Abstract
African Americans have a higher prevalence of hypertension and poorer cardiovascular and renal outcomes than white Americans. The objective of this study was to determine whether a telephonic nurse disease management (DM) program designed for African Americans is more effective than a home monitoring program alone to increase blood pressure (BP) control among African Americans enrolled in a national health plan.
A prospective randomized controlled study (March 2006—December 2007) was conducted, with 12 months of follow-up on each subject. A total of 5932 health plan members were randomly selected from the population of self-identified African Americans, age 23 and older, in health maintenance organization plans, with hypertension; 954 accepted, 638 completed initial assessment, and 485 completed follow-up assessment.
The intervention consisted of telephonic nurse DM (intervention group) including educational materials, lifestyle and diet counseling, and home BP monitor vs. home BP monitor alone (control group). Measurements included proportion with BP < 120/80, mean systolic BP, mean diastolic BP, and frequency of BP self-monitoring.
Results revealed that systolic BP was lower in the intervention group (adjusted means 123.6 vs. 126.7 mm Hg, P = 0.03); there was no difference for diastolic BP. The intervention group was 50% more likely to have BP in control (odds ratio [OR] = 1.50, 95% confidence interval [CI] 0.997–2.27, P = 0.052) and 46% more likely to monitor BP at least weekly (OR 1.46, 95% CI 1.07–2.00, P = 0.02) than the control group.
A nurse DM program tailored for African Americans was effective at decreasing systolic BP and increasing the frequency of self-monitoring of BP to a greater extent than home monitoring alone. Recruitment and program completion rates could be improved for maximal impact. (Population Health Management 2010;13:65–72)
Introduction
Hypertension has increased in prevalence for individuals of all races and ethnicities,1–5 but African Americans still have a higher prevalence of hypertension and poorer cardiovascular and renal outcomes than white Americans.6–12 The 1999–2002 National Health and Nutrition Examination Survey reported that 41.1% of black adults had hypertension compared to 28.1% of white adults, and that disparities in clinical outcomes persist.13 In spite of the substantial evidence of the efficacy of pharmacologic and nonpharmacologic interventions to control hypertension in African Americans, fewer than 50% of African American patients under usual primary care conditions attain adequate control.14
Strategies to help patients control their blood pressure (BP) have yielded mixed results.15–20 For example, the meta-analysis by Cappuccio et al of home monitoring programs found that these programs resulted in lower systolic and diastolic pressures when subsequently measured in office settings.16 On the other hand, the meta-analysis by Chodosh et al of 17 hypertension self management programs for older adults showed reductions in systolic and diastolic pressures but concluded that unaccounted heterogeneity and publication bias limit the generalizability of the conclusion.17 Computerized decision support has also been a subject of analysis, but the findings have been mixed.20
Few studies have focused on evaluating the success of comprehensive disease management (DM) techniques on BP control among African Americans. Disease management programs have been effective at helping individuals to adopt and maintain prescribed treatment regimens for conditions including heart failure and diabetes.21,22 Some studies have demonstrated that the effectiveness of DM programs can be greatly enhanced when patient education messages are mindful of health literacy and are presented in culturally sensitive ways.23–26
The purpose of the present study was to examine the effectiveness of a multimodal, population-based DM program at helping African American adults with hypertension achieve and maintain optimal BP (ie, <120/80) as defined by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7).23 The DM program incorporated nurse disease case managers who had received cultural competency training, home monitoring of BP, and educational materials specifically designed for this patient population.
Methods
Design
A prospective randomized controlled intervention trial was used to test the effectiveness of 2 levels of a hypertension DM program at helping privately insured African American adults achieve and maintain BP control. A stratified cluster randomization process was used with the individual's primary care physician (PCP) office as the unit of randomization. One level, the intervention group, consisted of a high-intensity, multimodal, culturally competent DM program with nurse support (DMP). The second level, the control group, was a light support educational program (LSP). Participants in both the control and intervention groups received BP monitors and written and nurse-directed phone call instructions to measure their BP at home at regular intervals. The Morehouse School of Medicine Institutional Review Board approved the study protocol.
Study hypotheses
It was hypothesized that a greater proportion of intervention group participants would have BP < 120/80 than control group participants at the end of the 12-month study. It was also hypothesized that intervention group participants would have lower mean systolic and diastolic pressures, would monitor their BP more frequently, and would be more likely to use 2 or more antihypertensive medications than control group participants.
Study population
A total of 6698 potential study subjects were identified through Aetna's eligibility and claims systems. Potential study subjects had medical benefits in a fully-insured health maintenance organization plan; were 19 years of age or older; had self-reported their race as black or African American; were identified to have a hypertension diagnosis through medical claims (International Classification of Diseases, Ninth Revision codes 401–405.99) during the previous 18 months; had a valid address and telephone number; had selected a PCP; and had not been previously recruited for a different Aetna DM program.
Recruitment
The double-blind recruitment process was implemented in 2 phases.
Phase 1—Welcome Call (March 2006 through September 2006)
An invitation to participate in the study was mailed to 5932 members. Within 2 weeks after the invitation was mailed, eligible members received a standardized welcome call from an external research organization that obtained informed consent from the potential participant and gathered baseline information. In all, 3617 members either had an invalid phone number or were unable to be reached. Welcome calls were completed for 2315 potential participants by September 2006, the study recruitment cutoff date. Prior to random assignment to either the intervention or control group, the external research organization sent an automatic arm cuff BP monitor and BP tracking tool to all study subjects.
Phase 2—Initial Assessments (March 2006 through November 2006)
Two weeks after the BP monitor had been mailed to participants, an Aetna DM nurse conducted a detailed telephonic initial assessment. A wrist cuff monitor was sent to participants whose arm circumference was too large for the arm cuff and the initial assessment was rescheduled. Participants reviewed their BP self-monitoring technique with the nurse and, after confirmation that a correct technique was used, reported their BP at the beginning and end of the call. The initial assessment tool was based on 2 behavior modification principles: the Health Belief Model28 and the Transtheoretical Model.29 The tool consisted of 23 health information questions including knowledge of hypertension risk factors and consequences, personal BP target as determined by the member's physician, healthy lifestyle behaviors, and antihypertensive medication use. Following the initial assessment, the participant was randomly assigned to a study group based on his or her current PCP office.
Cultural competence training for nurse case managers
Prior to initiation of the study, all DM nurses received special training in cardiac care and successfully completed the Manhattan Cross Cultural Group's Quality Interactions: A Patient-Based Approach to Cross-Cultural Care cultural competency training.30 The cultural competency training consisted of a 2.5-h interactive, case-based online course on communication with culturally diverse populations, which centered on the theme that patients are the best source of information. The nurses were taught to conduct a culturally competent patient history, identify the impact of cultural issues, effectively explain management options, and negotiate a treatment plan.
Interventions
The interventions provided to participants in both the DMP and the LSP groups are outlined in Table 1. All participants in the study received Omron BP monitors (accurate to ± 3 mm Hg or 2% of reading)31,32 and received written and verbal instructions to measure their BP at home at regular intervals. BP was collected from participants at the telephonic initial assessment, via a mailed request at 6 months, and via a final assessment conducted either telephonically or by mail. Participants in both the DMP and the LSP study groups were offered incentives worth $15–$55 to continue participation throughout the study period.
Table 1.
Intervention Matrix
| Study Group | ||
|---|---|---|
| Intervention Component | Intervention (DMP) | Control (LSP) |
| Invitiation Letter | ✓ | ✓ |
| Welcome Call & Informed Consent | ✓ | ✓ |
| BP Monitor | ✓ | ✓ |
| Initial Assessment (BP Monitor training & first BP measurements) | ✓ | ✓ |
| Hypertension Educational Mailing | ✓ | |
| Member Care Calls with DM Nurses | ✓ | |
| Quarterly PCP Reports on Member Progress | ✓ | |
| PCP Culturally Compentency Training Offered | ✓ | |
| Six Month BP Postcard (Mid-point BP measurements) | ✓ | ✓ |
| Final Assessment (Final BP measurements) | ✓ | ✓ |
BP-blood pressure; DM-disease management; DMP-disease management program; LSP-light support educational program; PCP-primary care physician.
In addition, DM nurses initiated monthly calls to participants in the culturally competent disease management arm of the study (ie, the intervention group) with the goals of improving their hypertension knowledge and supporting lifestyle changes such as smoking cessation, regular exercise, and adherence to the DASH (Dietary Approaches to Stop Hypertension) diet. The median number of completed calls per participant was 3, with a range of 1 to 10. Call duration was between 15–20 minutes. This intervention group received a 1-time mailing of educational materials developed specifically for African Americans: the 7 Steps to a Healthy Heart for African Americans,33 the African American Health and Dairy Foods Nutritional Fact Sheet,34 and Healthy Eating Tips.35
Three quarterly reports that contained the patient's most recent self-reported BP and DM goals were sent to each intervention group participant's PCP office. The report also provided the JNC 7 and International Society on Hypertension in Blacks (ISHIB) hypertension management guidelines, which recommend that African Americans be prescribed 2 or more antihypertensive drug classes based on optimal BP control success,36 and information about a free online cultural competency training entitled A Physician's Practical Guide to Culturally Competent Care offered by the Department of Health and Human Services' Office of Minority Health.37
Outcome variables
BP
The main dependent variable was the proportion of subjects in each group with BP < 120/80, the optimal level recommended by JNC 7 and ISHIB hypertension management guidelines.27,36 Two BP measurements were requested from the participant at the start and end of the initial assessment telephone call and the final assessment call. The lowest systolic and diastolic readings reported during a call were used in the analyses consistent with Healthcare Effectiveness Data and Information Set (HEDIS®) guidelines for multiple BP measurements on a single visit.38 Participants received follow-up for the 6-month and final assessments, regardless of whether they were still enrolled with the health plan. The 3 BP metrics evaluated were a binary variable representing whether BP was <120/80, systolic BP at final assessment, and diastolic BP at final assessment. Missing BP values at final assessment were replaced with the values from the initial assessment.
Frequency of BP Monitoring
The frequency of BP monitoring was collected at initial and final assessments using the following question: “About how often do you or your family member or friend take your blood pressure?” The frequency of BP monitoring categories were collapsed into “weekly or more” and “less than weekly” monitoring. For the analyses, missing values at the final assessment were replaced with the initial assessment response.
Number of antihypertension medication classes
The proportion of members taking 2 or more antihypertension medication classes was measured in 2 ways. First, information was collected from the participant during the initial and post-telephonic assessments using the following question: “What are the names of the blood pressure medications you take?” If participants did not respond at the final assessment, the response from the initial assessment was used for the analyses. The second method used pharmacy claims for participants who were with the health plan's pharmacy plan during the study period. The drug class for each medication was determined by the Medi-Span Generic Product Identifier code at the 4th digit. The number of drug classes was summed per member per period. A dichotomous variable was created with the following categories: 1 antihypertensive drug class filled, or 2 or more antihypertensive drug classes filled.
Health care utilization
Health care utilization data were obtained from the health plan's claims system. The mean numbers of PCP visits, cardiac specialist visits, and specialist visits were quantified for each individual, although there were no a priori expectations regarding changes in utilization. PCP designation included the physician-identified specialties of family practice or internal medicine. Specialist designation included cardiology, cardiothoracic surgery, endocrinology, and nephrology.
Statistical analysis
Demographic, clinical, initial assessment self-report, and pre-period claim health care utilization data were compared between study groups with Pearson's χ2 test for categorical variables or 2-sample t test for continuous variables. Multiple regression analyses were used to evaluate the dependent variables using the primary care office as a repeated subject measure to account for the clustering of patients within a physician office. Independent variables that were different between the groups at baseline at P < 0.10 level of significance were used as covariates in the regression models. Multiple logistic regression models yielding odds ratios were conducted on the binary metrics of final assessment BP < 120/80, final assessment BP monitoring frequency, and use of 2 or more antihypertensive medication classes. Ordinary least squares multiple regression models were used to compare the 2 study groups on final assessment systolic and diastolic BPs. Generalized linear models assuming a Poisson response distribution and deviance scaling for overdispersion were fitted to PCP visits, cardiologist visits, and specialist visits to investigate study group differences. P values were considered significant at 0.05. Statistical analysis was conducted using SAS version 9.1 (SAS Institute Inc., Cary, NC).
Results
Of the 5932 eligible members identified for recruitment, 3617 members (61%) were not reached by telephone or the available phone number was invalid. Of the 2315 members who accepted the welcome call, 1135 refused to participate in the study; 954 members (16.1% of 5,932 eligible members) were recruited. Figure 1 depicts the flow of members through the study including additional reasons for exclusion of potential subjects from the study. The post assessments were conducted 12 months after the initial assessments; the mean number of months elapsed was 12.9 (min 7.1, max 19.5).
FIG. 1.
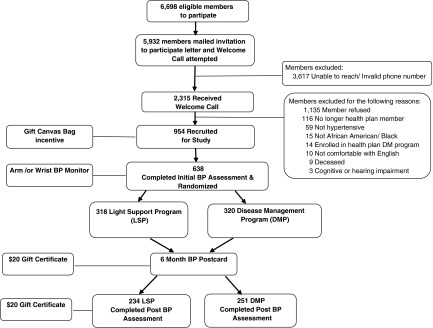
Participant flow.
Of the 954 members recruited, 638 (66.9%) completed the initial assessment. Of the 638 study members who completed the initial BP assessment, 485 (76.0% of initially assessed) either returned the 6-month BP mailing (N = 53) or completed the post BP assessment (N = 432). Of the 638 recruited members who completed the initial BP assessment, 153 (24.0%) did not provide a final BP value; missing values were replaced with the initial assessment BPs for each participant. The percentage of missing values replaced for each group was not significantly different (26% for the control group vs. 22% for the intervention group, χ2 = 2.06, P = 0.15).
Demographics
The recruited population was slightly older (mean age 54.9 vs. 51.2; t value = −8.92, P < 0.001) and more likely to be female (66.4% vs. 60.3%; χ2 = 12.21, P < 0.001) than the invited population. The final study population (those who completed the initial assessment) was 67% female and had a mean age of 55.7 (range 28–91); 94% had graduated high school, and 40% had a household income less than $50,000. Table 2 reveals that the control and intervention groups were broadly comparable at time of initial assessment, with the latter group being slightly better educated, less likely to be taking 2 antihypertensive medication classes, and less likely to have BP < 120/80. Therefore, education, 2 or more antihypertensive medication classes, and initial BP compliance were used as covariates in the multiple regression analyses.
Table 2.
Characteristics of Groups at Initial Assessment
| Characteristics | Control (LSP) (N = 318) | Intervention (DMP) (N = 320) | P value |
|---|---|---|---|
| Demographics | |||
| Mean (SD) | Mean (SD) | ||
| Age an Feb. 2006 | 56.1 (11.5) | 55.3 (11.5) | 0.39 |
| BMI Score | 33.1 (7.4) | 32.7 (6.9) | 0.52 |
| Education completed: high school or above | 292 (92) | 307 (96) | 0.03 |
| N (%) | N (%) | ||
| Female | 221 (70) | 206 (64) | 0.17 |
| Household income | |||
| below $50,000 | 125 (39) | 131 (41) | 0.53 |
| equal to or above $50,000 | 90 (28) | 78 (24) | |
| refused/unknown | 103 (32) | 111 (35) | |
| Diabetes | 79 (25) | 87 (27) | 0.50 |
| Hyperlipidemia | 158 (50) | 153 (48) | 0.64 |
| Kidney disease | 12 (4) | 8 (3) | 0.36 |
| Mean (SD) | Mean (SD) | ||
| Prospective Risk Score at Recruitment* | 2.8 (2.3) | 2.9(2.9) | 0.60 |
| Antihypertensive medication use | N (%) | N (%) | |
| Self-reported: members taking an anti-HYP medication | 304 (96) | 310 (97) | 0.40 |
| Self-reported: taking 2 or more anti-HYP drug classes | 212 (67) | 182 (57) | 0.01 |
| Drug plan benefit | 306 (96) | 309 (97) | 0.82 |
| Pharmacy claims: filled 2 or more anti-HYP drug classes | 215 (70) | 198 (64) | 0.10 |
| BP monitoring frequency | N (%) | N (%) | |
| Weekly or more | 87 (27) | 88 (28) | |
| Less than weekly | 231 (73) | 232 (72) | 0.97 |
| BP < 120/80 | 53 (17) | 38 (12) | 0.08 |
| Mean (SD) | Mean (SD) | ||
| Systolic BP at initial assessment—mean (sd) | 132.9 (20.5) | 133.2 (17.9) | 0.82 |
| Diastolic BP at initial assessment—mean (sd) | 83.6 (12.3) | 84.6 (10.9) | 0.33 |
| Health care utilization in pre-period | |||
| Primary care physician visits PMPY | 3.8 (2.8) | 3.8 (2.4) | 0.87 |
| Cardiac physician visits PMPY | 0.2 (0.7) | 0.2 (0.7) | 0.75 |
| Specialist physician visits PMPY | 0.4 (1.1) | 0.4 (1.0) | 0.88 |
| ER visits PMPY | 0.3 (0.7) | 0.3 (0.7) | 0.71 |
| Cardiac ER visits PMPY | 0.04 (0.3) | 0.04 (0.3) | 0.87 |
| Inpatient admissions PMPY | 0.1 (0.3) | 0.1 (0.4) | 0.92 |
| Cardiac inpatient admissions PMPY | 0.03 (0.2) | 0.03 (0.2) | 0.99 |
| Inpatient days | 0.2 (0.9) | 0.4 (1.5) | 0.17 |
| Cardiac inpatient days | 0.1 (0.4) | 0.1 (0.6) | 0.62 |
Prospective risk score is based on Ingenix Episode Treatment Groups™ (ETG™) software, Release 6.0. Ingenix Inc.
BMI = body mass index; BP = blood pressure; ER = emergency room; anti-HYP = antihypertensive; PMPY = per member per year.
Outcomes
While mean systolic and diastolic BPs were lower for both groups compared to initial assessment, the systolic BP adjusted mean of the intervention group was significantly lower than that of the control group (123.6 vs. 126.7, P = 0.03) post intervention (Table 3). There was no statistically significant difference in diastolic BPs between the groups at the end of the intervention. After adjusting for differences between the groups at time of initial assessment, the intervention group was 46% more likely to report monitoring BP at least weekly than the control group (odds ratio [OR] 1.46, 95% confidence interval [CI] 1.07–2.00, P = 0.02). The intervention group was 50% more likely to have BP in compliance at final assessment than the control group (OR = 1.50, 95% CI 0.997–2.27, P = 0.052), an improvement that approached the level of statistical significance established for the study.
Table 3.
Comparison of Results for DMP and LSP Groups at Final Assessment
| Control (LSP) | Unadjusted Intervention (DMP) | Adjusted* | ||||
|---|---|---|---|---|---|---|
| Blood pressure | N (%) | N(%) | P value | OR (DMP/LSP) | 95% CI | P value |
| BP < 120/80 | 70 (22) | 83 (26) | 0.25 | 1.50 | (0.997 to 2.27) | 0.05 |
| BP monitoring frequency (weekly or more) | 161 (51) | 191 (60) | 0.02 | 1.46 | (1.07 to 2.00) | 0.02 |
| Mean (SD) | Mean (SD) | P value | LSP Mean | DMP Mean | P value | |
| Systolic BP, mmHg | 129.5 (18.2) | 126.8 (16.9) | 0.05 | 126.7 | 123.6 | 0.03 |
| Diastolic BP, mmHg | 80.1 (10.4) | 80.6 (10.5) | 0.59 | 76.9 | 76.9 | 0.99 |
| Antihypertensive medication use | N (%) | N(%) | P value | OR (DMP/LSP) | 95% CI | P value |
| Self reported: taking 2 or more anti-HYP class drugs (yes) | 146 (46) | 139 (43) | 0.53 | 1.08 | (0.76 to 1.53) | 0.65 |
| Pharmacy: filled 2 or more anti-HYP class drugs (yes)† | 214 (71) | 214 (72) | 0.85 | 1.45 | (.93 to 2.25) | 0.10 |
| Health care utilization | Mean (SD) | Mean (SD) | P value | OR (DMP/LSP) | 95% CI | P value |
| Primary care physician visits PMPY | 3.4 (3.5) | 3.3 (2.8) | 0.69 | 0.98 | (0.85 to 1.14) | 0.81 |
| Cardiac physician visits PMPY | 0.3 (0.8) | 0.3 (0.8) | 0.50 | 1.18 | (0.75 to 1.86) | 0.48 |
| Specialist physician visits PMPY | 0.5 (1.2) | 0.5 (1.1) | 0.94 | 1.04 | (0.72 to 1.49) | 0.85 |
Adjusted for educational level, 2 or more anti-HYP medications at initial assessment, and the initial BP compliance as well as the physician office used as repeated measure.
41 members were removed from analysis who did not use or were not eligible for Aetna pharmacy benefit during follow-up period.
anti-HYP = antihypertensive; BP = blood pressure; DMP = disease management program; LSP = light support program; PMPY = per member per year.
There were no statistically significant differences between the groups in the use of 2 or more antihypertensive medication classes, or the mean number of PCP, cardiologist, and specialist physician visits. The reported rate of use of 2 or more antihypertensive classes of medications was quite a bit lower at final assessment than that reported at the time of initial assessment for both groups; however, this decrease in rate was not observed when this variable was examined using pharmacy claims.
The analyses were repeated using 2 other methods for replacing the missing BPs at final assessment. First, the missing values were replaced with the mean final systolic and diastolic BPs for the combined groups. Second, the analyses were conducted on the 485 participants who completed the final assessment. Results were similar using these additional methods, although the intervention group's likelihood of having BP in compliance was slightly greater using these methods (OR 1.84, P = 0.003 and OR 1.72, P = 0.01, respectively).
In addition, the difference between the groups on the odds of reaching optimal BP was analyzed with the dependent variable (optimal BP) defined as 130/80 for 161 individuals with diabetes and/or renal failure, and 120/80 for individuals who did not report these conditions. The groups were similar with respect to the proportions of individuals reporting these diagnoses. The results of the logistic regression analysis were similar to those reported above, with the DMP (intervention) group having greater odds of having BP in compliance than the LSP group (OR 1.50, P = 0.045).
Discussion
This study demonstrated that home BP monitoring, coupled with a DM program that employs nurses who received cultural competence training as well as culturally sensitive materials, can improve BP compliance and reduce systolic BP more than a home BP monitoring device alone. While a 3.1-point decrease in systolic BP may seem small, the ALLHAT study estimated that a 3-point change in systolic BP could explain a 10%–20% difference in the risk of major cardiovascular events.39 The current study was designed to be generalizable, building on standard DM design, but incorporating home monitoring, cultural competency training for DM staff, and culturally competent education materials. While this design does not isolate the impact of cultural competence training or materials, it provides an indication that cultural competence training and culturally sensitive materials may be helpful in improving self-management of hypertension.
Hypertension DM strategies have yielded mixed results.15–20 The present study builds on insights obtained from racially heterogeneous studies that show the effects of self-monitoring, pharmacy programs, and Web-based content, respectively, on BP control.21,22,40–41 One recent investigation that evaluated African Americans with hypertension who resided in Baltimore reported a decrease in both systolic and diastolic BP as a result of home monitoring and community-based programs.42 The Baltimore study involved an intensive intervention with a nurse practitioner/community health worker/physician team and included home visits, an approach that would likely be difficult to generalize to a large population given the resources involved. In light of the lessons from these studies, we specifically undertook cultural competence training for the DM team, an approach that we do not believe was incorporated into other similar hypertension programs. While our study did not isolate cultural competence training, compared to the studies cited, cultural competency training and culturally sensitive materials seem to have been the added factor that improved hypertension self-management.
The study represents a response to the fact that hypertension is more prevalent and less well treated in those who self-identify as African American. The cultural competence aspects of the DM program were the key modifications based on race; they appear to have played a role, even with the modest 180-minute training session. The impact of a culturally competent program may have been even more robust if the cultural competency training was increased. This study suggests that racial self-identification can provide the basis for tailored programs instituted by health plans.
Limitations of this randomized clinical trial include the potential for self-selection bias among participants, as evidenced by a low recruitment rate compared to the number of invited individuals. This underscores a common problem with large-scale DM programs and is not unique to our study.43
With the greater prevalence of both hypertension and uncontrolled hypertension in the African American community, and with effective hypertension treatments available, it is imperative that the health care community identify effective methods to engage African Americans in programs to improve their hypertension control. The success of the current program likely lies in the combination of BP monitoring in the home and a thoughtful, culturally sensitive DM program. The improvement in BP control should be generalizable to African American members with health insurance who will participate or interact with their health plan's DM program.
Acknowledgments
We thank Maryann McGuire, R.N., of Health & Technology Vector Inc., for her support in the early development of the study. We thank the nurses and staff of Aetna for their careful and committed implementation of the disease management program. Lastly, we wish to acknowledge the men and women who participated in this study in hopes of improving hypertension care for all. Sanofi–Aventis provided funding for the disease management educational materials, consulting costs, and the cost of review by the Morehouse Institutional Review Board.
Author Disclosure Statement
Dr. Spettell, Ms. McMahill–Walraven, and Ms. Lowy are employed by Aetna, the health plan that implemented the disease management program. Dr. Brennan was employed at Aetna during the study. Dr. Villagra received compensation from Sanofi–Aventis for consulting services during the course of the study. Dr. Ofili, Ms. Daniels, Dr. Quarshie, and Dr. Mayberry disclosed no potential conflicts of interest. Sanofi-Aventis had no access to the data and played no role in the analysis.
References
- 1.Berlowitz DR. Ash AS. Hickey EC, et al. Inadequate management of blood pressure in a hypertension population. N Engl J Med. 1998;339:1957–1963. doi: 10.1056/NEJM199812313392701. [DOI] [PubMed] [Google Scholar]
- 2.Oliveria SA. Laouerta P. McCarthy BD. L'Italien GJ. Berlowitz DR. Asch SM. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413–420. doi: 10.1001/archinte.162.4.413. [DOI] [PubMed] [Google Scholar]
- 3.Chobanian AV. Bakris GL. Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 4.Hyman DJ. Pavlik VN. Self-reported hypertension treatment practices among primary care physicians: Blood pressure thresholds, drug choices, and the role of guidelines and evidence-based medicine. Arch Intern Med. 2000;160:2281–2286. doi: 10.1001/archinte.160.15.2281. [DOI] [PubMed] [Google Scholar]
- 5.Hajjar I. Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 6.Sundquist J. Winkleby MA. Pudaric S. Cardiovascular disease risk factors among older black, Mexican-American, and white women and men: An analysis of NHANES III, 1988–1994. Third National Health and Nutrition Examination Survey. J Am Geriatr Soc. 2001;49:109–116. doi: 10.1046/j.1532-5415.2001.49030.x. [DOI] [PubMed] [Google Scholar]
- 7.Materson BJ. Lessons on the interaction of race and antihypertensive drugs from the VA cooperative study group on antihypertensive agents. Am J Hypertens. 1995;8:92s–93s. doi: 10.1016/0895-7061(95)00305-3. [DOI] [PubMed] [Google Scholar]
- 8.He J. Kiang MJ. Caballero B. Appel LJ. Charleston J. Whelton PK. Plasma insulin levels and incidence of hypertension in African Americans and whites. Arch Intern Med. 1999;159:498–509. doi: 10.1001/archinte.159.5.498. [DOI] [PubMed] [Google Scholar]
- 9.Hyman DJ. Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345:479–486. doi: 10.1056/NEJMoa010273. [DOI] [PubMed] [Google Scholar]
- 10.Wong MD. Shapiro MF. Boscardin WJ. Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. 2003;347:1585–1592. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 11.Hicks LS. Fairchild DG. Horng MS. Orav EJ. Bates DW. Ayanian JZ. Determinants of JNC VI guideline adherence, intensity of drug therapy, and blood pressure control by rate and ethnicity. Hypertension. 2004;44:429–434. doi: 10.1161/01.HYP.0000141439.34834.84. [DOI] [PubMed] [Google Scholar]
- 12.American Heart Association. Heart Disease and Stroke Statistics–2007 Update. Dallas, TX: American Heart Association; 2007. [Google Scholar]
- 13.Hertz RP. Unger AN. Cornell JA. Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 14.Douglas JG. Ferdinand KC. Bakris GL. Sowers JR. Barriers to blood pressure control in African Americans. Postgrad Med. 2002;112:51–70. doi: 10.3810/pgm.2002.10.1332. [DOI] [PubMed] [Google Scholar]
- 15.Staessen JA. Hond ED. Celis H, et al. Antihypertensive treatment based on blood pressure measurement at home or in the physician's office. JAMA. 2004;291:955–964. doi: 10.1001/jama.291.8.955. [DOI] [PubMed] [Google Scholar]
- 16.Cappuccio FP. Kerry SM. Forbes L. Donald A. Blood pressure control by home monitoring: Meta-analysis of randomized trials. BMJ. 2004;329:145–148. doi: 10.1136/bmj.38121.684410.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chodosh J. Morton SC. Mojica W, et al. Meta-analysis: Chronic disease self-management programs for older adults. Ann Intern Med. 2005;143:427–438. doi: 10.7326/0003-4819-143-6-200509200-00007. [DOI] [PubMed] [Google Scholar]
- 18.Halme L. Vesalainen R. Kaaja M. Kantola I. Self-monitoring of blood pressure promotes achievement of blood pressure target in primary health care. Am J Hypertens. 18:1415–1420. doi: 10.1016/j.amjhyper.2005.05.017. 205. [DOI] [PubMed] [Google Scholar]
- 19.Artinian NT. Washington OGM. Templin TN. Effects of home telemonitoring and community-based monitoring on blood pressure control in urban African Americans: A pilot study. Heart Lung. 2001;30:191–199. doi: 10.1067/mhl.2001.112684. [DOI] [PubMed] [Google Scholar]
- 20.Hicks LS. Sequist TD. Ayanian JZ, et al. Impact of computerized decision support on blood pressure management and control: A randomized controlled trial. J Gen Intern Med. 2007;23:429–441. doi: 10.1007/s11606-007-0403-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riegel B. Carlson B. Kopp Z. LePetri B. Glaser D. Unger A. Effect of a standardized case-management telephone intervention on resource use in patients with chronic heart failure. Arch Intern Med. 2002;162:705–712. doi: 10.1001/archinte.162.6.705. [DOI] [PubMed] [Google Scholar]
- 22.Villagra VG. Ahmed T. Effectiveness of a disease management program for patients with diabetes. Health Aff. 2004;23:255–266. doi: 10.1377/hlthaff.23.4.255. [DOI] [PubMed] [Google Scholar]
- 23.Riegel B. Carlson B. Glaser D. Romero T. Randomized controlled trial of telephone case management in Hispanics of Mexican origin with heart failure. J Card Fail. 2006;12:211–219. doi: 10.1016/j.cardfail.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 24.Ferdinand KC. Serrano CC. Ferdinand DP. Contemporary treatment of heart failure: Is there adequate evidence to support a unique strategy for African-Americans? Con position. Curr Hypertens Rep. 2002;4:311–318. doi: 10.1007/s11906-996-0010-2. [DOI] [PubMed] [Google Scholar]
- 25.Lorig KR. Ritter PL. Gonzalez VM. Hispanic chronic disease self-management: A randomized community-based outcome trial. Nurs Res. 2003;52:361–369. doi: 10.1097/00006199-200311000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Rothman RL. DeWalt DA. Malone R, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;292:1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 27.The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, Treatment of High Blood Pressure. Washington DC: U.S. Department of Health and Human Services; 2004. p. 11. [Google Scholar]
- 28.Finfgeld DL. Wongvatunyu S. Conn VS. Grando VT. Russell CL. Health belief model and reversal theory: A comparative analysis. J Adv Nurs. 2003;43:288–297. doi: 10.1046/j.1365-2648.2003.02712.x. [DOI] [PubMed] [Google Scholar]
- 29.Prochaska JO. Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 30.Carrillo JE. Green AR. Betancourt JR. Quality interactions. A patient-based approach to cross cultural care. http://www.qualityinteractions.org/prod_overview/index.html. [Nov 28;2007 ]. http://www.qualityinteractions.org/prod_overview/index.html
- 31.Automatic Blood Pressure Monitor with ComFit Cuff Model HEM-780. Banniockburn, IL: OMROM Healthcare; 2004. p. 27. [OMRON instruction manual.] [Google Scholar]
- 32.Wrist Blood Pressure Monitor with Advanced Positioning Sensor (APS) Model HED- 637. Banniockburn, IL: OMROM Healthcare; 2004. p. 29. [OMRON instruction manual.] [Google Scholar]
- 33.7 Steps to a Healthy Heart for African Americans. Atlanta, GA: Association of Black Cardiologists; 2005. [Google Scholar]
- 34.Nutrition fact sheet. African-American health and dairy foods. J Am Diet Assoc. 2004;104:3. [Google Scholar]
- 35.Healthy Eating Tips: Nutritional Tips from Aetna. Blue Bell, PA: Aetna; 2006. [Fact Sheet] [Google Scholar]
- 36.Douglas JG. Bakris GL. Epstein M, et al. Management of high blood pressure in African Americans: Consensus statement of the Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks. Arch Intern Med. 2003;163:525–541. doi: 10.1001/archinte.163.5.525. [DOI] [PubMed] [Google Scholar]
- 37.US Department of Health and Human Services, Office of Minority Health. A physician's practical guide to culturally competent care. https://cccm.thinkculturalhealth.org/ [Dec 19;2007 ]. https://cccm.thinkculturalhealth.org/
- 38.HEDIS 2006 Technical Specifications, Vol. 2. Washington DC: National Committee for Quality Assurance; 2005. p. 111. [Google Scholar]
- 39.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major cardiovascular events in hypertensive patients randomized to doxazosin vs chlorthalodone: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2000;283:1967–1975. [PubMed] [Google Scholar]
- 40.Lee JK. Grace KA. Taylor AJ. Effects on a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol. JAMA. 2006;296:2563–2571. doi: 10.1001/jama.296.21.joc60162. [DOI] [PubMed] [Google Scholar]
- 41.Green BB. Cook AJ. Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control. JAMA. 2008;299:2857–2867. doi: 10.1001/jama.299.24.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dennison CR. Post W. Kim MT, et al. Underserved urban African American men: Hypertension trial outcomes and mortality during 5 years. Am J Hypertens. 2007;20:164–171. doi: 10.1016/j.amjhyper.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 43.Perrin KM. Burke SG. O'Connor D, et al. Factors contributing to intervention fidelity in multi-site chronic disease self-management program. Implement Sci. 2006;1:26–31. doi: 10.1186/1748-5908-1-26. [DOI] [PMC free article] [PubMed] [Google Scholar]


