Abstract
Payers are considering bundled payments for inpatient surgery, combining provider reimbursements into a single payment for the entire episode. We found that current Medicare episode payments for certain inpatient procedures varied by 49–130 percent across hospitals sorted into five payment groups. Intentional differences in payments attributable to such factors as geography or illness severity explained much of this variation. But after adjustment for these differences, per episode payments to the highest-cost hospitals were higher than those to the lowest-cost facilities by up to $2,549 for colectomy and $7,759 for back surgery. Postdischarge care accounted for a large proportion of the variation in payments, as did discretionary physician services, which may be driven in turn by variations in surgeons’ practice styles. Our study suggests that bundled payments could yield sizable savings for payers, although the effect on individual institutions will vary because hospitals that were relatively expensive for one procedure were often relatively inexpensive for others. More broadly, our data suggest that many hospitals have considerable room to improve their cost efficiency for inpatient surgery and should look for patterns of excess utilization, particularly among surgical specialties, other inpatient specialist consultations, and various types of postdischarge care.
Surgery represents a large component of national health care spending: More than forty-five million procedures are performed each year in US hospitals.1 The large variation in payments per inpatient surgery episode suggests that there are opportunities for reducing these costs considerably.2
Toward this end, the Centers for Medicare and Medicaid Services (CMS) is evaluating bundled payments for inpatient surgery, incorporating into a single payment reimbursements to hospitals, physicians, and other providers involved in care around a surgical episode.3–5 CMS has already established the Medicare Acute Care Episode demonstration project, which involves a single payment for both Part A and Part B services for beneficiaries undergoing a variety of cardiac and orthopedic inpatient procedures.3,6 Private payers have expressed interest in following suit.7,8
From the perspective of CMS and other payers, bundled payments are intended to improve care coordination and reduce the use of duplicative or unnecessary services. The payments are designed to accomplish this goal by creating financial incentives for hospitals and affiliated providers to keep the costs of surgical and acute care episodes below the lump-sum payment.3,4,9
The magnitude of the savings will ultimately depend on the procedures and services included in bundled payments and on decisions about where to set reimbursement rates. Savings will also hinge on the extent of true variation in current payments.3 Obviously, extensive variation in current episode payments implies greater potential savings for payers than would be the case with less variation.
For hospitals and health systems, the implications of bundled payments will also depend on patterns of variation in payments across procedures and specialties. Hospitals that are consistently expensive across surgical specialties might face substantial financial risk with bundled payments. Conversely, hospitals that are low cost for a broad spectrum of inpatient surgical services could do quite well from a financial perspective.
It is also conceivable, however, that many hospitals fall between these extremes—that is, they are cost-efficient for some surgical specialties and inefficient for others. In those cases, bundled payments may actually cancel each other out with respect to the hospital’s financial bottom line.
In this context, we studied Medicare payments for hospital, physician, and postdischarge care around episodes of common types of inpatient surgeries. We defined surgical episodes as beginning on the date of hospital admission for the procedure of interest and ending thirty days after the hospital discharge date.
We then assessed the degree to which intentional differences in Medicare payments—such as price differences based on regional wage disparities, cost of living, illness severity, and the expense of caring for underinsured patients—explained variations in episode expenditures. Finally, we examined specific types of services that accounted for the remaining variation in payments around surgical episodes, while also evaluating relationships between episode payments for surgeries performed in the same hospital.
Study Data And Methods
Subjects And Databases
This study was based on complete Medicare claims data for a sample of patients undergoing selected inpatient procedures from January 2005 through November 2007. As described previously,2 we excluded from our analysis patients enrolled in Medicare managed care plans (approximately 16 percent of Medicare patients in 2005), patients under age sixty-five years or over age ninety-nine (approximately 13 percent), and patients not enrolled in both Parts A and B at the time of their procedures (approximately 4 percent).
We identified patients undergoing surgery from the inpatient Medicare Provider Analysis and Review file based on the presence of the appropriate procedure codes from the International Classification of Diseases, Ninth Revision (ICD-9) (specific codes are available from the authors on request). We linked the records for each of these cases to other CMS files containing claims potentially relevant to the surgical episode, including the carrier (that is, the physician), outpatient, home health, skilled nursing facility, long-stay hospital, and durable medical equipment files.2
The study cohorts included patients undergoing surgery between January 1, 2005, and November 30, 2007. To ensure that we included complete postoperative payment data, we excluded patients who had surgery in December 2007. Finally, in an effort to increase the statistical reliability of our hospital payment estimates, we also excluded cases from hospitals performing fewer than thirty of the procedures of interest during the study period.
For this study, we identified patients undergoing the following inpatient procedures (referred to throughout the article as the procedures of interest or the index procedures): hip replacement, coronary artery bypass grafting, back surgery, and colectomy (the surgical removal of all or part of the colon). The first two procedures have been selected by CMS for inclusion in an ongoing demonstration project for bundled payments.6 We added back surgery and colectomy because these procedures are common in the elderly, very expensive, and likely to be associated with substantial costs related to use of services both during the index hospitalization (the first hospitalization in which the primary diagnosis would be treated by one of the specified procedures) and following hospital discharge.
Calculation Of Medicare Payments
For each patient, we analyzed actual Medicare payments, not submitted charges. As described in our previous work,2 and in keeping with the approach employed by the Medicare Payment Advisory Commission, we extracted payment information for all service types from the date of hospital admission for the index procedure to thirty days after the hospital discharge date. We sorted the total payment data into four discrete components: index hospitalization, readmissions, physician services, and care provided after discharge from the short-term acute care hospital. The latter category includes payments for rehabilitation hospitals, home health care, skilled nursing facilities, and nursing homes. We referred to payments for care provided after discharge from the short-term acute care hospital as payments for postdischarge care.
To account for intended differences in Medicare payments—as noted above, these include differences in compensation based on regional wages—we then “price standardized” payments using methods described by researchers with the Dartmouth Atlas of Healthcare,10 which are quite similar to those employed by the Medicare Payment Advisory Commission.
Statistical Analyses
Our first goal was to describe hospital-level variation in Medicare payments for inpatient surgery. For each procedure, we ranked hospitals according to total episode payments and then grouped them into five groups, or quintiles. We reassigned hospital payment quintiles after price standardization and again after adjusting for both price and differences in demographics, comorbidity, and illness severity, or case-mix, among patients treated in different hospitals. To minimize chance variation, we also adjusted all hospital payment estimates for reliability using the empirical Bayes methods described previously.11 Because this technique tends to “shrink” hospital payments toward the mean, we used it to produce conservative estimates of variation in payments across hospitals.
We performed case-mix adjustment using multiple linear regression, accounting for clustering of patients within hospitals. We adjusted for patients’ age, sex, race, admission acuity—or how sick patients were, and therefore what the intensity of services delivered was—and pre-operative length-of-stay. To account for potential differences in procedure mix, such as two-vessel versus four-vessel coronary artery bypass grafting, our models also included the primary procedure code. Using codes developed by Anne Elixhauser and colleagues, we also considered individual comorbidities for inclusion in the risk-adjustment models.12 To minimize confounding by unmeasured differences in patient illness severity and their baseline costliness, we adjusted for expenditures occurring in the six months before surgery.
Finally, we determined hospital-level correlations between price-adjusted and case-mix-adjusted total payments for each pair of procedures. For hip replacement and coronary artery bypass grafting, we also determined whether total episode payments for each hospital were above or below the national average, or mean, for each procedure.
We performed all analyses using the statistical analysis software SAS, version 10, at the 5 percent significance level. The University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board determined that this study was exempt from its oversight.
Study Results
The average total episode payment for Medicare beneficiaries undergoing elective hip replacement, coronary artery bypass grafting, back surgery, or colectomy was $20,807, $42,194, $26,540, and $26,491, respectively. We observed wide variation in total payments around surgical episodes for each of the four procedures (Exhibit 1). With back surgery, for example, hospitals in the highest-cost quintile had total payments that were $22,801 (130 percent) higher than hospitals in the lowest-cost quintile. Similarly, total payments at the highest-cost hospitals were 73 percent, 70 percent, and 48 percent higher than at the lowest-cost hospitals for hip replacement, coronary artery bypass grafting, and colectomy, respectively. Differences in price per service explained a sizable proportion of variation in total payments across hospitals. Nonetheless, after price adjustment, there remained significant differences in total payments at the highest- and lowest-cost hospitals, ranging from $3,869 (16 percent) for colectomy to $15,828 (82 percent) for back surgery (Exhibit 1).
Exhibit 1.
Average Total Medicare Payments Around Episodes Of Four Common Inpatient Procedures, 2005–07
| Procedure | Total payments, by hospital quintile ($)
|
Difference between quintiles 1 and 5
|
|||||
|---|---|---|---|---|---|---|---|
| 1 (lowest cost) | 2 | 3 | 4 | 5 (highest cost) | Dollars | Percent | |
| Hip replacement | |||||||
| Actual cost | 15,997 | 18,314 | 20,126 | 22,441 | 27,676 | 11,679 | 73.0 |
| Cost after price adjustment | 17,524 | 19,477 | 20,837 | 22,252 | 24,963 | 7,439 | 42.5 |
| Cost after price and case-mix adjustment | 17,784 | 19,575 | 20,835 | 22,168 | 24,693 | 6,909 | 38.9 |
| Coronary artery bypass grafting | |||||||
| Actual cost | 34,143 | 38,295 | 41,690 | 46,722 | 57,976 | 23,833 | 69.8 |
| Cost after price adjustment | 38,083 | 40,464 | 42,278 | 44,260 | 47,863 | 9,780 | 25.7 |
| Cost after price and case-mix adjustment | 39,155 | 41,123 | 42,413 | 43,668 | 46,590 | 7,435 | 19.0 |
| Back surgery | |||||||
| Actual cost | 17,571 | 22,103 | 25,436 | 29,606 | 40,372 | 22,801 | 130.0 |
| Cost after price adjustment | 19,353 | 23,382 | 26,007 | 28,953 | 35,181 | 15,828 | 81.8 |
| Cost after price and case-mix adjustment | 23,249 | 24,943 | 26,123 | 27,568 | 31,009 | 7,759 | 33.4 |
| Colectomy | |||||||
| Actual cost | 22,385 | 24,340 | 26,081 | 28,297 | 33,217 | 10,832 | 48.4 |
| Cost after price adjustment | 24,740 | 25,640 | 26,317 | 27,115 | 28,609 | 3,869 | 15.6 |
| Cost after price and case-mix adjustment | 25,372 | 25,956 | 26,341 | 26,835 | 27,922 | 2,549 | 10.1 |
SOURCE Authors’ analysis of 2005–07 national Medicare claims data.
Patients treated at hospitals in the higher-cost quintiles differed from those at lower-cost hospitals in several regards. For all four procedures, higher-cost hospitals treated a larger proportion of black patients and patients with more co-morbidities. These hospitals were also more likely to admit patients on a nonelective basis, particularly before coronary artery bypass grafting and colectomy. As a result, they had longer preoperative lengths-of-stay. Finally, patients treated at hospitals in the higher-cost quintiles had consistently higher expenditures in the six months before the surgical episode (see the online Appendix for more details).13
Although price adjustment had larger effects, accounting for differences in case-mix had the net effect of narrowing variation in total episode payments across hospital quintiles (Exhibit 1). After both price and case-mix were accounted for, however, the total payments at the highest-cost hospitals remained between $2,549 (for colectomy) and $7,759 (for back surgery) higher than at the lowest-cost hospitals (Exhibit 1).
Among different components of the price-adjusted and case-mix-adjusted total payments, postdischarge care accounted for a large proportion of variation in payments for all four procedures (Exhibit 2). Postdischarge care for hip replacement accounted for a greater share—85 percent—of the difference in total payments to hospitals in the first and fifth payment quin-tiles than for any of the other procedures. With coronary artery bypass grafting, payments for the index hospitalization explained a large share of excess payments at the highest-cost hospitals, while with colectomy, readmissions were a more important factor than index hospitalization. Physician services accounted for a smaller, but nontrivial, share of variation in total payments for each procedure, ranging from 9 percent for hip replacement to 13 percent for back surgery (Exhibit 2).
Exhibit 2.
Average Medicare Payments For Different Components Of Care Around Surgical Episodes, By Procedure, 2005–07
| Total payments, by hospital quintile ($)
|
||||
|---|---|---|---|---|
| Component | 1 (lowest cost) | 5 (highest cost) | Difference between quintiles 1 and 5 ($) | Percent of total difference attributed to cost category |
| Hip replacement | ||||
| Index hospitalization | 11,306 | 11,265 | −41 | −0.6 |
| Readmissions | 582 | 1,052 | 470 | 6.8 |
| Physician services | 2,056 | 2,651 | 595 | 8.6 |
| Postdischarge care | 3,840 | 9,725 | 5,885 | 85.2 |
| Total episode | 17,784 | 24,693 | 6,909 | 100.0 |
| Coronary artery bypass grafting | ||||
| Index hospitalization | 29,749 | 33,139 | 3,390 | 45.6 |
| Readmissions | 1,810 | 2,715 | 905 | 12.2 |
| Physician services | 4,762 | 5,571 | 808 | 10.9 |
| Postdischarge care | 2,833 | 5,165 | 2,332 | 31.4 |
| Total episode | 39,154 | 46,590 | 7,435 | 100.0 |
| Back surgery | ||||
| Index hospitalization | 15,535 | 18,464 | 2,929 | 37.8 |
| Readmissions | 891 | 1,569 | 679 | 8.7 |
| Physician services | 4,085 | 5,081 | 996 | 12.8 |
| Postdischarge care | 2,738 | 5,894 | 3,156 | 40.7 |
| Total episode | 23,249 | 31,009 | 7,759 | 100.0 |
| Colectomy | ||||
| Index hospitalization | 18,847 | 19,130 | 283 | 11.1 |
| Readmissions | 988 | 1,893 | 905 | 35.5 |
| Physician services | 3,430 | 3,669 | 239 | 9.4 |
| Postdischarge care | 2,107 | 3,230 | 1,122 | 44.0 |
| Total episode | 25,372 | 27,922 | 2,549 | 100.0 |
SOURCE Authors’ analysis of 2005–07 national Medicare claims data. NOTES Payments are adjusted for price and case-mix. “Index hospitalization” is the first hospitalization in which the primary diagnosis would be treated by one of the specified procedures. Percentages might not sum to 100 because of rounding.
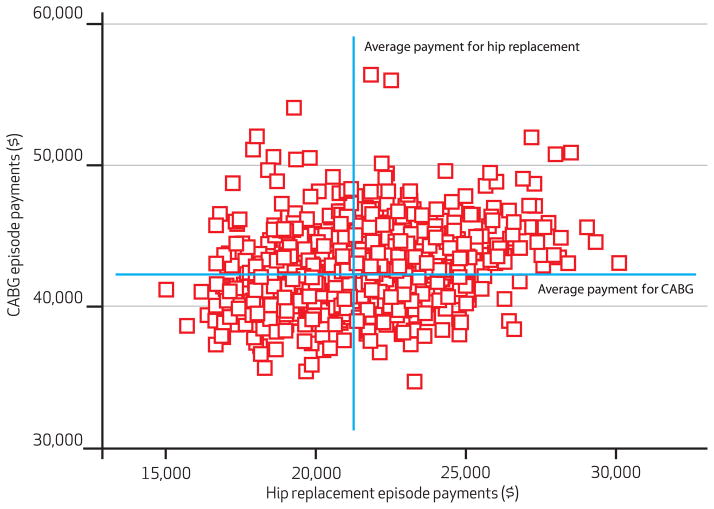
For individual hospitals, correlations between payments for different procedures were generally low, ranging from 0.219 to 0.280 (Exhibit 3). Exhibit 4 shows that 33.3 percent of hospitals were below the national mean for total episode payments for both hip replacement and coronary artery bypass grafting, while 28.3 percent of hospitals were above the national mean for both procedures.
Exhibit 3.
Hospital-Level Correlations Between Total Episode Payments For Four Common Inpatient Procedures, 2005–07
| Hip replacement | Coronary artery bypass grafting | Back surgery | |
|---|---|---|---|
| Coronary artery bypass grafting | 0.260 | — | — |
| Back surgery | 0.263 | 0.280 | — |
| Colectomy | 0.242 | 0.249 | 0.219 |
SOURCE Authors’ analysis of 2005–07 national Medicare claims data.
Exhibit 4.
Relationship Between Total Episode Payments For Coronary Artery Bypass Grafting And Hip Replacement Among Medicare Beneficiaries
SOURCE Authors’ analysis of 2005–07 national Medicare claims data. NOTES Each square represents a unique hospital. The mean total Medicare payment for episodes of hip replacement was $20,807; for coronary artery bypass grafting, it was $42,194. The quadrants indicate hospitals above or below the national mean payment for each procedure, with 28.3 percent of hospitals being above the national mean for both procedures, 33.3 percent being below the mean for both procedures, 18.8 percent being below the mean for hip replacement but above the mean for coronary artery bypass grafting, and 19.6 percent being below the mean for coronary artery bypass grafting but above the mean for hip replacement. CABG is coronary artery bypass grafting.
Discussion
Consistent with our previous work,2 we observed that Medicare payments around episodes of inpatient surgery varied widely across hospitals in the United States. The current study built on this body of research by examining explicitly how much of this variation in episode payments is due to intentional differences in Medicare payment rates—based on, as noted above, such factors as regional wage disparities. We also described the extent to which case-mix differences among providers—for example, the high cost to hospitals of caring for very sick patients—explained this variation. Finally, we identified and examined specific types of services that accounted for the remaining variation in payments around surgical episodes, while also assessing the extent to which there was correlation between episode payments across procedures and specialties.
Intentional differences in Medicare prices accounted for a large share of variation in surgical episode payments. A much smaller proportion could be explained by case-mix. After these two factors were accounted for, however, hospitals in the highest-cost quintile still had total payments that were 10–40 percent—approximately $2,500–7,750, depending on the procedure—higher per episode than hospitals in the lowest-cost quintile (Exhibit 1). This unexplained variation was arguably not a consequence of existing Medicare payment policy and may therefore be unwarranted.
The causes for this unexplained variation are undoubtedly complex. Broadly speaking, it appears to be driven by differences in the use of potentially discretionary physician services and—to a larger extent—in postdischarge care. With physician payments, for example, some services are obligatory—such as those of the operating surgeon and anesthesiologist. Others, including inpatient consultations by hospitalists, critical care physicians, and medical specialists, no doubt vary widely across hospitals.14 The use of postdischarge home health care and rehabilitation facilities for patients undergoing un-complicated procedures is similarly discretionary and for some procedures—such as hip replacement and back surgery—explains a considerable amount of overall variation in payments.
It is also important to recognize that population-level market factors may be pivotal determinants of these discretionary clinical decisions, and the consequent cost variations. This is particularly true for use of postdischarge care. For example, surgeons working in markets with long-term acute care hospitals may be more likely to discharge patients earlier because patients can go to these facilities. Conversely, in regions without long-term acute care hospitals, patients may stay longer in the short-term hospital before being discharged with home health care or to a skilled nursing facility. An important next step, therefore, is to better define the influence of local market factors—including the supply of postacute care providers—on the discretionary clinical decisions that underlie un- explained cost variations.
We observed only weak correlations between episode payments across procedures and specialties. Hospitals that were expensive for one procedure were not necessarily expensive for all surgical services. Thus, it appears that variations in episode payments are specialty-specific, perhaps driven by differences in quality or practice style. Moreover, the absence of hospital-level “cost signatures” suggests that variations attributable to practice style are driven more by the utilization patterns of distinct surgical specialists than by the practices of hospital-based providers, who care for patients across multiple surgical service lines.
Limitations Of The Study
Because our study was based on administrative data, we cannot exclude the possibility that some of the variation in episode payments could be attributable to unmeasured differences in illness severity across hospitals.15 To minimize this risk, we applied numerous restrictions to make our procedure cohorts as homogeneous as possible. We adjusted not only for measurable characteristics of patients at the time of surgery but also for their Medicare payments in the six months prior to surgery. Patients at high-cost hospitals did have higher preoperative expenditures, but these differences were smaller than those in total episode payments. Moreover, it is likely that pre-operative expenditures reflect local practice style and intensity as much as they reflect illness severity.
These data provide important insights on variations in surgical episode costs and the relationship between payments across procedures and specialties. They also highlight the need for additional work in this area. Because cost variations may be influenced by the clinical context, future studies should evaluate the composition of episode payments for other conditions, including medical diagnoses as opposed to surgical procedures alone. Studies examining the relationship between episode payments and patient outcomes are also essential. Along these lines, our own recent analyses suggest that higher episode costs are strongly associated with hospital complication rates.16
Finally, more work is needed to understand the value of discretionary physician services and postdischarge care associated with surgical episodes. For example, a better understanding of whether patients undergoing uncomplicated total hip replacement benefit from a short stay in a rehabilitation hospital or a skilled nursing facility would probably prove invaluable to efforts aimed at improving the efficiency of inpatient surgical care.
Implications For Payment Bundling
These considerations notwithstanding, results from this study have immediate implications for CMS and large private payers as they consider implementing bundled payments around episodes of inpatient surgery. Our findings suggesting the existence of wide variation in payments imply opportunities for substantial savings for CMS and other payers. This is particularly true if—after intentional differences in payment rates and disparities in case-mix are accounted for—bundled payment rates are set below the current national mean. Importantly, however, the potential savings will depend strongly on the procedures and services selected for bundled payment programs.
In its Acute Care Episode demonstration project involving cardiac surgery and joint replacement, CMS is bundling only payments for hospital and inpatient physician services.6,9 Because our findings indicate that outlays for postdischarge care constitute a large and highly variable fraction of total episode payments, it can be argued that strong incentives exist for CMS to expand or refine its bundled payment policies to include spending for home health, rehabilitative, and skilled nursing services provided after hospital discharge. In fact, the national Medicare bundling pilot authorized by the Affordable Care Act of 2010 includes a single payment for both the hospitalization and subsequent postacute care services.9 This modification could strengthen the impact of this policy on the cost-efficiency of surgical episodes.
Our findings suggest that bundled payment programs may have mixed effects on providers. For instance, among the majority of hospitals that are currently low cost for one or more of the services potentially covered by payment bundling, the proposed lump-sum payments may equal or exceed current fee-for-service reimbursements. In many cases, therefore, bundled payments could prove to be a financial “wash” for hospitals, with institutions getting higher payments for some services and lower payments for others. This scenario implies that the incentives may be weak for providers to focus on continued improvements in care coordination and efficiency. At the same time, however, our data suggest that nearly 30 percent of hospitals will be expensive—that is, receiving above the national mean payment—for multiple common procedures. These institutions will have very strong incentives to reduce costs under bundled payment programs aimed at multiple surgical services.
More broadly, our data suggest that many hospitals have considerable room for improving their cost efficiency for inpatient surgery. As a first step toward achieving this goal, hospital leaders should look for patterns of excess utilization across disciplines, perhaps including in-patient specialist consultations and various types of postdischarge care. Because cost efficiency is only weakly correlated across procedures, however, hospitals and health systems will also have to examine patterns of care unique to individual specialties. The CMS demonstration project and the bundling pilot authorized by the Affordable Care Act should serve as signals to hospitals that they need to improve their cost efficiency and reduce variation that leads to excess utilization across procedures.
Acknowledgments
This work was supported by funding from the Agency for Healthcare Research and Quality (Grant No. K08 HS018346-01A1 to David Miller) and the National Institute on Aging (Grant No. P01AG019783-07S1 to John Birkmeyer and Jonathan Skinner). John Birkmeyer and Justin Dimick have equity interests in ArborMetrix, which provides software and services for profiling hospital quality and episode cost efficiency. The company was not involved with this article in any way.
Biographies

David C. Miller is an assistant professor of urology at the University of Michigan Medical School.
In this month’s Health Affairs, David Miller and his coauthors report that current Medicare episode payments for particular inpatient procedures varied by 49 percent to 130 percent across hospitals, with higher per episode payments flowing to the higher-cost hospitals. They conclude that inpatient surgery is ripe for bundled payment experiments—and also suggest other ways in which hospitals could considerably improve their cost efficiency for inpatient surgery.
Miller is an assistant professor of urology at the University of Michigan Medical School. His research focuses on physician-led collaborative quality improvement and on understanding the relationship between physician organizations, integrated delivery systems, and the quality and cost of specialty care. Miller received his medical degree from Washington University in St. Louis.
Cathryn Gust is a senior statistician in the Center for Healthcare Outcomes and Policy at the University of Michigan.
Cathryn Gust is a senior statistician in the Center for Healthcare Outcomes and Policy at the University of Michigan. Her research has concentrated on the relationship of hospital quality and costs of inpatient surgery. She received a master’s degree in statistics from Iowa State University.

Justin B. Dimick is an assistant professor of surgery at the University of Michigan Medical School.
Justin Dimick is an assistant professor of surgery at the University of Michigan Medical School and director of policy research at the Center for Healthcare Outcomes and Policy. His research focuses on two main areas: developing better approaches for measuring hospital quality and evaluating the effectiveness of different policy options for improving quality and reducing costs with inpatient medical care. He earned his medical degree from the Johns Hopkins University Medical School.

Nancy Birkmeyer is an associate professor of surgery, University of Michigan Medical School.
Nancy Birkmeyer is an associate professor in the Department of Surgery, University of Michigan Medical School, and a senior scientist in the university’s Center for Healthcare Outcomes and Policy. Birkmeyer received a master of science degree in epidemiology from Harvard University and held a fellowship there in the epidemiology of cardiovascular disease. She is married to John Birkmeyer.

Jonathan Skinner is the John Sloan Dickey Third Century Professor of Economics at the Dartmouth Institute for Health Policy and Clinical Practice.
Jonathan Skinner is the John Sloan Dickey Third Century Professor of Economics at the Dartmouth Institute for Health Policy and Clinical Practice. His research interests include the economics of health and health care, the Medicare program, and the savings behavior of aging baby boomers. He is a research associate with the National Bureau of Economic Research, an associate editor of the American Economic Journal: Public Policy, and a former editor of the Journal of Human Resources. He was elected to the Institute of Medicine in 2007. Skinner received his doctorate in economics from the University of California, Los Angeles.

John D. Birkmeyer is the George D. Zuidema Professor of Surgery at the University of Michigan Medical School.
John Birkmeyer is the George D. Zuidema Professor of Surgery, and he directs the Center for Healthcare Outcomes and Policy at the University of Michigan. A member of the Institute of Medicine, he has focused his research career on understanding the main determinants of variation in hospital performance and strategies for improvement. He received his medical degree from Harvard Medical School and completed his surgical training and a fellowship in medical informatics at Dartmouth.
Contributor Information
David C. Miller, Email: dcmiller@med.umich.edu, Assistant professor of urology at the University of Michigan Medical School, in Ann Arbor
Cathryn Gust, Senior statistician in the Center for Healthcare Outcomes and Policy at the University of Michigan.
Justin B. Dimick, Assistant professor of surgery at the University of Michigan Medical School
Nancy Birkmeyer, Associate professor of surgery at the University of Michigan Medical School.
Jonathan Skinner, The John Sloan Dickey Third Century Professor of Economics at the Dartmouth Institute for Health Policy and Clinical Practice, in Hanover, New Hampshire.
John D. Birkmeyer, The George D. Zuidema Professor of Surgery at the University of Michigan Medical School. He directs the Center for Healthcare Outcomes and Policy at the University of Michigan
NOTES
- 1.Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WB, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372(9633):139–44. doi: 10.1016/S0140-6736(08)60878-8. [DOI] [PubMed] [Google Scholar]
- 2.Birkmeyer JD, Gust C, Baser O, Dimick JB, Sutherland JM, Skinner JS. Medicare payments for common inpatient procedures: implications for episode-based payment bundling. Health Serv Res. 2010;45(6):1783–95. doi: 10.1111/j.1475-6773.2010.01150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hussey PS, Sorbero ME, Mehrotra A, Liu H, Damberg CL. Episode-based performance measurement and payment: making it a reality. Health Aff (Millwood) 2009;28(5):1406–17. doi: 10.1377/hlthaff.28.5.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chernew M. Bundled payment systems: can they be more successful this time. Health Serv Res. 2010;45(5 Pt 1):1141–7. doi: 10.1111/j.1475-6773.2010.01173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hackbarth G, Reischauer R, Mutti A. Collective accountability for medical care—toward bundled Medicare payments. N Engl J Med. 2008;359(1):3–5. doi: 10.1056/NEJMp0803749. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare and Medicaid Services. Acute Care Episode Demonstration [Internet] Baltimore (MD): CMS; cited 2011 Oct 17. Available from: https://www.cms.gov/DemoProjectsEvalRpts/downloads/ACEFactSheet.pdf. [Google Scholar]
- 7.Rastogi A, Mohr BA, Williams JO, Soobader M-J, de Brantes F. Prometheus payment model: application to hip and knee replacement surgery. Clin Orthop Relat Res. 2009;467(10):2587–97. doi: 10.1007/s11999-009-0942-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.De Brantes F, Rosenthal MB, Painter M. Building a bridge from fragmentation to accountability—the Prometheus Payment model. N Engl J Med. 2009;361(11):1033–6. doi: 10.1056/NEJMp0906121. [DOI] [PubMed] [Google Scholar]
- 9.Dummit LA. Medicare’s bundling pilot: including post-acute care services. Washington (DC): George Washington University; 2011. (National Health Policy Forum Issue Brief No. 841) [PubMed] [Google Scholar]
- 10.Gottlieb DJ, Zhou W, Song Y, Andrews KG, Skinner JS, Sutherland JM. Prices don’t drive regional Medicare spending variations. Health Aff (Millwood) 2010;29(3):537–43. doi: 10.1377/hlthaff.2009.0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dimick JB, Staiger DO, Birkmeyer JD. Ranking hospitals on surgical mortality: the importance of reliability adjustment. Health Serv Res. 2010;45(6 Pt 1):1614–29. doi: 10.1111/j.1475-6773.2010.01158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 13.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 14.Pham HH, Devers KJ, Kuo S, Berenson R. Health care market trends and the evolution of hospitalist use and roles. J Gen Intern Med. 2005;20(2):101–7. doi: 10.1111/j.1525-1497.2005.40184.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nathan H, Pawlik TM. Limitations of claims and registry data in surgical oncology research. Ann Surg Oncol. 2008;15(2):415–23. doi: 10.1245/s10434-007-9658-3. [DOI] [PubMed] [Google Scholar]
- 16.Birkmeyer JD, Gust C, Dimick JB, Birkmeyer NJ, Skinner J. Hospital quality and the cost of inpatient surgery in the United States. Ann Surg. doi: 10.1097/SLA.0b013e3182402c17. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]