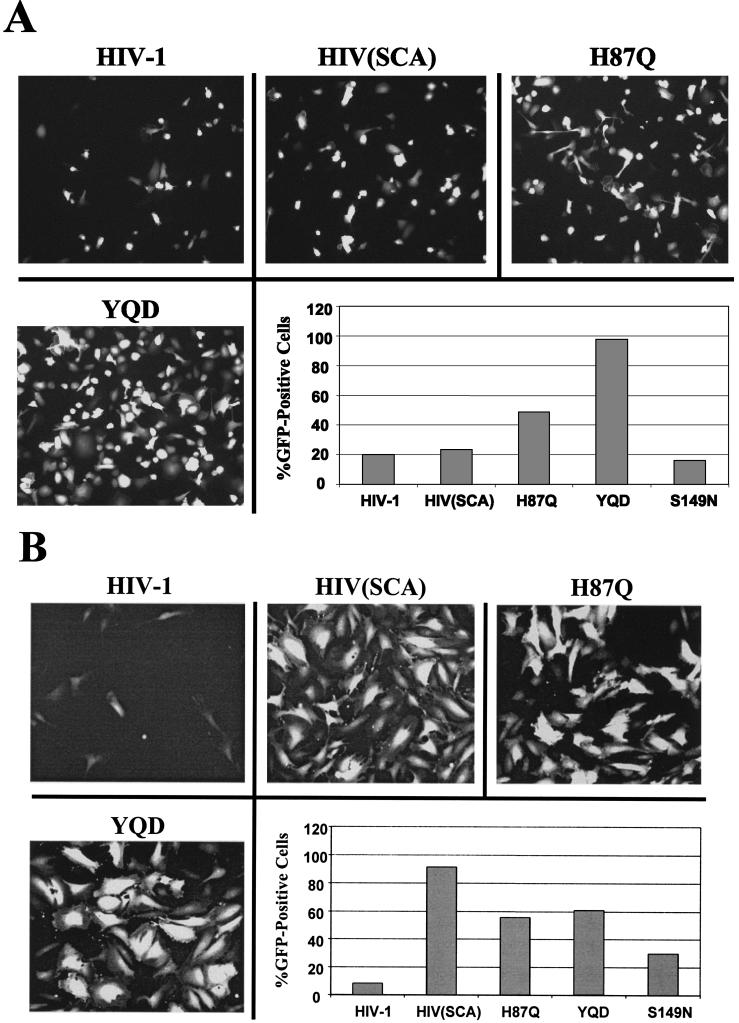
To examine the infectivities of the HIV-1 CA mutants in a target cell type that is relevant to natural HIV-1 infection, we infected primary rhesus monkey macrophages with a selected subset of mutants (Fig. 4A). In parallel, as a control, PRL fibroblasts were infected with the same virus samples (Fig. 4B). The HIV(SCA) mutant infected macrophages only marginally better than the wt virus, whereas for PRL cells, a ninefold increase in infection efficiency was observed for this mutant at the concentration of virus tested. The YQD mutant affecting the helix 3/6 ridge infected primary macrophages more efficiently than any of the mutants tested, whereas for PRL cells, the H87Q (in the CypA-binding loop) and YQD mutants were equally infectious, but not as infectious as the HIV(SCA) mutant. The S149N mutant was apparently restricted in primary macrophages; in contrast, a threefold increase in infection efficiency compared with that of the wt virus was observed in PRL fibroblasts. These data suggest that changes in both the CypA-binding loop and the helix 3/6 ridge can result in a decreased sensitivity of HIV-1 to restriction factors that are present in a biologically relevant simian cell type. However, there are some target cell-dependent differences in the infectivities of the mutants.
FIG. 4.
Infectivity of viruses in primary rhesus monkey cells. Mutant and wt reporter virus cell supernatants containing wt HIV-GFP and HIV-GFP with the indicated mutant capsids were normalized for RT activity and added at a concentration of 105 RT units/well to target cells. The target cells consisted of primary rhesus macaque macrophages purified from whole blood (A) or PRL fibroblasts (B). Cells were incubated with recombinant HIV-1 vectors for 3 days and then analyzed by microscopy and FACS. Fluorescence microscopy was performed by using a fluorescein isothiocyanate filter set on a Nikon TE300 inverted microscope. The results shown are representative of those obtained from two independent experiments.
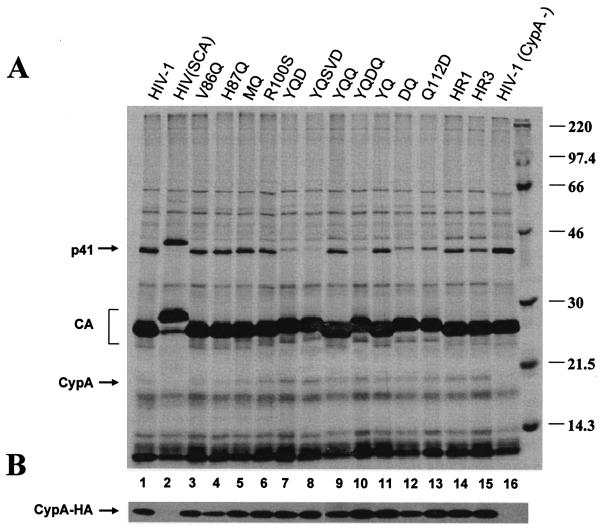
Gag precursor processing and CypA incorporation of HIV-1 CA mutants.
The rate of processing of the HIV-1 Pr55 Gag precursor reflects the efficiency of protein folding and assembly into virions. Processing of the Gag precursor has been suggested to be important for the interaction of HIV-1 CA with restriction factors in monkey target cells (15). As this interaction, at least in owl monkey cells, has been reported to be influenced by CypA-CA binding (46), we also assessed the incorporation of CypA by the CA mutants. 293T cells were transfected with plasmids expressing the wt or mutant Gag/Pol proteins, a human CypA protein with an HA epitope tag, and the HIV-1 Rev protein. The cells were metabolically labeled, and virions in the supernatants were pelleted through sucrose cushions, solubilized, and analyzed by SDS-PAGE. The efficiencies of proteolytic processing of the 55-kDa Gag precursor for all of the mutants are listed in Table 1, and the data for representative mutants are shown in Fig. 5. A few of the mutant Gag proteins were processed aberrantly, leading to additional CA bands; most of these mutants exhibited low levels of replicative ability in the human cell types examined (Table 1). All of the mutants that exhibited a decreased sensitivity to postentry restrictions in monkey cells demonstrated efficient processing of the Gag polyprotein (Fig. 5A and data not shown). Some of these mutants demonstrated processing of the MA-CA p41 proteolytic intermediate that was more efficient than that of the wt Gag protein. However, these differences in p41 processing did not correlate with the infectivity phenotypes.
FIG. 5.
Wild-type and mutant virion proteins. 293T cells were transfected with plasmids encoding the wt and mutant HIV-1 Gag/Pol proteins. Except for the control in lane 16, cells were cotransfected with a vector encoding CypA-HA. Metabolically labeled supernatants were pelleted through a 20% sucrose cushion and resuspended in radioimmunoprecipitation assay buffer. (A) [35S]Methionine-labeled viral proteins were separated by SDS-12.5% PAGE and visualized by autoradiography. The locations of the p41 (MA plus CA) and CA proteins as well as CypA are shown on the left. Values on the right represent the molecular masses in kilodaltons of the marker proteins (far right lane). (B) Solubilized virion pellets were separated by SDS-4 to 12% PAGE, transferred to nitrocellulose membranes, and blotted with a high-affinity rat anti-HA antibody (3F10). The viral samples in panels A and B were identical.
The CypA incorporated into the virions was directly visualized (Fig. 5A) or was detected by Western blotting, using antibodies against the HA epitope tag (Fig. 5B). CypA was not detected in wt HIV-1 particles produced from 293T cells that had not been transfected with the CypA expression plasmid (Fig. 5A, lane 16). This indicates that very little endogenous CypA is incorporated into HIV-1 virions under these experimental conditions. The expression of HA-tagged CypA in the virus-producing cells led to the detection of CypA in the virion particles of wt HIV-1 and all mutant derivatives, with the exception of the HIV(SCA) mutant, as expected. Infections of human and monkey cells with these viruses demonstrated no observed differences in infectivity when compared with viruses that had not been made in the presence of overexpressed CypA (data not shown). We conclude that, with the exception of G89A, all of the mutants that exhibited a decreased sensitivity to postentry restrictions in monkey cells retained the ability to bind CypA.
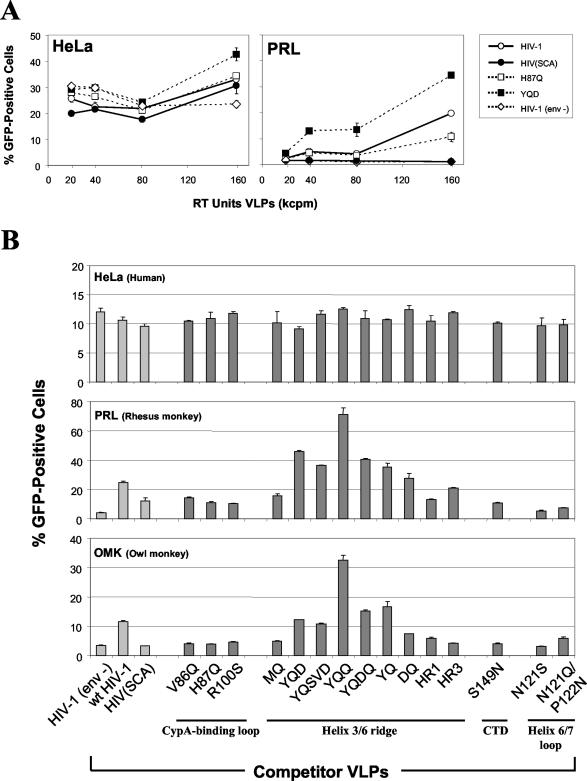
Ability of HIV-1 capsid mutants to compete for a restriction factor(s) in monkey cells.
The factors mediating the postentry restriction to HIV-1 infection in monkey cells can be saturated by noninfectious capsids (15, 28, 37). To examine whether the HIV-1 capsid mutants bind and compete for the simian restriction factor(s), we infected HeLa and PRL cells with a fixed concentration of wt HIV-1 encoding GFP (HIV-GFP) along with increasing concentrations of either wt or mutant VLPs. Additional negative controls were HIV(SCA) VLPs and wt HIV-1 VLPs lacking VSV-G [HIV-1(env−)]. None of the VLPs significantly affected the infectivity of the wt HIV-GFP virus in HeLa cells (Fig. 6A). The low level of infectivity of the HIV-GFP virus in PRL cells was increased in the presence of HIV-1 VLPs, as expected, but not in the presence of HIV-1(env−) VLPs. The HIV(SCA) VLPs also did not affect the infectivity of the HIV-GFP virus in PRL cells. H87Q VLPs did not enhance the infectivity of the HIV-GFP virus as efficiently as the wt HIV-1 VLPs. This result is consistent with a decrease in the affinity of the H87Q mutant for the restriction factor(s) in PRL cells. Such a decrease in affinity could explain the decreased susceptibility of the H87Q mutant viruses to postentry restrictions in PRL cells. Surprisingly, the YQD VLPs enhanced the infectivity of the HIV-GFP virus more efficiently than the wt HIV-1 VLPs. Thus, the YQD VLPs bind the restriction factor(s) present in PRL cells at least as effectively as the wt HIV-1 VLPs.
FIG. 6.
Competition for target cell restriction factors with wt and mutant HIV-1 VLPs. (A) The indicated amounts, in RT units, of VLPs were added to HeLa and PRL cells. Immediately thereafter, recombinant wt HIV-GFP virus was added to HeLa cells at 1 × 104 RT units/well or to PRL cells at 4 × 104 RT units/well. Samples were incubated for 3 days and analyzed by FACS. Labels indicate the identity of each VLP used. All VLPs were pseudotyped with VSV-G, except for the control, a wt HIV-1 VLP with no envelope glycoproteins [HIV-1(env−)]. (B) Approximately 1.5 × 105 RT units of the indicated VLPs/well were added to HeLa, PRL, and OMK cells. Immediately thereafter, the HIV-GFP virus was added to HeLa cells at 1 × 104 RT units/well or to PRL and OMK cells at 4 × 104 RT units/well. The percentages of cells that were positive for GFP expression were determined by FACS. The identities of the VLPs used for competition are indicated at the bottom of the figure.
To extend these findings, we investigated the ability of a larger panel of mutant VLPs to alter the infectivity of the wt HIV-GFP virus in HeLa, PRL, and OMK cells (Fig. 6B). The infectivity of the HIV-GFP virus in HeLa cells was not significantly affected by any of the VLPs. The effects of the different mutant VLPs on HIV-GFP infectivity were similar in PRL and OMK cells, again supporting a model in which the restricting factors in these respective Old World and New World monkey cells are related. In both monkey cell types, HIV-1(env−) did not enhance the infectivity of the HIV-GFP virus, whereas the wt HIV-1 VLPs did. The HIV(SCA) VLPs did not affect the infectivity of the HIV-GFP virus in OMK cells but caused an approximately threefold increase in the infectivity of the HIV-GFP virus in PRL cells. Although this effect was small, it may indicate that the SIV CA protein does not completely escape restriction factor binding. The mutant VLPs with alterations in the CypA-binding loop and the S149N VLPs were less efficient than wt HIV-1 VLPs in enhancing the infectivity of the HIV-GFP virus. In contrast, several of the mutant VLPs with changes in the helix 3/6 ridge caused increases in the infectivity of the HIV-GFP virus that were comparable to or larger than those observed for the wt HIV-1 VLPs. The YQQ mutant VLPs were especially effective in this regard. These results suggest fundamentally distinct modes of escape from the postentry restrictions in simian cells for the HIV-1 capsids altered in the CypA-binding loop and interdomain linker, which apparently exhibit diminished restriction factor binding, and for those altered in the helix 3/6 ridge, which retain the ability to interact with restriction factors.
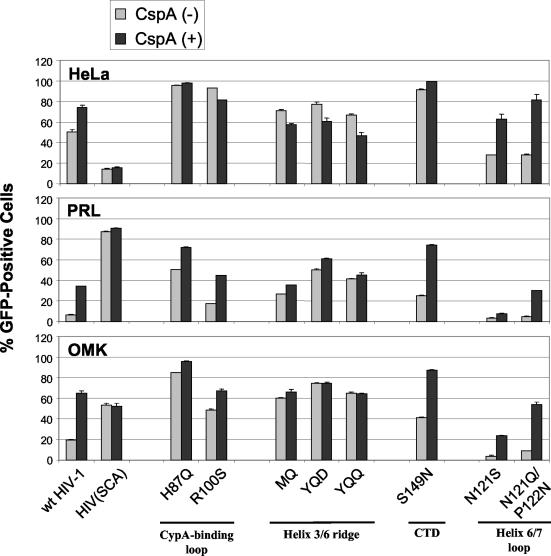
Effects of HIV-1 CA-CypA interactions on postentry restrictions in monkey cells.
It has been reported that CspA treatment of target owl monkey cells decreases the postentry restriction to HIV-1 (46). To investigate whether the interaction between HIV-1 CA and CypA could modulate the sensitivities of our mutants to monkey restriction factors, we infected HeLa, PRL, and OMK cells with wt and mutant GFP-expressing viruses in the absence and presence of 1 μg of CspA/ml (Fig. 7). We observed a three- to sixfold improvement in the infectivity of the wt HIV-GFP virus in both PRL and OMK cells in the presence of CspA, along with a small but consistent increase in infectivity in HeLa cells. Similar improvements in infectivity were observed for the S149N and helix 6/7 loop mutants. CspA treatment of HeLa cells during infection with CypA-binding loop and helix 3/6 ridge mutants either did not affect infectivity or resulted in a small reduction in infection efficiency. Additionally, the infectivities of these mutants either were unaffected by CspA treatment of PRL and OMK target cells or were enhanced modestly. The degree of this enhancement was inversely related to the basal level of infectivity of the mutant virus in the absence of CspA treatment. CspA treatment of the target cells did not influence the infectivity of the HIV(SCA) control virus in all three cell lines, as expected, because the virus is unrestricted in monkey cells and the SIVmac CA protein does not bind CypA (7, 43). These results confirm that CypA-CA interactions can influence the degree of HIV-1 restriction in monkey cells and demonstrate that the enhancing effect of CspA on HIV-1 infectivity in these cells is dependent upon the ability of restriction factors to bind and negatively modulate HIV-1 CA.
FIG. 7.
Effect of CspA treatment of target cells on infectivities of wt and mutant viruses. Target cells were treated with CspA (1 μg/ml) or the equivalent amount of dimethyl sulfoxide solvent 30 min prior to the addition of virus. Cell supernatants containing wt HIV-GFP (wt HIV-1) or the indicated mutant HIV-GFP viruses were normalized for RT activity and added to HeLa cells at 3 × 104 RT units/well or to PRL and OMK cells at 1 × 105 RT units/well. Cells were incubated for 3 days prior to FACS analysis for GFP expression. The means and standard deviations from duplicate experiments are shown.
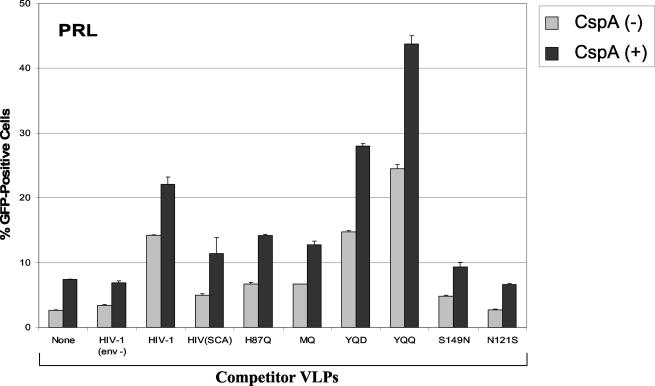
Effect of CspA treatment in combination with VLP competition on HIV-1 infectivity.
To examine the contribution of CypA-CA interaction to the HIV-1-suppressive activity in monkey cells, we infected PRL cells with wt HIV-GFP virus in the absence or presence of 1 μg of CspA/ml and competitor VLPs (Fig. 8). The infectivity of the HIV-GFP virus was increased by the treatment of PRL cells with CspA, as described above. The presence of competitor VLPs lacking envelope glycoproteins had no effect on the infectivity of the HIV-GFP virus. The wt HIV-1 VLPs and the YQD and YQQ mutant VLPs enhanced the basal infectivity of the HIV-GFP virus in the absence of CspA; CspA treatment resulted in a further infectivity increase, in proportion to the degree of enhancement observed for the particular mutant VLPs in the absence of CspA. The same relationship applied to mutant VLPs (H87Q, MQ, S149N, and N121S) that competed less effectively than wt HIV-1 VLPs for the restriction factors in PRL cells. These observations suggest that CypA and the monkey restriction factor(s) are distinct ligands that can bind simultaneously to the HIV-1 capsid. Furthermore, a CypA interaction with CA can positively influence the binding of the restriction factor(s) to HIV-1 capsids.
FIG. 8.
Combined effects of competitor VLPs and CspA treatment on wt HIV-1 infectivity in PRL cells. Cell supernatants containing the indicated wt and mutant HIV-1 VLPs were added to PRL cells at 2 × 105 RT units/well following treatment of the cells for 30 min with either CspA at 1 μg/ml or control dimethyl sulfoxide solvent. Control cells were not incubated with VLPs (none) or were incubated with VLPs lacking envelope glycoproteins [HIV-1(env−)]. The HIV-GFP virus was immediately added to the cells at 4 × 104 RT units/well. Cells were incubated for 3 days before being harvested for FACS analysis. The values represent the means and standard deviations derived from two independent experiments.
DISCUSSION
An understanding of the nature of postentry restrictions to HIV-1 infection in monkeys is important for several reasons. First, information on the viral and cellular factors that modulate these processes will shed light on the poorly understood series of events that govern the fate of retroviral capsids after entry. Second, species-specific barriers to HIV-1 infection present obstacles to the development of animal models for the study of HIV-1 pathogenesis, treatment, and prophylaxis. Finally, an understanding of this critical part of the HIV-1 life cycle may suggest approaches to intervene in its transmission or spread within the host.
Previous studies suggested that the HIV-1 and SIVmac CA proteins are the major determinants of susceptibility to early postentry restrictions in most Old World and New World monkeys, respectively (15, 28, 39). In this study, a large portion of the HIV-1 CA surface that differs from that of SIVmac was altered to structures found in the latter virus. HIV-1 CA mutants that exhibited lower sensitivities to restriction in several different primary and immortalized monkey cells were identified. The patterns of infectivity of mutant viruses and the abilities of mutant VLPs to relieve the blocks to infection were similar for different monkey cells. Notably, the results with the cells of owl monkeys, an unusual New World species that exhibits restrictions to HIV-1 but not to SIVmac (31), resembled those with Old World monkey cells. These observations imply that the factors mediating the restriction in different monkey species are related. Thus, the genes encoding the restriction factors were probably present in the primate genome prior to the divergence of Old World and New World monkeys. In this case, a species-specific polymorphism or variation in expression levels could explain the observed differences among primate species in supporting the early phase of HIV-1 replication.
The HIV-1 CA mutants that escaped the early postentry restrictions in monkey cells segregated into two groups based on their behavior in auxiliary assays (Table 2). One group of CA changes (hereafter referred to as group 1) involved the base of the CypA-binding loop and the interdomain region. VLPs containing these changes competed for the monkey cell restriction factor(s) less effectively than wt HIV-1 VLPs, suggesting a decreased affinity for the factor(s). A similar phenotype was previously seen for an HIV-1 CA mutant containing an alteration in the CypA-binding loop (32). Although the CypA-binding loop and interdomain linker are not proximal on the HIV-1 capsid structure (Fig. 1B), they both are located on the capsid surface distal from the hexameric symmetry axis. This surface forms the walls of a canyon on the HIV-1 capsid (34); the canyon has both dimeric and trimeric symmetry axes and represents an attractive potential binding site for a restriction factor. The CypA-binding loops of adjacent capsids are situated along the canyon rim, explaining the ability of CypA binding to promote restriction factor association with the capsid. Our studies indicate that, although CypA and the factor(s) mediating monkey cell restriction are distinct entities, at least unidirectional cooperativity in capsid binding is likely. Note that the CspA treatment of HeLa target cells was also associated with small increases in the infectivities of wt and some mutant strains of HIV-1, raising the possibility that moieties related to the monkey cell restriction factor(s) are present in some human cells. In this case, alterations in the factor or in expression levels could account for the differences in HIV-1 infectivities among species. Restriction factor expression levels also potentially differ among cell types within a species. We observed that the pattern of infectivity of mutant viruses differed between PRL fibroblasts and primary macrophages of rhesus monkeys. The degree of escape from restriction appeared to be lower for the H87Q and S149N mutants in primary macrophages than in PRL or other monkey cells. A high level of expression of the restriction factor(s) in primary macrophages could explain this observation, as this could compensate for the lower affinity of the group 1 HIV-1 capsid mutants.
TABLE 2.
Summary of mutant phenotypes
| Group no. | Location(s) of CA changes | Relative infectivity in monkey cells compared to wt | Relative ability to compete for restricting factors in monkey cells compared to wt | Effect of CspA on infectivity in HeLa cells |
|---|---|---|---|---|
| 1 | CypA-binding loop and Ser149 (phosphorylation site) | Increase | Decrease | Increase or no change |
| 2 | Helix 3/6 ridge | Increase | Increase | Decrease |
A second group of HIV-1 CA mutants efficiently infected various monkey cells but were still able, as VLPs, to compete for the restriction factor(s) (Table 2, group 2). Apparently, these mutants retain the ability to bind the restriction factor(s) but are not detrimentally affected by such binding. This implies that factor binding initiates subsequent processes that are required for the early block to HIV-1 infection. Examples of such processes are a modification of the HIV-1 capsid and/or the binding of additional factors. With respect to the latter possibility, the location of the amino acid changes in the group 2 mutants on a surface ridge formed by helices 3 and 6 is consistent with the location of a binding site. However, because the group 1 mutants did not efficiently compete for restriction factors, either the binding of a factor to the helix 3/6 ridge must be dependent on prior binding of a restricting factor to the capsid or the factor that binds the helix 3/6 ridge is not able to be competed away from the infectious capsids. Further work aimed at the identification of the restricting factor(s) will be required to distinguish these possibilities.
As VLPs, some of the mutants (YQQ, YQD, YQSVD, and YQDQ) with changes in the helix 3/6 ridge competed for the monkey restricting factor(s) better than wt HIV-1 VLPs. This could reflect a higher affinity of these mutants for the restricting factor(s), although the distance of the helix 3/6 ridge from the putative restriction factor-binding site and the diverse set of changes in the helix 3/6 ridge that engender this phenotype render this explanation less satisfying. It is also possible that these mutants exhibit more capsid stability and are therefore more available to compete for the restriction factor(s). The high degree of replication competence of these mutants suggests that such changes in capsid stability, if present, must be subtle, as large positive or negative changes in this parameter have been reported to be detrimental to viral infectivity (18).
The group 2 mutants exhibited a small but consistent decrease in infectivity in HeLa cells upon CspA treatment. It is not clear whether this effect is secondary to altered binding of the mutant capsids to restriction factors present in human cells.
Our studies suggest three properties of the SIVmac capsid that distinguish it from the HIV-1 capsid and that contribute to its ability to bypass early restriction in monkey cells. First, the SIVmac capsid exhibits a low affinity for the restriction factors in monkey cells. This is due, at least in part, to the identities of residues lining the canyon on the capsid surface, which serves as a putative binding site for the restriction factor(s). Second, the SIVmac capsid does not interact with CypA, which can promote the binding of restriction factors to the HIV-1 capsid (46). As the structure of the SIVmac CA protein has not yet been solved, it is impossible to predict whether the native configuration of the SIVmac CA loop analogous to the CypA-binding loop of HIV-1 CA inhibits the binding of restriction factors. Third, we expect that the structure of the helix 3/6 ridge on the SIVmac capsid renders it resistant to the effects of restriction factor binding. These insights should contribute to the design of HIV-1-like capsids that optimally escape postentry early blocks in monkey cells. Such changes, in combination with alterations designed to allow HIV-1 to overcome the inhibitory effects of simian APOBEC3G in virus-producing cells (36), may allow the development of new primate models of HIV-1 infection.
Acknowledgments
We thank Kimberley Lowe, Maris Handley, and Joyce LaVecchio at the Dana-Farber Cancer Institute flow cytometry core facility for providing excellent technical support; Christine Bogle, Mary Tamucci, and Katherine Hohmann at the Dana-Farber Cancer Institute sequencing core for their expert assistance; and Antoniya M. Ganeva at Mount Holyoke College for data analysis support and FACS sample preparations. We thank Stéphane Basmaciogullari for expert technical assistance with Western blot analysis. We thank Yvette McLaughlin and Sheri Farnum for manuscript preparation.
This work was supported by a grant from the National Institutes of Health (HL54785) and by a Center for AIDS Research award (P30 AI28691).
REFERENCES
- 1.Berthet-Colominas, C., S. Monaco, A. Novelli, G. Sibai, F. Mallet, and S. Cusack. 1999. Head-to-tail dimers and interdomain flexibility revealed by the crystal structure of HIV-1 capsid protein (p24) complexed with a monoclonal antibody Fab. EMBO J. 18:1124-1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Besnier, C., Y. Takeuchi, and G. Towers. 2002. Restriction of lentivirus in monkeys. Proc. Natl. Acad. Sci. USA 99:11920-11925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bieniasz, P. D. 2003. Restriction factors: a defense against retroviral infection. Trends Microbiol. 11:286-291. [DOI] [PubMed] [Google Scholar]
- 4.Bosco, D. A., E. Z. Eisenmesser, S. Pochapsky, W. I. Sundquist, and D. Kern. 2002. Catalysis of cis/trans isomerization in native HIV-1 capsid by human cyclophilin A. Proc. Natl. Acad. Sci. USA 99:5247-5252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braaten, D., C. Aberham, E. K. Franke, L. Yin, W. Phares, and J. Luban. 1996. Cyclosporine A-resistant human immunodeficiency virus type 1 mutants demonstrate that Gag encodes the functional target of cyclophilin A. J. Virol. 70:5170-5176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braaten, D., E. K. Franke, and J. Luban. 1996. Cyclophilin A is required for an early step in the life cycle of human immunodeficiency virus type 1 before the initiation of reverse transcription. J. Virol. 70:3551-3560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braaten, D., E. K. Franke, and J. Luban. 1996. Cyclophilin A is required for the replication of group M human immunodeficiency virus type 1 (HIV-1) and simian immunodeficiency virus SIV(CPZ)GAB but not group O HIV-1 or other primate immunodeficiency viruses. J. Virol. 70:4220-4227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braaten, D., and J. Luban. 2001. Cyclophilin A regulates HIV-1 infectivity, as demonstrated by gene targeting in human T cells. EMBO J. 20:1300-1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bram, R. J., D. T. Hung, P. K. Martin, S. L. Schreiber, and G. R. Crabtree. 1993. Identification of the immunophilins capable of mediating inhibition of signal transduction by cyclosporin A and FK506: roles of calcineurin binding and cellular location. Mol. Cell. Biol. 13:4760-4769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bukovsky, A. A., A. Weimann, M. A. Accola, and H. G. Gottlinger. 1997. Transfer of the HIV-1 cyclophilin-binding site to simian immunodeficiency virus from Macaca mulatta can confer both cyclosporin sensitivity and cyclosporin dependence. Proc. Natl. Acad. Sci. USA 94:10943-10948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cartier, C., M. Deckert, C. Grangeasse, R. Trauger, F. Jensen, A. Bernard, A. Cozzone, C. Desgranges, and V. Boyer. 1997. Association of ERK2 mitogen-activated protein kinase with human immunodeficiency virus particles. J. Virol. 71:4832-4837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cartier, C., P. Sivard, C. Tranchat, D. Decimo, C. Desgranges, and V. Boyer. 1999. Identification of three major phosphorylation sites within HIV-1 capsid. Role of phosphorylation during the early steps of infection. J. Biol. Chem. 274:19434-19440. [DOI] [PubMed] [Google Scholar]
- 13.Chen, C., and H. Okayama. 1987. High-efficiency transformation of mammalian cells by plasmid DNA. Mol. Cell. Biol. 7:2745-2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen, Z., P. Zhou, D. D. Ho, N. R. Landau, and P. A. Marx. 1997. Genetically divergent strains of simian immunodeficiency virus use CCR5 as a coreceptor for entry. J. Virol. 71:2705-2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cowan, S., T. Hatziioannou, T. Cunningham, M. A. Muesing, H. G. Gottlinger, and P. D. Bieniasz. 2002. Cellular inhibitors with Fv1-like activity restrict human and simian immunodeficiency virus tropism. Proc. Natl. Acad. Sci. USA 99:11914-11919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daniel, M. D., N. L. Letvin, N. W. King, M. Kannagi, P. K. Sehgal, R. D. Hunt, P. J. Kanki, M. Essex, and R. C. Desrosiers. 1985. Isolation of T-cell tropic HTLV-III-like retrovirus from macaques. Science 228:1201-1204. [DOI] [PubMed] [Google Scholar]
- 17.Fassati, A., and S. P. Goff. 2001. Characterization of intracellular reverse transcription complexes of human immunodeficiency virus type 1. J. Virol. 75:3626-3635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forshey, B. M., U. von Schwedler, W. I. Sundquist, and C. Aiken. 2002. Formation of a human immunodeficiency virus type 1 core of optimal stability is crucial for viral replication. J. Virol. 76:5667-5677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Franke, E. K., H. E. Yuan, and J. Luban. 1994. Specific incorporation of cyclophilin A into HIV-1 virions. Nature 372:359-362. [DOI] [PubMed] [Google Scholar]
- 20.Freed, E. O. 1998. HIV-1 Gag proteins: diverse functions in the virus life cycle. Virology 251:1-15. [DOI] [PubMed] [Google Scholar]
- 21.Gamble, T. R., F. F. Vajdos, S. Yoo, D. K. Worthylake, M. Houseweart, W. I. Sundquist, and C. P. Hill. 1996. Crystal structure of human cyclophilin A bound to the amino-terminal domain of HIV-1 capsid. Cell 87:1285-1294. [DOI] [PubMed] [Google Scholar]
- 22.Gamble, T. R., S. Yoo, F. F. Vajdos, U. K. von Schwedler, D. K. Worthylake, H. Wang, J. P. McCutcheon, W. I. Sundquist, and C. P. Hill. 1997. Structure of the carboxyl-terminal dimerization domain of the HIV-1 capsid protein. Science 278:849-853. [DOI] [PubMed] [Google Scholar]
- 23.Ganser, B. K., S. Li, V. Y. Klishko, J. T. Finch, and W. I. Sundquist. 1999. Assembly and analysis of conical models for the HIV-1 core. Science 283:80-83. [DOI] [PubMed] [Google Scholar]
- 24.Garrus, J. E., U. K. von Schwedler, O. W. Pornillos, S. G. Morham, K. H. Zavitz, H. E. Wang, D. A. Wettstein, K. M. Stray, M. Cote, R. L. Rich, D. G. Myszka, and W. I. Sundquist. 2001. Tsg101 and the vacuolar protein sorting pathway are essential for HIV-1 budding. Cell 107:55-65. [DOI] [PubMed] [Google Scholar]
- 25.Gitti, R. K., B. M. Lee, J. Walker, M. F. Summers, S. Yoo, and W. I. Sundquist. 1996. Structure of the amino-terminal core domain of the HIV-1 capsid protein. Science 273:231-235. [DOI] [PubMed] [Google Scholar]
- 26.Gottlinger, H. G., J. G. Sodroski, and W. A. Haseltine. 1989. Role of capsid precursor processing and myristoylation in morphogenesis and infectivity of human immunodeficiency virus type 1. Proc. Natl. Acad. Sci. USA 86:5781-5785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greene, W. C., and B. M. Peterlin. 2002. Charting HIV's remarkable voyage through the cell: basic science as a passport to future therapy. Nat. Med. 8:673-680. [DOI] [PubMed] [Google Scholar]
- 28.Hatziioannou, T., S. Cowan, S. P. Goff, P. D. Bieniasz, and G. J. Towers. 2003. Restriction of multiple divergent retroviruses by Lv1 and Ref1. EMBO J. 22:385-394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Himathongkham, S., and P. A. Luciw. 1996. Restriction of HIV-1 (subtype B) replication at the entry step in rhesus macaque cells. Virology 219:485-488. [DOI] [PubMed] [Google Scholar]
- 30.Hirsch, V. M., G. Dapolito, P. R. Johnson, W. R. Elkins, W. T. London, R. J. Montali, S. Goldstein, and C. Brown. 1995. Induction of AIDS by simian immunodeficiency virus from an African green monkey: species-specific variation in pathogenicity correlates with the extent of in vivo replication. J. Virol. 69:955-967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hofmann, W., D. Schubert, J. LaBonte, L. Munson, S. Gibson, J. Scammell, P. Ferrigno, and J. Sodroski. 1999. Species-specific, postentry barriers to primate immunodeficiency virus infection. J. Virol. 73:10020-10028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kootstra, N. A., C. Munk, N. Tonnu, N. R. Landau, and I. M. Verma. 2003. Abrogation of postentry restriction of HIV-1-based lentiviral vector transduction in simian cells. Proc. Natl. Acad. Sci. USA 100:1298-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li, J., C. I. Lord, W. Haseltine, N. L. Letvin, and J. Sodroski. 1992. Infection of cynomolgus monkeys with a chimeric HIV-1/SIVmac virus that expresses the HIV-1 envelope glycoproteins. J. Acquir. Immune Defic. Syndr. 5:639-646. [PubMed] [Google Scholar]
- 34.Li, S., C. P. Hill, W. I. Sundquist, and J. T. Finch. 2000. Image reconstructions of helical assemblies of the HIV-1 CA protein. Nature 407:409-413. [DOI] [PubMed] [Google Scholar]
- 35.Marcon, L., H. Choe, K. A. Martin, M. Farzan, P. D. Ponath, L. Wu, W. Newman, N. Gerard, C. Gerard, and J. Sodroski. 1997. Utilization of C-C chemokine receptor 5 by the envelope glycoproteins of a pathogenic simian immunodeficiency virus, SIVmac239. J. Virol. 71:2522-2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mariani, R., D. Chen, B. Schrofelbauer, F. Navarro, R. Konig, B. Bollman, C. Munk, H. Nymark-McMahon, and N. R. Landau. 2003. Species-specific exclusion of APOBEC3G from HIV-1 virions by Vif. Cell 114:21-31. [DOI] [PubMed] [Google Scholar]
- 37.Munk, C., S. M. Brandt, G. Lucero, and N. R. Landau. 2002. A dominant block to HIV-1 replication at reverse transcription in simian cells. Proc. Natl. Acad. Sci. USA 99:13843-13848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nermut, M. V., and A. Fassati. 2003. Structural analyses of purified human immunodeficiency virus type 1 intracellular reverse transcription complexes. J. Virol. 77:8196-8206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Owens, C. M., P. C. Yang, H. Gottlinger, and J. Sodroski. 2003. Human and simian immunodeficiency virus capsid proteins are major viral determinants of early, postentry replication blocks in simian cells. J. Virol. 77:726-731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parolin, C., B. Taddeo, G. Palu, and J. Sodroski. 1996. Use of cis- and trans-acting viral regulatory sequences to improve expression of human immunodeficiency virus vectors in human lymphocytes. Virology 222:415-422. [DOI] [PubMed] [Google Scholar]
- 41.Strack, B., A. Calistri, M. A. Accola, G. Palu, and H. G. Gottlinger. 2000. A role for ubiquitin ligase recruitment in retrovirus release. Proc. Natl. Acad. Sci. USA 97:13063-13068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Takahashi, H., M. Matsuda, A. Kojima, T. Sata, T. Andoh, T. Kurata, K. Nagashima, and W. W. Hall. 1995. Human immunodeficiency virus type 1 reverse transcriptase: enhancement of activity by interaction with cellular topoisomerase I. Proc. Natl. Acad. Sci. USA 92:5694-5698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thali, M., A. Bukovsky, E. Kondo, B. Rosenwirth, C. T. Walsh, J. Sodroski, and H. G. Gottlinger. 1994. Functional association of cyclophilin A with HIV-1 virions. Nature 372:363-365. [DOI] [PubMed] [Google Scholar]
- 44.Towers, G., M. Bock, S. Martin, Y. Takeuchi, J. P. Stoye, and O. Danos. 2000. A conserved mechanism of retrovirus restriction in mammals. Proc. Natl. Acad. Sci. USA 97:12295-12299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Towers, G., M. Collins, and Y. Takeuchi. 2002. Abrogation of Ref1 retrovirus restriction in human cells. J. Virol. 76:2548-2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Towers, G. J., T. Hatziioannou, S. Cowan, S. P. Goff, J. Luban, and P. D. Bieniasz. 2003. Cyclophilin A modulates the sensitivity of HIV-1 to host restriction factors. Nat. Med. 9:1138-1143. [DOI] [PubMed] [Google Scholar]
- 47.VerPlank, L., F. Bouamr, T. J. LaGrassa, B. Agresta, A. Kikonyogo, J. Leis, and C. A. Carter. 2001. Tsg101, a homologue of ubiquitin-conjugating (E2) enzymes, binds the L domain in HIV type 1 Pr55(Gag). Proc. Natl. Acad. Sci. USA 98:7724-7729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wiegers, K., G. Rutter, H. Kottler, U. Tessmer, H. Hohenberg, and H. G. Krausslich. 1998. Sequential steps in human immunodeficiency virus particle maturation revealed by alterations of individual Gag polyprotein cleavage sites. J. Virol. 72:2846-2854. [DOI] [PMC free article] [PubMed] [Google Scholar]