Abstract
Replication-competent recombinant vesicular stomatitis viruses (rVSVs) expressing the type I transmembrane glycoproteins and selected soluble glycoproteins of several viral hemorrhagic fever agents (Marburg virus, Ebola virus, and Lassa virus) were generated and characterized. All recombinant viruses exhibited rhabdovirus morphology and replicated cytolytically in tissue culture. Unlike the rVSVs with an additional transcription unit expressing the soluble glycoproteins, the viruses carrying the foreign transmembrane glycoproteins in replacement of the VSV glycoprotein were slightly attenuated in growth. Biosynthesis and processing of the foreign glycoproteins were authentic, and the cell tropism was defined by the transmembrane glycoprotein. None of the rVSVs displayed pathogenic potential in animals. The rVSV expressing the Zaire Ebola virus transmembrane glycoprotein mediated protection in mice against a lethal Zaire Ebola virus challenge. Our data suggest that the recombinant VSV can be used to study the role of the viral glycoproteins in virus replication, immune response, and pathogenesis.
Viral hemorrhagic fever viruses are perfect examples of emerging and reemerging pathogens. Infections are serious public health concerns not just in developing countries where these viruses are endemic but also in many developed countries. Some of them are listed on the category A list of bioterrorism agents (Centers for Disease Control, 2003, http://www.bt.cdc.gov/Agent/Agentlist.asp) and thus represent a threat to the world's population. Studies on many of these pathogens, such as Lassa virus, Marburg virus, and Ebola virus, have been impeded in the past by the biocontainment needed for their manipulation, biosafety level 4 (BSL4). Although these viruses can be grown in tissue culture, virus propagation is comparatively slow, and titers are generally lower than those of other viral pathogens.
Vesicular stomatitis virus (VSV) is a nonsegmented, negative-stranded RNA virus that belongs to the family Rhabdoviridae, genus Vesiculovirus (27). The simple structure and rapid high-titer growth of VSV in mammalian and many other cell types has made it a favored tool for molecular and cell biologists in the past 30 years, and this was further strengthened with the establishment of the reverse genetic system for VSV (25). The ability of VSV to tolerate additional transcription units and genes has been reported previously (15, 23, 41). These characteristics make this system suitable for studying the role of foreign soluble and transmembrane glycoproteins in the context of infectious viral particles. Additionally, VSV is relatively easy to manipulate, and in general, classic virological approaches are easily applicable.
The VSV system has already been used to generate pseudotype virus for studying the role of the Ebola virus transmembrane glycoprotein in cell entry (17, 18, 47). The use of pseudotype particles is limited to a single-step infection and therefore provides a poor model for real infectious processes. Replication-competent recombinant VSVs (rVSVs) are a far more authentic and powerful tool for investigating infection both in vitro and in vivo. Such recombinant viruses may help to overcome some of the limitations required to work with viruses that require BSL4 containment.
The goal of our study was to produce rVSV particles expressing transmembrane and soluble glycoproteins derived from selected BSL4 agents, particularly filoviruses (Ebola virus and Marburg virus) and arenaviruses (Lassa virus). Ebola virus and Marburg virus are nonsegmented negative-stranded RNA viruses that belong to the family Filoviridae (38). Biosynthesis of the transmembrane glycoprotein involves a series of co- and posttranslational events, including cleavage by furin or a furin-like cellular protease (50, 51). Cleavage leads to two disulfide-linked subunits, GP1 and GP2, of which GP2 anchors the molecule in the membrane. Expression of the transmembrane glycoprotein of Ebola virus requires transcriptional editing. Unedited transcripts yield the nonstructural glycoprotein sGP, which is secreted extensively from infected cells (39, 49). The role of the different soluble glycoproteins produced during filovirus infections is currently not well understood, but they may interfere with host defense mechanisms (8, 9, 52).
Lassa virus is a member of the family Arenaviridae and belongs to the Old World arenaviruses (4). Its bisegmented, single-stranded, negative-sense RNA genome is organized in an ambisense coding strategy. The smaller segment encodes the nucleoprotein and the glycoprotein precursor (GPC) (4). Cleavage takes place in the endoplasmic reticulum and is mediated by the cellular subtilase SKI-1/S1P (26). A characteristic of arenavirus glycoproteins is an unusually long signal peptide with two predicted hydrophobic domains (3, 7). The presence of the authentic signal peptide is a requirement for protein processing and maturation (6). Only the cleaved subunits, GP1 and GP2, form the spikes on the virus particles (26).
Here we describe the generation, characterization, and biological phenotypes of several rVSV particles containing different forms of the glycoproteins from the above-mentioned filoviruses and arenaviruses. A first attempt to use rVSV to induce protection in mice against Ebola virus infection suggested the potential value of the VSV platform as possible vaccine vectors against viral hemorrhagic fevers.
MATERIALS AND METHODS
Virus stocks, cell lines, and animals.
The glycoprotein genes were derived from Zaire Ebola virus, strain Mayinga, Lake Victoria marburgvirus (Marburg virus), strain Musoke, and Lassa virus, strain Josiah. The VSV system (Indiana serotype) was provided by J. Rose, Yale University, and was described in detail earlier (25, 42). VeroE6 and 293T cells were grown in Dulbecco's modified Eagle's medium (DMEM) containing penicillin (100 U/ml), streptomycin (100 μg/ml), l-glutamine (2 mM) (all from Invitrogen, Burlington, Canada), and 10% fetal bovine serum (FBS) (Sigma, Oakville, Canada). Baby hamster kidney cells constitutively expressing the bacteriophage T7 polymerase (2) (BSR-T7; kindly provided by K. Conzelmann, Pettenkoffer Institute, Munich, Germany) were maintained in Glasgow minimal essential medium (MEM) enriched with 5% tryptose phosphate broth, G418 (0.5 mg/ml), and the same amounts of penicillin, streptomycin, glutamine, and FBS as described above. Jurkat cells were cultured in RPMI 1640 (American Type Culture Collection) supplemented with the same amounts of penicillin, streptomycin, glutamine, and FBS as described above for Vero E6 and 293T cells. For the animal experiments, we used 6-week-old female BALB/c mice purchased from Charles River Laboratories, Inc. (Wilmington, Mass.).
Plasmid construction.
A plasmid expressing the positive-strand RNA complement of the VSV genome with a site for foreign gene expression was described previously (42). This plasmid (VSVXN2) contains the five VSV genes (nucleoprotein N, phosphoprotein P, matrixprotein M, glycoprotein G, and polymerase L) in order, flanked by the bacteriophage T7 promoter, the VSV leader, and the hepatitis delta virus ribozyme, and the T7 terminator sequence. Between the G and the L genes, a unique linker site (XhoI-NheI) is present, flanked by a transcriptional start and stop signal for the additional gene to be expressed (Fig. 1). The open reading frames encoding the soluble glycoprotein (sGP) of Zaire Ebola virus and the larger cleavage fragment (GP1) of Marburg virus were cloned into the XhoI and NheI sites of the VSVXN2 vector, which contains the transcriptional start and stop signals for insertion of an additional gene (42). The plasmids obtained were designated pVSVXN2/MARVGP1 and pVSVXN2/ZEBOVsGP, respectively. The open reading frames encoding the transmembrane glycoproteins of Marburg virus and Zaire Ebola virus (GP) as well as Lassa virus (GPC) were cloned into the XhoI and NheI sites of the modified full-length VSVXN2ΔG vector lacking the VSV G (Fig. 1). The resulting plasmids were called pVSVXN2ΔG/MARVGP, pVSVXN2ΔG/ZEBOVGP, and pVSVXN2ΔG/LASVGPC, respectively.
FIG. 1.
Schematic drawing of the infectious clone system for VSV, Indiana serotype. BSR-T7 cells were cotransfected with a plasmid containing the VSV genome (VSVXN2 or VSVXN2ΔG) and plasmids expressing the VSV nucleoprotein (pBS-VSV N), phosphoprotein (pBS-VSV P), or polymerase (pBS-VSV L). Transcription of all plasmids is under the control of the bacteriophage T7 RNA promoter. For this study, the glycoproteins of Zaire Ebola virus (ZEBOV GP), Marburg virus (MARV GP), and Lassa virus (LASV GPC) were inserted between the VSV matrix and polymerase (L) genes by using plasmid VSVXN2ΔG (A). In addition, Zaire Ebola virus sGP and Marburg virus GP1 were inserted as an additional gene into vector VSVXN2 (B).
Transfection and rescue of recombinant VSV.
BSR-T7 cells were grown to approximately 90% confluence in 6-cm dishes. The cells were then transfected in BSL2 with the support plasmids encoding the viral ribonucleoprotein constituents (0.5 μg of pBS-VSV N, 1.25 μg of pBS-VSV P, and 0.25 μg of pBS-VSV L) and 2 μg of the plasmid encoding one of the five recombinant genomic clones described above. Transfections were performed with Lipofectamine 2000 (Invitrogen) according to manufacturer's instructions. Since the work with these recombinant viruses had not at this time been classified (i.e., the required biosafety level), we transferred the transfected cells immediately into BSL4. After 48 h at 37°C, supernatants were blind passaged onto VeroE6 cells (80 to 90% confluent). Recovery of infectious virus was confirmed by scanning VeroE6 monolayers for cytopathic effect. Rescued rVSVs were passaged on VeroE6 cells to obtain a virus stock. The virus stock was plaque titrated on VeroE6 cells.
Immunofluorescence assay.
VeroE6 cells grown on coverslips were infected with the rVSV at a multiplicity of infection (MOI) of 0.1. Following virus adsorption for 1 h at 37°C, the inoculum was replaced with DMEM containing 2% FBS. Cells were fixed 24 h postinfection with 4% paraformaldehyde in phosphate-buffered saline (PBS) overnight. After a change of paraformaldehyde, cells were removed from BSL4 and gamma irradiated (2 × 106 rads). After inactivation, cells were washed with PBS and permeabilized with 0.1% Triton X-100 in PBS for 15 min. Subsequently, the cells were washed three times with PBS and incubated for 1 h at room temperature with the appropriate protein-specific antibody diluted in PBS. The samples were washed three times with PBS and incubated for another hour with an indocarbocyanine-conjugated anti-species-specific antibody (Jackson ImmunoResearch Laboratories, West Grove, Pa.). After being washed three times with PBS, the coverslips were mounted with SuperMount (BioGenex, San Ramon, Calif.) and examined with a Zeiss microscope.
Electron microscopy.
rVSVs were grown in VeroE6 cells, and virions were recovered from culture supernatants by ultracentrifugation and fixed in a solution of 2% paraformaldehyde and 0.5% glutaraldehyde. Fixed viral suspensions were transferred to copper electron microscopy grids coated with carbon. The coated grids were bag sealed and removed from BSL4. For inactivation, the grids were gamma irradiated as described above. Negative staining was performed with 2% phosphotungstic acid (pH 6.8) for 1 min. Excess fluid was removed, and the grids were examined with a transmission electron microscope (Zeiss, Jena, Germany).
Metabolic labeling, immunoprecipitation, and immunoblotting.
VeroE6 cells (6 cm dish) were inoculated with the rVSV at an MOI of 10 PFU/cell. The inoculum was replaced after 1 h by DMEM containing 2% FBS. When Jurkat cells (clone E6-1, a T-cell clone) were infected, a slightly modified version of the protocol described earlier (29) was used. Briefly, cells were infected for 1 h at an MOI of 10 PFU/cell, at room temperature with gentle mixing every 10 to 20 min. RPMI 1640 medium containing 2% FBS was then added, and culturing was continued for 1 h at 37°C. The cells were then washed three times in RPMI 1640, resuspended at 106 cells/ml in medium containing 2% FBS, with 1 ml per well of a 12-well dish. For metabolic labeling experiments, cells were incubated for 24 h, washed with DMEM deficient in methionine and cysteine, pulse labeled for 30 min in the same medium supplemented with 20 μCi of [35S]methionine-cysteine per ml, and subsequently chased for 240 min.
For cleavage inhibition studies, the infected cells were incubated during starvation, pulse, and chase periods with the decanoylated peptidylchloromethylketone (decRVKR-cmk; Bachem Distribution Services GmbH, Weil am Rhein, Germany) at a concentration of 25 μM. Labeled cells were lysed in coimmunoprecipitation buffer (1% Nonidet P-40, 0.4% sodium deoxycholate, 5 mM EDTA, 100 mM NaCl, 20 mM Tris-HCl [pH 7.6], 25 mM iodoacetamide, 1 mM phenylmethylsulfonyl fluoride) at 4°C and inactivated by gamma irradiation (2 × 106 rads). Immunoprecipitation was performed with a protein-specific monoclonal antibody (II9G4; see Acknowledgments). Precipitated proteins were subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE, 10% gel) under reducing conditions and visualized by fluorography. For immunoblot analysis, cells were washed 24 or 36 h postinfection with PBS and lysed in SDS gel loading buffer. Supernatants harvested at 12 h postinfection and clarified from cell debris by centrifugation (8,000 × g, 4°C, 10 min) were mixed with SDS gel loading buffer and gamma irradiated (2 × 106 rads). Proteins were resolved by SDS-PAGE (10%) and transferred to polyvinylidene difluoride membranes (Immobilon P; Millipore, Nepean, Canada). Expression of the foreign protein was detected with appropriate antibodies as described above.
Growth characteristics.
VeroE6 and Jurkat cells were grown to 80% confluence or to a cell density of 106 per well of a 12-well dish, respectively, and infected with the different rVSVs at an MOI of 10 PFU/cell. Cells were then washed three times in DMEM, and finally 1 ml of fresh medium containing 2% FBS was added. Cultures (cells and supernatants) were harvested at the time points indicated and centrifuged at 3,000 × g for 5 min at 4°C. The supernatants were stored at −80°C. Titration was performed by defining the 50% tissue culture infectious dose (TCID50). For this, the supernatants were diluted 10-fold and the dilutions were used to infect VeroE6 cells in 96-well plates (five wells for each dilution). The cultures were scored periodically for cytopathic effect over a period of 7 days. The endpoint virus titers for culture supernatants were calculated with the method of Reed and Muench (32). Viral titers were expressed as the log10 of the 50% titration endpoint for infectivity as calculated by the methods of Karber and Spearman (21, 43).
rVSV infection and Zaire Ebola virus challenge of mice.
Groups of 6-week-old female BALB/c mice (n = 5) were injected intraperitoneally with approximately 2 × 104 PFU of rVSVs or gamma-irradiated rVSV, and a further group was left untreated. Following infection with rVSVs, mice were checked daily for clinical symptoms, and their weight was recorded for the first 11 days postinfection. Mice were reinfected with the same rVSV 14 days after the initial infection. At 28 days after the initial infection, all of the mice were challenged intraperitoneally with 1,000 50% lethal doses of the mouse-adapted strain of Zaire Ebola virus (1). Weight and clinical symptoms were recorded daily for 11 days postchallenge. Surviving animals were observed for three times the period needed to kill the controls. All animal work was performed under the guidelines of the Canadian Council on Animal Care and an appropriate Animal Use Document approved by the local Animal Care Committee.
RESULTS AND DISCUSSION
The ability to genetically manipulate VSV has already led to a variety of new insights into the structure and function of viral genes and the analysis of promoter elements and other noncoding elements of VSV (10, 19, 22, 28, 34, 44). The ability of the VSV genome to tolerate foreign transcription units and genes and to accept the replacement of VSV G with a foreign transmembrane glycoprotein has been extremely helpful for studies on the structure and function of these foreign proteins in the context of virus infection (23, 31). In addition, rVSVs are being investigated as promising live virus vaccine candidates for several viruses, such as influenza virus, human immunodeficiency virus, and bovine viral diarrhea virus (14, 33, 36, 37). The potential to serve as vaccine candidates is related to the high-titer growth of VSV and rVSVs in many cell lines (20, 23, 25), the elucidation of a strong cellular and humoral immune response by VSV in vivo (11, 24, 53), and the normally asymptomatic or mild clinical course of VSV infections in humans (35, 48).
In this study, we attempted to establish a system to express and study the function of soluble glycoproteins and transmembrane glycoproteins of BSL4 agents causing viral hemorrhagic fevers. For this, we modified the full-length cDNA clone (pVSVXN2) by either replacing the VSV G gene with the transmembrane glycoproteins of Marburg virus, Zaire Ebola virus, and Lassa virus or generating a new gene encoding Zaire Ebola virus sGP (39, 49) or Marburg virus GP1 (51) between the VSV G and L genes (Fig. 1). These cDNAs were transfected into BSR-T7 cells, and rVSVs were rescued in all cases. The rescued viruses were designated VSVΔG/MARVGP, VSVΔG/ZEBOVGP, VSVΔG/LASVGPC, VSV/MARVGP1, and VSV/ZEBOVsGP.
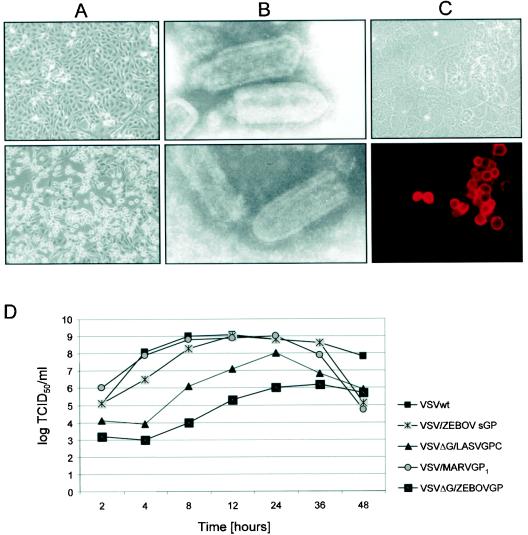
Infection of VeroE6 cells with rVSVs resulted in cytopathic effect (Fig. 2A), which, in general, appeared much earlier than the cytopathic effect observed following infection with the authentic viral hemorrhagic fever pathogens. The cytopathic effect was strong and resembled that of wild-type VSV, indicating that the recombinant viruses replicate similarly. Electron microscopy studies of negatively contrasted rVSV progeny particles demonstrated that replacement of the VSV G with a foreign transmembrane glycoprotein and the insertion of an additional gene had no impact on the morphology of the virions (Fig. 2B). Regardless of the inserted glycoprotein, rVSVs showed typical bullet-shaped rhabdovirus morphology and contained an electron-dense bullet-shaped nucleocapsid, which was bound by an envelope. The viral envelopes were coated with surface projections consisting of the foreign glycoprotein, indicating that the foreign glycoproteins could completely substitute for VSV G in assembly and did not influence particle structure formation (Fig. 2B).
FIG. 2.
Characterization of rescued rVSVs. Rescued rVSVs were used to infect VeroE6 cells at an MOI of 0.1 PFU/cell. (A) Cytopathogenic effect of infected VeroE6 cells is shown by phase-contrast microscopy 24 h postinfection with VSVΔG/MARVGP (lower panel) in comparison with a mock-infected culture (upper panels). (B) Particle morphology. Electron micrographs show wild-type VSV (upper panel) and VSVΔG/MARVGP (lower panel). (C) Immunofluorescence staining of VeroE6 cells infected with VSVΔG/MARVGP with the GP-specific monoclonal antibody 5EII (dilution, 1:1,000) (lower panel). The upper panel shows the same cells in bright-field microscopy. (D) Growth curves. VeroE6 cells were infected with wild-type VSV (VSVwt), VSV/ZEBOVsGP, VSV/MARVGP1, VSVΔG/ZEBOVGP, VSVΔG/LASVGP, or VSVΔG/MARVGP at an MOI of 10. Supernatants were collected at the indicated times and titrated by defining the TCID50.
Replication of the recombinant viruses under single-step growth conditions was examined in VeroE6 cells infected at an MOI of 10. Supernatant fluids were harvested at various times, and the virus yields were measured by TCID50. The recombinant viruses containing additional transcription units (VSV/ZEBOVsGP and VSV/MARVGP1) were not attenuated in their growth kinetics, with maximum titers occurring between approximately 8 and 12 h postinfection, as observed for wild-type VSV (Fig. 2D). rVSVs with a replacement of the VSV glycoprotein, such as VSVΔG/LASVGPC and VSVΔG/ZEBOVGP, reached maximum titers at approximately 24 and 36 h postinfection, respectively, indicating attenuation for all rVSVs if VSV G was replaced with a foreign transmembrane glycoprotein.
Previous studies have shown that efficient budding requires the presence of the cytoplasmic domain of the VSV G but that particular motifs are not required (40). Our results indicated that the cytoplasmic domains of the Marburg virus, Zaire Ebola virus, and Lassa virus glycoproteins provided sufficient signals for budding. However, these signals seem to be less optimal, as indicated by the attenuated growth kinetics (Fig. 2D). The reduction in virus titers could also be explained by a reduced expression rate or delayed processing of the foreign glycoprotein, resulting in decreased particle maturation.
The biosynthesis and processing of the foreign glycoproteins seemed to occur in the same manner as during infection with the authentic viral hemorrhagic fever viruses. Immunofluorescence staining, exemplarily shown for VSVΔG/MARVGP-infected VeroE6 cells with a GP-specific monoclonal antibody, detected Marburg virus glycoprotein on the surface of infected cells (Fig. 2C). Proteolytic processing of the Marburg virus glycoprotein into the two cleavage fragments, GP1 (160 kDa) and GP2 (38 kDa), is shown in Fig. 3A. The cleavage of Marburg virus glycoprotein was significantly reduced when the infected cells were treated with the decanoylated peptidyl chloromethylketone decRVKR-cmk, a potent inhibitor of the subtilisin-like endoprotease furin (Fig. 3A, lane 2) (12, 50, 51).
FIG. 3.
Biosynthesis of the foreign glycoproteins expressed after infection with rVSVs. VeroE6 cells were infected with rVSVs at an MOI of 10. (A) For cells infected with VSVΔG/MARVGP, proteins were pulse labeled at 24 h postinfection for 30 min with 20 μCi of [35S]cysteine per ml and chased for 240 min. GP-specific proteins were immunoprecipitated from cell lysates with mouse anti-Marburg virus GP immunoglobulin (II9G4) (dilution, 1:800) and analyzed on SDS-10% PAGE under reducing conditions. The presence of decRVKR (25 μM) during labeling and chase abolished cleavage of pre-GP (lane 2). (B) For cells infected with VSVΔG/EBOVGP, cells were lysed 24 h postinfection and analyzed by Western blotting with a GP1-specific antibody at a dilution of 1:4,000 (lane 1) and GP2-specific rabbit antiserum at a dilution of 1:2,000 (lane 2). (C) For cells infected with VSVΔG/LASVGPC, cells were lysed 24 h postinfection and analyzed by Western blotting with a GP2-specific antiserum (dilution, 1:2,000). (D) For cells infected with wild-type VSV (VSVwt) (lane 1), VSV/ZEBOVsGP (lane 2), and VSV/MARVGP1 (lane 3), supernatants were analyzed 12 h postinfection by Western blotting with a VSV G-specific antibody (dilution, 1:1,000), a Zaire Ebola virus GP-specific antibody (12/1.1; dilution, 1:4,000), and a Marburg virus GP1-specific antibody (5EII; dilution, 1:4,000).
Expression and proteolytic processing of Zaire Ebola virus GP and Lassa virus GPC were demonstrated by immunoblot analysis. The two cleavage fragments of the Zaire Ebola virus transmembrane glycoprotein, GP1 (140k Da) and GP2 (26k Da), were detected with a Zaire Ebola virus-specific antiserum and a monospecific anti-GP2 serum (Fig. 3B). Figure 3C demonstrates the cleavage of the Lassa virus glycoprotein precursor GPC (76 kDa) into GP1 (44 kDa) and GP2 (36 kDa). In this case, detection was performed with a specific antiserum raised against the carboxyl terminus of GP2. In addition to the precursor (not fully cleaved) and the GP2 fragment, an unknown 10-kDa fragment was detected, which needs further attention. Expression of the soluble glycoproteins by the rVSVs is shown in Fig. 3D. In addition to VSV G, which was expressed following infection of VeroE6 cells with wild-type VSV (Fig. 3D, lane 1), VSV/ZEBOVsGP (Fig. 3D, lane 2), and VSV/MARVGP1 (Fig. 3D, lane 3), Zaire Ebola virus sGP and Marburg virus GP1 were detected in supernatants of cells infected with the respective rVSVs (Fig. 3D, lanes 2 and 3, respectively).
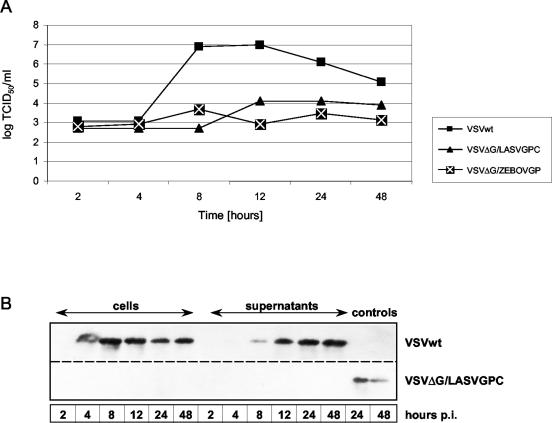
Replacement of VSV G with foreign glycoproteins should result in a change in cell tropism. Therefore, by manipulating the glycoprotein, target cell specificity can be influenced. This property has already been utilized by constructing VSVΔG/GFP particles complemented with the glycoproteins of Zaire Ebola virus and Reston ebolavirus (in trans) to determine the susceptibility of different cell lines (18, 47). To investigate a change in cell tropism, we used infection of Jurkat cells (a human T-cell leukemia clone), which are known to be susceptible to wild-type VSV but not Zaire Ebola virus, Marburg virus, or Lassa virus (5, 16, 30). Wild-type VSV reached maximum titers between 8 and 12 h postinfection, whereasVSVΔG/LASVGPC, VSVΔG/ZEBOVGP, and VSVΔG/MARVGP failed to replicate in Jurkat cells (Fig. 4A; data for VSVΔG/MARVGP not shown). This result was confirmed by immunoblot assays targeting the production of the VSV nucleoprotein in the infected cells and virus particle release into the culture medium over a period of 48 h. No viral protein production could be detected in Jurkat cells infected with VSVΔG/LASVGPC, VSVΔG/ZEBOVGP, or VSVΔG/MARVGP (Fig. 4B; data for VSVΔG/ZEBOVGP and VSVΔG/MARVGP not shown). rVSVs carrying an additional transcription unit (VSV/ZEBOVsGP and VSV/MARVGP1) replicated like wild-type VSV in Jurkat cells (data not shown). Thus, the tropism of the recombinant viruses was dependent on the transmembrane glycoprotein, as expected, and was not influenced by the additional soluble glycoproteins expressed from an additional transcription unit.
FIG. 4.
Cell tropism of rVSVs. Jurkat cells were infected with wild-type VSV (VSVwt), VSVΔG/LASVGPC, or VSVΔG/EBOVGP at an MOI of 10. (A) Virus production. Virus titers for the indicated time points were measured in VeroE6 cells by determining the TCID50 /ml. (B) Protein expression. At the indicated times, cells and supernatants were harvested, and virus growth was demonstrated by Western blotting with a rabbit serum raised against the VSV nucleoprotein (N) (dilution, 1:2,000). Controls included mock-infected Jurkat cells (upper panel) and VSVΔG/LASVGP-infected VeroE6 cells (lower panel).
An advantage of replication-competent recombinant viruses is their potential use in vivo, where multiple replication cycles are necessary. This includes, for example, the investigation of host range or organ tropism and use as potential vaccine vectors. In order to determine changes in pathogenicity in vivo, we infected 6-week-old female BALB/c mice intraperitoneally with wild-type VSV and each of the different rVSVs described in this study. None of the mice displayed weight loss, usually a sensitive indicator of a symptomatic infection, or developed any clinical symptoms (Table 1). Viremia was not detectable 3 days after infection, suggesting that systemic virus replication in mice is transient and may only occur at selected locations that are not easily accessible.
TABLE 1.
Pathogenicity of VSV and vVSV
| Virus | No. of mice with symptoms/no. in group
|
||||
|---|---|---|---|---|---|
| After 1st infection | After 2nd infection | After challenge with Zaire Ebola virus | No. of survivors at day 28 after challenge | Mean time to death (days) | |
| None (naïve controls) | N/Aa | N/A | 4/4 | 0/4 | 5.8 |
| Wild-type VSV | 0/5 | 0/5 | 5/5 | 0/5 | 5.5 |
| VSVΔG/LASVGPC | 0/5 | 0/5 | 5/5 | 0/5 | 7.2 |
| VSVΔG/MARVGP | 0/5 | 0/5 | 5/5 | 0/5 | 6.6 |
| VSVΔG/ZEBOVGP | 0/5 | 0/5 | 0/5 | 5/5 | N/A |
| Gamma-irradiated VSVΔG/EBOVGP | 0/5 | 0/5 | 5/5 | 0/5 | 7 |
| VSV/ZEBOVsGP | 0/5 | 0/5 | N/Db | N/D | N/A |
| VSV/MARVGP1 | 0/5 | 0/5 | N/D | N/D | N/A |
N/A, not applicable.
N/D, not determined.
In a follow-up study (S. M. Jones, H. Feldmann, U. Ströher, J. B. Geisbert, L. Fernando, V. Volchkov, H.-D. Klenk, N. J. Sullivan, P. B. Jahrling, and T. W. Geisbert, submitted for publication), we infected guinea pigs and nonhuman primates (Macaca fascicularis) with VSVΔG/ZEBOVGP and VSVΔG/MARVGP. Despite low-level transient viremia in the nonhuman primates (detectable on day 2 postinfection; undetectable on day 4 postinfection), none of the animals showed signs of clinical disease, nor was virus shedding detected. The results obtained from infection of three animal species indicated that the incorporation of the foreign glycoproteins did not alter the in vivo biological phenotype of wild-type VSV.
VSVΔG/ZEBOVGP was investigated further for a potential protective effect against a lethal Zaire Ebola virus challenge with the mouse-adapted strain of Zaire Ebola virus (1). In a limited study including five animals per group, protection could be achieved after two infections with VSVΔG/ZEBOVGP prior to challenge with 1,000 LD50 of the mouse-adapted strain (Table 1). VSVΔG/MARVGP, VSVΔG/LASVGP, and wild-type VSV infection did not result in protection, indicating a specific protective immune response upon infection with VSVΔG/ZEBOVGP. In contrast to the nonprotected animals, Zaire Ebola virus replication was undetectable in blood (no viremia) and organs of the protected animals, suggesting complete protection in this model upon immunizationwith VSVΔG/ZEBOVGP. Gamma-inactivated VSVΔG/ZEBOVGP did not protect the mice against a lethal challenge, demonstrating that virus replication was needed to induce protective immunity (Table 1).
In conclusion, we generated replication-competent rVSVs carrying glycoproteins derived from filoviruses and arenaviruses as well as viruses carrying additional transcription units for the expression of soluble filovirus glycoproteins. All recombinant viruses exhibited rhabdovirus morphology and replicated cytolytically in tissue culture. The recombinant viruses carrying foreign transmembrane proteins but not the viruses with additional transcription units were attenuated in growth. The synthesis and processing of the foreign glycoproteins were authentic, and the cell tropism was mediated by the transmembrane glycoprotein. None of the recombinant viruses were pathogenic in mice (this study) or guinea pigs and nonhuman primates (Macaca fascicularis) (Jones et al., submitted for publication), and VSVΔG/ZEBOVGP mediated protection in mice against a lethal Zaire Ebola virus challenge. The precise mechanism of protection for mice requires further characterization. These rVSVs thus represent excellent systems for studying the role of glycoproteins in cell tropism, immune response, and pathogenesis in vivo and in vitro. Protection in mice is not necessarily predictive of protection in nonhuman primates, the gold standard for Ebola virus challenge experiments (13). Nevertheless, we are encouraged to develop rVSVs further as a vaccine platform against Ebola virus and, thus, an alternative approach to the currently existing DNA priming-adenovirus boosting and accelerated adenovirus-based strategies, which both have shown intriguing protection in nonhuman primates against lethal Zaire Ebola virus challenge (45, 46).
Acknowledgments
We thank Daryl Dick for critical review of the manuscript. We thank John Rose (Yale University) and Klaus Conzelmann (University of Munich) for kindly providing us with the vesicular stomatitis virus reverse genetics system and the BSR-T7 cell line, respectively. We are grateful to Ayato Takada (University of Tokyo) and Yoshihiro Kawaoka (University of Wisconsin and University of Tokyo) for providing the monoclonal antibody (12/1.1) against the Zaire Ebola virus glycoprotein, to Oliver Lenz (University of Marburg) for providing the anti-Lassa virus GP2 immunoglobulins, to M. Hevey and A. Schmaljohn (U.S. Army Medical Research Institute of Infectious Diseases, Fort Detrick, Md.) for providing the monoclonal antibodies (5EII and II9G4) against the Marburg virus glycoprotein, and to Yan Li (National Microbiology Laboratory, Health Canada) for providing the vesicular stomatitis virus nucleoprotein antiserum.
This work was supported by grants from the Canadian Institutes of Health Research (MOP-43921) and the Deutsche Forschungsgemeinschaft.
REFERENCES
- 1.Bray, M., K. Davis, T. Geisbert, C. Schmaljohn, and J. Huggins. 1998. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J. Infect. Dis. 178:651-661. [DOI] [PubMed] [Google Scholar]
- 2.Buchholz, U. J., S. Finke, and K. K. Conzelmann. 1999. Generation of bovine respiratory syncytial virus (BRSV) from cDNA: BRSV NS2 is not essential for virus replication in tissue culture, and the human RSV leader region acts as a functional BRSV genome promoter. J. Virol. 73:251-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buchmeier, M. J. 2002. Arenaviruses: protein structure and function. Curr. Top. Microbiol. Immunol. 262:159-173. [DOI] [PubMed] [Google Scholar]
- 4.Buchmeier, M. J., M. D. Bowen, and C. J. Peters. 2001. Arenaviridae: The viruses and their replication, p. 1635-1668. In D. M. Knipe, P. M. Howley, D. E. Griffin, M. A. Martin, R. A. Lamb, and B. Roizman (ed.), Fields virology, vol. 2. Lippincott Williams & Wilkins, Philadelphia, Pa. [Google Scholar]
- 5.Cao, W., M. D. Henry, P. Borrow, H. Yamada, J. H. Elder, E. V. Ravkov, S. T. Nichol, R. W. Compans, K. P. Campbell, and M. B. A. Oldstone. 1998. Identification of dystroglycan as a receptor for lymphocytic choriomeningitis virus and Lassa fever virus. Science 282:2079-2081. [DOI] [PubMed] [Google Scholar]
- 6.Eichler, R., O. Lenz, T. Strecker, M. Eickmann, H. D. Klenk, and W. Garten. 2003. Identification of Lassa virus glycoprotein signal peptide as a trans-acting maturation factor. EMBO Rep. 4:1084-1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eichler, R., O. Lenz, T. Strecker, and W. Garten. 2003. Signal peptide of Lassa virus glycoprotein GP-C exhibits an unusual length. FEBS Lett. 538:203-206. [DOI] [PubMed] [Google Scholar]
- 8.Feldmann, H., S. Jones, H. D. Klenk, and H. J. Schnittler. 2003. Ebola virus: from discovery to vaccine. Nat. Rev. Immunol. 3:677-685. [DOI] [PubMed] [Google Scholar]
- 9.Feldmann, H., V. E. Volchkov, V. A. Volchkova, U. Stroher, and H. D. Klenk. 2001. Biosynthesis and role of filoviral glycoproteins. J. Gen. Virol. 82:2839-2848. [DOI] [PubMed] [Google Scholar]
- 10.Fredericksen, B. L., and M. A. Whitt. 1998. Attenuation of recombinant vesicular stomatitis viruses encoding mutant glycoproteins demonstrate a critical role for maintaining a high pH threshold for membrane fusion in viral fitness. Virology 240:349-358. [DOI] [PubMed] [Google Scholar]
- 11.Freer, G., C. Burkhart, I. Ciernik, M. F. Bachmann, H. Hengartner, and R. M. Zinkernagel. 1994. Vesicular stomatitis virus Indiana glycoprotein as a T-cell-dependent and -independent antigen. J. Virol. 68:3650-3655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garten, W., S. Hallenberger, D. Ortmann, W. Schafer, M. Vey, H. Angliker, E. Shaw, and H. D. Klenk. 1994. Processing of viral glycoproteins by the subtilisin-like endoprotease furin and its inhibition by specific peptidylchloroalkylketones. Biochimie 76:217-225. [DOI] [PubMed] [Google Scholar]
- 13.Geisbert, T. W., P. Pushko, K. Anderson, J. Smith, K. J. Davis, and P. B. Jahrling. 2002. Evaluation in nonhuman primates of vaccines against Ebola virus. Emerg. Infect. Dis. 8:503-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grigera, P. R., M. P. Marzocca, A. V. Capozzo, L. Buonocore, R. O. Donis, and J. K. Rose. 2000. Presence of bovine viral diarrhea virus (BVDV) E2 glycoprotein in VSV recombinant particles and induction of neutralizing BVDV antibodies in mice. Virus Res. 69:3-15. [DOI] [PubMed] [Google Scholar]
- 15.Haglund, K., J. Forman, H. G. Krausslich, and J. K. Rose. 2000. Expression of human immunodeficiency virus type 1 Gag protein precursor and envelope proteins from a vesicular stomatitis virus recombinant: high-level production of virus-like particles containing HIV envelope. Virology 268:112-121. [DOI] [PubMed] [Google Scholar]
- 16.Hobbs, J. A., R. H. Schloemer, G. Hommel-Berrey, and Z. Brahmi. 2001. Caspase-3-like proteases are activated by infection but are not required for replication of vesicular stomatitis virus. Virus Res. 80:53-65. [DOI] [PubMed] [Google Scholar]
- 17.Ito, H., S. Watanabe, A. Sanchez, M. A. Whitt, and Y. Kawaoka. 1999. Mutational analysis of the putative fusion domain of Ebola virus glycoprotein. J. Virol. 73:8907-8912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ito, H., S. Watanabe, A. Takada, and Y. Kawaoka. 2001. Ebola virus glycoprotein: proteolytic processing, acylation, cell tropism, and detection of neutralizing antibodies. J. Virol. 75:1576-1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jayakar, H. R., and M. A. Whitt. 2002. Identification of two additional translation products from the matrix (M) gene that contribute to vesicular stomatitis virus cytopathology. J. Virol. 76:8011-8018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson, J. E., M. J. Schnell, L. Buonocore, and J. K. Rose. 1997. Specific targeting to CD4+ cells of recombinant vesicular stomatitis viruses encoding human immunodeficiency virus envelope proteins. J. Virol. 71:5060-5068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kärber, G. 1931. Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Arch. Exp. Pathol. Pharmakol. 162:480-487. [Google Scholar]
- 22.Kopecky, S. A., and D. S. Lyles. 2003. Contrasting effects of matrix protein on apoptosis in HeLa and BHK cells infected with vesicular stomatitis virus are due to inhibition of host gene expression. J. Virol. 77:4658-4669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kretzschmar, E., L. Buonocore, M. J. Schnell, and J. K. Rose. 1997. High-efficiency incorporation of functional influenza virus glycoproteins into recombinant vesicular stomatitis viruses. J. Virol. 71:5982-5989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kundig, T. M., I. Castelmur, M. F. Bachmann, D. Abraham, D. Binder, H. Hengartner, and R. M. Zinkernagel. 1993. Fewer protective cytotoxic T-cell epitopes than T-helper-cell epitopes on vesicular stomatitis virus. J. Virol. 67:3680-3683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lawson, N. D., E. A. Stillman, M. A. Whitt, and J. K. Rose. 1995. Recombinant vesicular stomatitis viruses from DNA. Proc. Natl. Acad. Sci. USA 92:4477-4481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lenz, O., J. ter Meulen, H. D. Klenk, N. G. Seidah, and W. Garten. 2001. The Lassa virus glycoprotein precursor GP-C is proteolytically processed by subtilase SKI-1/S1P. Proc. Natl. Acad. Sci. USA 98:12701-12705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Letchworth, G. J., L. L. Rodriguez, and J. Del Barrera. 1999. Vesicular stomatitis. Vet. J. 157:239-260. [DOI] [PubMed] [Google Scholar]
- 28.Mastromarino, P., C. Conti, P. Goldoni, B. Hauttecoeur, and N. Orsi. 1987. Characterization of membrane components of the erythrocyte involved in vesicular stomatitis virus attachment and fusion at acidic pH. J. Gen. Virol. 68:2359-2369. [DOI] [PubMed] [Google Scholar]
- 29.Montel, A. H., G. Hommel-Berrey, and Z. Brahmi. 1997. Fas-mediated cytotoxicity induces degradation of vesicular stomatitis virus RNA transcripts and reduces viral titer. Mol. Immunol. 34:1055-1066. [DOI] [PubMed] [Google Scholar]
- 30.Peters, C. J., P. B. Jahrling, T. G. Ksiazek, E. D. Johnson, and H. W. Lupton. 1992. Filovirus contamination of cell cultures. Dev. Biol. Stand. 76:267-274. [PubMed] [Google Scholar]
- 31.Quinones-Kochs, M. I., L. Buonocore, and J. K. Rose. 2002. Role of N-linked glycans in a human immunodeficiency virus envelope glycoprotein: effects on protein function and the neutralizing antibody response. J. Virol. 76:4199-4211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reed, L. J., and H. A. Muench. 1938. A simple method of determining fifty percent end points. Am. J. Hyg. 27:493-497. [Google Scholar]
- 33.Roberts, A., E. Kretzschmar, A. S. Perkins, J. Forman, R. Price, L. Buonocore, Y. Kawaoka, and J. K. Rose. 1998. Vaccination with a recombinant vesicular stomatitis virus expressing an influenza virus hemagglutinin provides complete protection from influenza virus challenge. J. Virol. 72:4704-4711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robison, C. S., and M. A. Whitt. 2000. The membrane-proximal stem region of vesicular stomatitis virus G protein confers efficient virus assembly. J. Virol. 74:2239-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rose, J. K., and M. A. Whitt. 2001. Rhabdoviridae, p. 1221-1244. In D. M. Knipe and P. M. Howley (ed.), Fields Virology, 4th ed., vol. 1. Lippincott Williams & Wilkins, Philadelphia, Pa. [Google Scholar]
- 36.Rose, N. F., P. A. Marx, A. Luckay, D. F. Nixon, W. J. Moretto, S. M. Donahoe, D. Montefiori, A. Roberts, L. Buonocore, and J. K. Rose. 2001. An effective AIDS vaccine based on live attenuated vesicular stomatitis virus recombinants. Cell 106:539-549. [DOI] [PubMed] [Google Scholar]
- 37.Rose, N. F., A. Roberts, L. Buonocore, and J. K. Rose. 2000. Glycoprotein exchange vectors based on vesicular stomatitis virus allow effective boosting and generation of neutralizing antibodies to a primary isolate of human immunodeficiency virus type 1. J. Virol. 74:10903-10910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sanchez, A., A. S. Khan, S. R. Zaki, G. J. Nabel, T. G. Ksiazek, and C. J. Peters. 2001. Filoviridae: Marburg and Ebola viruses, p. 1279-1304. In D. M. Knipe, P. M. Howley, D. E. Griffin, M. A. Martin, R. A. Lamb, and B. Roizman (ed.), Fields virology, vol. 1. Lippincott Williams & Wilkins, Philadelphia, Pa. [Google Scholar]
- 39.Sanchez, A., S. G. Trappier, B. W. Mahy, C. J. Peters, and S. T. Nichol. 1996. The virion glycoproteins of Ebola viruses are encoded in two reading frames and are expressed through transcriptional editing. Proc. Natl. Acad. Sci. USA 93:3602-3607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schnell, M. J., L. Buonocore, E. Boritz, H. P. Ghosh, R. Chernish, and J. K. Rose. 1998. Requirement for a non-specific glycoprotein cytoplasmic domain sequence to drive efficient budding of vesicular stomatitis virus. EMBO J. 17:1289-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schnell, M. J., L. Buonocore, E. Kretzschmar, E. Johnson, and J. K. Rose. 1996. Foreign glycoproteins expressed from recombinant vesicular stomatitis viruses are incorporated efficiently into virus particles. Proc. Natl. Acad. Sci. USA 93:11359-11365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schnell, M. J., L. Buonocore, M. A. Whitt, and J. K. Rose. 1996. The minimal conserved transcription stop-start signal promotes stable expression of a foreign gene in vesicular stomatitis virus. J. Virol. 70:2318-2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spearman, C. 1908. The method of right and wrong cases (constant stimuli) with Gauss formulae. Br. J. Psychol. 2:227-242. [Google Scholar]
- 44.Stillman, E. A., and M. A. Whitt. 1999. Transcript initiation and 5′-end modifications are separable events during vesicular stomatitis virus transcription. J. Virol. 73:7199-7209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sullivan, N. J., T. W. Geisbert, J. B. Geisbert, L. Xu, Z. Y. Yang, M. Roederer, R. A. Koup, P. B. Jahrling, and G. J. Nabel. 2003. Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates. Nature 424:681-684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sullivan, N. J., A. Sanchez, P. E. Rollin, Z. Y. Yang, and G. J. Nabel. 2000. Development of a preventive vaccine for Ebola virus infection in primates. Nature 408:605-609. [DOI] [PubMed] [Google Scholar]
- 47.Takada, A., C. Robison, H. Goto, A. Sanchez, K. G. Murti, M. A. Whitt, and Y. Kawaoka. 1997. A system for functional analysis of Ebola virus glycoprotein. Proc. Natl. Acad. Sci. USA 94:14764-14769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tesh, R. B., P. H. Peralta, and K. M. Johnson. 1969. Ecologic studies of vesicular stomatitis virus. I. Prevalence of infection among animals and humans living in an area of endemic VSV activity. Am. J. Epidemiol. 90:255-261. [DOI] [PubMed] [Google Scholar]
- 49.Volchkov, V. E., S. Becker, V. A. Volchkova, V. A. Ternovoj, A. N. Kotov, S. V. Netesov, and H. D. Klenk. 1995. GP mRNA of Ebola virus is edited by the Ebola virus polymerase and by T7 and vaccinia virus polymerases. Virology 214:421-430. [DOI] [PubMed] [Google Scholar]
- 50.Volchkov, V. E., H. Feldmann, V. A. Volchkova, and H. D. Klenk. 1998. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc. Natl. Acad. Sci. USA 95:5762-5767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Volchkov, V. E., V. A. Volchkova, U. Stroher, S. Becker, O. Dolnik, M. Cieplik, W. Garten, H. D. Klenk, and H. Feldmann. 2000. Proteolytic processing of Marburg virus glycoprotein. Virology 268:1-6. [DOI] [PubMed] [Google Scholar]
- 52.Yang, Z., R. Delgado, L. Xu, R. F. Todd, E. G. Nabel, A. Sanchez, and G. J. Nabel. 1998. Distinct cellular interactions of secreted and transmembrane Ebola virus glycoproteins. Science 279:1034-1037. [DOI] [PubMed] [Google Scholar]
- 53.Zinkernagel, R. M., B. Adler, and J. J. Holland. 1978. Cell-mediated immunity to vesicular stomatitis virus infections in mice. Exp. Cell Biol. 46:53-70. [DOI] [PubMed] [Google Scholar]