Abstract
Purpose/Background:
A number of different balance assessment techniques are currently available and widely used. These include both subjective and objective assessments. The ability to provide quantitative measures of balance and posture is the benefit of objective tools, however these instruments are not generally utilized outside of research laboratory settings due to cost, complexity of operation, size, duration of assessment, and general practicality. The purpose of this pilot study was to assess the value and validity of using software developed to access the iPod and iPhone accelerometers output and translate that to the measurement of human balance.
Methods:
Thirty healthy college‐aged individuals (13 male, 17 female; age = 26.1 ± 8.5 years) volunteered. Participants performed a static Athlete's Single Leg Test protocol for 10 sec, on a Biodex Balance System SD while concurrently utilizing a mobile device with balance software. Anterior/posterior stability was recorded using both devices, described as the displacement in degrees from level, and was termed the “balance score.”
Results:
There were no significant differences between the two reported balance scores (p = 0.818. Mean balance score on the balance platform was 1.41 ± 0.90, as compared to 1.38 ± 0.72 using the mobile device.
Conclusions:
There is a need for a valid, convenient, and cost‐effective tool to objectively measure balance. Results of this study are promising, as balance score derived from the Smartphone accelerometers were consistent with balance scores obtained from a previously validated balance system. However, further investigation is necessary as this version of the mobile software only assessed balance in the anterior/posterior direction. Additionally, further testing is necessary on a healthy populations and as well as those with impairment of the motor control system.
Level of Evidence:
Level 2b (Observational study of validity)1
Keywords: Accelerometer, Single Leg Balance Test, Smartphone Application, Stability assessment
INTRODUCTION
Human balance is a general term used to describe the coordination of complex sensory, motor, and biomechanical processes for the purpose of maintaining one's center of mass (COM) with respect to their base of support (BOS).2,3 The ability to maintain balance, or postural stability, is an essential component in motor skills ranging from simply maintaining posture to performing complex voluntary movements.4,5,6 Improving balance has been shown to help with recovery from injury, injury prevention, and improved functional performance in both young and elderly individuals.4,7,8 As such, the ability to quickly and reliably assess balance for any population, in any clinical, recreational, or wellness setting is becoming increasingly important.
Multiple methods of assessing balance, both objective and subjective, have been developed. Subjective assessment methods vary widely in testing methodology. They generally include a set of testing and scoring procedures unique to the test chosen, and tend to be utilized in clinical settings. Here a test administrator utilizes their clinical knowledge and experience to evaluate the patient. The benefits of these balance tests are that they are easily administered and require little to no equipment. However, while many have been validated, they do not provide quantifiable data and rely on the skill and experience of the test administrator for scoring and interpretation.9
Objective methods of balance assessment include the use of force platforms, strain gauges, and accelerometers. The benefits of these devices are their ability to generate quantitative scores by which clinicians and researchers are able to track change over multiple tests. However, while these test methods have improved validity and reliability over subjective methods, with the exception of accelerometers, the equipment needed is generally large and difficult to transport.9 This makes equipment‐based balance assessments difficult to perform when outside of the clinical or laboratory environment. Accelerometers, on the other hand, are small, lightweight, and able to be attached to the subject. Additionally, they have been shown to be useful for assessing balance during both static and dynamic activities.10,11 However, despite their advantages over other objective measures, accelerometers are still primarily only used in laboratory settings, thus limiting widespread clinical use of this balance assessment method.9,12
As technology has advanced, there has been an increase in the prevalence of consumer electronics, which incorporate the use of multiple accelerometers. One such advancement can be found in the iPod and iPhone developed by Apple Inc. These systems incorporate Micro Electro‐Mechanical Systems (MEMS) nano‐accelerometers that measure the instantaneous acceleration of an object, compared to gravity at any given time, in a free‐fall reference frame. Measurements are accomplished using a moveable bar suspended on micro‐machined springs that quantify acceleration by the deflection of the bar as the device moves in reference to gravity.12 MEMS accelerometers typically incorporate three measurement axes that quantify acceleration independently, yet are housed in the same device. These accelerometers are termed tri‐axial or tri‐axis accelerometers.
The concept of a wireless accelerometer system for quantifying the attributes of gait and balance has been illustrated through the G‐link® Wireless Accelerometer Node and Apple iPod and iPhone.13,14,15,16,17,18 These devices have the capacity to store data samples, which can be conveyed wirelessly to a remote location for post‐processing. Several authors have indicated that the iPod and iPhone demonstrate the capacity to accurately acquire quantified balance parameters with a sufficient level of consistency.16,18,19 However, further studies are needed to continue to validate the accuracy and reliability of accelerometric mobile devices. Furthermore, there is a need to validate the accuracy and reliability of smart phone applications utilizing accelerometry.
The current study utilized the Biodex Balance System SD (Biodex Medical Systems, Shirley, NY, USA) and the SWAY Balance Mobile Application (SWAY Medical, Tulsa, OK, USA) installed on an Apple iPod Touch device (Apple Computer Inc., Cupertino, CA, USA). The Biodex system uses a circular platform that is free to move about the anterior‐posterior (AP) and medial‐lateral (ML) axes simultaneously, and measures the degree of tilt about each axis. The device then calculates the medial‐lateral stability index (MLSI), anterior‐posterior stability index (APSI), and the overall stability index (OSI) by means of strain gauges, which measure the change in pressure and force within the springs of the underside of the platform.20,21 The units representing the stability index are interpretations of the change in strain, determined by undisclosed calculations from Biodex Medical Systems, Inc. Conversely, the SWAY Balance Mobile Application, installed on the mobile device, accesses the output generated from the tri‐axial accelerometers to determine a balance (stability) score. The units representing the balance score are interpretations of the acceleration of deflection within the accelerometers, and are also determined by undisclosed calculations from SWAY Medical.
The purpose of this pilot study was to assess the value and validity of using software developed to access the iPod and iPhone accelerometers output and translate that to the measurement of human balance.
METHODS
Thirty healthy college‐aged individuals (13 male, 17 female; mean age = 26.1 + 8.5 yr) free from any pre‐existing condition that may have altered their ability to balance normally participated in this study. All testing procedures were approved by the Wichita State University Institutional Review Board for Research involving Human Subjects, and informed consent was obtained from all subjects prior to participation.
Subjects performed a single trial of the Athlete Single Leg Test protocol, requiring them stand on their non‐dominant foot for 10 seconds on a Balance System SD platform. Subject height and weight were recorded and foot placement on the platform was conducted following manufacturer recommendations. Postural sway was concurrently measured utilizing an Apple iPod Touch loaded with the SWAY Balance Mobile Application software. Subjects were instructed to hold the iPod in an upright position, and with the screen side of the device against the approximate mid‐point of their sternum. The Balance System SD and SWAY tests were initiated and terminated simultaneously in order to maintain synchronized recording. Upon completion of the test, the Anterior‐Posterior Stability Index (APSI) score generated by Biodex and anterior‐posterior postural sway data generated by the SWAY Balance Mobile Application were exported for analysis. Statistical analysis for this study were completed with the use of Statistical Packages for the Social Sciences (SPSS) version 17.0.
RESULTS
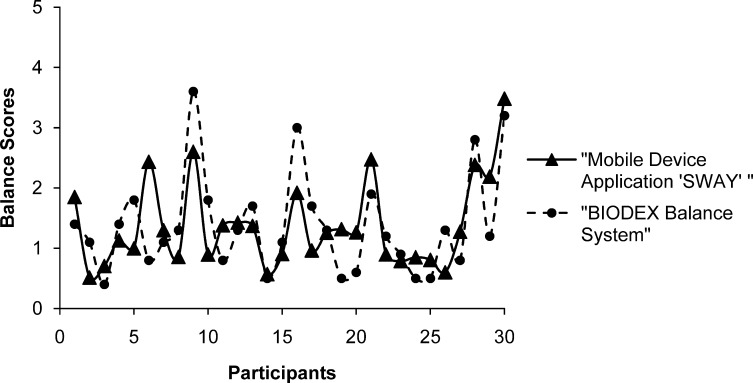
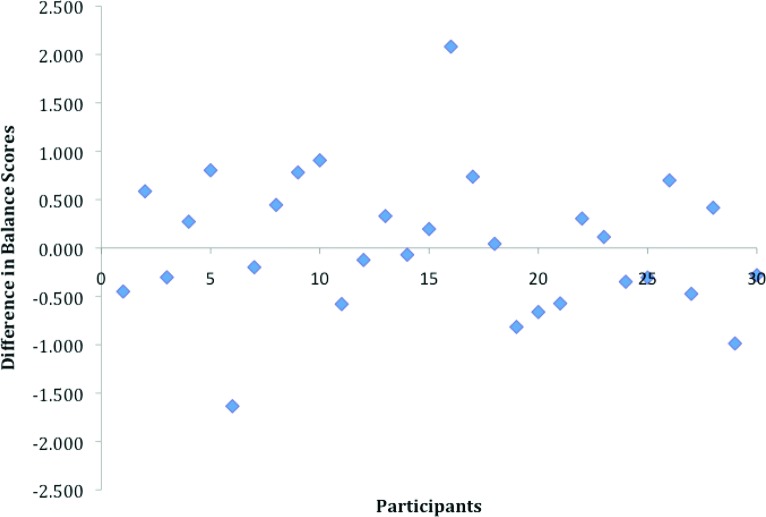
Data are summarized in Table 1. Preliminary data showed strong consistency in the SWAY Balance Mobile Application Software outcomes when compared to those from the BIODEX Balance System SD (Figure 1). APSI Scores on the balance platform were 1.41 + 0.90 compared to 1.38 + 0.72 using the SWAY Balance Smartphone Application. Paired samples t‐Test revealed no significant difference between the mean sway measures for the subjects when measured by each device (p = 0.818). A significant correlation between the two data sets was found with a mean difference (0.030 + 0.713) (p < 0.01, r = 0.632) (Figure 2).
Table 1.
Data Summary
| Age (years ± sd) | 26.1 ± 8.5 |
| Height (cm ± sd) | 170.1± 7.9 |
| Weight (kg ± sd) | 72.3 ± 15.5 |
| Biodex Balance System SD* (anterior/posterior score ± sd) | 1.41 ± 0.90 |
| SWAY Balance Mobile Application* (anterior/posterior score ± sd) | 1.38 ± 0.72 |
Biodex Balance System SD and SWAY use arbitrary units generally referred to as Balance Score
Figure 1.
Consistency in balance scores between Biodex Balance System SD and SWAY Balance Smartphone Application.
Figure 2.
The difference in measured balance scores between the Biodex Balance System SD and SWAY Balance Smartphone Application. The mean difference (0.030 + 0.713) showed a significant correlation between the two methods.
DISCUSSION
Balance assessment tools can be utilized to assess the neuromuscular effects of aging, identify neurological disorders, aid in the diagnosis of injury related to brain trauma, and identify functional deficits related to activities of daily living. Additionally, the implementation of a balance training program can aid in injury prevention, be used as a prescriptive rehabilitative tool in injury recovery, reduce the risk of falls in the aging, enhance functional or athletic performance, as well as provide a better overall understanding of the physiological systems contributing to postural movement and stability.5,6,22,23,24 Though balance training programs and assessments are being utilized for many conditions and populations, proper assessment and measures of balance must be determined in order to select the appropriate method of balance training. For implementation of balance training programs to be successful, assessment protocols must be reliable, valid, reproducible, and sensitive enough to measure minor changes. In a study that ran concurrently with this pilot study, the author's tested five iPod Touch devices in order to determine the sensitivity of the acceleration outputs.25 The results demonstrated low coefficients of variability, suggesting that sensitivity values in these devices are highly consistent. Appropriate software accessing these outputs would be capable of sensing small movements associated with postural stability. The purpose of this pilot study was to determine the consistency of a mobile device application that accesses data from the tri‐axial accelerometers within the iPod Touch for assessing human balance.
Preliminary results from this pilot study demonstrate that software used to access the tri‐axial accelerometers within the iPod/iPhone may be a useful method for assessing balance. However, this is a pilot study and is limited in scope. At the time this study was conducted the SWAY Balance Mobile Application was in its beta version and unavailable on the market. This version of the software accessed the iPod Touch accelerometers to only measure movement in the anterior/posterior plane. The reason for this was to determine if the consistency between the Biodex Balance System SD and the SWAY Balance Mobile Application measures were sufficiently acceptable to continue with the further development of the SWAY Balance assessment. Since the completion of this pilot study, the software has been updated to capture both anterior/posterior as well as medial/lateral movement. Subsequent studies are currently underway assessing the additional balance parameters that can be evaluated using this software update. Despite the limitations in the SWAY Balance software, the results of the current study showed consistency in output when compared to the Biodex Balance System SD. Further studies will determine the validity and reliability of the final version of the SWAY Balance Assessment. It is also worth noting that the study participants were a sample of convenience, all were undergraduate students of Exercise Science and familiar with methods of assessing human balance.
CONCLUSION
The information obtained from this pilot study can be of benefit to medical professionals, physical education coaches, parents, and the athletic community. There is an unmet need for a convenient, easy to use, cost‐effective tool to measure balance. A device meeting those criteria would be an important development in the task of identifying individuals with postural instability. Results from this initial pilot are promising. Balance measures, although with a small sample size, were consistent with measurements obtained using a previously validated system, demonstrating concurrent validity of the measurement using the SWAY application on a handheld device. However, recent updates in the SWAY application warrant further studies in order to assess its reproducibility, both in a healthy population and in a population with impairment of the motor control system.
REFERENCES
- 1.OCEBM Levels of Evidence Working Group. “The Oxford Levels of Evidence 2”. Oxford Centre for Evidence‐Based Medicine. http://www.cebm.net/index.aspx?o=5653
- 2.Pollock A. S. Durward B. R. Rowe P. J., et al. What is balance? Clin Rehabil. 2000;14:402‐406 [DOI] [PubMed] [Google Scholar]
- 3.Rose D. J. Balance, Posture, and Locomotion. In Spirduso W. W. Francis K. L. MacRae P. G. (Eds.), Physical Dimensions of Aging (2nd ed.). Champaign, IL: Human Kinetics, 2005: 131‐151 [Google Scholar]
- 4.Rogers M.E. N.L. Rogers N. Takeshima Balance training in older adults. Aging Health. 2005;1(3):475‐486 [Google Scholar]
- 5.Guskiewicz K. M. Perrin D. H. Research and clinical applications of assessing balance. J Sport Rehabil. 1996;5:45‐63 [Google Scholar]
- 6.Woollacott M. H. Shumway‐Cook A. Concepts and methods for assessing postural instability. J Aging Phys Activ. 1996;4:214‐233 [Google Scholar]
- 7.Davlin C. D. Dynamic balance in high level athletes. Percept Motor Skill. 2004;83(3,Pt2): 1171‐1176 [DOI] [PubMed] [Google Scholar]
- 8.Alexander N.B., Postural control in older adults. J Am Geriatr Soc. 1994;42(1):93‐108 [DOI] [PubMed] [Google Scholar]
- 9.Rogers M. E. Rogers N. L. Takeshima N., et al. Methods to assess and improve the physical parameters associated with fall risk in older adults. Prev Med. 2003;36:255‐264 [DOI] [PubMed] [Google Scholar]
- 10.Cho C. Y. Kamen G. Detecting balance deficits in frequent fallers using clinical and quantitative evaluation tools. J Am Geriatr Soc. 1998;46(4):426‐430 [DOI] [PubMed] [Google Scholar]
- 11.Yack H. J. Berger R. C. Dynamic stability in the elderly: Identifying a possible measure. J Gerontol. 1993;48(5):M225‐M230 [DOI] [PubMed] [Google Scholar]
- 12.Culhane K. M. O’Connor M. Lyons D., et al. Accelerometers in rehabilitation medicine for older adults. Age Ageing. 2005;34(6):556‐560 [DOI] [PubMed] [Google Scholar]
- 13.Lemoyne R. Coroian C. Mastroianni T. Grundfest W. Accelerometers for quantification of gait and movement disorders: A perspective review. J Mech Med Biol. 2008;8(2):137‐152 [Google Scholar]
- 14.LeMoyne R. Coroian C. Mastroianni T. Wireless accelerometer reflex quantification system characterizing response and latency. Presented at: Annual International Conference of the IEEE; Sept 3‐6, 2009; Minneapolis, MN [DOI] [PubMed] [Google Scholar]
- 15.Lemoyne R. Coroian C. Mastroianni T. Wireless accelerometer system for quantifying gait. Presented at: International Conference on Complex Medical Engineering; April 9‐11, 2009; Tempe, AZ [Google Scholar]
- 16.LeMoyne R., et al. Wireless accelerometer iPod application for acquiring quantified gait attributes. Presented at: 5th Frontiers in Biomedical Devices Conference and Exposition, New York, American Society of Mechanical Engineers; Sept 20‐21, 2010; Newport Beach, CA [Google Scholar]
- 17.Lemoyne R., et al. Implementation of an iPhone for characterizing Parkinson's disease tremor through a wireless accelerometer application. Presented at: 32nd Annual International Conference of the IEEE EMBS; Aug 31‐Sept 4, 2010; Buenos Aires, Argentina [DOI] [PubMed] [Google Scholar]
- 18.Lemoyne R. Mastroianni T. Grundfest W. Wireless accelerometer iPod application for quantifying gait characteristics. Presented at: 33rd Annual International Conference of the IEEE EMBS; Aug 30‐Sept 3, 2011; Boston, MA [DOI] [PubMed] [Google Scholar]
- 19.Lemoyne R. Mastroianni T. Coroian C., et al. Wireless three‐dimensional accelerometer reflex quantification device with artificial reflex system. J Mech Med Biol. 2010;10(3):401‐415 [Google Scholar]
- 20.Karimi N. Ebrahimi I. Kahrizi S., et al. Evaluation of postural balance using the biodex balance system in subjects with and without low back pain. Pak J Med Sci. 2008;24(3):372‐377 [Google Scholar]
- 21.Hinman M. R. Factors affecting reliability of the Biodex Balance System: A summary of four studies. J Sport Rehabil. 2000;9(3):240‐252 [Google Scholar]
- 22.Bell D.R. Guskiewicz K.M. Clark M.A., et al. Systematic review of the balance error scoring system. Sports Health. 2011;3(3): 287‐295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horak F. B. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Ageing. 2006;35(suppl 2):ii7‐ii11 [DOI] [PubMed] [Google Scholar]
- 24.Tyson S. F. How to measure balance in clinical practice. A systematic review of the psychometrics and clinical utility of measures of balance activity for neurological conditions. Clin Rehabil. 2009;23(9):824‐840 [DOI] [PubMed] [Google Scholar]
- 25.Amick R.Z. Patterson J.A. Jorgensen M.J. Sensitivity of Tri‐Axial Accelerometers within Mobile Consumer Electronic Devices: A Pilot Study. Int J Appl Sci Tech. 2013; 3(2):97‐100 [Google Scholar]