Abstract
Head injuries, including concussions, in athletes can account for an extended period of time lost from sports competition. Neurocognitive and balance deficits which may linger following a concussion affect an athlete's ability to return to sport safely. If these deficits are not specifically addressed in a rehabilitation program then the athlete may be at risk for not only additional concussions but possible musculoskeletal injury. ImPACT testing is a reliable method for identifying neurocognitive deficits and assists in the development of a neurocognitive training program. The information gathered from ImPACT may also indicate risk for musculoskeletal injuries. Research evidence suggesting specific rehabilitation strategies and interventions addressing neurocognitive deficits following a concussion is lacking. Progressions in a neurocognitive training program may include the integration of balance, reaction training, and activities that address memory deficits. The purpose of this case report is to discuss the evaluation and treatment plan for a female snowboard athlete following a concussion.
Level of Evidence:
5
Keywords: Concussion, neurocognitive rehabilitation, reaction training
BACKGROUND AND PURPOSE
Emergency department data in the United States indicates that roughly 173,285 sports and recreational related traumatic brain injuries (TBI) occur per year, including concussions.1 Additionally, national injury surveillance data has indicated that TBI accounts for 9% of all injuries in high school sports.2 A concussion is typically defined as a temporary loss of brain function which may be accompanied by physical, cognitive or emotional symptoms and may be categorized as a traumatic head injury depending upon severity. Concussion rates in high school athletes have been found to be highest in the athletes who participate in boys lacrosse, boys hockey, football, girls lacrosse, and girls soccer.3,4 While there is an obvious correlation between the contact nature of sports like hockey, football and lacrosse with concussion rate, sports that require change of direction, acceleration, high‐risk maneuvers and participation on varied surfaces with the potential for changing climate conditions must also be considered. A sport such as snowboarding fits this category and also involves a high‐risk for musculoskeletal injuries as well. While there is extensive research evidence which discuss the rate of musculoskeletal injuries in snowboarding, with injuries to the wrist, hand, shoulder and ankle having the highest occurrence,5,6,7,8 literature investigating the concussion rate in this sport is lacking. Data from injury surveillance records indicates that while head injuries do occur in snowboarding, these injuries are categorized in most studies as injuries to the head and face, which may include both lacerations and traumatic brain injuries, with no mention of concussion occurrence in either case.9,10,11,12 In a ten‐year retrospective review of ski and snowboard‐related injuries, head injuries accounted for 52% of total injuries with roughly 24% of these injuries occurring in the snowboard population.11 The majority of these head injuries were then identified as traumatic brain injuries which occurs when an external force traumatically injures the brain and can be potentially fatal.11 Given the increased focused on concussion and head injury occurrence in contact sports such as football, hockey and lacrosse as previously discussed,3,4 it would be important to further investigate the prevalence and risk of concussion in sports such as snowboarding, freestyle skiing, skateboarding, or extreme freestyle motorbiking which combine high velocity with the performance of aerial stunts or tricks. This becomes especially relevant as experienced athletes in these sports attempt more technical jumps and stunts, often associated with increased risk for injury in general.13
Wilkerson and Swanik identified a possible link between neurocognitive deficits and risk for musculoskeletal injuries.14,15 A reaction time composite score ≥ .545 seconds on ImPACT testing was correlated to a two‐fold risk of injury.14 Delayed reaction time is hypothesized to contribute to injury risk due to a diminished capacity for neuromuscular control resulting from deficits in cortically driven reaction time and processing speed.15 This may indicate that improvements in neurocognitive function must be achieved before returning an athlete to sport following a concussion as increased musculoskeletal injury risk may exist. Medical information should also include concussion and orthopedic injury history in order to determine if further evaluation is needed to specifically identify risk factors for further injury.
An important component of return to play decision‐making following a concussion is neurocognitive testing. Immediate Post‐Concussion Assessment and Cognitive Testing (ImPACT, ImPACT Applications, Inc., Pittsburgh, PA) has been shown to be a valid measure for examining deficits in reaction time, processing speed, working memory, attention and concentration in addition to having considerable specificity and sensitivity in identifying neurocognitive deficits following a concussion.16,17 In addition, ImPACT has been used as a reliable tool to determine neurocognitive function and guide decision‐making while managing athletes who have sustained a concussion.18 While ImPACT testing is widely used and accepted, reliability and validity of scores between age groups requires further investigation. Despite information that can be gathered from ImPACT testing with regard to neurocognitive deficits, literature supporting a specific rehabilitation program designed to address memory, concentration, processing speed and reaction time following sports‐related concussion is lacking. An active recovery program implemented by Gagnon et al has been shown to promote recovery in children and adolescents with post‐concussion symptoms.19 The program included gradual progression of aerobic and sports specific activities in addition to sports‐specific imagery and visualization training that was integrated with an individualized home program.19 However, this active recovery program did not specifically address specific neurocognitive deficits.
The purpose of this case report is to review the presentation of signs and symptoms as well as the evaluation of neurocognitive deficits and development of a neurocognitive retraining program in a female adolescent snowboard athlete following a concussion. In addition, a clinic‐based rehabilitation program specifically addressing balance and neurocognitive deficits will be presented.
CASE DESCRIPTION
The subject of this case report was a 17‐year‐old female snowboard cross athlete who was referred from her family medicine doctor for ImPACT testing and vestibular rehab following a concussion. The subject provided signed consent and permission was granted to use her case for publication purposes. She presented to the sports medicine clinic for initial evaluation and treatment thirteen days following a concussion sustained when she caught her heel edge of her snowboard while landing from a jump and subsequently hit her head backwards. She reported wearing a helmet at the time of injury. She was initially evaluated by medical personnel at her local snowboarding club then referred to a doctor trained in concussion management. She denied loss of consciousness but verbalized difficulty in remembering events that occurred during and immediately following the injury. In addition, she reported post‐concussion symptoms which included occasional headaches, difficulty with memory and concentration, as well as difficulty falling asleep. She reported a history of four previous concussions (March 2008, November 2009, February 2011, January 2012) leading up to her most recent episode in January 2013. Orthopedic history included injuries to her low back and left cervical spine while shoveling snow eight days prior and well as a right tibial plateau fracture while snowboarding which required surgical intervention three years prior to her recent concussion episode.
INITIAL EXAMINATION FINDINGS
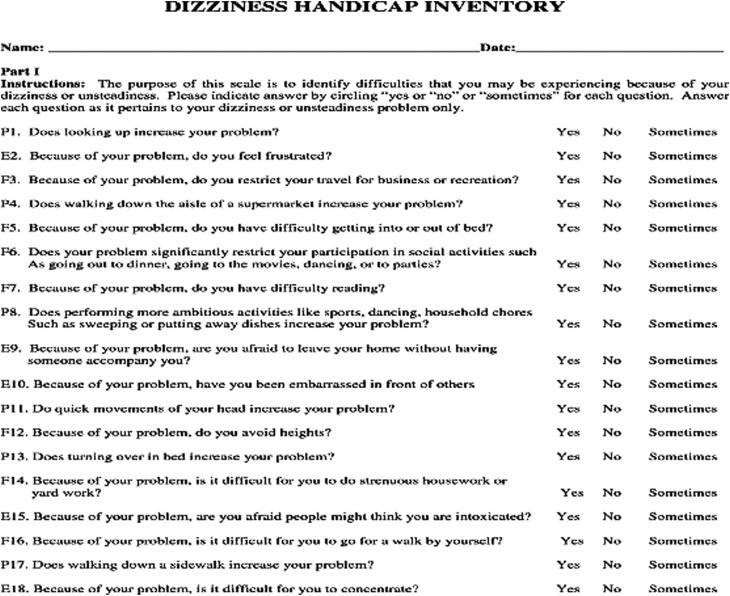
Subjective questionnaires included a self‐reported confidence rating (0‐100 scale where 100% represents complete confidence in full return to sports activities) and a Dizziness Handicap Inventory (DHI) which has been shown to have excellent reliability and validity when identifying perceived physical, emotional and functional limitations resulting from vestibular dysfunction.20 The DHI is scored 0‐100 with a high score of 70‐100 indicating a severe perception of handicap, 40‐69 moderate, and 39‐0 low (Appendix 1). Items are scored according to responses that include never (0), sometimes (2) and always (4).
A higher perception of handicap on the DHI has been correlated with increased episodes of dizziness or unsteadiness in subjects with balance deficits.20 Given the athlete's concussion history and self‐reported symptoms, completion of an ImPACT test for post‐injury baseline measures was appropriate in order to gather information regarding her neurocognitive status and to assess memory, processing speed, and reaction time given her self‐reported difficulty concentrating and with both short and long‐term memory. Data from subjective questionnaires and ImPACT testing can be found in Table 1. Information gathered from ImPACT testing would be an important component for development of this athlete's neurocognitive training program. The score report indicated that the athlete was in the lower 6th and 51st percentile for verbal memory and reaction time, respectively, as well as 64th percentile for visual motor speed within her age group. Thus, her training program would likely incorporate exercises addressing these problem areas.
Table 1.
| CASE STUDY OUTCOMES | INITIAL EVALUATION | RE‐EVALUATION |
|---|---|---|
| Baseline (week 1) | Follow‐up (week 8) | |
| Verbal Memory | 69 | 70 |
| Visual Memory | 77 | 72 |
| Visual Motor Speed | 42.33 | 43.18 |
| Reaction Time | .56 | .51 |
| Cognitive Efficiency Index | .24 | .26 |
| BESS (total errors) | 25 | 18 |
| DHI | 38 | 14 |
| Confidence rating (%) | 30 | 70 |
Red font indicates outcomes with poor performance noted at initial evaluation.
In addition to neurocognitive testing, a thorough post‐concussion examination should include cervical spine assessment and balance testing in order to identify deficits which may exist in cervical range of motion (ROM) and balance which, if not addressed in a formal rehab program, could contribute to risk for further injury or concussion when returning to sport. Furthermore, restrictions in cervical motion as well as pain could limit the athlete's ability to tolerate reaction training and visual processing activities which would be incorporated in her neurocognitive retraining program. In this case, assessment findings included cervical active and passive ROM which were symmetrical and within normal limits. Balance was assessed using the Balance Error Scoring System (BESS) as this has been supported as both a valid and reliable measure for assessing postural stability.21,22,23 A higher score on the BESS test indicates a high number of balance errors and possible deficits in the somatosensory, visual, and vestibular components of the balance system as tests are performed on both stable and unstable surfaces with eyes either open or closed. This athlete's BESS score was 25 which would be categorized as very poor according to her closest age group (20‐29) reference values where averages for men and women in this age group were 10 and 11, respectively.24 Norms for her age group (10‐19) were not available. This indicates that significant balance deficits were present in this subject following concussion and that she would likely benefit from balance training as a part of her rehabilitation program.
INITIAL INTERVENTIONS
The initial phase of her rehabilitation program included education on proper transversus abdominis and gluteal muscle activation patterns through isometric and isotonic strengthening exercises with the goal of providing stabilization of the pelvic area during balance exercises (Table 2). These activation patterns were then integrated with BESS testing exercise progressions which included standing with double leg, single leg and tandem stance support on both firm ground and foam surfaces while also challenging visual input by performing exercises with eyes closed. Static balance positions were integrated initially, prior to dynamic positions to allow for proper stabilization and muscle activation sequences while challenging all components of the balance system (Figure 1). Visual focus exercises, designed to strengthen muscles around the eyes responsible for dynamic gaze stabilization, were integrated separately to improve focus and concentration while incorporating visual tracking. These exercises have been shown to improve balance as well as both hand and eye coordination and consisted of visual tracking activities at various speeds across multiple planes.25 The athlete was instructed on integration of these exercises in her home program, to be performed daily for three sets of 30 seconds of visual tracking across all planes, as well as daily short and long‐term word recall exercises to address memory deficits.
Table 2.
| Rehab Phase | Balance/Cognitive Retraining Activities |
|---|---|
| Phase 1‐Foundational core/gluteal muscle strengthening with static balance exercises |
Core/Gluteal strengthening (2 of 15 reps each) Transversus Abdominis contractions (supine) Supine bridging (double to single leg) Clams Prone hip extension Sidelying hip abduction |
|
Static Balance (performed on ground/foam, 2 sets of 15‐30 second holds) Double to single leg stance Tandem stance Weightshifting (all stance positions) with perturbations Weightshifting (all stance positions) with eyes closed Weightshifting with eyes closed, add perturbations |
|
| Phase 2‐Dynamic balance with reaction/cognitive training exercises |
Dynamic Balance (3 sets of 30 second holds each) Weightshifting on Bosu (both sides) with eyes open or closed, perturbations added Snowboard balance on Bosu (both sides) with eyes open or closed, perturbations added |
|
ADD Reaction/Cognitive Training Exercises (performed for duration of balance exercise) Reach within/outside BOS towards laser target Perform “go/no go” task (red light=go, blue light=no go) Eyes closed, open to verbal command and perform “go/no go task” Perturbations added during reaction/cognitive training tasks |
|
| Phase 3‐Plyometric training combined with cognitive training exercises |
Plyometric exercises (2 sets of 10 reps each direction) Forward/backward jumps (ground, onto/off box/foam) Lateral jumps (ground, onto/off box/foam) Multidirectional jumps (diagonal, 90/180 degree turns) on ground or onto/off box/foam |
| ADD verbal and visual cues (laser, manual direction) | |
| ADD “go/no go” task |
Figure 1.
Example of static balance training exercise, tandem stance on foam.
After two treatment sessions which occurred at the rate of one session per week over the course of two weeks, the athlete was able to progress to dual task training exercises without occurrence of headaches or exacerbation of symptoms initially reported. Integration of visual tracking and stabilization exercises with balance exercises has been shown to improve balance scores following a dual task training program.26 Visual tracking exercises also incorporated reaction training which involved tracking a laser pointer on fixed points and locating points that would appear while balancing on both stable and unstable surfaces (Figure 2). In addition, cognitive retraining exercises were combined with these dual tasks to improve outcomes.27,28 Examples would include balance on an unstable surface with perturbations while completing long and short‐term word recall, number sequencing, and word association tasks. Reaction training using a laser pointer was only introduced when the athlete could demonstrate good dynamic stability, focus, and concentration on dual tasks, without complaint of headaches. Progressions included performing stability exercises on an unstable surfaces with eyes closed then opening upon verbal command to perform reaction training, which consisted of reaching within and outside base of support towards the location of the laser target (Table 2). Exercises could be made more sports specific by having the athlete balance on a snowboard while performing exercises that challenge the components of the balance system (Figure 3). Perturbations were added if the athlete was able to maintain postural control while performing dual tasks. These exercises were added to the athlete's home program. She was advised to complete them daily using a pen light which was provided for reaction training with the assistance of a family member while following the parameters and suggested progressions listed in Table 2.
Figure 2.
Visual tracking exercises using laser pointer to provide a target.
Figure 3.
Sport specific balance training using snowboard on BOSU™.
The last phase of the rehabilitation program included plyometric exercises with reaction training to incorporate the dynamic components of jumping and landing in the sport of snowboarding while addressing deficits in reaction timing (Table 2). The athlete was instructed on proper landing mechanics during forward and lateral jumps with double foot contact. Jumps were performed to either verbal or visual command. Visual commands would include either laser pointer or hand‐direction. Previously mentioned neurocognitive retraining exercises were also integrated during this phase. Progressions would include multi‐directional and single‐leg jumps with verbal and visual cues (Figures 4,5). The reaction training component was advanced by giving conflicting cues such as pointing left while giving a verbal command of “forward” when the athlete was instructed to follow the verbal command. The athlete was advised to perform the plyometric exercises in her home program three times per week under the supervision of a certified strength and conditioning specialist at her local snowboard club while continuing to independently perform word recall and dynamic balance/reaction training activities daily.
Figure 4.
Example jumping exercises, medial/lateral.
Figure 5.
OUTCOMES
The athlete was seen for a total of 4 visits over the course of six weeks before relocating back to the east coast for the summer season. After six weeks, the athlete completed a follow‐up ImPACT test in the clinic. A lower composite score in the reaction time category indicates an overall quicker response to written and visual cues on the ImPACT test. The visual motor speed composite score is determined by scores on both the memory and reaction time tasks with a higher composite score indicating improved performance. Verbal and visual memory tasks are scored 0‐100 with 100 being a better score. The subject improved in both reaction time and visual processing with scores of .51 and 43.18, respectively, compared to .56 and 42.33 from baseline testing which indicates improvement in both categories (Table 1). There was only slight improvement in verbal memory scores with a lower score on visual memory. This indicates that a greater emphasis on verbal and visual memory activities may have been needed in her daily home program moving forward as well as an increased frequency of physical therapy visits to address these remaining deficits. She still reported symptoms of headaches from reading for more than 20 minutes and when in noisy environments, though not as frequent, and deficits in concentration despite an increased subjective confidence rating. She demonstrated decreased errors on her follow‐up BESS test but error score remained elevated which indicates continued vestibular rehabilitation and improved balance scores would be needed before the subject could return to sport. At that time, the subject had not been released by her family physician for participation in snowboarding or contact sports activities due to continued symptoms and was advised to follow‐up prior to snowboard season for reassessment. She was instructed to continue with her advanced home program in order to improve balance and memory deficits.
DISCUSSION
Proper management of a concussion requires gathering a thorough medical history, a complete subjective report of symptoms, and the use of neurocognitive testing baseline measures in order to determine neurocognitive deficits. Testing environment where a neurocognitive test is administered must be considered. In this case, testing was performed in a quiet, closed‐door environment in a sports medicine clinic. Completion of the ImPACT test in a noisy, crowded environment or in an athlete's home setting, where distractions from unmonitored cell phone or television use could affect reliability and validity of testing results, is not recommended. ImPACT testing should not be the primary source of information when determining the return to play status in athletes following concussion. Information gathered from neurocognitive testing should be integrated with a program that includes gradual progression in aerobic and sports specific activities as outlined in the National Athletic Trainer's Association position statement on management of sport‐related concussion to determine if an athlete is ready for return to sport.22 In addition, it is recommended that athletes undergo baseline neurocognitive testing before each competitive season prior to an incidence of concussion, especially in adolescents whose cognitive development is likely to vary significantly from season to season. In this case study, the subject completed a pre‐season baseline neurocognitive test eighteen months prior to her most recent concussion as baseline measures were gathered every two years for athletes within this subject's age group. These baseline test results were not available or provided by the subject.
Proper fitting equipment and helmet use also play an important role in reducing the risk for traumatic brain injury and possibly decreasing the severity of a concussion. In cases of traumatic head injury, helmet use by injured snowboarders has been poorly documented.11 However, several studies indicate reduced risk for severe head injury when a helmet is worn.12,14,29 Sulheim et al found a 60% reduction in brain injury risk when a helmet was worn in the ski and snowboard population.12 Similarly, helmet use has been shown to significantly reduce the risk of severe or traumatic head injury in the biking and motorcycling populations where the combination of high velocity and falls onto hard surfaces are common.30,31 While this does not imply that a concussion can be prevented when wearing a helmet, it would be prudent to advise snowboard athletes, as well as those that participate in sports involving aerial maneuvers and/or high velocity activities such as skateboarding, freestyle skiing, or motorcycling, to wear a helmet given the possibility of sustaining a head injury when participating in their sport or activity. Educating coaches and parents on the importance of helmet use is also advised.
While incorporating balance, neurocognitive retraining, and reaction training progressions, the medical practitioner should be sensitive to overloading the sensory and motor systems. Integrating excessive stimuli in an athlete during post‐concussion rehab may result in increased symptoms and delay rehab progressions attempted through dual task training. Slowed reaction time during these activities should be expected as attention is divided between balance and cognitive tasks with postural control being prioritized.32,33 In this case report, exercises were only progressed as tolerated and if the subject demonstrated the ability to maintain postural control while successfully completing dual tasks challenging the visual, somatosensory and vestibular components of the balance system.
In this case report, the subject's reaction time composite score was above the previously established cut‐off which may indicate a predisposition to musculoskeletal injury that may have contributed to her recent concussion given the athlete reported an injury to her low back and cervical spine one week prior. Her medical history also indicates a prior surgery to her right lower extremity. With this being said, gathering of a thorough medical history should include considerations of both orthopedic injury and concussion history. Also, given the indication from previous research that musculoskeletal injury risk may be increased following a concussion, it would be prudent to assess both neurocognitive function and functional movement patterns. Following assessment, implementation of an appropriate musculoskeletal and neurocognitive training program which addresses these risk factors would be beneficial before returning an athlete to sport following a concussion. Additional research which further investigates the combined integration of neurocognitive and musculoskeletal training programs within post‐concussion rehabilitation programs may be beneficial in addressing various deficits which may put athletes returning to sport to quickly at risk for injury.
Return to sport decision making should address the psychological components of injury and the rehabilitation process. Subjective ratings of confidence and use of questionnaires to identify functional limitations, in addition to symptom checklists, balance scores, neurocognitive testing, and response to activity progressions, should assist in guiding return to sport decision making following a concussion. An athlete's decreased levels of confidence in returning to sport could be indicative of psychological limitations associated with perceived negative life events such as previous injury or personal stress. If an athlete returns to sport too quickly without his or her psychological limitations being addressed, injury may result due to a narrowing of peripheral vision as well as subsequent delays in visual processing and reaction timing in response to environmental stimuli.34,35
Limitations of this case include reassessment after only four treatment sessions and a program length of six weeks due to athlete relocation. In addition, baseline ImPACT testing results closer to the time of her most recent concussion episode were lacking. Outcomes of this case report are of a single subject only and cannot be applied with confidence to other athletes or athletic populations.
CONCLUSIONS
This case report presents an integrated rehabilitation program that specifically addresses neurocognitive deficits that are identified on ImPACT testing following concussion. A program which incorporates dual‐task training by combining balance and reaction training activities may improve both balance and neurocognitive function in the categories of reaction timing and visual motor speed processing, based upon the findings of this case report. Future research should investigate the benefits of a combined neurocognitive and balance training program over a longer period of time as well as the effectiveness of computer‐based and visual training activities as they relate to improving both short and long‐term memory, visual processing, and reaction timing in athletes following a concussion. Additionally, more research is needed investigating the risk for concussion in sports such as snowboarding, freestyle skiing, skateboarding and motorbiking which combine high velocity with aerial stunts and tricks.
Acknowledgments
The author acknowledges the contributions of Kevin Heinz from Vail Valley Medical Center for his assistance in obtaining photographs of exercises demonstrated in this case report.
Appendix 1
REFERENCES
- 1.Gilchrist J Thomas K Xu L, et al. Nonfatal sports and recreation related traumatic brain injuries among children and adolescents treated in emergency departments in the United States, 2001‐2009. MMWR 2011: 60;1337‐134221976115 [Google Scholar]
- 2.Gessel L Fields S Collins C, et al. Concussions among United States high school and collegiate athletes. J Athl Train 2007;42:495‐503 [PMC free article] [PubMed] [Google Scholar]
- 3.Marar M McIllvain N Fields S, et al. Epidemiology of concussions among United States high school athletes in 20 sports. Am J Sports Med 2012; 40:747‐755 [DOI] [PubMed] [Google Scholar]
- 4.Meehan W d'Hemecourt P Comstock R High school concussions in the 2008‐2009 academic year: mechanism, symptoms, and management. Am J Sports Med 2010;38:2405‐2409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bladin C McCrory P Pogorzelski A Snowboarding injuries. Sports Med 2004;34:133‐138 [DOI] [PubMed] [Google Scholar]
- 6.Davidson T Laliotis A Snowboarding injuries: a four‐year study with comparison with alpine ski injuries. West J Med 1996;164:231‐237 [PMC free article] [PubMed] [Google Scholar]
- 7.Dohjima T Sumi Y Ohno T, et al. The dangers of snowboarding: a 9‐year prospective comparison of snowboarding and skiing injuries. Acta Orthop 2001;72:657‐660 [DOI] [PubMed] [Google Scholar]
- 8.Idzikowski J Janes P Abbott P Upper extremity snowboarding injuries: ten‐year results from the Colorado snowboard injury survey. Am J Sports Med 2000;28:825‐832 [DOI] [PubMed] [Google Scholar]
- 9.Langran M Selvaraj S Snow sports injuries in Scotland: a case‐control study. Br J Sports Med 2002;36:135‐140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Macnab A Smith T Macnab M Effect of helmet wear on the incidence of head/face and cervical spine injuries in young skiers and snowboarders. Inj Prev 2002;8:324‐327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McBeth P Ball C Mulloy H, et al. Alpine ski and snowboarding traumatic injuries: incidence, injury patterns and risk factors for 10 years. Am J Surg 2009;197:560‐564 [DOI] [PubMed] [Google Scholar]
- 12.Sulheim S Holme I Ekeland A, et al. Helmet use and risk of head injuries in alpine skiers and snowboarders. JAMA 2006;295:919‐924 [DOI] [PubMed] [Google Scholar]
- 13.Fountain J Meyers M Skateboarding injuries. Sports Med 1996;22:360‐366 [DOI] [PubMed] [Google Scholar]
- 14.Wilkerson G Neurocognitive reaction time predicts lower extremity sprains and strains. Int J Athl Ther Train 2012;17:4‐9 [Google Scholar]
- 15.Swanik C Covassin T Stearne D, et al. The relationship between neurocognitive function and noncontact anterior cruciate ligament injuries. Am J Sports Med 2007;35:943‐948 [DOI] [PubMed] [Google Scholar]
- 16.Iverson G Gaetz M Lovell M, et al. Relation between subjective fogginess and neuropsychological testing following concussion. J Int Neuropsych Soc 2004;10:904‐906 [DOI] [PubMed] [Google Scholar]
- 17.Schatz P Pardini J Lovell M, et al. Sensitivity and specificity of the ImPACT Test Battery for concussion in athletes. Arch Clin Neuropsych 2006;21:91‐99 [DOI] [PubMed] [Google Scholar]
- 18.Lovell M Collins M Iverson G, et al. Recovery from mild concussion in high school athletes. J Neurosurg 2003;98:296‐301 [DOI] [PubMed] [Google Scholar]
- 19.Gagnon I Galli C Friedman D, et al. Active rehabilitation for children who are slow to recover following sport‐related concussion. Brain Injury 2009;23:956‐964 [DOI] [PubMed] [Google Scholar]
- 20.Jacobson G Newman C The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg 1990;116:424‐427 [DOI] [PubMed] [Google Scholar]
- 21.Guskiewicz K Ross S Marshall S Postural stability and neuropsychological deficits after concussion in collegiate athletes. J Athl Train 2001;36:263‐273 [PMC free article] [PubMed] [Google Scholar]
- 22.Guskiewicz K Bruce S Cantu R, et al. National Athletic Trainers’ Association Position Statement: Management of Sport‐Related Concussion. J Athl Train 2004;39:280‐297 [PMC free article] [PubMed] [Google Scholar]
- 23.Riemann B Guskiewicz K Shields E Relationship between clinical and forceplate measures of postural stability. J Sport Rehabil 1999;8:71‐62 [Google Scholar]
- 24.Iverson G Koehle M Normative data for the Balance Error Scoring System in adults. Rehab Res Pract 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McLeod B Effects of Eyerobics visual skills training on selected performance measures of female varsity soccer players. Perceptual and Motor Skills 1991;72: 863‐866 [Google Scholar]
- 26.Broglio S Tomporowski P Ferrara M Balance performance with a cognitive task: a dual‐task testing paradigm. Med Sci Sports Exerc 2005;37:689‐695 [DOI] [PubMed] [Google Scholar]
- 27.Gillen G Cognitive and Perceptual Rehabilitation: Optimizing Function. St Louis, MO: Mosby Inc; 2009 [Google Scholar]
- 28.Neistadt M Perceptual retraining for adults with diffuse brain injury. Am J Occup Ther 1994;48:225‐233 [DOI] [PubMed] [Google Scholar]
- 29.Hagel B Pless I Goulet C, et al. Effectiveness of helmets in skiers and snowboarders: case‐control and case crossover study. Br J Sports Med 2005;330:281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Davidson J Epidemiology and outcome of bicycle injuries presenting to an emergency department in the United Kingdom. Eur J Emerg Med 2005;12:24‐29 [DOI] [PubMed] [Google Scholar]
- 31.Liu B Ivers R Norton R Boufous S Blows S Lo S Cochrane Database Syst Rev 2008;1 [DOI] [PubMed] [Google Scholar]
- 32.Resch J May B Tomporowski P, et al. Balance performance with a cognitive task: a continuation of the dual‐task testing paradigm. J Athl Train 2011; 46:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teel E Register‐Mihalik J Blackburn J, et al. Balance and cognitive performance during a dual‐task: preliminary implications for use in concussion assessment. J Sci Med Sport 2013;16:190‐194 [DOI] [PubMed] [Google Scholar]
- 34.Andersen M Williams J Athletic injury, psychosocial factors and perceptual changes during stress. J Sports Sci 1999;17:735‐741 [DOI] [PubMed] [Google Scholar]
- 35.Williams J Andersen M Psychosocial influences on central and peripheral vision and reaction time during demanding tasks. Behav Med 1997;22:160‐167 [DOI] [PubMed] [Google Scholar]