Abstract
There is a growing interest in musculoskeletal rehabilitation for young active individuals with non‐arthritic hip pathology. History and physical examination can be useful to classify those with non‐arthritic intra‐articular hip pathology as having impingement or instability. However, the specific type of deformity leading to symptoms may not be apparent from this evaluation, which may compromise the clinical decision‐making. Several radiological indexes have been described in the literature for individuals with non‐arthritic hip pathology. These indexes identify and quantify acetabular and femoral deformities that may contribute to instability and impingement. The aim of this paper is to discuss clinical indications, methods, and the use of hip radiological images or radiology reports as they relate to physical examination findings for those with non‐arthritic hip pathology.
Level of evidence:
5
Keywords: Examination, Femoroacetabular impingement (FAI), imaging, labrum
INTRODUCTION
There is a growing interest in musculoskeletal rehabilitation for young active individuals with non‐arthritic hip pathology. Physical therapists generally base their assessment of those with hip pathology on history and physical examination.1 However, bony abnormalities may influence the patient's prognosis and therefore may need to be identified. When abnormalities of bone morphology are present, direct repercussions on the biomechanics of the hip and adjacent joints can occur.2 Several radiological indexes have been described in the literature for individuals with non‐arthritic hip pathology.3,4 The aim of this paper is to discuss clinical indications, methods, and interpretation of hip radiological images as they relate to physical examination findings for those with non‐arthritic hip pathology.
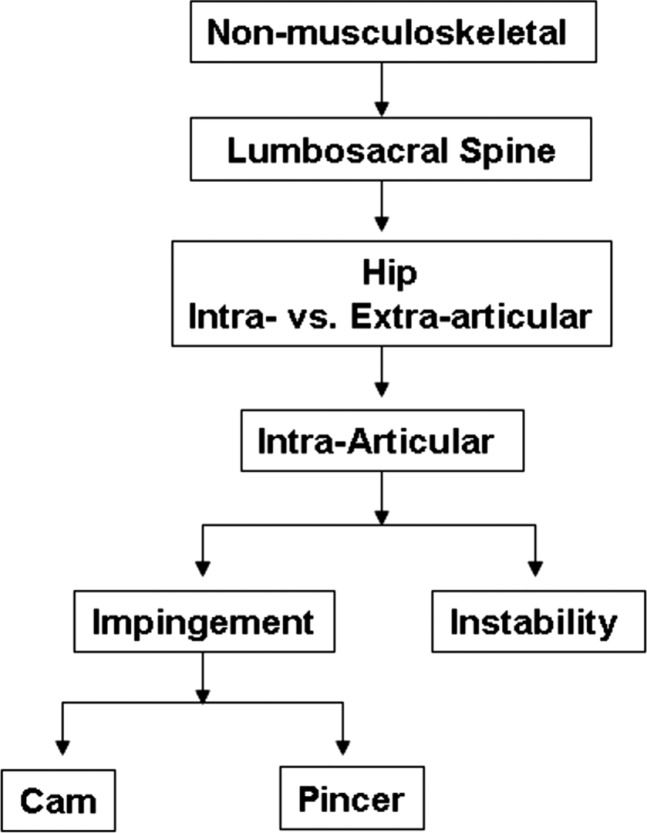
There are a limited number of evaluation algorithms for those with hip related symptoms. An evaluation algorithm and classification based treatment system have recently been described to guide physical therapists in the management of individuals with hip pain, including those with non‐arthritic related pathology.5,6 This evaluation includes considerations for non‐musculoskeletal, lumbosacral spine, extra‐articular, and intra‐articular sources of pain. Intra‐articular pathologies for individuals with non‐arthritic hip pain are further classified as impingement and hypermobility as outlined in Figure 1. While evidence to support the use of this algorithm is lacking it does relate to relevant non‐arthritic radiographic abnormalities that have been described.
Figure 1.
Evaluation algorithm for young active individuals.
History and physical examination are commonly used to assess for non‐musculoskeletal and lumbosacral spine pathology as potential sources of hip pain as described in detail elsewhere.5‐12
Once non‐musculoskeletal and lumbar spine pathology are ruled out as potential sources of hip pain, the clinician must determine if there is an intra‐ and/or extra‐articular source of symptoms. The Flexion‐Abduction‐External Rotation (FABER), Internal Range of Motion with Over‐Pressure (IROP), and Scour tests may be useful in this capacity.13‐15 The FABER and IROP tests have sensitivity values in identifying individuals with intra‐articular pathology of 0.82 and 0.91, respectively.14
The Scour test has sensitivity values ranging between 0.62 and 0.91 in identifying those with intra‐articular pathology.13,15 Extra‐articular pain generators, such as musculotendinous pathologies, should not be provoked with the FABER, IROP, and Scour tests. Musculotendinous pathologies, including muscle strains and/or tendon disorders, should be painful with palpation, stretching, and resisted movements directed at the involved muscle and/or tendon. If the source of pain is solely from intra‐articular origin, palpable pain is rarely present.16 If FABER, IROP, and Scour tests are positive, the source of pain is likely due to intra‐articular sources.7,17 Once it is determined that the source of pain is intra‐articular, additional tests can be conducted in order to further classify individuals into an impingement or hypermobility classification.
FEMOROACETABULAR IMPINGEMENT
Two types of femoroacetabular impingement (FAI) have been described; cam and pincer types.18 Cam impingement results from an abnormal bump, thickening, and/or loss of femoral‐head neck offset which can be localized anteriorly, superiorly, posteriorly, and/or inferiorly.19 Cam deformities cause labral compression and sheer forces leading to acetabular cartilage damage.19,20 The location of the deformity and direction of hip movement will determine the specific location of injury. A cam deformity at the anterior‐superior femoral head‐neck junction will compress the anterior‐superior labrum during the combined motion of hip internal rotation, flexion, and adduction. Posterior head‐neck deformities can cause posterior‐superior labral compression with hip external rotation and extension, while head‐neck deformities that are located superiorly can cause superior labral compression with hip abduction.21
Differing from cam impingement, pincer type impingement results from an acetabular deformity. Focal or global over coverage of the femoral head by the acetabulum are terms used to further describe pincer impingement.19 Superior focal over coverage results from the anterior and superior acetabular rim extending laterally over the femoral head. This deformity can cause the femoral head‐neck junction to abut the anterior‐superior labrum when the hip moves into internal rotation, flexion, and adduction.21 Excessive acetabular retroversion and anteversion are also potential causes of focal over coverage. Acetabular retroversion results in anterior over coverage but posterior under coverage of the femoral head. This anterior over coverage will cause the head‐neck junction to come into contact with anterior‐superior labrum when the hip is internally rotated in flexion. Conversely, acetabular anteversion causes posterior over coverage but anterior under coverage with the head‐neck junction abutting the posterior‐superior labrum in a position of hip external rotation and extension.21 Coxa profunda and protrusio are acetabular global over coverage deformities.19 Depending on the severity of the over coverage, labral damage from compression can occur in locations where the head‐neck junction comes into contact with the labrum. Acetabular deformities can also cause the femoral head to be levered out of the acetabulum and result in cartilage and/or labral pathology in a location opposite to the labral compression. These types of injuries are called ‘countra‐coup’ lesions.22,23
In addition to cam and pincer type FAI, mechanical impingement may be caused by rotational deformities of the femur in the transverse plane.24 The femoral head‐neck is normally rotated approximately 158 anteriorly. Decreased anteversion is noted when the femoral head‐neck is rotated less than 158. The anterior‐superior head‐neck junction will be closer to the anterior rim of the acetabulum when angle of anteversion is decreased. Therefore, movements that incorporate hip internal rotation in 30‐608 of flexion may cause the femoral head‐neck junction to compress the anterior‐superior labrum. Excessive femoral anteversion is said to be present when the femoral head‐neck is rotated greater than 158 anteriorly. When anteversion is greater than 308 the posterior head‐neck junction will be close to the posterior rim of the acetabulum and compress the posterior‐superior labrum with the femoral head‐neck junction with combined hip external rotation and extension.21
Prospective studies have demonstrated potential diagnostic indicators of FAI. These studies have found those with FAI commonly complain of an insidious onset of sharp or aching groin pain that limits activity.25,26 Those with FAI also have physical examination findings of limited hip flexion, internal rotation, and abduction range of motion and positive Flexion‐Adduction‐Internal Rotation Impingement (FADDIR) and FABER tests.4,27‐29
Special tests to identify the specific source of impingement as either anterior, superior, and/or posterior have been developed and include two dynamic impingement tests.30 The Dynamic Internal Rotation Impingement test (DIRI) circumducts the hip through an arc of flexion, adduction, and internal rotation in order to cause contact of the femoral head‐neck junction with the anterior and anterior‐superior rim of acetabulum.30 The dynamic external rotation impingement test (DEXTRI) circumducts the hip through an arc of extension, abduction, and external rotation in order to cause contact of the femoral head‐neck junction with the posterior and posterior‐superior rim of acetabulum.30 The position(s) that recreate the pinching pain can be used to identify the potential location of impingement.
While the DIRI and DEXTRI have been described to potentially assess for the source of Cam and Pincer impingements, Craig's test may be used to identify those with abnormal femoral version. This method involves positioning an individual prone and flexing the knee to 90 degrees. The greater trochanter is then palpated as the thigh is internally and externally rotated, until the greater trochanter is at its most prominent position laterally. Femoral anteversion is measured as the angle formed by the long axis of the lower leg and the vertical, and is quantified using a goniometer or inclinometer.31 A normal test is a position of 158 hip internal rotation when the greater trochanter is parallel to the floor/table. Individuals in a position of more than approximately 158 may be considered to have increased femoral anteversion, which would lead to a greater anterior exposure of the femoral head.
INSTABILITY
Labral‐chondral pathology can also be caused by either focal rotational or global hip laxity.32 Although there are many causes of instability27 in a young active population, localized laxity of ligamentous and capsular structures is commonly caused by excessive repetitive forceful hip rotation. This type of injury is defined as focal rotational instability.33‐35 The most common injury is iliofemoral ligament laxity caused by repetitive forceful hip external rotation beyond the limit of normal motion. Although less common, excessive internal rotation could potentially lead to ishiofemoral ligament laxity.30 Instability is usually combined with some form of acetabular undercover.36 This can be from acetabular anteversion, retroversion, or global under coverage. Although any malformation of the acetabular shape could be termed dysplasia, hip dysplasia is a term commonly associated with global under coverage resulting from a shallow acetabulum. Abnormal loading of the anterior‐superior labrum and subsequent labral‐chondral damage can occur with either focal rotational or global hip laxity.34,35,37 Regarding the femoral head neck deformities, coxa valgum may also lead to instability and abnormal loading of the superior labrum, thus contributing to labral‐chondral pathology(38,39).
The diagnosis of instability can be suspected when complaints of hip pain are associated with findings of hypermobility. Individuals may note movement dependent hip instability or apprehension. Clinically, range of motion measurements, the log roll test, and Beighton Scale can be used to assess for hypermobility. Hip range of motion measures that exceed established normative values or that are increased compared to the uninvolved side without the presence of an anteverted or retroverted femur should raise suspicion of hypermobility. Signs for select iliofemoral ligament laxity include increased hip external rotation but normal internal rotation range of motion.40 The log roll test specifically assesses rotational motion and is used to observe asymmetrical increases in internal and external rotation as well as quality of end‐feel.30 Excessive external rotation motion with softer than normal end‐feel would indicate iliofemoral ligament laxity. Additionally, the Beighton Scale can be used to identify those with general ligament laxity.41 Using this scale three or more of the following would indicate general ligament laxity: extension of the 2nd metacarpal phalangeal joint beyond 90°, flexion of the thumb to the forearm, extension of the knee beyond 10°, extension of the elbow beyond 10°, and palms touching the floor while bending at the waist.
History and physical examination can be useful to classify young active individuals with non‐arthritic hip pathology as having impingement or instability. However, the specific type of deformity leading to symptoms may not be apparent from this evaluation. For example, an individual may have signs and symptoms consistent with impingement, including a positive DIRI. While FAI would be suspected, the bony deformity being an anterior‐superior cam, acetabular retroversion, or global over coverage, may be difficult to determine solely from the physical examination. Also, prognosis for conservative care may be linked to the degree of boney deformity. An individual with signs and symptoms consistent with instability and excessive global acetabular under coverage may have a worse prognosis than an individual with similar signs and symptoms but only a slight degree of under coverage. Therefore, physical therapists may use the results of radiographic assessment of acetabulum and femur to help verify the classification; more precisely identify the type of bony deformity, and assist in determining a potential prognosis based on the degree of the deformity.17 While there are not absolute values that define how the degree of deformity will relate to prognosis, severe deformities are likely to be associated less favorable outcomes.
RADIOGRAPHIC ASSESSMENT
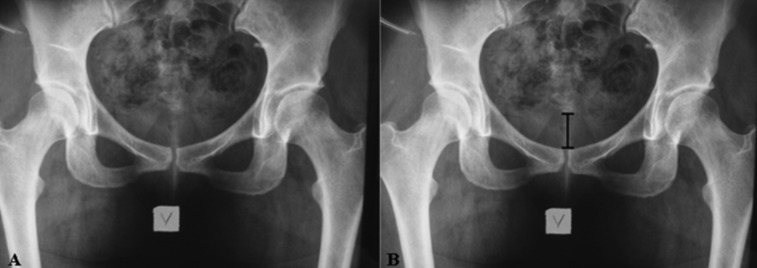
Radiographic examination is widely used because it is readily available, simple, and fairly inexpensive. However, as with any tool it must be performed properly. Standard conventional radiographic imaging for femoroacetabular investigation includes two radiographs: an anteroposterior (AP) view and an axial cross‐table view.4 Some alternatives to the axial view are the Ducroquet and Dunn radiographs and because they provide similar information which will not be discussed. In the case of an anteroposterior (AP) X‐ray, neutral rotation of the pelvis in the transverse plane is defined when the lower end of the coccyx is located perpendicular to the pubic symphysis (Figure 2). In relation to sagittal plane, neutral pelvic inclination is established when the distance between the coccyx and pubic symphysis is approximately 3 cm for men and 5 cm for women.4,42 Determining that the radiograph was taken with neutral pelvic inclination is critical and must be done before the radiograph can be interpreted. An AP radiograph that does not follow this standardization cannot reliably diagnose boney deformities of the hip joint.4 The cross‐table radiograph is performed with the hip in neutral position or internally rotated at 15 degrees in order for the femoral neck‐head junction to be appropriately visualized.43
Figure 2.
Anteroposterior X‐ray of the pelvis in neutral position (A). The black line indicates the distance between the coccyx and the public symphysis. The acceptable distance is considered to be between 3 and 5 cm (B).
ACETABULAR CONDITIONS
Acetabular depth
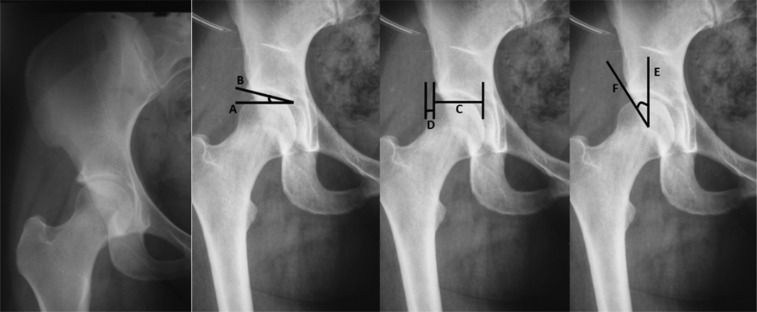
The AP radiograph can be used to identify abnormal acetabular morphology in terms of focal or global over or under coverage (Figure 3). There are a number of indexes that can be used to assist in quantifying acetabular depth and include acetabular index (also known as acetabular roof angle), femoral head extrusion index and lateral center edge angle of Wiberg.44,45
Figure 3.
A) Anteroposterior X‐ray of a normal hip; B) Acetabular index–angle formed by a horizontal line (line A) and a line connecting the medial point of the sclerotic zone with the lateral edge of the acetabulum (line B); C) Femoral head extrusion index–line C corresponding to the connection of both extremities of the acetabulum esclerotic zone and line D corresponding to the connection of the femoral head‐neck junction and the sclerotic zone of the acetabulum; and D) Lateral center edge angle of Wiberg–a vertical line from the femoral head center (line E) and a line connecting the femoral head center with the lateral edge of the acetabulum (line F).
The acetabular index in the AP X‐ray (Figure 3) is determined by making a horizontal line from the most medial point of the sclerotic zone of the acetabulum (line A). Another line is placed from this same point to the lateral edge of acetabulum (line B). When the angle formed by these two lines is equal or less than 08 superior focal over coverage of the acetabulum is suggested.46
The femoral head extrusion index (Figure 3) is determined by measuring the distance between a vertical line over the most medial point of the sclerotic zone of the acetabulum and a vertical line over the lateral most edge of the acetabulum. The distance between these two lines in the frontal plane corresponds to line A. Another vertical line is placed from the femoral head‐neck junction and the distance between this point and the vertical line over the lateral edge of the acetabulum corresponds to line B. The distance of line B is then divided by the distance of lines A+B and a percentage is created. This index defines the percentage of the femoral head that is without acetabular coverage. Femoral head extrusion index greater than 25% would indicate global undercoverage.19,44
The lateral center edge angle of Wiberg (Figure 3) is created between a vertical line from the center of the femoral head (line A) and a line connecting the center of the femoral head with the lateral edge of the acetabulum (line B). The angle formed is normally between 25° and 39°. Values less than 25° indicate global acetabular under coverage where values above 39° indicate superior focal over coverage or excessive global acetabular over coverage.24,44‐47
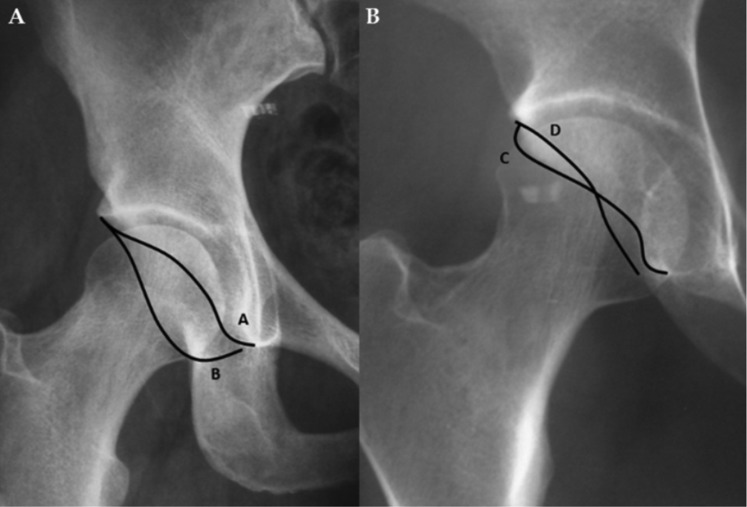
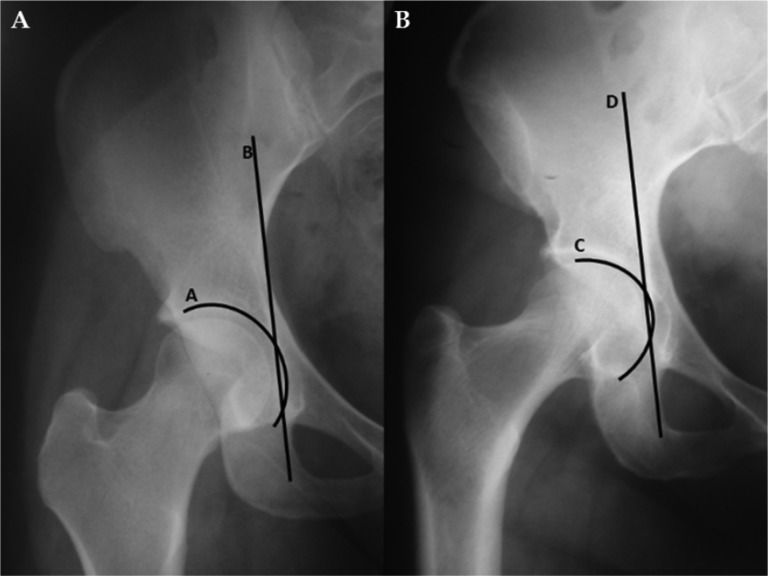
As previously noted, excessive acetabular retroversion and anteversion result in focal over coverage in one direction and under coverage in the opposite. An increased anterior wall characterizes an acetabular retroversion and is detected by the cross‐over sign in an AP X‐ray of the hip. In those with anatomically normal acetabular anteversion, the edge of the anterior wall (line A) is visualized medially in relation to the posterior wall (line B) (Figure 4). In the case of an acetabular retroversion, the anterior wall is more lateral than the posterior wall and then crosses it medially and noted as a positive cross‐over sign (Figure 4).42,44,48
Figure 4.
Anterosposterior X‐ray of normal hip (A)–anterior wall (line A) being projected more medially than posterior wall (line B); Acetabular retroversion (B)–anterior wall (line C) being more lateral than posterior wall (line D), i.e., showing a crossover sign.
Coxa profunda and protrusio as noted are acetabular deformities that cause global over coverage. Coxa profunda is defined radiographically when the tear‐dropped shaped articular surface of the acetabulum lies medial to the ilioischial line from an anterior‐posterior view. Protrusio refers to a medialization of the femoral head position within the acetabulum.19,49 In the AP image, the line traced over the medial wall of the acetabulum (line A) would normally be visualized laterally to the ilioischial line (line B). When line A touches or surpasses line B, it is classified as a coxa profunda.4 The protrusio index is determined by tracing a line over the medial extremity of the femoral head (line C), which would normally be visualized laterally to the ilioischial line (line B). When the line over the femoral head surpasses the ilioischial line medially, this is classified as acetabular protrusio (Figure 5).4,50
Figure 5.
Anterosposterior X‐ray–A) The acetabular fossa line (line A) overlapping the ilioischial line medially (line B), indicating a coxa profunda; and B) The femoral head line (line C) touching or overlapping the ilioischial line medially (line D), indicating an acetabulum protusio.
Evidence for interpretation of acetabular deformities
Several authors have discussed the validity of these indices, as well as the frequency at which they are found in symptomatic and asymptomatic populations. When those with a surgically identified labral tear were compared to controls, Peelle et al51 found a larger acetabular index (9.6° vs 6.2°; p=0.02), but no difference in lateral center edge angle of Wiberg and acetabular retroversion. The Wiberg angle and retroversion may better correlate to the presence of osteoarthritis.52 A Wiberg angle higher than 45°, i.e., a deep acetabular socket, was considered a risk factor for hip osteoarthritis.53 Corroborating this information, Ezoe et al54 showed that subjects with osteoarthritis were more likely to have acetabular retroversion than are normal subjects. Radiographic acetabular retroversion was present in 20% of patients with hip osteoarthritis compared to 5‐7% among the general population.
FEMORAL CONDITIONS
Cam quantification
The cam type impingement is identified in the cross‐table radiographic views and quantified by measuring the alpha angle and anterior offset distance.22,44,55 Figure 6 displays the measurement of the alpha angle. The circumference of the femoral head is first outlined. Then, a line is traced (A) from the center of the femoral head towards the central neck region. Another line (B) is traced from the center of the femoral head to the point where the neck ends and the sphericity of the femoral head begins. The angle formed by the two lines is normally less than 50°.4,28,56,57 Values greater than 50° indicate an enlarged anterior‐superior femoral head‐neck junction. A greater alpha angle has been also identified in those with clinical signs of impingement,58 labral tears,28,51,59 acetabular rim chondral defects, and osteoarthritis28 when compared to asymptomatic controls.
Figure 6.
Cross‐table X‐ray of the right hip (A); Alpha angle (B)–circumference of the femoral head; line A which connects the head center of the femoral neck and line B connecting the head center witht the point of beginning asphericity of the head‐neck junction. An angle exceeding 50° is an indicator of an abnormally shaped femoral head‐neck junction; Anterior offset (C)–two horizontal lines touching the anterior femoral head (line C) and femoral head‐neck junction (line D). The distance between both lines corresponds to the anterior offset (line E).
The femoral anterior offset distance (Figure 6) is an index that is defined by the distance between the anterior the femoral head and anterior femoral neck. This distance is measured between a horizontal line at the most superior point of the femoral head (line A) and another horizontal line at the point where the femoral head ends and the neck begins (line B). The perpendicular distance (line C) between the two lines is the anterior femoral offset distance. An offset less than 10 mm also indicates an enlarged anterior‐superior femoral head‐neck junction.4,44,57
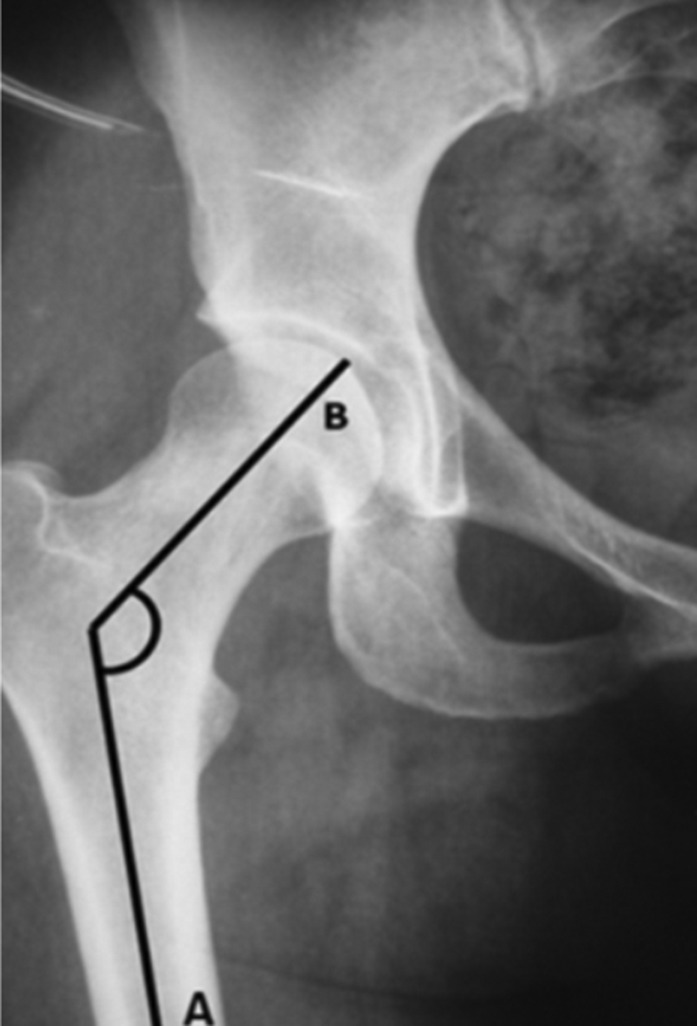
Cervico‐diaphyseal angle
The femoral neck is tilted upwards in relation to the diaphysis of the femur at an angle of approximately 125° during adulthood. This cervico‐diaphyseal angle can be determined by an AP radiograph. It is the angle formed by the axis of the femoral shaft (line A) and a line drawn along the axis of the femoral neck passing through the femoral head center (line B) (Figure 7).3,60 If a subject exhibits a cervico‐diaphyseal angle less than 120°, it is classified as coxa vara, whereas an angle greater than 130° is classified as a coxa valga61 Coxa vara is thought to be associated with instability and coxa valga associated with anterior superior labral tears.
Figure 7.
Cervico‐diaphyseal angle–it is the angle formed by the axis of the femoral shaft (line A) and the line a drawn along the axis of the femoral neck passing through the femoral head center (line B).
Evidence for Interpretation of Femoral Deformities
An alpha angle higher than 50.5° had sensitivity and specificity values of 72% and 100%, respectively, in identifying those with clinical signs of impingement from controls.55 Patients with a clinical exam consistent with FAI showed a significant reduction in head‐neck offset in the lateral and anterior aspect of the femoral neck.62 However it is important to highlight that this study used an MRI‐assessment.
INTEGRATION OF CLINICAL AND RADIOGRAPHIC ASSESSMENT
It is important to highlight the necessity of using radiographs in conjunction with physical exam finding because the imaging findings are not always related to the presence of pain, and vice‐versa. A summary relating the sign, radiographic measures and interpretation can be found in Table 1. Related to acetabular conditions, a recent study conducted by Kang et al63 evaluated 100 hips in asymptomatic population and found an increased Wiberg angle in 16%, acetabular retroversion in 14%, and positive cross‐over sign in 20% of subjects. Moreover, Tannast et al4 evaluated the cross‐over sign in 55 patients with FAI and it was present in only 53% of hips. Although, the cross‐over sign had a sensitivity of 71% and specificity of 88% for hip impingement, the authors noted that this sign by itself was not enough to diagnose FAI. Similarly, femoral changes found in radiological analysis are not sufficient to ensure the presence of pain or functional deficits. Kang et al63 also found an increased alpha angle in 10% of the hips and changes in the femoral head sphericity in 74% of asymptomatic population. In clinical terms, the bone abnormalities may provoke pain by causing repetitive microtrauma in the hip joint, especially in subjects with abnormal movement patterns of lower limbs during physical activity of functional tasks.4,21,61,64‐66 Clinicians should be aware of the large number of false positive findings associated with the radiographic measures discussed in the paper. This exemplifies the notion that radiographic findings must be used in conjunction with history and clinical examination in order to be properly interpreted.
TABLE 1.
Physical Exam Findings, Radiographic Findings, and Interpretation in Young Active Individuals with Non‐Arthritic Hip Pain
| Physical Exam Findings | Radiographic Findings | Interpretation |
|---|---|---|
| Femoroacetabular Impingement | ||
| + DIRI and ↓IR ROM | Acetabular Index >0° Lateral Center Edge Angle of Weiberg >39° | Anterior Superior Acetabular Overcoverage |
| Cross‐over Sign | Acetabular Retroversion | |
| Alpha Angle >50° Femoral Anterior Offset <10mm | Anterior Superior Cam | |
| + DEXTRI and ↓ER ROM | Edge of the Anterior Acetabular Wall Excessively Medial to the Posterior Wall | Acetabular Anteversion |
| + DEXTRI/DIRI and ↓ER and IR ROM | Medial Wall of the Acetabulum Touches or Surpasses Ilioischial Line | Acetabular Profunda |
| Medial Aspect of the Femoral Head Surpasses the llioischial Line Medially | Acetabular Protrusio | |
| Instability | ||
| Apprehension and ↑ ER and IR ROM | Femoral Head Extrusion Index > 25% | Global Undercoverage |
| Lateral Center Edge Angle of Weiberg < 25° | ||
| Apprehension with ER ROM | Edge of the anterior acetabular wall excessively medial to the posterior wall | Acetabular Anteversion |
| Apprehension with IR ROM | Cross‐over Sign | Acetabular Retroversion |
+ positive; ↓ decrease; ↑ increase; ROM range of motion; IR internal rotation; ER external rotation; DIRI dynamic internal rotation impingement test; DEXTRI dynamic external rotation impingement test
CONCLUSION
History and physical examination can be useful to classify young active individuals with non‐arthritic intra‐articular hip pathology as having impingement or instability. However, the specific type of deformity leading to symptoms may not be apparent from this evaluation. Several radiological indexes have been described in the literature for individuals with non‐arthritic hip pathology. The paper outlines the clinical indications, methods, and interpretation of hip radiological images as it relates to physical examination findings for those with non‐arthritic hip pathology.
REFERENCES
- 1.Martin RL Sekiya JK The interrater reliability of 4 clinical tests used to assess individuals with musculoskeletal hip pain. J Orthop Sports Phys Ther. 2008;38(2):71‐7 [DOI] [PubMed] [Google Scholar]
- 2.Pfirrmann CWA Mengiardi B Dora C Kalberer F Zanetti M Hodler J Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006: 240(3): 778‐85 [DOI] [PubMed] [Google Scholar]
- 3.Robertson DD Britton CA Latona CR Armfield DR Walker PS Maloney WJ Hip Biomechanics: Importance to Functional Imaging. Semin Musculoskelet Radiol. 2003;7(1):27‐41 [DOI] [PubMed] [Google Scholar]
- 4.Tannast M Siebenrock KA Anderson SE Femoroacetabular Impingement: radiographic diagnosis ‐ what the radiologist should know. AJR. 2007;188:1540–52 [DOI] [PubMed] [Google Scholar]
- 5.Kivlan BR Martin RL Classification‐based treatment of hip pathology in older adults. Topics Ger Rehab. 29:218‐226; 2013 [Google Scholar]
- 6.Martin RL Enseki KR: Nonoperative Management and Rehabilitation of the Hip. In: Sekiya JK Safran M Ranawat A Leunig M eds. Techniques in Hip Arthroscopy and Joint Preservation Surgery. Philadelphia PA: Elsevier; 67‐73; 2010 [Google Scholar]
- 7.Goodman CC Snyder TEK Differential Diagnosis for Physical Therapists. Screeing fro Referral. 4th ed. 2007, Philadelphia, PA: Saubders Elsevier [Google Scholar]
- 8.Brown MD Gomez‐Marin O Brookfield KF Li PS Differential diagnosis of hip disease versus spine disease. Clin Orthop Relat Res. 2004;(419)(419):280‐284 [DOI] [PubMed] [Google Scholar]
- 9.Fritz JM Cleland JA Childs JD Subgrouping patients with low back pain: Evolution of a classification approach to physical therapy. J Orthop Sports Phys Ther. 2007;37(6):290‐302 [DOI] [PubMed] [Google Scholar]
- 10.Laslett M Young SB Aprill CN McDonald B Diagnosing painful sacroiliac joints: A validity study of a McKenzie evaluation and sacroiliac provocation tests. Aust J Physiother. 2003;49(2):89‐97 [DOI] [PubMed] [Google Scholar]
- 11.Maher C Adams R Reliability of pain and stiffness assessments in clinical manual lumbar spine examination. Phys Ther. 1994;74(9):801‐9; discussion 809‐11. [DOI] [PubMed] [Google Scholar]
- 12.Sugioka T Hayashino Y Konno S Kikuchi S Fukuhara S Predictive value of self‐reported patient information for the identification of lumbar spinal stenosis. Fam Pract. 2008;25(4):237‐244. 10.1093/fampra/cmn031. [DOI] [PubMed] [Google Scholar]
- 13.Leunig M Werlen S Ungersbock A Ito K Ganz R Evaluation of the acetabular labrum by MR arthrography. J Bone Joint Surg Br. 1997;79:230‐4 [DOI] [PubMed] [Google Scholar]
- 14.Maslowski E Sullivan W Forster Harwood J, et al. The diagnostic validity of hip provocation maneuvers to detect intra‐articular hip pathology. PM & R J Injury, function, and rehabilitation. 2010;2:174‐81 [DOI] [PubMed] [Google Scholar]
- 15.Sutlive TG Lopez HP Schnitker DE, et al. Development of a clinical prediction rule for diagnosing hip osteoarthritis in individuals with unilateral hip pain. J Orthop Sports Phys Ther. 2008;38:542‐50 [DOI] [PubMed] [Google Scholar]
- 16.Cacchio A Borra F Severini G Foglia A Musarra F Taddio N De Paulis F Reliability and validity of three pain provocation tests used for the diagnosis of chronic proximal hamstring tendinopathy. Br J Sports Med. 2012;46(12):883‐7 [DOI] [PubMed] [Google Scholar]
- 17.Martin HD Clinical examination of the hip. Oper Tech Orthop. 2005;15:177‐81 [Google Scholar]
- 18.Ganz R Parvizi J Beck M Leunig M Notzli H Siebenrock KA Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112‐20 [DOI] [PubMed] [Google Scholar]
- 19.Ganz R Leunig M Leunig‐Ganz K Harris WH The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264‐72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anderson LA Peters CL Park BB Stoddard GJ Erickson JA Crim JR Acetabular cartilage delamination in femoroacetabular impingement. Risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg Am. 2009;91:305‐13 [DOI] [PubMed] [Google Scholar]
- 21.Klingenstein GG Martin R Kivlan B Kelly BT Hip injuries in the overhead athlete. Clin Orthop Relat Res. 2012;470:1579‐85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beck M Kalhor M Leunig M Ganz R Hip morphology influences the pat‐tern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012‐8 [DOI] [PubMed] [Google Scholar]
- 23.Beck M Leunig M Parvizi J Boutier V Wyss D Ganz R Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67‐73 [PubMed] [Google Scholar]
- 24.Tonnis D Heinecke A Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747‐70 [DOI] [PubMed] [Google Scholar]
- 25.Anderson SE Siebenrock KA Tannast M Femoroacetabular impingement. Eur J Radiol. 2012;81(12):3740‐4 [DOI] [PubMed] [Google Scholar]
- 26.Banerjee P Mclean CR Femoroacetabular impingement: a review of diagnosis and management. Curr Rev Musculoskelet Med. 2011;4:23‐32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clohisy JC Knaus ER Hunt DM Lesher JM Harris‐Hayes M Prather H Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467:638‐44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnston TL Schenker ML Briggs KK Philippon MJ Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy. 2008;24:669‐75 [DOI] [PubMed] [Google Scholar]
- 29.Philippon MJ Maxwell RB Johnston TL Schenker M Briggs KK Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007; 15(7):908‐14 [DOI] [PubMed] [Google Scholar]
- 30.Martin HD Shears SA Palmer IJ Evaluation of the hip. Sports Med Arthrosc. 2010;18:63‐75 [DOI] [PubMed] [Google Scholar]
- 31.Souza RB Powers CM Concurrent criterion‐related validity and reliability of a clinical test to measure femoral anteversion. J Orthop Sports Phys Ther. 2009;39(8):586‐92 [DOI] [PubMed] [Google Scholar]
- 32.Boykin RE Anz AW Bushnell BD Kocher MS Stubbs AJ Philippon MJ Hip instability. J Am Acad Orth Surg. 2011;19:340‐9 [DOI] [PubMed] [Google Scholar]
- 33.Martin RL Enseki KR Draovitch P Trapuzzano T Philippon MJ Acetabular labral tears of the hip: Examination and diagnostic challenges. J Orthop Sports Phys Ther. 2006;36:503‐15 [DOI] [PubMed] [Google Scholar]
- 34.Philippon MJ The role of arthroscopic thermal capsulorrhaphy in the hip. Clin Sports Med. 2001;20:817‐29 [DOI] [PubMed] [Google Scholar]
- 35.Schenker ML Weiland DE Philippon MJ Current Ttrends in Hip Arthroscopy: A review of injury Diagnosis, Techniques and Outcome Scoring. Current Opnion in Orthopaedics. 2005;16:89‐94 [Google Scholar]
- 36.Li H Mao Y Oni JK Dai K Zhu Z Total hip replacement for developmental dysplasia of the hip with more than 30% lateral uncoverage of uncemented acetabular components. Bone Joint J. 2013;95(9):1178‐83 [DOI] [PubMed] [Google Scholar]
- 37.Smith CD Masouros S Hill AM Amis AA Bull AM A biomechanical basis for tears of the human acetabular labrum. Br J Sports Med. 2009;43:574‐8 [DOI] [PubMed] [Google Scholar]
- 38.Martin RL Palmer I Martin HD Ligamentum teres: a functional description and potential clinical relevance. Knee Surg Sports Traumatol Arthrosc. 2012;20:1209‐14 [DOI] [PubMed] [Google Scholar]
- 39.Mitchell B McCrory P Brukner P O'Donnell J Colson E Howells R Hip joint pathology: clinical presentation and correlation between magnetic resonance arthrography, ultrasound, and arthroscopic findings in 25 consecutive cases. Clin J Sports Med. 2003;13:152‐6 [DOI] [PubMed] [Google Scholar]
- 40.Neumann DA Cinesiologia do aparelho musculoesquelético. Fundamentos para reabilitação física. 1st ed. 2006, Rio de Janeiro, RJ: Guanabara Koogan [Google Scholar]
- 41.Beighton P Solomon L Soskolne CL Articular mobility in an African population. Ann Rheum Dis. 1973;32:413‐8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Siebenrock KA Kalbermatten DF Ganz R Effect of pelvic inclination on determination of acetabular retroversion: a study on cadaver pelvis. Clin Orthop Relat Res. 2003;407:241–8 [DOI] [PubMed] [Google Scholar]
- 43.Polesello GC Nakao TS Queiroz MC, et al. Proposal for standardization of radiographic studies on the hip and pelvis. Rev Bras Ortop. 2011;46(6):634‐42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Armfield DR Towers JD Robertson DD Radiographic and MR imaging of the athletic hip. Clin Sports Med. 2006;25:211–39 [DOI] [PubMed] [Google Scholar]
- 45.Wiberg G Studies on Dysplastic Acetabula and Congenital Subluxation of the Hip Joint. Acta Chirurgica Scandinavica. 1939;83, Supplementum 58. [Google Scholar]
- 46.Murphy SB Kijewski PK Millis MB Harless A Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1990;261:214–23 [PubMed] [Google Scholar]
- 47.Philippon MJ Wolff AB Briggs KK Zehms CT Kuppersmith DA Acetabular rim reduction for the treatment of femoroacetabular impingement correlates with preoperative and postoperative center‐edge angle. Arthroscopy. 2010;26(6):757‐61 [DOI] [PubMed] [Google Scholar]
- 48.Reynolds D Lucac J Klaue K Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–8 [DOI] [PubMed] [Google Scholar]
- 49.Samora JB Ng VY Ellis TJ Femoroacetabular Impingement: A Common Cause of Hip Pain in Young Adults. Clin J. Sport med. 2011;21(1):51‐6 [DOI] [PubMed] [Google Scholar]
- 50.Sotelo‐Garza A Charnley J The Results of Charnley Arthroplasty of the Hip Performed for Protrusio Acetabuli. Clin Orthop. 1978;132:12‐8 [PubMed] [Google Scholar]
- 51.Ecker TM Tannast M Puls M Siebenrock KA Murphy SB Pathomorphologic alterations predict presence or absence of hip osteoarthrosis. Clin Orthop Relat Res. 2007;465:46‐52 [DOI] [PubMed] [Google Scholar]
- 52.Gosvig KK Jacobsen S Sonne‐Holm S Palm H. Troelsen A Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population‐based survey. J Bone Joint Surg Am. 2010;92:1162‐9 [DOI] [PubMed] [Google Scholar]
- 53.Ezoe M Naito M Inoue T The prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006;88:372‐9 [DOI] [PubMed] [Google Scholar]
- 54.Meyer DC Beck M Ellis T Ganz R Leunig M Comparison of six radio‐graphic projections to assess femoral head/neck asphericity. Clin Orthop. 2006;445:181‐5 [DOI] [PubMed] [Google Scholar]
- 55.Hack K Di Primo G Rakhra K Beaule PE Prevalence of cam‐type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:436‐44 [DOI] [PubMed] [Google Scholar]
- 56.Pollard TCB Villar RN Norton MR Fern ED Williams MR Simpson DJ, et al. Femoroacetabular impingement and classification of the cam deformity: the reference interval in normal hips. Acta Orthop. 2010;81(1):134–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Clohisy JC Nunley RM Otto RJ Schoenecker PL The frog‐leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115‐21 [DOI] [PubMed] [Google Scholar]
- 58.Peele MW Della Rocca GJ Maloney WJ Curry MC Clohisy JC Acetabular and femoral radiographic abnormalities associated with labral tears. Clin Orthop Relat Res. 2005;441:327‐33 [DOI] [PubMed] [Google Scholar]
- 59.Narvani AA Tsiridis E Kendall S Chaudhuri R Thomas P A preliminary report on prevalence of acetabular labrum tears in sports patients with groin pain. Knee Surg Sports Traumatol Arthrosc. 2003;11:403‐8 [DOI] [PubMed] [Google Scholar]
- 60.Millis MB Kim YJ Kocher MS Hip joint‐preserving surgery for the mature hip: the Children's Hospital experience. Orthop J Harv Med S. 2004;6:84–7 [Google Scholar]
- 61.Polkowski GG Clohisy JC Hip Biomechanics. Sports Med Arthrosc Rev. 2010;18(2):56–62 [DOI] [PubMed] [Google Scholar]
- 62.Ito K Minka MA Leunig M Werlen S Ganz R Femoroacetabular impingement and the cam‐effect. A MRI‐based quantitative anatomical study of the femoral head‐neck offset. J Bone Joint Surg Br. 2001;83:171‐6 [DOI] [PubMed] [Google Scholar]
- 63.Kang ACL Gooding AJ Coates MH Goh TD Armour P Rietveld J Computed tomography assessment of hip joints in asymptomatic individuals in relation fo femoroacetabular impingement. Am J Sports Med. 2010,38(6):1160‐5 [DOI] [PubMed] [Google Scholar]
- 64.Austin AB Souza RB Meyer JL Powers CM Identification of abnormal hip motion associated with acetabular labral pathology. J Orthop Sports Phys Ther. 2008;38(9):558‐65 [DOI] [PubMed] [Google Scholar]
- 65.Emara K Samir W Motasem H Ghafar KA Conservative treatment for mild femoroacetabular impingement. J Orthop Surg. 2011;19(1):41‐5 [DOI] [PubMed] [Google Scholar]
- 66.Yazbek PM Ovanessian V Martin RL Fukuda TY Nonsurgical treatment of acetabular labrum tears: a case series. J Orthop Sports Phys Ther. 2011:41(5):346‐56 [DOI] [PubMed] [Google Scholar]