Abstract
Purpose/Background:
Female adolescents change their landing mechanics during puberty. It is unknown whether implementation of anterior cruciate ligament (ACL) injury prevention training reduces the loss of knee control in female athletes during puberty. The purpose of this study was to evaluate the effect of injury prevention training on dynamic knee alignment in female basketball players specifically when the knee mechanics were changing during puberty.
Methods:
Sixty female junior high school basketball players participated and were divided into two groups: a training group (n = 32) and a control group (n = 28). The training group underwent an injury prevention program for 6 months, whereas the control group maintained a regular training routine. The knee valgus motion and knee flexion range of motion during a drop vertical jump were measured before and after the training period. The probability of a high knee abduction moment (pKAM) was also evaluated using an ACL injury prediction algorithm.
Results:
The knee valgus motion was significantly increased in the control group (p < 0.001), whereas it did not change in the training group (p = 0.64). Similarly, the knee flexion range of motion was significantly decreased in the control group (p < 0.001), whereas it was not changed in the training group (p = 0.55). The pKAM was significantly increased in the control group (p < 0.001), but not in the training group (p = 0.06).
Conclusions:
Implementation of injury prevention training was effective in limiting the loss of knee control in female athletes during puberty. Lowering the risk of ACL injury might be possible in this population.
Level of Evidence:
2b
Keywords: Anterior cruciate ligament, adolescent, female, injury prevention, landing
INTRODUCTION
Anterior cruciate ligament (ACL) injuries are one of the most common injuries in sports, specifically basketball. Female athletes between the ages of 14 and 19 years are among those who have the highest incidence of ACL injury.1‐4 Injury to the ACL during this period is problematic because surgery in skeletally immature patients might cause growth disturbance. Also, surgery and rehabilitation prevent adolescents from participating in sports activities for a long period, affecting healthy physical development. In addition, regardless of management, the risk of developing osteoarthritis is significantly increased after an ACL injury.5‐7 This could potentially affect later quality of life as well.
One of the risk factors for developing ACL injuries is poor lower extremity kinematics. Levine et al found that a combination of anterior tibial shear force, knee abduction, and internal tibial rotation led to ACL failure.8 In addition, video analysis of actual injury situations revealed that the main mechanisms of ACL injury were increased knee valgus motion with internal tibial rotation.9,10 A reduced knee flexion angle was also commonly observed in injury situations.9,10 Female athletes with an increased knee valgus motion and reduced knee flexion angle during landing are at a high risk of developing ACL injury.11
Female adolescents increase knee valgus motion following the onset of the pubertal growth spurt.12‐14 Female athletes might also land with a reduced knee flexion angle after puberty as age increases.15 This phenomenon is probably the consequence of rapid physical development. In addition, female adolescents do not demonstrate sufficient neuromuscular adaptation to rapid skeletal growth like male adolescents.12 Since these changes in female adolescent movement patterns coincide with an increase in the number of ACL injuries, changes in landing mechanics might be a factor contributing to the increased incidence of ACL injuries in female athletes after the pubertal growth spurt.
Implementation of neuromuscular training strategies in children and adolescents to reduce the risk of developing ACL injuries has been recently encouraged.16 A meta‐analysis revealed that implementing injury prevention training in the mid‐teen years was more effective in reducing ACL injury than in the late teen or early adult period.17 This finding suggests that injury prevention training should be initiated in young athletes.
Although injury prevention training seems to be effective in reducing the number of ACL injuries in adolescents, there is a need to understand the underlying mechanisms of this phenomenon. There is a lack of knowledge regarding the relationship between the changes in knee mechanics that may be associated with pubertal growth and injury prevention training. Several studies have evaluated the effect of injury prevention training on dynamic knee alignment in adolescents.18‐20 However, it is still unknown whether injury prevention training is effective in limiting the movement pattern changes associated with pubertal growth in female adolescents.
To the best of the authors' knowledge, no studies have investigated the effect of injury prevention training on knee mechanics, specifically during puberty. Thus, the purpose of this study was to evaluate the effect of injury prevention training on dynamic knee alignment in female basketball players specifically when the knee mechanics were changing during puberty. The authors hypothesized that the implementation of an injury prevention training program in female basketball players during puberty could limit the loss of dynamic knee control.
METHODS
Subjects
Seventy‐one female basketball players from five local junior high school basketball teams were recruited to participate in this study. A power analysis was performed based on a pilot study. Thirty‐one subjects were needed in each group to achieve 80% power with alpha level of 0.05 (20% difference in pKAM means, pooled standard deviation of 30.8%, effect size of 0.65). All teams trained 6 days/week and had similar skill level. Subjects participated in the study during the first 6 months of a 12‐month season. Subjects were excluded from the study if they had a history of ACL injury, a lower extremity injury within 6 weeks that prevented full participation in basketball, any medical or neurological pathology, or previously participated in an injury prevention program. Maturational stage was evaluated using the self‐administered rating scale for pubertal development.21 Subjects were categorized into five maturational stages: pre‐pubertal, early pubertal, middle pubertal, late pubertal, and post‐pubertal. To evaluate pubertal subjects, females who were categorized at a pre‐ or post‐pubertal stage were excluded from the study. There were 2 pre‐pubertal and 4 post‐pubertal subjects. A total of 65 subjects participated in the study. Two teams (n = 36; age, 13.1 ± 0.8 years) that were able to participate in the injury prevention training were assigned to the training group. The other three teams (n = 29; age, 13.1 ± 0.8 years) were assigned to the control group. A total of 60 subjects (training group: n=32; control group: n=28) completed the study and were analyzed. Four subjects from the training group and one subject from the control group were unable to participate in the post‐training testing session for personal reasons.
Injury prevention training
An injury prevention training program (Table 1) was developed based upon previous literature.22‐25 The program was modified considering basketball specific skills. The focus of this program was to ensure proper movement patterns, particularly avoiding knee valgus motion and encouraging knee flexion during landing and cutting. The program was 20 minutes long and was implemented as a warm‐up routine. The training group performed the program three times per week for 6 months. A six‐month training period was selected to observe the changes associated with growth. The initial training session was conducted by a physical therapist. To ensure that the exercises were correctly performed and to help advance, the therapist followed up with the subjects every two weeks. The coach was also trained on how to instruct athletes on each skill at the initial training session. The coach led the training during the two weeks between therapist follow‐ups. The control group performed their regular training routine for six months. Both groups did not perform any additional training or conditioning which may have had an influence on their landing performance.
Table 1.
Injury prevention training program.
| Exercise | Instruction | Repetitions |
|---|---|---|
| Two‐legged squat | Keep the feet, knees, and hips in a straight line. Do not let the knees fall inward. Bend the knees and hips. | 2 × 10 reps |
| One‐legged squat | Keep the feet, knees, and hips in a straight line. Do not let the knees fall inward. Bend the knees and hips. Keep the pelvis level. | 10 reps/side |
| Squat jumps | Drop into a squat position and perform a maximal vertical jump. Upon landing, return to the starting position and repeat. Keep the feet, knees, and hips in a straight line. Make a soft landing. | 10 reps |
| Tuck jumps | Leap up in the air, tucking the knees into the chest. Land softly and immediately explode back up. Keep the feet, knees, and hips in a straight line. | 10 reps |
| 180° jumps | Jump into the air and rotate 180°. Land softly, keeping the feet, knees, and hips in a straight line. Bend the knees and hips. | 10 reps/side |
| Contact jumps | Jump towards a partner to make a shoulder‐to‐shoulder contact. Land softly, keeping the feet, knees, and hips in a straight line. Bend the knees and hips. | 10 reps/side |
| Lateral hops | Stand on one leg and jump to the side. Land softly on the other foot, keeping the feet, knees, and hips in a straight line. Bend the knees and hips. Keep the pelvis level. | 10 reps/side |
| Pivoting | Stand on the balls of the feet with the knees bent. Turn on the balls of the feet approximately 45° to the right and left. Keep the feet and knees pointing in the same direction. | 20 reps/side |
Planting and cutting
|
|
10 reps/side |
Data collection
Pre‐training data were collected prior to the initial training session and post‐training data were obtained after the 6‐month training period in all subjects. An ACL injury prediction algorithm developed by Myer et al. was used to evaluate knee mechanics and ACL injury risk.26‐28 This algorithm was reported to have high sensitivity and specificity and was able to identify female athletes who demonstrate a high knee abduction moment that increases the risk of ACL injury.26‐28
Height, weight, and tibia length were measured. Tibia length was measured as the distance between the lateral knee joint line and prominence of the lateral malleolus with the subjects standing with their knees extended. The quadriceps: hamstrings (QH) strength ratio was obtained using surrogate calculations by multiplying the female athlete's body mass by 0.01 and adding the resultant value to 1.10.28
Two‐dimensional lower extremity kinematics measurements were conducted. Eight bilateral markers were placed on each subject in the following locations: the greater trochanter, lateral knee joint line, patella, and lateral malleolus. Frontal and sagittal plane images were simultaneously captured with three video cameras (30 Hz; CASIO EXILIM, Japan). A basketball goal was used as an overhead target. The subjects performed a drop vertical jump (DVJ) as described previously.28 The subjects stood on a box (31 cm high) with their feet positioned 35 cm apart. The subjects were instructed to drop off the box and immediately perform a maximum vertical jump, raising both arms towards the target. Prior to testing, the subjects were allowed to perform one to three practice trials to familiarize themselves with the test maneuver. Once the subjects were able to perform the test maneuver, each subject performed three DVJ trials. No feedback was provided between the trials.
Data analysis
Frontal and sagittal images of the first DVJ landing were analyzed. The video files were first de‐interlaced using VirtualDub software (Avery Lee). Then the data were imported into ImageJ software (National Institute of Health, USA) to measure the knee valgus motion and knee flexion range of motion. The knee valgus motion was defined as the displacement between the patellar markers at the frame prior to initial contact and at the frame with a maximum medial position on the analyzing leg, and was calculated using the frontal view. The displacement measurements were calibrated using a known distance. The knee flexion angle was measured in the sagittal view with the angle made by the greater trochanter, lateral knee joint line, and lateral malleolus. The knee flexion range of motion was defined as the difference in the knee flexion angles at the frame prior to initial contact and maximum knee flexion. Using the tibia length, body mass, QH ratio, knee valgus motion, and knee flexion range of motion, the ACL injury prediction algorithm was used to obtain the probability of a high knee abduction moment (pKAM). Only the left leg was analyzed since previous literatures found that female athletes were more likely to tear their left ACL than the right.29‐31 Based on these studies, left leg was analyzed to limit data from bilateral subjects with assumed normal growth and risk in both legs.
Statistical Analysis
The mean and standard deviation of the knee valgus motion, knee flexion range of motion, and pKAM were calculated for each group. A 2 × 2 (group × time) analysis of variance with a mixed model design was conducted for each dependent variable. When there were significant interaction effects, a post hoc test was performed using a Bonferroni correction. The alpha level was set at 0.05. SPSS Ver. 21 (SPSS Inc. Chicago IL, USA) was used to perform the statistical analysis.
RESULTS
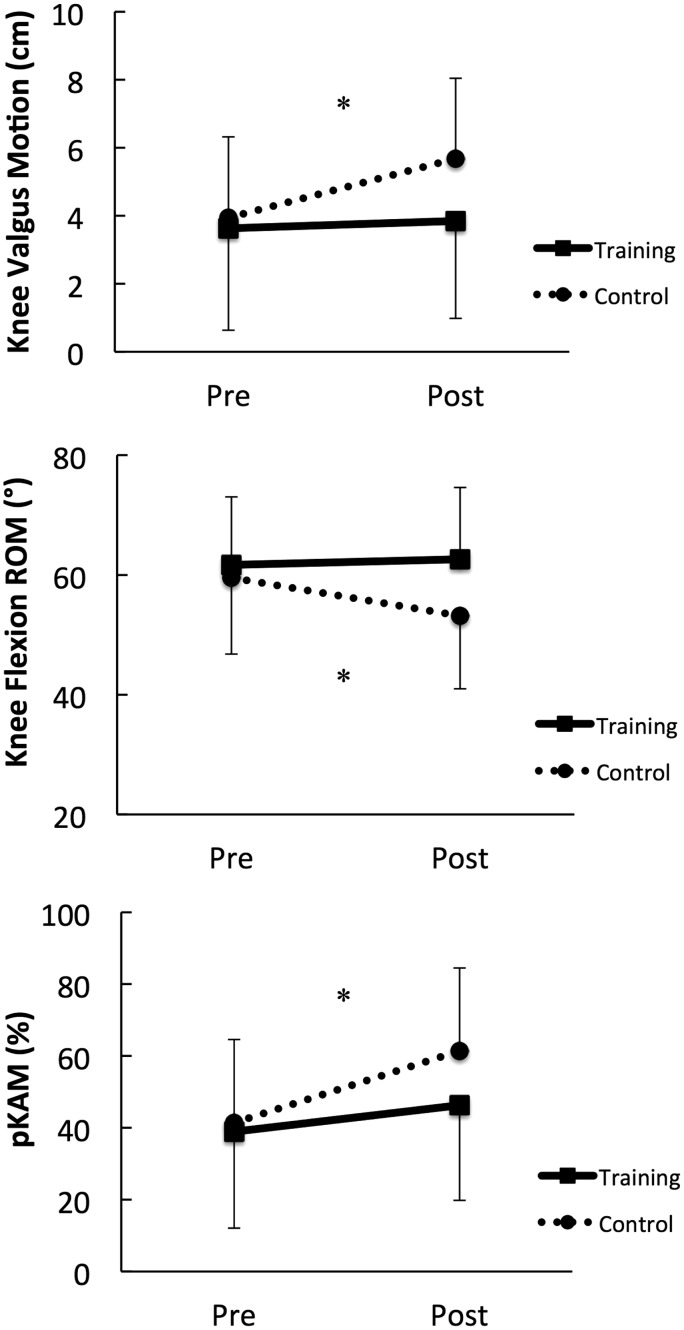
There were no statistically significant differences in the number of subjects in each stage between the training and control groups (p=0.09) (Table 2). No statistically significant differences were found between the training and control groups for age, height, or body mass at the two testing sessions (Table 3). Data for the knee valgus motion and knee flexion range of motion are summarized in Table 4. A significant group × time interaction was found for the knee valgus motion (p = 0.01), knee flexion range of motion (p = 0.01), and pKAM (p=0.02) (Figure 1). Post hoc analysis revealed that the knee valgus motion was significantly increased in the control group (p < 0.001), whereas it did not change in the training group (p = 0.64) (Table 4). Similarly, the knee flexion range of motion was significantly decreased in the control group (p < 0.001); however, it did not change in the training group (p = 0.55) (Table 4). The pKAM was significantly increased in the control group (p < 0.001), but not in the training group (p = 0.06) (Table 4).
Table 2.
Number of subjects in each pubertal stage.
| Training |
Control |
|||||
|---|---|---|---|---|---|---|
| Early pubertal | Middle pubertal | Late pubertal | Early pubertal | Middle pubertal | Late pubertal | |
| Number of subjects | 2 | 5 | 25 | 3 | 9 | 16 |
Note: Early‐pubertal stage is equivalent to Tanner stage 2, middle‐pubertal stage is equivalent to Tanner stage 3, late‐pubertal stage is equivalent to Tanner stage 4.
Table 3.
Subject demographics. Data are shown as mean ± SD. Training group: n = 32, control group: n = 28.
| Pretest |
Posttest |
|||
|---|---|---|---|---|
| Training | Control | Training | Control | |
| Age (years) | 13.1 ± 0.8 | 13.1 ± 0.8 | ||
| Height (cm) | 156.1 ± 6.8 | 157.0 ± 7.9 | 157.7 ± 6.7 | 158.0 ± 7.7 |
| Weight (kg) | 47.0 ± 7.0 | 46.7 ± 8.7 | 50.5 ± 6.5 | 49.4 ± 9.1 |
Table 4.
Changes in the knee valgus motion, knee flexion range of motion, and probability of a high knee abduction moment (pKAM). Data are shown as mean ± SD.
| Pretest | Posttest | Difference | P Value | 95% CI |
|||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Knee valgus motion (cm) | Training | 3.63 ± 2.38 | 3.85 ± 2.36 | 0.22 | 0.64 | −0.73 | 1.16 |
| Control | 3.94 ± 3.00 | 5.68 ± 2.87 | 1.74 | <0.001 | 1.06 | 2.43 | |
| Knee flexion ROM (°) | Training | 61.67 ± 11.37 | 62.63 ± 11.98 | 0.96 | 0.55 | −2.3 | 4.22 |
| Control | 59.52 ± 12.74 | 53.15 ± 12.17 | −6.37 | <0.001 | −9.22 | −3.52 | |
| pKAM (%) | Training | 38.91 ± 23.19 | 46.28 ± 23.10 | 7.36 | 0.06 | −0.21 | 14.96 |
| Control | 41.36 ± 26.83 | 61.43 ± 26.51 | 20.07 | <0.001 | 12.81 | 27.33 | |
Figure 1.
The pretest and posttest knee valgus motion, knee flexion range of motion, and pKAM in the training and control groups. *Significant difference between pretest and posttest (p < 0.001).
DISCUSSION
The incidence of ACL injury increases after puberty in female athletes.4 Recent authors have suggested that the biomechanical changes associated with pubertal growth may contribute to the increased occurrence of ACL injury after puberty.12‐15 Injury prevention strategies that minimize these biomechanical changes during puberty are necessary.
The results of this study support the hypothesis that the implementation of injury prevention training is effective in limiting the loss of dynamic knee control in female basketball players during puberty. Although injury prevention training was able to limit the changes in knee mechanics, no improvement was observed. Previous studies evaluating high school female athletes found that injury prevention training improved knee mechanics in both the frontal and sagittal planes.18‐20 Although the methods of evaluating knee mechanics were different, it seems that the injury prevention training was not as effective in pubertal girls compared with post‐pubertal girls. This may be due to the changes in landing mechanics that pubertal girls naturally develop during this period. A rapid increase in height and weight might increase torque at the knee joint.32 In addition, the width of the pelvis increases in girls during puberty. An increase in pelvic width might bring the hips to a more adducted position and therefore affect dynamic knee alignment.33 Moreover, it has been reported that female adolescents do not have a significant neuromuscular development during puberty compared with male adolescents.12 With a combination of structural and neuromuscular changes, pubertal girls demonstrate changes in landing mechanics. Implementation of injury prevention training could potentially enhance the neuromuscular system in female adolescents. Although a significant improvement might not be possible, limiting the changes in knee mechanics during this period might be a starting point to prevent ACL injury. In some athletes, this might be enough to reduce the risk of ACL injury, while in those who are at very high risk further training would need to be done. The effect sizes of the difference between the two groups in the knee valgus motion, knee flexion range of motion, and pKAM were Cohen's d = 0.70, 0.79, and 0.61, respectively. With these medium to large effect sizes, the authors believe that the posttest differences between the two groups were clinically important.
The pKAM in the training group was increased following the training period, although it was not statistically significant. This may be due to the physical growth factors, as the algorithm includes the body weight and tibia length. During the 6‐month period, the height and weight of the training group subjects increased by 1.6 cm and 3.5 kg, respectively. Similarly, the control group subjects gained 1.1 cm in height and 2.7 kg in weight. These physical growth factors might have played a role when evaluating ACL injury risk in female adolescents.
One of the limitations of this study was that the knee kinematics was evaluated using two‐dimensional measurements. Although a good correlation between two‐dimensional and three‐dimensional analysis has been reported in the previous studies,26,27 two‐dimensional measures might not represent the complex 3 dimensional movements that occur about the knee during athletics. In addition, the use of the pKAM might not be as accurate as the laboratory‐based assessment to evaluate the risk of ACL injury. However, the use of this assessment tool is less costly and easier to apply; thus, it is more clinically relevant. Another limitation was that the subjects in this study were junior high school students with an age between 12 and 14 years. This age group might not be representative of all of the stages of puberty, as many of the subjects were categorized in the middle or late pubertal stages. In addition, in this study, randomization during group allocation and blinding of the examiner were not achieved. This may have produced unintentional biases. Also, the generalizability of the results of the present study was limited due to the use of a convenience sample. Additional factors such as ethnicity or position played were not considered. Since these factors could affect landing mechanics, they may have influenced the results of this study.
Future studies should focus on evaluation of factors that contribute to the changes in landing mechanics in girls during puberty such as body composition, strength, and neuromuscular control. Further understanding of these factors would help identify what should be addressed in the injury prevention programs for maturing female athletes. In addition, a long‐term follow‐up and investigations of ACL injury rates after injury prevention training for pubertal females are necessary.
CONCLUSION
Implementation of an injury prevention training program was effective in limiting the increase in knee valgus motion and decrease in the knee flexion range of motion during landing in female basketball players during puberty. Although a significant improvement in the landing technique was not observed, affecting the factors that contribute to the risk of ACL injury might be possible in this population.
Acknowledgements
The authors would like to acknowledge the participants, parents/ guardians, and coaches who volunteered for this study.
REFERENCES
- 1.Shea KG Grimm NL Ewing CK, et al. Youth sports anterior cruciate ligament and knee injury epidemiology: who is getting injured? In what sports? When? Clin Sports Med. 2011;30:691–706 [DOI] [PubMed] [Google Scholar]
- 2.Powell JW Barber‐Foss KD Sex‐related injury patterns among selected high school sports. J Sports Med. 2000;28:385–391 [DOI] [PubMed] [Google Scholar]
- 3.Louw QA Manilall J Grimmer KA, et al. Epidemiology of knee injuries among adolescents: a systematic review. Br J Sports Med. 2008;42:2–10 [DOI] [PubMed] [Google Scholar]
- 4.Renstrom P Ljungqvist A Arendt E, et al. Non‐XEcontact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med. 2008;42:394–412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lohmander LS Englund PM Dahl LL, et al. The long‐term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–1769 [DOI] [PubMed] [Google Scholar]
- 6.Myklebust G Holm I Maehlum S, et al. Clinical, functional, and radiologic outcome in team handball players 6 to 11 years after anterior cruciate ligament injury: a follow‐up study. Am J Sports Med. 2003;31:981–989 [DOI] [PubMed] [Google Scholar]
- 7.Caine DJ Golightly YM Osteoarthritis as an outcome of paediatric sport: an epidemiological perspective. Br J Sports Med. 2011;45:298–303 [DOI] [PubMed] [Google Scholar]
- 8.Levine JW Kiapour AM Quatman CE, et al. Clinically relevant injury patterns after an anterior cruciate ligament injury provide insight into injury mechanisms. Am J Sports Med. 2013;41:385–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krosshaug T Nakamae A Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35:359–367 [DOI] [PubMed] [Google Scholar]
- 10.Koga H Nakamae A Shima Y, et al. Mechanisms for noncontact anterior cruciate ligament injuries: Knee joint kinematics in 10 injury situations from female team handball and basketball. Am J sports Med. 2010;38:2218–2225 [DOI] [PubMed] [Google Scholar]
- 11.Hewett TE Myer GD Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am J Sports Med. 2005;33:492–501 [DOI] [PubMed] [Google Scholar]
- 12.Hewett TE Myer GD Ford KR Decrease in neuromuscular control about the knee with maturation in female athletes. JBJS. 2004;86‐A:1601–1608 [DOI] [PubMed] [Google Scholar]
- 13.Schmitz RJ Shultz SJ Nguyen A Dynamic valgus alignment and functional strength in males and females during maturation. J Athl Train. 2009;44:26–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ford KR Shapiro R Myer GD, et al. Longitudinal sex differences during landing in knee abduction in young athletes. Med Sci Sports Exerc. 2010;42:1923–1931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu B McClure SB Onate JA, et al. Age and gender effects on lower extremity kinematics of youth soccer players in a stop‐jump task. Am J Sports Med. 2005;33:1356–1364 [DOI] [PubMed] [Google Scholar]
- 16.Myer GD Faigenbaum AD Ford KR, et al. When to initiate integrative neuromuscular training to reduce sports‐related injuries in youth? Curr Sports Med Rep. 2011;10:155–166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Myer GD Sugimoto D Thomas S, et al. The influence of age on the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: A meta‐analysis. Am J Sports Med. 2012;41:203–215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Myer GD Ford KR McLean SG, et al. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34:445–455 [DOI] [PubMed] [Google Scholar]
- 19.Lim B Lee YS Kim JG, et al. Effects of sports injury prevention training on the biomechanical risk factors of anterior cruciate ligament injury in high school female basketball players. Am J Sports Med. 2009;37:1728–1734 [DOI] [PubMed] [Google Scholar]
- 20.Pollard CD Sigward SM Ota S, et al. The influence of in‐season injury prevention training on lower‐extremity kinematics during landing in female soccer players. Clin J Sports Med. 2006;16:223–227 [DOI] [PubMed] [Google Scholar]
- 21.Carskadon MA Acebo C A self‐administrated rating scale for pubertal development. J Adolescent Health. 1993;14:190–195 [DOI] [PubMed] [Google Scholar]
- 22.Mandelbaum BR Silvers HJ Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes. 2‐year follow‐up. Am J Sports Med. 2005;33:1003–1010 [DOI] [PubMed] [Google Scholar]
- 23.Olsen OE Myklebust G Engebretsen L et al. Exercises to prevent lower limb injuries in youth sports: cluster randomized controlled trial. BMJ. 2005;330:449–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pfeiffer RP Shea KG Roberts D, et al. Lack of effect of a knee ligament injury prevention program on the incidence of noncontact anterior cruciate ligament injuries. J Bone Joint Surg. 2006;88‐A:1769–1774 [DOI] [PubMed] [Google Scholar]
- 25.Hewett TE Lindenfeld TN Riccobene JV, et al. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27:699–706 [DOI] [PubMed] [Google Scholar]
- 26.Myer GD Ford KR Khoury J, et al. Clinical correlates to laboratory measures for use in non‐contact anterior cruciate ligament injury risk prediction algorithm. Clin Biomech. 2010;25:693–699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Myer GD Ford KR Khoury J, et al. Development and validation of a clinic‐based prediction tool to identify female athletes at high risk for anterior cruciate ligament injury. Am J Sports Med. 2010;38:2025–2033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Myer GD Ford KR Hewett TE, et al. New method to identify athletes at high risk of ACL injury using clinic‐based measurements and freeware computer analysis. Br J Sports Med. 2011;45:238–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Negrete RJ Schick EA Cooper JP Lower‐limb dominance as a possible etiologic factor in noncontact anterior cruciate ligament tears. J Strength Cond Res. 2007;21:270‐273 [DOI] [PubMed] [Google Scholar]
- 30.Brophy R Silvers HJ Gonzales T Mandelbaum BR Gender influences: the role of leg dominance in ACL injury among soccer players. Br J Sports Med. 2010;44:694‐697 [DOI] [PubMed] [Google Scholar]
- 31.Ruedl G Webhofer M Helle K, et al. Leg dominance is a risk factor for noncontact anterior cruciate ligament injuries in female recreational skiers. Am J Sports Med. 2012;40:1269‐1273 [DOI] [PubMed] [Google Scholar]
- 32.Quatman CE Ford KR Myer GD, et al. Maturation leads to gender differences in landing force and vertical jump performance. A longitudinal study. Am J Sports Med. 2006;34:806–813 [DOI] [PubMed] [Google Scholar]
- 33.Pantano KJ White SC Gilchrist LA, et al. Difference in peak knee valgus between individuals with high and low Q‐angles during a single limb squat. Clin Biomech. 2005;20:966–972 [DOI] [PubMed] [Google Scholar]