Abstract
Purpose/Background:
It is not clear whether the addition of hip strengthening exercises will improve outcomes during the early stages of ACL rehabilitation. The purpose of this study was to determine the effects of the addition of isolated hip strengthening exercises to traditional rehabilitation on early outcomes (within the first 3 months) after ACL reconstruction (ACLR).
Methods:
A total of 43 subjects (18.8±6.9, 21 females, 22 males) who were in the process of rehabilitation following ACLR participated. Subjects were randomly assigned to one of two different treatment groups (1= traditional rehabilitation [NoHip], 2= traditional plus isolated hip strengthening rehabilitation [Hip]). Assessment included the International Knee Documentation Committee (IKDC) Subjective Knee Form, Visual Analog Scale (VAS) for pain during activities of daily living, and knee extension range of motion (ROM) side to side difference taken at weeks 1, 4, 8, and 12. In addition, dynamic balance was assessed with the Y Balance Test™ at 8 and 12 weeks. A mixed model repeated measures ANOVA was performed for IKDC, VAS, and ROM. A one‐way ANOVA was used to assess mean group differences for Y Balance Test – Lower Quarter (YBT‐LQ) side to side difference scores at 8 and 12 weeks.
Results:
There was no significant interaction for group by time across VAS (p = .463), IKDC (p = .819), or ROM (p = .513) side to side differences A significant difference was found between groups for YBT‐LQ Anterior Reach (ANT) side to side difference at 12 weeks (p = .008) with the Hip group demonstrating smaller side to side reach differences than the NoHip group. No significant side to side differences were seen between groups for YBT‐LQ Posteromedial (PM) or Posterolateral (PL) at 12 weeks (PM: p = .254; PL: p = .617).
Conclusions:
Rehabilitation including hip strengthening exercises appears to improve sagittal plane dynamic balance at three months post ACLR as compared to traditional rehabilitation. No differences were seen between groups for pain, ROM, and subjective function during the first 3 months following ACLR.
Level of Evidence:
Level 2b
Keywords: Anterior cruciate ligament, hip strengthening, rehabilitation
INTRODUCTION
Injuries to the anterior cruciate ligament (ACL) are common in a variety of sports. Mechanisms of injury to the ACL are often non‐contact in nature and involve landing, planting, cutting, and deceleration activities.15 These mechanisms may include movements in the frontal plane of motion which places the knee in a valgus loading position,3,4,6,7 thus increasing the risk of injury through an increased relative strain of the ACL.8,9 This valgus loading occurs rapidly after initial ground contact4 and weakness in the hip abductor muscles has been identified as a potential contributor to this motion.6 In healthy adults performing a single leg squat, there was a negative correlation between knee valgus and hip abduction strength.10 The greater the hip strength, the less the knee moved into a valgus position. When college athletes were tested on the single leg squat, hip external rotation strength was related to the amount of frontal plane motion at the knee.11 Likewise, when college athletes were tracked for lower extremity injury, those with greater strength in hip abduction and external rotation were less likely to be injured.12 Similarly, increased trunk displacement is greater in athletes with ACL injuries, signifying the body's ability to use the core muscles to control the knee may be impaired.13 These results suggest that hip strength may play a role in motion at the knee that could potentially predispose an athlete to a second ACL injury.
Paterno et al14 biomechanically tested fifty‐six athletes who had undergone ACL reconstruction (ACLR) and had been allowed to return to sport.Those (thirteen) who demonstrated altered hip kinetics and knee kinematics, and decreased single‐limb postural stability were more likely to suffer a subsequent second ACL injury. One of the factors that predisposed these athletes to a second ACL injury involves a loss of proximal neuromuscular control in the frontal and transverse planes.14 Likewise, deficits in hip muscle torque generated during landing contributed to future ACL injury. From these findings, the authors suggested that interventions following initial ACL reconstruction that target hip strength may be beneficial in reducing the risk of second ACL injury.14
The relationship between hip strength and knee pain has been established in the literature.15‐17 For the most part, this relationship has been studied in patients with patellofemoral pain (PFP); however, it is speculated that similar mechanics may play a role in ACL injury.6 The mechanics of ACL and patellofemoral injuries are comparable.6,11 As the knee moves into valgus there is an increase in strain on the ACL8,9 and this position has successfully predicted ACL injury in female athletes.3 Weakness in gluteal muscle strength has been suggested to contribute to this position and subsequent injury.3,13,14 The fact that hip strengthening in those with PFP has played a role in functional improvements leads one to question whether these exercises may have similar effects in the ACL‐reconstructed population. There is a lack of current evidence for the inclusion of specific hip strengthening exercises in the post‐operative rehabilitation of patients who have undergone ACLR, therefore, the purpose of this study was to determine the effects of the addition of isolated hip strengthening exercises to traditional rehabilitation on early outcomes (within the first 3 months) after ACLR. The authors hypothesized that patients who performed specific hip strengthening exercises in the early stages following ACLR would demonstrate better outcomes at 12 weeks post‐operative in self‐reported function, pain, ROM, and dynamic balance than those patients who did not perform hip strengthening exercises.
METHODS
Forty‐three participants (21 females, 22 males) volunteered for this study. Each participant was enrolled during the initial week of physical therapy following ACL reconstruction with an average starting date of 5 days post‐operative. A total of 92% of the reconstructions involved the dominant limb (right) of the participants. Demographics for the participants are listed in Table 1. Inclusion criteria were 1) an isolated ACL reconstruction, 2) between the ages of 14 and 40, and 3) physically or recreationally active a minimum of three times per week. Participants were excluded from the study if there was 1) a previous ACL tear and/or reconstruction on either side, 2) an associated chondral defect requiring surgical intervention, or 3) a meniscus tear requiring a repair. Patients gave informed consent once they were confirmed to meet the inclusion and exclusion criteria. Child assent and parental permission were obtained for those participants who were minors at the time of the study. Once enrolled in the study, objective measurements were taken on the participant's knee and patient outcome forms were completed. The Institutional Review Board of Texas Health Resources approved the research procedures.
Table 1.
Participant demographics for the Hip and NoHip groups following anterior cruciate ligament reconstruction
| Hip (n = 22) | No Hip (n = 21) | P Value | |
|---|---|---|---|
| Age (y/o) | 17.5±6.2 | 18.1±5.5 | .739 |
| Gender | |||
| • Male | 10 | 12 | .443 |
| • Female | 12 | 9 | |
| Involved Limb | |||
| • Right | 8 | 10 | .455 |
| • Left | 14 | 11 | |
| Mechanism of Injury | |||
| • Non‐contact | 14 | 14 | .414 |
| • Contact | 3 | 5 | |
| • Indirect contact | 5 | 2 | |
| Type of Graft | |||
| • Patellar Tendon | 20 | 18 | .491 |
| • Hamstring | 1 | 2 | |
| • Allograft | 1 | 1 |
Participants were randomly assigned into one of two different treatment groups (1 = traditional rehabilitation [NoHip], 2 = traditional plus isolated hip strengthening rehabilitation [Hip]). All participants began their rehabilitation program on the first day of study enrollment (average of 5 days post‐operative) and averaged two times per week in physical therapy for 12 weeks. Each participant was instructed in a home exercise program (HEP) to be performed a minimum of three times per week. Participants in the Hip group performed a series of hip strengthening exercises during each of their visits for a total of eight weeks (Appendix 1). Those in the NoHip group were not allowed to perform any of the hip strengthening exercises initially (Appendix 2), but were allowed to begin performing the exercises as part of their program at the 8 week mark. Between weeks 8 and 12, both groups continued to perform structured physical therapy (to include hip strengthening exercises) two times per week with an emphasis on developing the ability to demonstrate neuromuscular control with single limb activities.
The hip strengthening exercises (Table 2) were selected based on previous electromyographical (EMG) studies that demonstrated significant gluteal muscle activation, adequate for a strengthening stimulus.18‐22 The dosage for the hip strengthening exercises was gradually increased based upon the ability of the subject to perform the exercises correctly for a total of three sets of 10 repetitions. As example, if a subject could perform three sets of 10 repetitions of sidelying hip abduction without weight, then the decision was made to add between one and two pounds to the exercise as a means of progression. Because of the clinical nature of the study, the decision to progress in resistance with an exercise was made by the supervising physical therapist and in conjunction with the principal investigator.
Table 2.
Electromyographical (EMG) activity of the gluteus medius and gluteus maximus expressed as % of maximum voluntary contraction (MVIC) during selected exercises, as reported in the literature
| Hip Strengthening Exercise | Range of % MVIC Gluteus Medius | Range of % MVIC Gluteus Maximus |
|---|---|---|
| Sidelying Hip Abduction 21,23,24 | 42‐81 | 39‐51 |
| Sidelying Clam Shell21,23 | 38‐67 | 34‐53 |
| Bridge – Double Limb25 | 28 | 25 |
| Bridge – Single Limb21,25 | 47‐55 | 40‐54 |
| Prone Hip Extension21 | 46 | 59 |
| Quadruped arm/lower extremity lift25 | 42 | 56 |
| Side Bridge21,25 | 74‐103 | 21‐71 |
| Standing Hip Abduction24 | 33 | NT |
| Lateral Step‐up21,25 | 43‐59 | 29‐63 |
NT = Not tested
Knee extension range of motion (ROM) side to side difference, the International Knee Documentation Subjective Knee Form (IKDC), and a Visual Analog Scale (VAS) for pain were collected at 1, 4, 8, and 12 weeks post‐operative. The IKDC has previously been shown to be reliable and valid across a broad patient population23 and has demonstrated both internal consistency and validity in adolescents.24 For the measurement of pain, the VAS has been shown to be reliable25 and for purposes of this study, was recorded based upon activities of daily living during the 48 hours preceding the participant's physical therapy visit. In addition, the Y Balance Test – Lower Quarter (YBT‐LQ) (side to side difference) was measured at 8 and 12 weeks post‐operative. Knee extension ROM measurements were taken with a bubble goniometer while the patient was in a supine position with both knees in extension. The patient was instructed to actively tighten their quadriceps and fully straighten the knee to the best of their ability. The axis of the goniometer was placed at the center of the knee while the stationary arm was aligned through the shaft of the femur and the greater trochanter. The moving arm of the goniometer was aligned through the shaft of the fibula and pointed toward the center of the lateral malleolus. Knee extension measurements were taken by two physical therapists to ensure consistency. Prior to beginning the study, inter‐rater reliability for knee extension was calculated and found to be good (ICC(2,1) = 0.88, SEM = 0.10°).
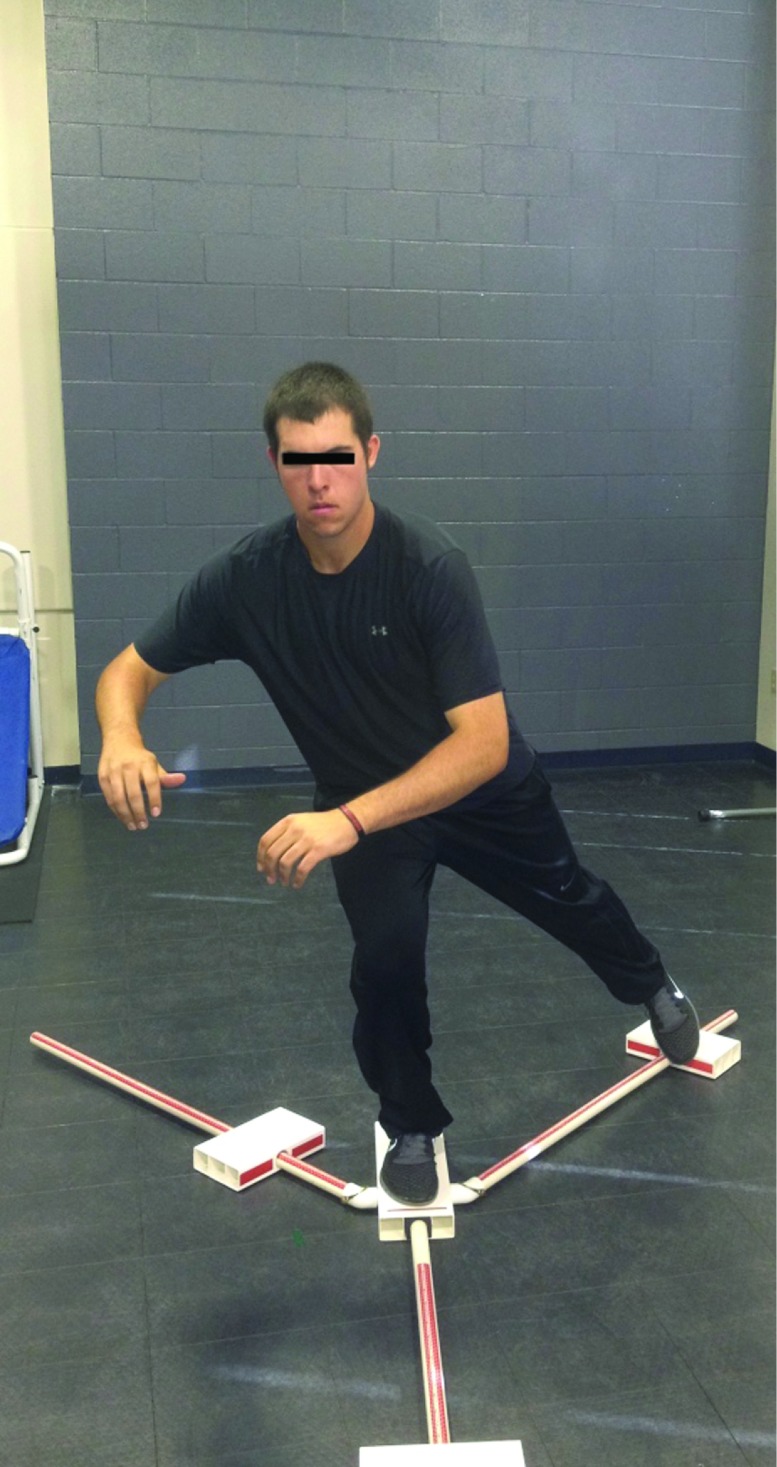
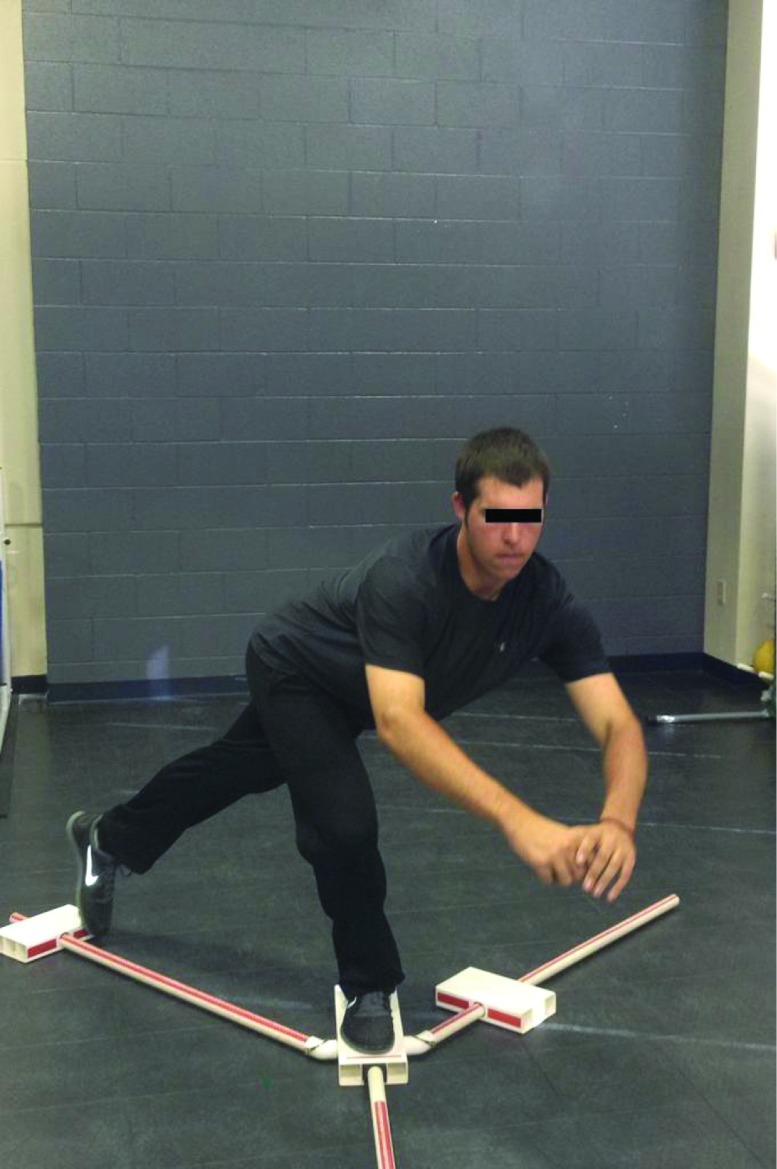
The YBT‐LQ™ was measured at both 8 and 12 weeks following ACL reconstruction. Measurements were taken in the anterior (ANT) (Figure 1), posteromedial (PM) (Figure 2), and posterolateral (PL) (Figure 3) directions on both the involved and uninvolved limbs. The participants were instructed in the YBT‐LQ protocol using a combination of verbal cues and demonstration.26 All participants wore shoes during testing and began on their uninvolved limb. The participants were asked to perform single limb stance on the extremity while reaching outside their base of support to push a reach indicator box along the measurement pipe. Elevation of the heel, toe or loss of balance resulting in a stepping strategy was recorded as a trial error indicating the trial should then be repeated.26 Participants were allowed at least three practice trials in the ANT, PM and PL directions prior to recording the best of three formal trials in each plane. Three trials were completed on the uninvolved limb in the ANT direction followed by three trials completed on the involved limb. This protocol was then replicated in the PM and PL directions. The maximal reach distance was recorded at the place where the most distal part of the foot reached based on the measurement pipe.26 Side‐to‐side limb reach differences were calculated by subtracting reach distance of the involved limb from the uninvolved limb. This measurement was used in order to establish asymmetries between the involved and uninvolved limbs during the first three months following ACLR. All balance measurements were taken by two physical therapists and one athletic trainer. Reliability standards were established between the clinicians involved in each of the three directions measured, ANT (ICC2,k = .86, SEM = 3.3 cm), PM (ICC2,k = .99, SEM = 1.7 cm), and PL (ICC2,k = .95, SEM = 2.7 cm). The reproducibility of this method was found to be acceptable.
Figure 1.
Y‐Balance Test‐Lower Quarter, anterior reach direction.
Figure 2.
Y‐Balance Test‐Lower Quarter, posteromedial reach direction.
Figure 3.
Y‐Balance Test‐Lower Quarter, posterolateral reach direction.
Statistical Analysis
An a priori analysis with YBT‐LQ Anterior reach side to side difference determined that 10 participants in each group were needed at .80 power, p < 0.05 for statistical significance. A mixed model repeated measures ANOVA was used to determine differences between IKDC, VAS, and knee extension ROM. Two one‐way ANOVAs were used to calculate mean group differences for YBT‐LQ at 8 and 12 weeks. All analyses were calculated using SPSS version 19.0 (Chicago, IL 60606).
RESULTS
The mean number of physical therapy visits per week was not statistically different between both the Hip (1.90±.53) and NoHip. (2.1±.48) groups (p = 0.14). There was a significant main effect for time on IKDC, VAS, and extension ROM (p < 0.001). No significant interaction was seen for IKDC (F1, 41 = .053, p = .819), VAS (F1,41 = .549, p = .463), or extension ROM (F1,41 = .434, P = .513) between groups at 1 week, 4 weeks, 8 weeks, or 12 weeks. For YBT‐LQ measurements at 8 weeks, there were no significant differences between groups for ANT (p = .535), PM (p = .494), or PL (p = .265). At 12 weeks, participants in the hip strengthening group demonstrated significantly less side to side differences in the ANT direction when compared to those in the NoHip group (p = .008); however, there were no significant differences in PM (p = .254), or PL (p = .617). Table 3 outlines the group means and standard deviations for each variable across all time points.
Table 3.
Means and standard deviations for measurements at time points of 1 week, 4 weeks, 8 weeks, and 12 weeks between both groups
| Hip Strength | NoHip Strength | Significance Level | ||
|---|---|---|---|---|
| IKDC | 1 week | 22.3±12.2 | 25.6±11.5 | p = 0.819 |
| 4 weeks | 53.7±8.1 | 53.5±7.8 | ||
| 8 weeks | 62.8±7.6 | 62.6±16.4 | ||
| 12 weeks | 71.3±10.1 | 72.7±10.7 | ||
| VAS | 1 week | 5.8±2.1 | 5.1±1.9 | p = 0.463 |
| 4 weeks | 1.95±1.5 | 1.3±1.6 | ||
| 8 weeks | .89±1.0 | .52±.67 | ||
| 12 weeks | .69±1.1 | .67±1.1 | ||
| Knee Extension ROM | 1 week | 10.5±7.4° | 10.0±3.0° | p = 0.513 |
| 4 weeks | 3.4±2.2° | 3.7±3.0° | ||
| 8 weeks | 1.7±1.5° | 1.7±2.1° | ||
| 12 week | 1.4±1.9° | 1.5±2.2° | ||
| Y Balance (cm) | 8 weeks | |||
| ANT | 5.9±3.2 | 6.7±5.1 | p = 0.535 | |
| PM | 4.6±3.5 | 4.5±4.6 | p = 0.494 | |
| PL | 6.3±4.6 | 4.9±3.3 | p = 0.265 | |
| 12 weeks | ||||
| ANT | 2.7±2.9 | 6.1±4.6 | p = 0.008* | |
| PM | 2.5±2.8 | 3.7±3.9 | p = 0.254 | |
| PL | 3.4±3.5 | 2.9±3.6 | p = 0.617 |
Denotes statistically significant difference
DISCUSSION
The purpose of this study was to investigate the effects of isolated hip strengthening exercises (added to a traditional rehabilitation program) on early outcomes following ACLR. The authors' hypothesized that those in the Hip group would demonstrate better outcomes in self‐reported function, pain, ROM, and dynamic balance than those who did not perform hip strengthening exercises at 12 weeks post‐operative. Participants who performed hip strengthening exercises during the first eight weeks following ACLR demonstrated lower side to side YBT‐LQ anterior reach differences at three months between the involved and uninvolved limbs when compared to participants who did not perform hip strengthening exercises. No differences were seen in IKDC, VAS, or knee extension ROM at 1, 4, 8 or 12 weeks between groups. Because these exercises were performed early in the rehabilitation process following ACL reconstruction, any improvements in hip strength or neuromuscular control might not have translated to less functional patient‐reported outcomes (IKDC, VAS). Similarly, the exercises chosen for the study may not have provided a training stimulus great enough to elicit a change in the participant's perception of function, pain level, or knee extension ROM. The results of this study suggest that hip strength may not be directly related to IKDC or VAS and may not play a role in the restoration of knee extension ROM.
Proximal control at the pelvis and trunk is required during single limb activities.20 The hip strengthening exercises performed by the Hip group in this study have previously been shown sufficient to provide a strength training stimulus in both the gluteus medius and maximus.18,20‐22 In order to reach a muscle activation threshold to produce a strengthening effect at the trunk and hip musculature, the exercise must elicit between 40% and 60% of maximum voluntary isometric contraction (MVIC).22,27 Based upon the existing evidence, the majority of hip strengthening exercises in the current study met these criteria. These results of the current investigation suggest that it is plausible there may have been an increase in strength in the Hip group that may not have been present in the NoHip group; however, the fact that the hip strength of these patients was not tested at either the beginning or at the 12 week mark precludes the conclusion of strength gains in the Hip group. Participants in this study were post‐operative, so it was not possible to obtain an accurate hip strength measurement during the initial stages of physical therapy and thus baseline strength for the gluteus medius and maximus was unable to be established.
Norris et al28 previously demonstrated that the gluteus medius produces a higher normalized EMG signal in the anterior reach direction when compared to the posteromedial reach. Likewise, the action of the anterior reach is essentially a single leg squat and, as such, produces high EMG activation of the gluteus medius and maximus19,20,29 and earlier gluteus medius activity in individuals who perform a “good” squat.30 This increase in gluteal muscle activation is theorized to promote pelvic stability during single limb functional movements,31 minimize trunk collapse and valgus movement at the knee,30 and may explain why participants in the Hip group demonstrated smaller side to side reach differences in the anterior direction than the participants in the NoHip group. Furthermore, the mean side to side anterior reach difference (2.7 cm) in the Hip group was below the 4 cm cut‐off for risk of lower extremity injury in basketball players that was previously published32 while those in the NoHip group (6.1 cm) demonstrated larger differences. While this data involves post‐operative ACL reconstruction participants and cannot be directly compared to healthy basketball players,32 it does provide a guideline that can be used in the clinical decision‐making process.
YBT‐LQ reach differences were not seen between groups at 8 weeks in any of the directions (ANT, PM, PL). Each participant in the Hip group performed hip strengthening exercises for the first eight weeks following surgery at which time the NoHip group was not allowed to begin hip strengthening. Any gains in strength that may have occurred in the Hip group during the first eight weeks are most likely related to neural adaptations from performing these exercises.33,34 While the hip strengthening exercise program may have produced high EMG activity in the gluteal muscles,18,19,21,22 the movements performed during the YBT‐LQ testing require a synergy of muscles working together and could reflect efficiency of neuromuscular coordination.33 It is possible that one of the reasons there were no differences in YBT‐LQ reach between the two groups at eight weeks is that the Hip group had yet to establish an efficient neuromuscular control pattern in this complex movement despite building a foundation of hip strength in less functional exercises. Likewise, the overall total volume of exercises performed by the Hip group was greater at 12 weeks than at the 8‐week mark. This increase in volume may have led to improvements in neuromuscular activation or actual strength parameters at the hip which allowed the participants in the hip strengthening group to reach outside their base of support.35
Previous research in the realm of examination of subjects with patellofemoral pain has demonstrated that weakness in the gluteal muscles may contribute to altered kinematics at the knee.15‐17 Dynamic MRI demonstrates greater knee adduction and hip internal rotation in patients with patellofemoral pain.36 These altered mechanics are believed to be similar to the mechanism for ACL injuries. Biomechanical measures of frontal plane loading in knee valgus and decreased neuromuscular control at the hip predict ACL injury in female athletes.3 Similarly, knee valgus loading and compensations at the contralateral hip are partially responsible for predicting a second ACL injury.14 As such, it would seem plausible that a rehabilitation program that addresses these altered kinematics and potential ACL risk factors through hip strengthening exercises may be important following ACLR. Those participants in our study who performed hip strengthening exercises in the early phases of rehabilitation following ACLR demonstrated less asymmetry in performance of single leg squat at three months than those who did not perform hip strengthening. These results suggest that hip strengthening exercises help to build single leg strength and neuromuscular control and may provide a platform on which to build in the later stages of ACL rehabilitation.
Limitations
The fact that gluteal muscle strength was not measured in these patients precludes a direct association between improvements in YBT‐LQ anterior reach and strength in the Hip group from being made. Although it would appear that participants in the Hip group may have benefited from performing the gluteal exercises during the initial stages of the rehabilitation process, the results from the current investigation are unable to validate whether actual strength gains occurred that might have contributed to the YBT‐LQ performance at 12 weeks.
All participants in this study averaged two times per week of structured physical therapy over a 12‐week period; however, absolute compliance with the HEP when they were not under the supervision of the physical therapists cannot be guaranteed. Attempts were made to minimize non‐compliance with participant and treating therapist education regarding the exercise programs for both groups (Hip and NoHip) in the clinic and in the HEP. Each participant was a patient within the physical therapy setting and the principal investigator was able to visit with each individual on a weekly basis and monitor the exercise programs.
CONCLUSION
Isolated hip strengthening exercises may not influence early outcome measurements such as patient outcome forms, pain levels or ranges of motion, but they may be beneficial for the development of single limb function during the first three months of a rehabilitation program following ACL reconstruction.
Appendix 1
ACL ReconstructionHip Strengthening Rehabilitation Program
| Exercises should be gradually progressed based upon the patient's ability to perform correctly and without an increase in pain. |
| Phase 1 (0 to 4 weeks) ‐ |
| Goals: Control of pain and swelling |
| Restoration of Patellar Mobility |
| Emphasis on full extension |
| Increased quadriceps isometric strength |
| Normalized gait/Weight Shifting |
| Specific Exercises: |
| Patellar Mobilizations (superior‐inferior‐medial‐lateral; anterior interval, suprapatellar pouch) |
| Quad Sets (with NM E‐stim) – if patient is unable to perform a straight leg raise without an extension lag |
| Heel slides |
| Gastrocnemius Stretch |
| Isometric hamstring contractions |
| Straight leg raise (SLR) – hip flexion |
| Dynamic Warm‐up |
| Short Arc Quads (SAQ) – range of 90° to 40° |
| Mini‐Squats – range of 0°to 30° |
| Weight shifts (body weight) – progress to single leg balance |
| Double Leg Dead Lift (shortened range of motion with gradual progression) |
| Bilateral Shuttle Leg Press |
Hip strengthening exercises performed during the first 8 weeks following surgery:
|
*Prior to progressing into Phase 2:
|
| Phase 2 (5 to 12 weeks) ‐ |
| Goals: Improving single leg strength and neuromuscular control |
| Developing strength and stability in all planes of motion and under various proprioceptive conditions Maximizing cardiovascular fitness and muscle endurance |
| Specific Exercises: |
| Continue with and increase repetitions/weight of Phase 1 exercises, plus: |
| Single Leg Dead Lift (Progression: Sagittal → Transverse) |
| Shuttle (Progression: Bilateral → Unilateral → Bilateral Jumps → Unilateral Jumps) |
| Lunge (Progression: Forward → Backward → Lateral → Transverse) |
| Balance Board (Progression: Sagittal → Frontal → UE manipulation w/ balance board) |
| Step‐ups (Progression: Sagittal → Frontal → Transverse → UE manipulation with step‐ups) |
| * Addition: Lateral Step‐up |
| BW double/single leg squats (progress depth and resistance with sport cord as hip/knee control improves) |
| Lateral Band Walk |
| Forward + Backward Jogging/Lateral agility (Progression: no weight → green sport cord → black sport cord) |
| *Must demonstrate shuttle jump control prior to F/B jogging/lateral agility activities |
Appendix 2
ACL Reconstruction NoHip Strengthening Rehabilitation Program
| Exercises should be gradually progressed based upon the patient's ability to perform correctly and without an increase in pain. |
| Phase 1 (0 to 4 weeks) ‐ |
| Goals: Control of pain and swelling |
| Restoration of Patellar Mobility |
| Emphasis on full extension |
| Increased quadriceps isometric strength |
| Normalized gait/Weight Shifting |
| Specific Exercises: |
| Patellar Mobilizations (superior‐inferior‐medial‐lateral; anterior interval, suprapatellar pouch) |
| Quad Sets (with NM E‐stim) – if patient is unable to perform a straight leg raise without an extension lag |
| *initiated during 1st week and continued through 4 weeks if necessary |
| Heel slides |
| Gastrocnemius Stretch |
| Isometric hamstring contractions |
| Straight leg raise (SLR) – hip flexion |
| Dynamic Warm‐up |
| Short Arc Quads (SAQ) – range of 90° to 40° |
| Mini‐Squats – range of 0°to 30° |
| Weight shifts (body weight) – progress to single leg balance |
| Double Leg Dead Lift (shortened range of motion with gradual progression) |
| Bilateral Shuttle Leg Press |
NOTE: Prior to progressing into Phase 2:
|
| Phase 2 (5 to 12 weeks) ‐ |
| Goals: Improving single leg strength and neuromuscular control |
| Developing strength and stability in all planes of motion and under various proprioceptive conditions |
| Maximizing cardiovascular fitness and muscle endurance |
| Specific Exercises: |
| increase repetitions/weight of Phase 1 exercises, plus: |
| Single Leg Dead Lift (Progression: Sagittal → Transverse) |
| Shuttle (Progression: Bilateral → Unilateral → Bilateral Jumps → Unilateral Jumps) |
| Lunge (Progression: Forward → Backward → Lateral → Transverse) |
| Balance Board (Progression: Sagittal → Frontal → UE manipulation w/ balance board) |
| Step‐ups (Progression: Sagittal → Frontal → Transverse → UE manipulation with step‐ups) |
| BW double/single leg squats (progress depth and resistance with sport cord as hip/knee control improves) |
| Forward + Backward Jogging/Lateral agility (Progression: no weight → green sport cord → black sport cord) |
| *Must demonstrate shuttle jump control prior to F/B jogging/lateral agility activities |
| *Participants are allowed to begin hip strengthening exercises (below) after 8 weeks of rehabilitation. |
| Sidelying Hip Abduction * |
| Prone Hip Extension * |
| Clam Shells * |
| Double leg Bridges * |
| Single leg bridges * |
| Quadruped Arm/LE lift * |
| Side Bridge (Plank) * |
| Standing Hip Abductions * |
REFERENCES
- 1.Arendt EA Agel J Dick R Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34:86‐92 [PMC free article] [PubMed] [Google Scholar]
- 2.Boden BP Torg JS Knowles SB Hewett TE Video analysis of anterior cruciate ligament injury: Abnormalities in hip and ankle kinematics. Am J Sports Med. 2009;37:252‐259 [DOI] [PubMed] [Google Scholar]
- 3.Hewett TE Myer GD Ford KR Heidt RS Colosimo AJ McLean SG van den Bogert AJ Paterno MV Succop P Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes. Am J Sports Med. 2005;33:492‐501 [DOI] [PubMed] [Google Scholar]
- 4.Koga H Nakamae A Shima Y Iwasa J Myklebust G Engebretsen L Bahr R Krosshaug T Mechanisms for noncontact anterior cruciate ligament injuries. Knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med. 2010;38:2218‐2225 [DOI] [PubMed] [Google Scholar]
- 5.Krosshaug T Slauterbeck JR Engebretsen L Bahr R Biomechanical analysis of anterior cruciate ligament injury mechanisms: three‐dimensional motion reconstruction from video sequences. Scand J Med Sci Sports. 2007;17:508‐519 [DOI] [PubMed] [Google Scholar]
- 6.Geiser CF O'Connor KM Earl JE Effects of isolated hip abductor fatigue on frontal plane knee mechanics. Med Sci Sports Med. 2010;42:535‐545 [DOI] [PubMed] [Google Scholar]
- 7.Joseph MF Rahl M Sheehan J MacDougal B Horn E Denegar CR Trojian TH Anderson JM Kraemer WJ Timing of lower extremity frontal plane motion differs between female and male athletes during a landing task. Am J Sports Med. 2011;39:1517‐1521 [DOI] [PubMed] [Google Scholar]
- 8.Markolf KL Burchfield DM Shapiro MM Shepard MF Finerman GA Slauterbeck JR Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13:930‐935 [DOI] [PubMed] [Google Scholar]
- 9.Quatman CE Kiapour AM Demetropoulos CK Kiapour A Wordeman SC Levine JW Goel VK Hewett TE Preferential loading of the ACL compared with the MCL during landing. A novel In Sim approach yields the multiplanar mechanism of dynamic valgus during ACL injuries. Am J Sports Med. 2013;42:177‐186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Claiborne TL Armstrong CW Gandhi V Pincivero DM Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech. 2006;22:41‐50 [DOI] [PubMed] [Google Scholar]
- 11.Willson JD Ireland ML Davis IS Core strength and lower extremity alignment during single leg squats. Med Sci Sports Med. 2006;38:945‐952 [DOI] [PubMed] [Google Scholar]
- 12.Leetun DT Ireland ML Willson JD Ballantyne BT Davis IS Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Med. 2004;36:926‐934 [DOI] [PubMed] [Google Scholar]
- 13.Zazulak BT Hewett TE Reeves NP Goldberg B Cholewicki J Deficits in neuromuscular control of the trunk predict knee injury risk. A prospective biomechanical‐epidemiologic study. Am J Sports Med. 2007;35:1123‐1130 [DOI] [PubMed] [Google Scholar]
- 14.Paterno MV Schmitt LC Ford KR Rauh MJ Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968‐1978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fukuda TY Rossetto FM Magalhaes E Bryk FF Lucareli PR de Almeida Aparecida Carvalho N Short‐term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther. 2010;40:736‐742 [DOI] [PubMed] [Google Scholar]
- 16.Earl JE Hoch AZ A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011;39:154‐163 [DOI] [PubMed] [Google Scholar]
- 17.Bolgla LA Malone TR Umberger BR Uhl TL Comparison of hip and knee strength and neuromuscular activity in subjects with and without patellofemoral pain syndrome. Int J Sports Phys Ther. 2011;6:285‐296 [PMC free article] [PubMed] [Google Scholar]
- 18.Ayotte NW Stetts DM Keenan G Greenway EH Electromyographical analysis of selected lower extremity muscles during 5 unilateral weight‐bearing exercises. J Orthop Sports Phys Ther. 2007;37:48‐55 [DOI] [PubMed] [Google Scholar]
- 19.Boren KB Conrey C Le Coguic J Paprocki L Voight M Robinson TK Electromyographic analysis of gluteus medius and gluteus maximus during rehabilitation exercises. Int J Sports Phys Ther. 2011;6:206‐223 [PMC free article] [PubMed] [Google Scholar]
- 20.DiStefano LJ Blackburn JT Marshall SW Padua DA Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther. 2009;39:532‐540 [DOI] [PubMed] [Google Scholar]
- 21.Bolgla LA Uhl TL Electromyographic analysis of hip rehabilitation exercises in a group of healthy subjects. J Orthop Sports Phys Ther. 2005;35:487‐494 [DOI] [PubMed] [Google Scholar]
- 22.Ekstrom RA Donatelli RA Carp KC Electromyographic analysis of core, trunk, hip, and thigh muscles during 9 rehabilitation exercises. J Orthop Sports Phys Ther. 2007;37:754‐762 [DOI] [PubMed] [Google Scholar]
- 23.Higgins LD Taylor MK Park D Ghodadra N Marchant M Pietrobon R Cook C Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Joint Bone Spine. 2007;74:594‐599 [DOI] [PubMed] [Google Scholar]
- 24.Schmitt LC Paterno MV Huang S Validity and internal consistency of the International Knee Documentation Committee Subjective Knee Evaluation Form in children and adolescents. Am J Sports Med. 2010;38:2443‐2447 [DOI] [PubMed] [Google Scholar]
- 25.Bijur PE Silver W Gallagher EJ Reliability of the Visual Analog Scale for measurement of acute pain. Academic Emergency Medicine. 2001;8:1153‐1157 [DOI] [PubMed] [Google Scholar]
- 26.Plisky PJ Gorman PP Butler RJ Kiesel KB The reliability of an instrumented device for measuring components of the star excursion balance test. N Amer J Sports Phys Ther. 2009;4:92‐99 [PMC free article] [PubMed] [Google Scholar]
- 27.Andersen LL Magnusson SP Nielsen M Haleem J Poulsen K Aagaard P Neuromuscular activation in conventional therapeutic exercises and heavy resistance exercises: implications for rehabilitation. Phys Ther. 2006;86:683‐697 [PubMed] [Google Scholar]
- 28.Norris B Trudelle‐Jackson E Hip‐ and thigh‐muscle activation during the Star Excursion Balance Test. J Sport Rehab. 2011;20:428‐441 [DOI] [PubMed] [Google Scholar]
- 29.Lubahn AJ Kernozek TW Tyson TL Merkitch KW Reutemann P Chestnut JM Hip muscle activation and knee frontal plane motion during weight bearing therapeutic exercises. Int J Sports Phys Ther. 2011;6:92‐103 [PMC free article] [PubMed] [Google Scholar]
- 30.Crossley KM Zhang WJ Schache AG Bryant A Cowan SM Performance on the single‐leg squat task indicates hip abductor muscle function. Am J Sports Med. 2011;39:866‐873 [DOI] [PubMed] [Google Scholar]
- 31.Vezina MJ Hubley‐Kozey C Muscle activation in therapeutic exercises to improve trunk stability. Arch Phys Med Rehabil. 2000;81:1370‐1379 [DOI] [PubMed] [Google Scholar]
- 32.Plisky PJ Rauh MJ Kaminski TW Underwood FB Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36:911‐919 [DOI] [PubMed] [Google Scholar]
- 33.Carroll TJ Riek S Carson RG Neural adaptations to resistance training. Sports Med. 2001;31:829‐840 [DOI] [PubMed] [Google Scholar]
- 34.McCarthy JP Pozniak MA Agre JC Neuromuscular adaptations to concurrent strength and endurance training. Med Sci Sports Exerc. 2002;34:511‐519 [DOI] [PubMed] [Google Scholar]
- 35.Filipia A Byrnes R Paterno MV Myer GD Hewett TE Neuromuscular training improves performance on the Star Excursion Balance Test in young female athletes. J Orthop Sports Phys Ther. 2010;40:551‐558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Souza RB Draper CE Fredericson M Powers CM Femur rotation and patellofemoral joint kinematics: a weight‐bearing magnetic resonance imaging analysis. J Orthop Sports Phys Ther. 2010;40:277‐285 [DOI] [PubMed] [Google Scholar]