Abstract
The development of tyrosine kinase inhibitors (TKIs) for the treatment of chronic myelogenous leukemia (CML) was based on the discovery that CML stem and progenitor cells overexpress the abnormal fusion protein kinase BCR-ABL. The prototype TKI, imatinib, selectively inhibits BCR-ABL, as well as several other kinases, including DDR, KIT, PDGFR, and CSF-1R. Although the management of CML improved dramatically with the introduction of imatinib, not all patients benefit from treatment because of resistance or intolerance. Consequently, research efforts have focused on developing more potent TKIs with the ability to circumvent imatinib resistance. Nilotinib, a second-generation oral TKI, was rationally designed based on the crystal structure of imatinib to be highly active against a wide range of imatinib-resistant BCR-ABL mutants and is approved for the treatment of newly diagnosed or imatinib-resistant or -intolerant CML, and has shown superiority over imatinib in first-line in newly diagnosed CML. Furthermore, the activity of nilotinib against KIT and PDGFRα has led to its evaluation in advanced gastrointestinal stromal tumors (GIST). The purpose of this review is to describe the development of nilotinib, providing a structural explanation for the differential activity of nilotinib and imatinib in GIST. Activity of nilotinib against KIT and PDGFR and emerging evidence of differences in cellular uptake between nilotinib and imatinib are discussed.
Keywords: Nilotinib, AMN107, fusion proteins, BCR-ABL, stem cell factor receptor, receptors, platelet-derived growth factor, gastrointestinal stromal tumors, drug resistance
INTRODUCTION
The design and development of tyrosine kinase inhibitors (TKIs) for the treatment of chronic myelogenous leukemia (CML) was driven by the knowledge that the protein kinase BCR-ABL, encoded by the BCR-ABL fusion oncogene, is constitutively activated in patients with this disease. This oncogene is present in 95% of patients with CML and is the result of a chromosomal aberration known as the Philadelphia chromosome (Ph), which arises from the accidental fusion of the BCR gene with the gene encoding for the intracellular non-receptor tyrosine kinase c-ABL.1 In normal cells, the activity of ABL1 is tightly controlled; in contrast, BCR-ABL fusion proteins have constitutive catalytic activity leading to cell transformation and ultimately uncontrolled cellular proliferation and reduced apoptosis.2,3 Based on this premise, BCR-ABL kinase represents a logical therapeutic target for the development of drugs to treat CML.
The small-molecule prototype TKI, imatinib mesylate (Glivec®, formerly known as STI-571, Novartis Pharma AG, Basel, Switzerland), selectively targets BCR-ABL and also the stem cell factor receptor (KIT), discoidin domain receptor (DDR), and platelet-derived growth factor receptor (PDGFR) tyrosine kinases.4 Imatinib was the first TKI to be licensed for the treatment of CML; however, despite its well-established efficacy in this setting,5 many patients fail on imatinib therapy due to the development of resistance or loss of response. Resistance to imatinib may be categorized as primary, manifesting as a lack of efficacy from the very start of therapy, or secondary (acquired resistance), defined as a lack of response in patients who initially responded to treatment.6 Point mutations within the kinase domain of BCR-ABL that reduce the binding affinity of imatinib to the protein are the most common cause of imatinib resistance. However, increased expression of BCR-ABL kinase through gene amplification, overexpression of the SRC family of kinases, and pharmacokinetic and pharmacodynamic factors also are understood to play a role in the development of resistance in some patients.6,7
Nilotinib (Tasigna®, formerly known as AMN107, Novartis Pharma AG, Basel, Switzerland) is a new oral TKI, rationally designed to overcome imatinib resistance in CML.8 In Phase I and II studies, nilotinib achieved good tolerability and durable responses in adult patients with Ph+ CML resistant or intolerant to at least one prior therapy, including imatinib.9,10 This subsequently resulted in the approval of nilotinib for the treatment of patients with newly diagnosed CML or imatinib-resistant/-intolerant patients with chronic or accelerated-phase CML.11–13 In addition to inhibiting BCR-ABL, nilotinib, similar to imatinib, also has potent activity against the DDR, KIT, PDGFR, and colony stimulating factor receptor-1 (CSF-1R) tyrosine kinases.8,14,15 Mutations in the genes encoding for these tyrosine kinases have been shown to play a key role in the pathogenesis of certain malignancies, including gastrointestinal stromal tumors (GIST), subtypes of melanoma, and pigmented villonodular synovitis (PVNS).16–18 In recent years, the introduction of TKI therapy, in the form of imatinib, has significantly improved the outcome of patients with GIST.19 Further progress continues to be made in the treatment of this malignancy, with the ongoing clinical evaluation of nilotinib and other TKIs in patients with advanced GIST in several different treatment settings.
CHEMICAL STRUCTURE OF NILOTINIB
A phenylamino-pyrimidine derivative, nilotinib was rationally designed based on the crystal structure of imatinib and an understanding of the molecular mechanism of imatinib activity in relation to inhibition of BCR-ABL kinase (Figure 1).20 Imatinib has a high affinity for ABL kinase. Like others, this kinase incorporates a highly conserved bi-lobed structure with an ATP binding domain situated in a deep cleft between the N- and C- terminal lobes. Adjacent to this is the centrally located activation loop that incorporates a conserved Asp-Phe-Gly (DFG) sequence and controls catalytic activity by switching between different states in a phosphorylation-dependent manner.3 Autophosphorylation of the activation loop is essential for BCR-ABL activity, as without it the activation loop is not properly positioned for catalysis and ATP binding is not feasible.21 Imatinib achieves BCR-ABL kinase inhibition by binding to the inactive, unphosphorylated conformation of the kinase (DFG-out), thereby reducing the availability of the catalytically active phosphorylated conformation (DFG-in), necessary for ATP binding. This blocks signal transduction, ultimately resulting in inhibition of proliferation and loss of viability and proliferation.3,21,22 As there is much greater structural heterogeneity between the inactive conformations of protein kinases in comparison to the highly conserved active conformations, drugs like imatinib have much greater target selectivity than those agents that bind to active conformations. Examination of spatial changes in the ABL kinase domain that allow imatinib to bind led researchers to hypothesize that the selectivity and potency of imatinib for BCR-ABL kinase could be improved upon by filling the imatinib binding site more efficiently by taking advantage of it’s lipophilicity. Based on this principle, nilotinib was designed to maintain binding to the inactive conformation of the ABL kinase domain, while incorporating alternative binding groups to the N-methylpiperazine moiety and preserving an amide pharmacophore to retain H-bond interactions with Glu286 and Asp381.20 Substitution of the N-methylpiperazine moiety present in imatinib by a phenyl group bearing trifluoromethyl and imidazole substituents in the nilotinib structure greatly contributes to the potency of nilotinib by reducing the requirement for hydrogen bonding with nilotinib (4 H-bond interactions compared with 6 H-bonds for imatinib). As described later in this review, these structural modifications provide nilotinib with greater affinity and inhibitory activity compared with imatinib against wild-type BCR-ABL kinase, while preserving activity against KIT and PDGFR kinases.8,20 In addition, the structural differences between nilotinib and imatinib are reflected in minimal cross-intolerance between the two drugs with respect to non-hematologic toxicities in patients with CML.14,23 Among patients with imatinib-resistant CML, nilotinib has not been associated with the toxic effects commonly seen with imatinib treatment, such as fluid retention, edema, and weight gain.9
Figure 1.
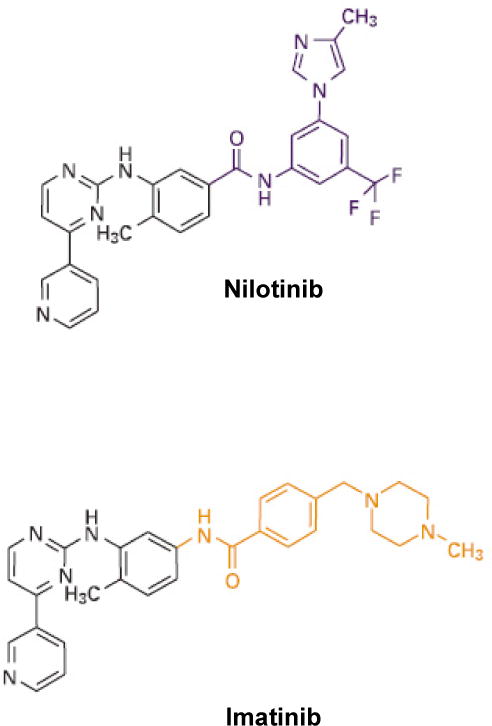
Molecular structures of nilotinib and imatinib20
Reprinted by permission from Macmillan Publishers Ltd: Cancer Cell Weisberg E, Manley PW, Breitenstein W et al. Characterization of AMN107, a selective inhibitor of native and mutant Bcr-Abl. 7:129–141, copyright 2005.
NILOTINIB: MECHANISM OF ACTION IN GIST
Because of its chemical structure, nilotinib has demonstrated anticancer activity in CML through its ability to selectively inhibit autophosphorylation of BCR-ABL. Small changes in the mode of binding to ABL enable nilotinib to inhibit cellular proliferation of imatinib-sensitive and -resistant CML cell lines more potently than imatinib.8,20,24,25 Additional preclinical work indicated that the anticancer activity of nilotinib in CML is antiproliferative rather than proapototic.26
Although nilotinib was not rationally designed specifically to treat GIST, its in vitro activity against kinases other than BCR-ABL, particularly KIT- and PDGFRα (both of which are known to be oncogenic in GIST) led to its evaluation in this setting. Specific oncogenic mutations within the KIT or PDGFRα receptor tyrosine kinase lead to constitutive phosphorylation and activation of the receptor resulting in uncontrolled cellular proliferation and the subsequent development of several human malignancies, including GIST. Four different regions of KIT are known to be mutated in GIST, and of these the juxtamembrane portion coded for by exon 11 is most often affected (~67% of GIST), followed by mutations in exon 9 (~10%), exon 13 (~1–2%), and exon 17 (~1%).27 Across all known mutation types, approximately 80% of GIST harbor mutations in KIT, while 5–8% have mutations in PDGFRA and 12–15% are wild-type.28
Activity against KIT and mutant cell lines
In vitro studies have shown nilotinib to be a potent inhibitor of several KIT mutant cell lines (Table 1). Nilotinib was as effective as imatinib at inhibiting the proliferation of exon 11 KITV560del and exon 13 KITK642E mutant cells20 and also potently inhibited the proliferation of exon 11 KITV560G mutant cells in vitro (IC50 108 nM).29 Activity against xenografts harboring KITV560G mutant-tumors has also been demonstrated in vivo.30 Against murine Ba/F3 cells expressing wild-type KIT, nilotinib also was a more potent inhibitor of cellular proliferation compared with other TKIs, achieving an IC50 of 35 nM compared with 245, 316, 910, and 3132 nM for the TKIs sunitinib, dasatinib, sorafenib, and imatinib, respectively.31
Table 1.
Activity of nilotinib and imatinib against kinases involved in the pathogenesis of GIST. IC50 values are presented as means.
| KIT mutation (cell lines) | Nilotinib IC50, nM | Imatinib IC50, nM | Reference |
|---|---|---|---|
| Exon 11 KITV560del (Ba/F3) | 26 | 27 | 20 |
| Exon 13 KITK462E (GIST882) | 160 | 120 | 20 |
| Exon 11 KITV560G (HMC-1560) | 108 | 74 | 55 |
| Exon 11/exon 13 KITV560del/V654A (Ba/F3) | 192 | 3927 | 33 |
| Exon 11/exon 17 KITV559D/D820Y (Ba/F3) | 297 | 3202 | 33 |
| PDGFRA + PDGFRB (A31) | 71a | 74a | 20 |
| PDGFRB (Tel Ba/F3) | 57 | 39 | 20 |
Data shown represent kinase autophosphorylation.
In addition to its activity against cell lines expressing single KIT mutations, nilotinib also has demonstrated in vitro activity against double mutations involving KIT exons 13 or 17, which confer resistance to imatinib. Approximately half of all patients with GIST who experience an initial response to imatinib therapy will develop imatinib resistance as a result of secondary mutations in the KIT kinase domain. These most commonly occur in exon 17, although single amino acid mutations in exons 13 and 14 also have been reported.32 Nilotinib was more effective than dasatinib and sorafenib in inhibiting the growth of imatinib-resistant cells carrying KIT double mutants involving exon 11 and exons 13 (KITV560del/V654A) or 17 (KITV559D/D820Y) mutations. For KITv560del/V654A mutations, an IC50 value of 192 nM was reported for nilotinib compared with 585 and 1074 nmol/L for dasatinib and sorafenib, respectively. Corresponding IC50 values for the KITV559D/D820Y mutation were 297, 432, and 944 nM, respectively.33 In contrast to imatinib, nilotinib also inhibited the proliferation of FDC-P1 cells expressing KITV560G/V564A mutations to a similar extent to wild-type KIT in autophosphorylation and cell proliferation assays, suggesting that nilotinib may be less susceptible to resistance arising from the V654A mutation that is frequently associated with imatinib resistance.29,34 By modifying the structure of the kinase domain, this missense mutation is thought to confer resistance by interfering with interactions between imatinib and the receptor.
Activity against PDGFRα and PDFRβ mutant cell lines
In studies of other receptor tyrosine kinases implicated in the oncogenesis of GIST, nilotinib achieved potent and selective inhibition of PDGFRα and PDGFRβ. As is the case with imatinib, nilotinib potently inhibited the autophosphorylation of A31 cells transformed by PDGFRA and PDGFRB double mutations (Table 1).20 Nilotinib also showed in vitro and ex vivo activity similar to imatinib against FIP1L1-PDGFRα,35 a fusion protein associated with the myeloproliferative syndrome hypereosinophilia (HES),36 as well as the D842V- and V561-PDGFRA-Ba/F3 mutant cell lines.37 Against EOL-1 cell lines with constitutive activation of FIP1L1-PDGFRα, nilotinib was as effective as imatinib at inhibiting proliferation (IC50 0.54 and 0.20 nM, respectively) and inducing apoptosis. Nilotinib and imatinib also were equipotent as inhibitors of PDGFRα phosphorylation in EOL-1 cells and primary cells from patients with HES.35 Furthermore, in Ba/F3 cells transformed by FIP1L1-PDGFRA,nilotinib inhibited cell proliferation (IC50 <25 nM) and phosphorylation of this fusion kinase and the downstream signaling target STAT5.38 Nilotinib also showed in vitro activity against Ba/F3 cells expressing FIP1L1-PDGFRα/T674I, a mutation that renders these cells resistant to imatinib.39 The possibility that the development of resistance to imatinib in patients with HES may parallel that in CML suggests that nilotinib may have a potential role in the treatment of CML and other myeloproliferative disorders. Additional antitumor effects have been observed against PDGFRB mutations in that nilotinib prolonged survival of mice with TEL-PDGFRB mutations in an in vivo model.38
CELLULAR UPTAKE OF NILOTINIB AND IMATINIB IN GIST CELL LINES
Cellular uptake mechanisms of imatinib and nilotinib appear to be different.40 Imatinib is transported intracellularly via an active transporter mechanism involving the organic cation transporter-1 (OCT-1) influx protein.40 Inhibition of OCT-1 results in significantly reduced intracellular uptake and retention (IUR) of imatinib at all concentrations (P<0.001) but does not significantly affect the IUR of nilotinib (P>0.05). This difference (OCT-1 transport) may contribute to the interpatient variability in drug blood levels observed with imatinib but not nilotinib. Moreover, because the majority of substrates transported by OCT proteins are cations, imatinib uptake also may be influenced by the degree of protonation of the basic N-methylpiperazine group at physiological pH, a group that is absent in nilotinib. The lack of identified active transport mechanisms for nilotinib intracellular concentration suggests that nilotinib transport is mostly passive. Because imatinib and nilotinib display similar potency in vitro, a more uniform cellular uptake via passive transport may result in an advantage for nilotinib over imatinib in diseases driven by KIT and PDGFR.41
Analysis of the cellular uptake of nilotinib and imatinib in GIST cell lines is suggestive of increased cellular uptake or decreased cellular efflux of nilotinib compared with imatinib. In an investigation involving two human GIST patient-derived cell lines, both of which expressed constitutively activated KIT, uptake of nilotinib was significantly higher than that of imatinib. Compared with imatinib, uptake of nilotinib was 7-fold higher in the imatinib-sensitive cell line GIST882 and 10-fold higher in the imatinib-resistant cell line GIST GDG1. Furthermore, combining the two compounds had no influence on the uptake of either agent in GIST882 cells, and uptake of imatinib was not influenced by co-administration with nilotinib in GIST GDG1 cells. However, the uptake of nilotinib was significantly increased when combined with imatinib 1 μM in GIST GDG1 cells (Figure 2).42 A more recent investigation also reported an increase in the IUR of nilotinib following co-administration with imatinib. Assays to measure IUR in five newly diagnosed patients with CML and two cell lines revealed an increase in the IUR of 14C-labelled nilotinib (1 and 2 μM) following administration of unlabelled imatinib; however, when the converse was performed (administration of 14C-labelled imatinib and unlabelled nilotinib), the IUR of imatinib was decreased in most patients.43 These findings have led to the suggestion that the increase in nilotinib intracellular uptake mediated by imatinib may be responsible for the synergy observed between the two drugs in BCR-ABL leukemic cell lines.44
Figure 2.
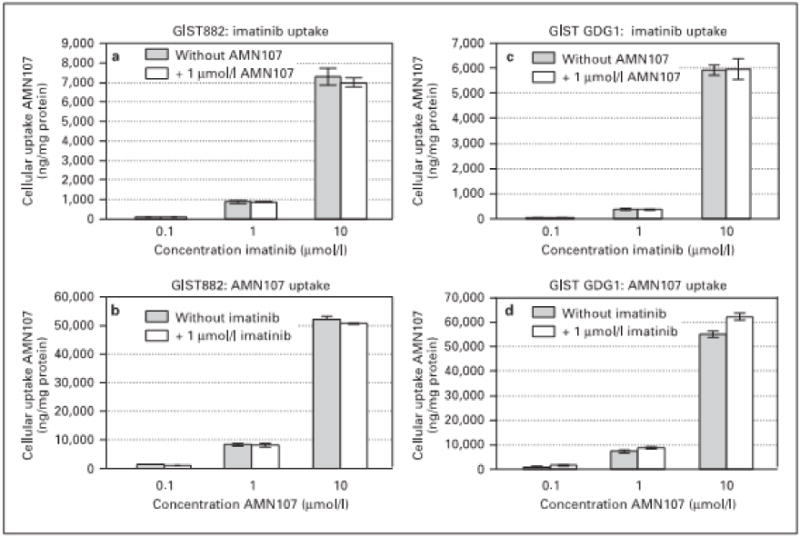
Intracellular uptake of nilotinib and imatinib in GIST882 cells and imatinib-resistant GIST GDG1 cells42
Reprinted by permission from S. Karger AG Basel: Prenen H, Guetens G, de Boeck G et al. Cellular uptake of the tyrosine kinase inhibitors imatinib and AMN107 in gastrointestinal stromal tumor cell lines. Pharmacology 2006;77:11–16
Based on the differential cellular uptake of nilotinib and imatinib, it has been suggested that nilotinib may be less susceptible to cellular transport-driven imatinib resistance.42 Available evidence indicates that multi-drug-resistant (MDR) P-glycoprotein (PGP) functions as a transporter of imatinib in transformed cell lines and that MDR1 expression acts to confer drug resistance.40,45–47 One of the consequences of transport-driven imatinib resistance in GIST cells and the resulting decrease in intracellular concentrations of imatinib may be a reduced likelihood of cellular apoptosis, leading to the generation of imatinib-resistant subclones. Decreased intracellular concentrations of imatinib also may potentiate the selection of cells harboring mutant copies of the BCR-ABL gene, making the tumor cell resistant to the compound.40 However, nilotinib does not appear to be a substrate of imatinib transport pumps, suggesting a stability in intracellular drug levels that may benefit patients with GIST, particularly those in whom imatinib resistance has developed.42
NILOTINIB MECHANISM OF ACTION IN PVNS
In addition to the BCR-ABL, KIT, and PDGFR kinases, nilotinib has also shown in vitro activity against CSF1R, albeit weaker than that of imatinib, which is strongly expressed in PVNS.14,18 This benign but painful neoplastic condition, also known as tenosynovial giant cell tumor (TGCT), affects the synovium in young and middle-aged adults with the potential for severe joint morbidity and results from a specific alteration that affects the CSF1 gene.18,48 Inhibition of CSF-1R with imatinib has been reported to produce tumor remission in patients with PVNS, suggesting that targeting this pathway can provide additional treatment options beyond surgery for this tumor type.49–51 Nilotinib is being investigated for this indication.
CONCLUSIONS
The unique binding characteristics of nilotinib—combined with the limitations of other available TKIs—have led to the investigation of nilotinib in GIST. Although the prototype TKI imatinib transformed the treatment of patients with GIST, the increasing incidence of acquired resistance to imatinib and, subsequently to sunitinib, in patients with this malignancy suggests that other therapeutic agents are needed.32,34 Sunitinib is commonly used as a second-line TKI following imatinib failure, but it typically provides only ~6 months of additional time to tumor progression and ~6 months of additional progression-free survival.52
Among the multiple mechanisms believed to contribute to imatinib resistance in GIST, secondary mutations in the KIT kinase domain, most commonly exon 17 and to a lesser extent exons 13 and 14, are known to make a significant contribution.32 Notably, nilotinib has demonstrated potent antiproliferative activity against cell lines harboring such KIT mutations, including KIT double mutants involving exon 11 and exons 13 or 17,33 and also against cells harboring the missense V654A mutation that is frequently associated with imatinib resistance.29,34 These findings, together with emerging evidence suggesting a reduced susceptibility of nilotinib to cellular transport-driven imatinib resistance, highlight the potential activity of nilotinib against KIT mutations responsible for clinical resistance in certain patients with GIST. Recently reported data with nilotinib in patients with GIST who had progressed on available approved methods of treating the disease show that it provides significant clinical benefit in this patient population.53,54 Moreover, the structural differences between nilotinib and imatinib suggest potential differences in safety as evidenced by the minimal cross-intolerance between the two drugs. Based on this premise, nilotinib was evaluated in the third-line setting, with assessment of these data indicating that it may have some clinical benefit in patients that have progressed on imaitinib and sunitinib (see article 3 of this series). Other trials are under way that are designed to leverage nilotinib’s unique biochemical properties compared with other TKIs in the treatment of patients in the first-line setting (ENEST g1) and as an alternative to dose escalation for patients progressing on imatinib 400 mg/d (LANGIST). These trials are described in the third article in this series. Taken together, nilotinib is a novel TKI that has potent activity against GIST cells and has been shown to provide clinical benefit in GIST patients who have limited treatment options.
Acknowledgments
Financial support for medical editorial assistance was provided by Novartis Pharmaceuticals. We thank Angelo Russo for his medical editorial assistance with this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Druker BJ, Tamura S, Buchdunger E, et al. Effects of a selective inhibitor of the Abl tyrosine kinase on the growth of Bcr-Abl positive cells. Nat Med. 1996;2:561–566. doi: 10.1038/nm0596-561. [DOI] [PubMed] [Google Scholar]
- 2.Hazlehurst LA, Bewry NN, Nair RR, Pinilla-Ibarz J. Signaling networks associated with BCR-ABL-dependent transformation. Cancer Control. 2009;16:100–107. doi: 10.1177/107327480901600202. [DOI] [PubMed] [Google Scholar]
- 3.Schindler T, Bornmann W, Pellicena P, et al. Structural mechanism for STI-571 inhibition of abelson tyrosine kinase. Science. 2000;289:1938–1942. doi: 10.1126/science.289.5486.1938. [DOI] [PubMed] [Google Scholar]
- 4.Buchdunger E, Cioffi CL, Law N, et al. Abl protein-tyrosine kinase inhibitor STI571 inhibits in vitro signal transduction mediated by c-kit and platelet-derived growth factor receptors. J Pharmacol Exp Ther. 2000;295:139–145. [PubMed] [Google Scholar]
- 5.NCCN. NCCN Clinical Practice Guidelines in Oncology. Chronic myelogenous leukemia v.2.2010. 2010 doi: 10.6004/jnccn.2009.0065. Available from: http://www.nccn.org/professionals/physician_gls/PDF/cml.pdf. Last accessed Jan 2010. [DOI] [PubMed]
- 6.Hochhaus A, La Rosee P. Imatinib therapy in chronic myelogenous leukemia: strategies to avoid and overcome resistance. Leukemia. 2004;18:1321–1331. doi: 10.1038/sj.leu.2403426. [DOI] [PubMed] [Google Scholar]
- 7.Quintas-Cardama A, Kantarjian HM, Cortes JE. Mechanisms of primary and secondary resistance to imatinib in chronic myeloid leukemia. Cancer Control. 2009;16:122–131. doi: 10.1177/107327480901600204. [DOI] [PubMed] [Google Scholar]
- 8.Weisberg E, Manley P, Mestan J, et al. AMN107 (nilotinib): a novel and selective inhibitor of BCR-ABL. Br J Cancer. 2006;94:1765–1769. doi: 10.1038/sj.bjc.6603170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kantarjian H, Giles F, Wunderle L, et al. Nilotinib in imatinib-resistant CML and Philadelphia chromosome-positive ALL. N Engl J Med. 2006;354:2542–2551. doi: 10.1056/NEJMoa055104. [DOI] [PubMed] [Google Scholar]
- 10.le Coutre P, Ottmann OG, Giles F, et al. Nilotinib (formerly AMN107), a highly selective BCR-ABL tyrosine kinase inhibitor, is active in patients with imatinib-resistant or -intolerant accelerated-phase chronic myelogenous leukemia. Blood. 2008;111:1834–1839. doi: 10.1182/blood-2007-04-083196. [DOI] [PubMed] [Google Scholar]
- 11.FDA 2007 nilotinib. National Cancer Institute. FDA Approval for nilotinib. 2007 Available from: http://www.cancer.gov/cancertopics/druginfo/fda-nilotinib. Last accessed: Jan 2010.
- 12.Saglio G, Kim DW, Issaragrisil S, et al. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med. 2010;362:2251–2259. doi: 10.1056/NEJMoa0912614. [DOI] [PubMed] [Google Scholar]
- 13.Tasigna SOPC. Tasigna (nilotinib) 200mg hard capsules. Novartis; 2010. Electronic Medicines Compendium Summary of Product Characteristics. Last updated 21 Sept 2009. Available from: http://emc.medicines.org.uk/medicine/20827/SPC/Tasigna+200+mg+hard+capsules/#INDICATIONS. Last accessed Jan 2010. [Google Scholar]
- 14.Manley PW, Stiefl N, Cowan-Jacob SW, et al. Structural resemblances and comparisons of the relative pharmacological properties of imatinib and nilotinib. Bioorg Med Chem. 2010;18:6977–6986. doi: 10.1016/j.bmc.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 15.Manley PW, Drueckes P, Fendrich G, et al. Extended kinase profile and properties of the protein kinase inhibitor nilotinib. Biochim Biophys Acta. 2010;1804:445–453. doi: 10.1016/j.bbapap.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Heinrich MC, Corless CL, Duensing A, et al. PDGFRA activating mutations in gastrointestinal stromal tumors. Science. 2003;299:708–710. doi: 10.1126/science.1079666. [DOI] [PubMed] [Google Scholar]
- 17.Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279:577–580. doi: 10.1126/science.279.5350.577. [DOI] [PubMed] [Google Scholar]
- 18.West RB, Rubin BP, Miller MA, et al. A landscape effect in tenosynovial giant-cell tumor from activation of CSF1 expression by a translocation in a minority of tumor cells. Proc Natl Acad Sci U S A. 2006;103:690–695. doi: 10.1073/pnas.0507321103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blanke CD, Rankin C, Demetri GD, et al. Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol. 2008;26:626–632. doi: 10.1200/JCO.2007.13.4452. [DOI] [PubMed] [Google Scholar]
- 20.Weisberg E, Manley PW, Breitenstein W, et al. Characterization of AMN107, a selective inhibitor of native and mutant Bcr-Abl. Cancer Cell. 2005;7:129–141. doi: 10.1016/j.ccr.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 21.Liu Y, Gray NS. Rational design of inhibitors that bind to inactive kinase conformations. Nat Chem Biol. 2006;2:358–364. doi: 10.1038/nchembio799. [DOI] [PubMed] [Google Scholar]
- 22.Nagar B, Bornmann WG, Pellicena P, et al. Crystal structures of the kinase domain of c-Abl in complex with the small molecule inhibitors PD173955 and imatinib (STI-571) Cancer Res. 2002;62:4236–4243. [PubMed] [Google Scholar]
- 23.Jabbour E HAlCPeal. Minimal cross-intolerance between nilotinib and imatinib in patients with imatinib-intolerant chronic myelogenous leukemia (CML) in chronic phase (CP) or accelerated phase (AP) J Clin Oncol. 2008;26 Abstract 7063. [Google Scholar]
- 24.Golemovic M, Verstovsek S, Giles F, et al. AMN107, a novel aminopyrimidine inhibitor of Bcr-Abl, has in vitro activity against imatinib-resistant chronic myeloid leukemia. Clin Cancer Res. 2005;11:4941–4947. doi: 10.1158/1078-0432.CCR-04-2601. [DOI] [PubMed] [Google Scholar]
- 25.O’Hare T, Walters DK, Stoffregen EP, et al. In vitro activity of Bcr-Abl inhibitors AMN107 and BMS-354825 against clinically relevant imatinib-resistant Abl kinase domain mutants. Cancer Res. 2005;65:4500–4505. doi: 10.1158/0008-5472.CAN-05-0259. [DOI] [PubMed] [Google Scholar]
- 26.Jorgensen HG, Allan EK, Jordanides NE, Mountford JC, Holyoake TL. Nilotinib exerts equipotent antiproliferative effects to imatinib and does not induce apoptosis in CD34+ CML cells. Blood. 2007;109:4016–4019. doi: 10.1182/blood-2006-11-057521. [DOI] [PubMed] [Google Scholar]
- 27.Dirnhofer S, Leyvraz S. Current standards and progress in understanding and treatment of GIST. Swiss Med Wkly. 2009;139:90–102. doi: 10.4414/smw.2009.12166. [DOI] [PubMed] [Google Scholar]
- 28.Corless CL, Heinrich MC. Molecular pathobiology of gastrointestinal stromal sarcomas. Annu Rev Pathol. 2008;3:557–586. doi: 10.1146/annurev.pathmechdis.3.121806.151538. [DOI] [PubMed] [Google Scholar]
- 29.Roberts KG, Odell AF, Byrnes EM, et al. Resistance to c-KIT kinase inhibitors conferred by V654A mutation. Mol Cancer Ther. 2007;6:1159–1166. doi: 10.1158/1535-7163.MCT-06-0641. [DOI] [PubMed] [Google Scholar]
- 30.Cullinane C, Natoli A, Hui Y, et al. Preclinical evaluation of nilotinib efficacy in an imatinib-resistant KIT-driven tumor model. Mol Cancer Ther. 2010;9:1461–1468. doi: 10.1158/1535-7163.MCT-09-1181. [DOI] [PubMed] [Google Scholar]
- 31.Agaram NP, Laquaglia MP, Ustun B, et al. Molecular characterization of pediatric gastrointestinal stromal tumors. Clin Cancer Res. 2008;14:3204–3215. doi: 10.1158/1078-0432.CCR-07-1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Antonescu CR, Besmer P, Guo T, et al. Acquired resistance to imatinib in gastrointestinal stromal tumor occurs through secondary gene mutation. Clin Cancer Res. 2005;11:4182–4190. doi: 10.1158/1078-0432.CCR-04-2245. [DOI] [PubMed] [Google Scholar]
- 33.Guo T, Agaram NP, Wong GC, et al. Sorafenib inhibits the imatinib-resistant KITT670I gatekeeper mutation in gastrointestinal stromal tumor. Clin Cancer Res. 2007;13:4874–4881. doi: 10.1158/1078-0432.CCR-07-0484. [DOI] [PubMed] [Google Scholar]
- 34.Chen LL, Trent JC, Wu EF, et al. A missense mutation in KIT kinase domain 1 correlates with imatinib resistance in gastrointestinal stromal tumors. Cancer Res. 2004;64:5913–5919. doi: 10.1158/0008-5472.CAN-04-0085. [DOI] [PubMed] [Google Scholar]
- 35.Verstovsek S, Giles FJ, Quintas-Cardama A, et al. Activity of AMN107, a novel aminopyrimidine tyrosine kinase inhibitor, against human FIP1L1-PDGFR-alpha-expressing cells. Leuk Res. 2006;30:1499–1505. doi: 10.1016/j.leukres.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 36.Cools J, DeAngelo DJ, Gotlib J, et al. A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome. N Engl J Med. 2003;348:1201–1214. doi: 10.1056/NEJMoa025217. [DOI] [PubMed] [Google Scholar]
- 37.Weisberg E, Wright RD, Jiang J, et al. Effects of PKC412, nilotinib, and imatinib against GIST-associated PDGFRA mutants with differential imatinib sensitivity. Gastroenterology. 2006;131:1734–1742. doi: 10.1053/j.gastro.2006.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stover EH, Chen J, Lee BH, et al. The small molecule tyrosine kinase inhibitor AMN107 inhibits TEL-PDGFRbeta and FIP1L1-PDGFRalpha in vitro and in vivo. Blood. 2005;106:3206–3213. doi: 10.1182/blood-2005-05-1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.von Bubnoff N, Gorantla SP, Thone S, Peschel C, Duyster J. The FIP1L1-PDGFRA T674I mutation can be inhibited by the tyrosine kinase inhibitor AMN107 (nilotinib) Blood. 2006;107:4970–4971. doi: 10.1182/blood-2006-01-0285. [DOI] [PubMed] [Google Scholar]
- 40.Thomas J, Wang L, Clark RE, Pirmohamed M. Active transport of imatinib into and out of cells: implications for drug resistance. Blood. 2004;104:3739–3745. doi: 10.1182/blood-2003-12-4276. [DOI] [PubMed] [Google Scholar]
- 41.White DL, Saunders VA, Dang P, et al. OCT-1-mediated influx is a key determinant of the intracellular uptake of imatinib but not nilotinib (AMN107): reduced OCT-1 activity is the cause of low in vitro sensitivity to imatinib. Blood. 2006;108:697–704. doi: 10.1182/blood-2005-11-4687. [DOI] [PubMed] [Google Scholar]
- 42.Prenen H, Guetens G, de Boeck G, et al. Cellular uptake of the tyrosine kinase inhibitors imatinib and AMN107 in gastrointestinal stromal tumor cell lines. Pharmacology. 2006;77:11–16. doi: 10.1159/000091943. [DOI] [PubMed] [Google Scholar]
- 43.White DL, Saunders VA, Quinn SR, Manley PW, Hughes TP. Imatinib increases the intracellular concentration of nilotinib, which may explain the observed synergy between these drugs. Blood. 2007;109:3609–3610. doi: 10.1182/blood-2006-11-058032. [DOI] [PubMed] [Google Scholar]
- 44.Weisberg E, Catley L, Wright RD, et al. Beneficial effects of combining nilotinib and imatinib in preclinical models of BCR-ABL+ leukemias. Blood. 2007;109:2112–2120. doi: 10.1182/blood-2006-06-026377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Burger H, van Tol H, Brok M, et al. Chronic imatinib mesylate exposure leads to reduced intracellular drug accumulation by induction of the ABCG2 (BCRP) and ABCB1 (MDR1) drug transport pumps. Cancer Biol Ther. 2005;4:747–752. doi: 10.4161/cbt.4.7.1826. [DOI] [PubMed] [Google Scholar]
- 46.Hamada A, Miyano H, Watanabe H, Saito H. Interaction of imatinib mesilate with human P-glycoprotein. J Pharmacol Exp Ther. 2003;307:824–828. doi: 10.1124/jpet.103.055574. [DOI] [PubMed] [Google Scholar]
- 47.Mahon FX, Belloc F, Lagarde V, et al. MDR1 gene overexpression confers resistance to imatinib mesylate in leukemia cell line models. Blood. 2003;101:2368–2373. doi: 10.1182/blood.V101.6.2368. [DOI] [PubMed] [Google Scholar]
- 48.Mendenhall WM, Mendenhall CM, Reith JD, et al. Pigmented villonodular synovitis. Am J Clin Oncol. 2006;29:548–550. doi: 10.1097/01.coc.0000239142.48188.f6. [DOI] [PubMed] [Google Scholar]
- 49.Blay JY, El Sayadi H, Thiesse P, Garret J, Ray-Coquard I. Complete response to imatinib in relapsing pigmented villonodular synovitis/tenosynovial giant cell tumor (PVNS/TGCT) Ann Oncol. 2008;19:821–822. doi: 10.1093/annonc/mdn033. [DOI] [PubMed] [Google Scholar]
- 50.Cassier PA, Blay JY. Imatinib mesylate for the treatment of gastrointestinal stromal tumor. Expert Rev Anticancer Ther. 2010;10:623–634. doi: 10.1586/era.10.33. [DOI] [PubMed] [Google Scholar]
- 51.Ravi V, Wang W, Araujo DM, et al. Imatinib in the treatment of tenosynovial giant-cell tumor and pigmented villonodular synovitis. J Clin Oncol. 2010;28 doi: 10.1097/CCO.0b013e328347e1e3. Abstract 10011. [DOI] [PubMed] [Google Scholar]
- 52.Demetri GD, van Oosterom AT, Garrett CR, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet. 2006;368:1329–1338. doi: 10.1016/S0140-6736(06)69446-4. [DOI] [PubMed] [Google Scholar]
- 53.Demetri GD, Casali PG, Blay JY, et al. A Phase I Study of Single-Agent Nilotinib or in Combination with Imatinib in Patients with Imatinib-Resistant Gastrointestinal Stromal Tumors. Clin Cancer Res. 2009;15:5910–5916. doi: 10.1158/1078-0432.CCR-09-0542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Montemurro M, Schoffski P, Reichardt P, et al. Nilotinib in the treatment of advanced gastrointestinal stromal tumours resistant to both imatinib and sunitinib. Eur J Cancer. 2009;45:2293–2297. doi: 10.1016/j.ejca.2009.04.030. [DOI] [PubMed] [Google Scholar]
- 55.Verstovsek S, Akin C, Manshouri T, et al. Effects of AMN107, a novel aminopyrimidine tyrosine kinase inhibitor, on human mast cells bearing wild-type or mutated codon 816 c-kit. Leuk Res. 2006;30:1365–1370. doi: 10.1016/j.leukres.2006.04.005. [DOI] [PubMed] [Google Scholar]


