Abstract
Background
Functionally favorable survival remains low after out-of-hospital cardiac arrest (OHCA). When initial interventions fail to achieve return of spontaneous circulation (ROSC), they are repeated with little incremental benefit. Patients without rapid ROSC do not typically survive with good functional outcome. Novel approaches to OHCA have yielded functionally favorable survival in patients who failed traditional measures, but the optimal transition point from traditional measures to novel therapies is ill defined. Our objective was to estimate the dynamic probability of survival and functional recovery as a function of resuscitation effort duration, in order to identify this transition point.
Methods and Results
Retrospective cohort study of a cardiac arrest database at a single site. We included 1,014 adult (≥18 years) patients suffering non-traumatic OHCA between 2005–2011, defined as receiving CPR or defibrillation from a professional provider. We stratified by functional outcome at hospital discharge (modified Rankin scale–mRS). Survival to hospital discharge was 11%, but only 6% had mRS 0–3. Within 16.1 minutes of CPR, 89.7% (95%CI: 80.3%, 95.8%) of patients with good functional outcome had achieved ROSC, and the probability of good functional recovery fell to 1%. Adjusting for prehospital and inpatient covariates, CPR duration (minutes) is independently associated with favorable functional status at hospital discharge (OR 0.84; 95%CI 0.72, 0.98;p=0.02).
Conclusions
Probability of survival to hospital discharge with mRS 0–3 declines rapidly with each minute of CPR. Novel strategies should be tested early after cardiac arrest rather than after complete failure of traditional measures.
Keywords: cardiopulmonary resuscitation, heart arrest, resuscitation
Introduction
Over 540,000 persons suffer sudden cardiac arrest annually in United States, the majority of which occur out-of-hospital.1 Neurologically favorable survival from out-of-hospital cardiac arrest (OHCA) has increased over the past decade,2–4 with the implementation of integrated systems of care focused on emergency response and systematic post-resuscitation care.4, 5–8 Despite these advances, mortality remains high after OHCA with only 5–15% survival to hospital discharge.1
Besides immediate CPR, rapid defibrillation, and 1–2 mg of epinephrine, no other intervention has been demonstrated to increase the likelihood of return of spontaneous circulation (ROSC). Recently, even the long-term benefits of epinephrine have been questioned.9 When these interventions fail to achieve ROSC after a few minutes, some EMS systems transport patients who fail these interventions to the hospital, where the same resuscitation techniques are repeated. In either setting, no additional resources are brought to bear after initial interventions fail, and the majority of patients who do not have rapid ROSC will not survive or experience a good functional outcome. Other EMS systems will terminate the resuscitation, based on the duration of resuscitation efforts, which has been included into some versions of termination of resuscitation (TOR) guidelines.10–12
Alternative approaches to treatment of OHCA, such as extra-corporeal life support (ECLS), have yielded functionally favorable survival in selected patients who failed traditional CPR.13–15 However, the results of ECLS were poor when initiation of the procedure was restricted to patients who failed 30 minutes or more of traditional resuscitation.16 Choosing the optimal duration of traditional resuscitation after which to switch to an alternate approach requires an estimate of the probability of survival and functional recovery as a function of the duration of resuscitative efforts until ROSC. Longer durations of CPR during in-hospital cardiac arrest are associated with higher rates of ROSC and survival to discharge.17 However, similar data are lacking for OHCA.
We analyzed data from emergency medical services (EMS) that do not use a rigid termination of resuscitation guideline. In this study, we describe the relationship between the duration of CPR until ROSC and functional outcome at hospital discharge, in order to determine if there is a duration of CPR after which repeating traditional resuscitation interventions ceases to result in meaningful survival.
Methods
Data Source
We examined cardiac arrest database data from December 2005 and April 2011 at the Pittsburgh site of the Resuscitation Outcomes Consortium (ROC). ROC is a multicenter clinical trial network focused on cardiac arrest and severe traumatic injury that has previously been described in detail.18 Data for the cardiac arrest database are obtained under a waiver of informed consent, approved by the University of Pittsburgh IRB, as well as participating hospital IRBs. Briefly, research personnel at participating sites prospectively collect patient care reports, monitor ECG data, and audio recordings from all consecutive cardiac arrest patients treated by participating EMS systems. Research coordinators review the hospital records for patients transported to the hospital in order to determine in-hospital interventions, in-hospital mortality, and functional status at the time of hospital discharge.18 Coordinators assigned a modified Rankin Scale (mRS) score at hospital discharge to each subject by review of all available chart information using a standard chart-review instrument.19
Study Design and Population
This was a retrospective cohort study of adult (age ≥18 years) patients suffering out-of-hospital cardiac arrest. Cardiac arrest was defined as receiving chest compressions from a professional provider or rescue shocks from a professional provider or any automated external defibrillator. We excluded both suspected and confirmed cases of traumatic arrest.
Study Definitions & Endpoints
Our primary endpoint was survival to hospital discharge with favorable functional status, defined as modified Rankin scale (mRS) 0–3.20 Additionally, we classified patients into three other groups based on resuscitation outcome: survival to hospital discharge with unfavorable functional status (mRS 4–5), ROSC without survival to hospital discharge (mRS 6), and no ROSC. Resuscitation duration, defined as CPR duration in minutes, was the primary independent variable. CPR duration was defined as the time from first chest compression provided by EMS providers to termination of resuscitation efforts either because of ROSC or declaration of death. Paramedics are permitted to cease resuscitative efforts at the scene after consultation with a physician either on-scene or via radio.
Time-stamped data (hours: minutes: seconds) on the initiation and conclusion of CPR by EMS providers were recorded by the monitor-defibrillator, which stays with the patient throughout resuscitation. CPR performance was detected either indirectly by changes in thoracic impedance recorded from external defibrillator electrodes21, or directly by an accelerometer between the rescuer and patient’s chest.
Statistical Analyses
Analyses were performed with STATA 12.0 (StataCorp, College Station, TX). We stratified patients by outcome and tabulated patient characteristics, cardiac arrest characteristics, EMS interventions, and inpatient interventions.
For the subset of patients achieving ROSC, we constructed simple curves of the proportion of subjects achieving ROSC over time, stratified by outcome (mRS 0–3, mRS 4–5, mRS 6), and compared distributions with the Kruskal-Wallis test. We then determined the estimated 50th, 75th, and 90th percentiles of CPR duration for each stratum. We also determined the duration of CPR corresponding to the estimated 50%, 75%, 90%, and 99% proportion of patients achieving ROSC, stratified by outcome. We used the data point closest to, but not exceeding, each proportion. Finally, we calculated the dynamic probability of survival with mRS 0–3 among all attempted resuscitations.
We created both unadjusted and adjusted logistic regression models to evaluate the association between CPR duration and mRS 0–3 on hospital discharge. We used two separate adjusted models to evaluate the association between CPR duration and survival to hospital discharge with mRS 0–3. Based on prior work,4, 22–25 we adjusted each regression model for covariates that are associated with outcome. The first model was adjusted for prehospital covariates (age, sex, witnessed arrest, AED shock, EMS dispatch interval, shockable initial rhythm, chest compression fraction, advanced airway attempts, and epinephrine administration). This model represents the association between CPR duration and patient outcome at the time of CPR. The second model was additionally adjusted for therapeutic hypothermia and cardiac catheterization, which are subsequent confounders that may have altered patient outcome.
Results
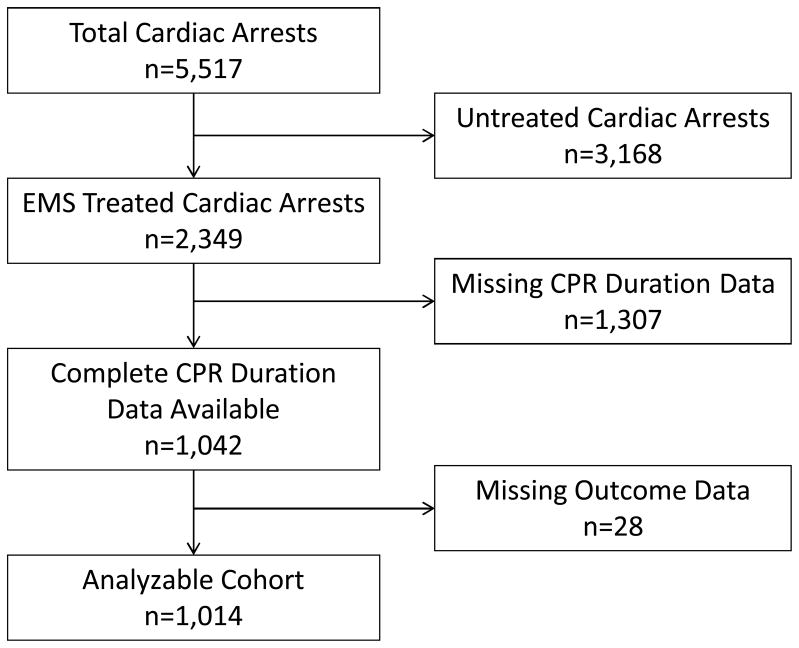
A total of n=5,517 subjects suffered OHCA during the specified time frame, with 2,349 treated by EMS and considered for analysis. Of these, 1,042 had complete data for analysis of CPR duration. Subjects with complete CPR duration data did not differ in clinical features from the subjects excluded because of incomplete data. An additional 28 subjects were excluded because of missing survival or functional outcome data, leaving n=1,014 for final analysis. (Figure 1) Of these 1,014 attempted resuscitations, 475 (47%) achieved ROSC, 113 (11%) survived to hospital discharge, and 58 (6%) had a favorable functional status.
Figure 1.
Study cohort and exclusions. EMS: emergency medical services. CPR: cardiopulmonary resuscitation.
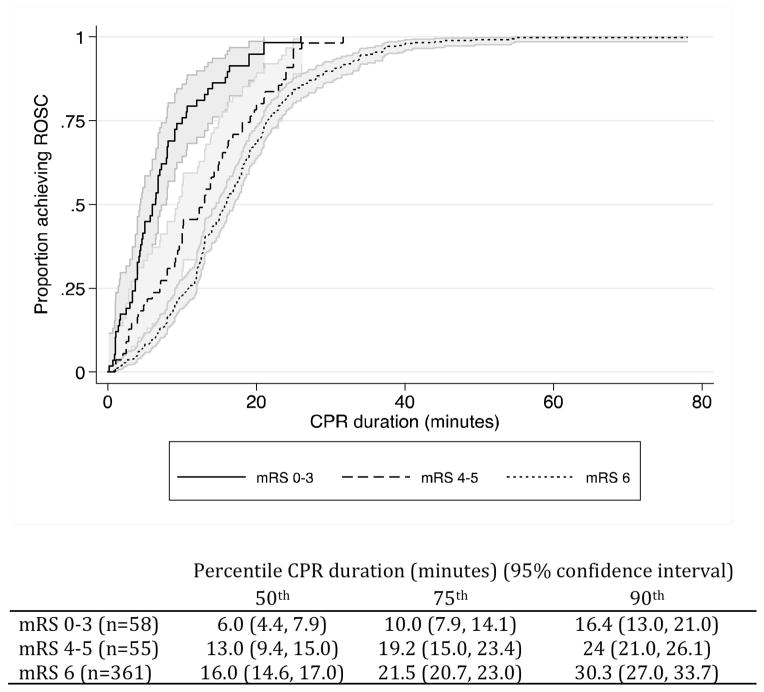
Demographic and clinical features stratified by outcome are presented in Table 1. The simple curves and estimated percentiles of CPR duration for patients achieving ROSC, stratified by patient outcome, are presented in Figure 2. The distribution of CPR duration differed across strata (p=0.0001).
Table 1.
Clinical features stratified by functional outcome at hospital discharge. Continuous variables are given either as mean ± standard deviation, or median (interquartile range). Categorical variables are given as count (%). EMS: emergency medical services. ECG: electrocardiogram. VF: ventricular fibrillation. VT: ventricular tachycardia. PEA: pulseless electrical activity. AED: automated external defibrillator. min: minutes. CPR: cardiopulmonary resuscitation. SBP: systolic blood pressure. PCI: percutaneous coronary intervention. CABG: coronary artery bypass graft. ICD: implantable cardiac defibrillator. ICU: intensive care unit. DNR: do not resuscitate. N/A: not applicable.
| mRS 0–3 n=58 |
mRS 4–5 n=55 |
mRS 6 n=362 |
ROSC=0 n=539 |
|
|---|---|---|---|---|
| Baseline characteristics | ||||
| Age (years) | 56.2 ± 15.5 | 63.0 ± 16.7 | 68.0 ± 15.8 | 64.5 ± 18.4 |
| Male sex | 39 (67.2%) | 28 (50.9%) | 198 (54.7) | 312 (58.0%) |
| Residence prior to event | ||||
| Home | 58 (100%) | 46 (83.6%) | 239 (66.0%) | 0 (0%) |
| Rehabilitation center | 0 (0%) | 0 (0%) | 2 (0.5%) | 0 (0%) |
| Assisted living facility | 0 (0%) | 1 (1.8%) | 11 (3.0%) | 0 (0%) |
| Nursing home | 0 (0%) | 5 (9.1%) | 72 (19.9%) | 1 (0.2%) |
| Event characteristics | ||||
| Witnessed status | ||||
| EMS-witnessed | 10 (17.2%) | 5 (9.1%) | 41 (11.3%) | 17 (3.2%) |
| Bystander-witnessed | 38 (65.5%) | 26 (47.3%) | 157 (43.4%) | 102 (18.9%) |
| Not witnessed | 2 (3.5%) | 2 (3.6%) | 23 (6.4%) | 71 (13.2%) |
| Bystander CPR | 27 (46.6%) | 21 (38.2%) | 171 (47.2%) | 175 (32.5%) |
| AED shock delivered | 5 (8.6%) | 0 (0%) | 8 (2.2%) | 3 (0.6%) |
| Initial ECG Rhythm | ||||
| VF/VT | 43 (74.1%) | 27 (49.1%) | 79 (21.8%) | 45 (8.4%) |
| PEA | 6 (10.3%) | 16 (29.1%) | 107 (29.6%) | 64 (11.9%) |
| Asystole | 3 (5.2%) | 6 (10.9%) | 131 (36.2%) | 315 (58.4%) |
| AED – no shock advised | 3 (5.2%) | 4 (7.3%) | 37 (10.2%) | 105 (19.5%) |
| EMS interventions | ||||
| 911 call – EMS arrival (min) | 6.0 ± 4.3 | 5.2 ± 2.8 | 6.6 ± 3.3 | 5.9 ± 2.8 |
| CPR duration (min) | 6.2 (3.7, 10.0) | 13.0 (7.0, 19.2) | 16.0 (10.8, 21.5) | 17.5 (6.8, 26.7) |
| Chest compression fraction | 0.48 ± 0.18 | 0.58 ± 0.16 | 0.65 ± 0.13 | 0.66 ± 0.15 |
| Advanced airway attempted | 26 (44.8%) | 35 (63.6%) | 244 (67.4%) | 243 (45.1%) |
| Epinephrine administered | 14 (24.1%) | 39 (70.9%) | 334 (92.3%) | 313 (58.1%) |
| Dose epinephrine (mg) | 2.8 ± 1.4 | 2.8 ± 1.5 | 3.5 ± 1.9 | 3.7 ± 0.6 |
| Any shock delivered | 39 (67.2%) | 23 (41.8%) | 118 (32.6%) | 61 (11.3%) |
| Number of shocks delivered | 3 (1, 5) | 3 (1, 5) | 3 (1, 5) | 2 (1, 3) |
| Inpatient interventions | ||||
| First recorded SBP (mmHg) | 139.9 ± 36.7 | 135.8 ± 36.7 | 116.3 ± 42.4 | N/A |
| Therapeutic hypothermia | 12 (20.7%) | 27 (49.1%) | 102 (28.2%) | |
| Cardiac catheterization | 33 (56.9%) | 17 (30.9%) | 26 (7.2%) | |
| PCI | 24 (41.4%) | 13 (23.6%) | 18 (5.0%) | |
| CABG | 6 (10.3%) | 2 (3.6%) | 1 (0.3%) | |
| Pacemaker/ICD implant | 23 (39.7%) | 9 (16.4%) | 1 (0.3%) | |
| ICU length of stay (days) | 5 (3, 9) | 13 (6, 18) | 2 (0, 4) | |
| DNR order | 0 (0%) | 11 (21.2%) | 201 (63.4%) | |
Figure 2.
Distribution of CPR duration for patients achieving return of spontaneous circulation, stratified by outcome (p=0.0001).
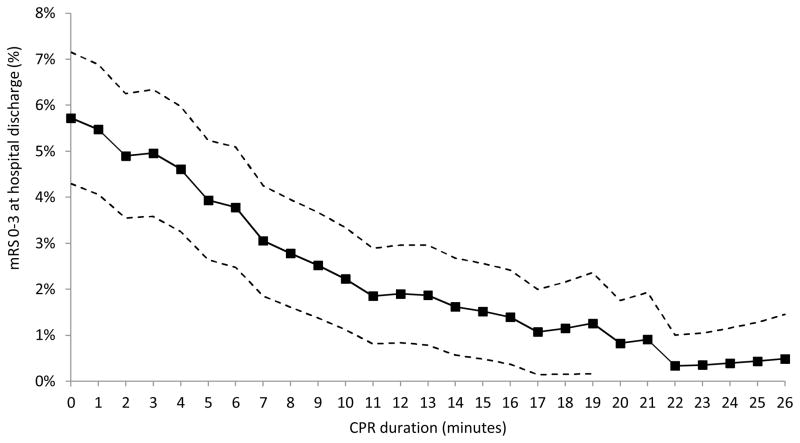
The dynamic probabilities and 95% confidence intervals for survival with mRS 0–3 among all resuscitations is presented in Figure 3. Each data point represents favorable functional outcome achieved among patients with CPR durations greater than or equal to the interval indicated.
Figure 3.
Dynamic probability of survival to hospital discharge with mRS 0–3 by CPR duration with 95% confidence intervals. mRS: modified Rankin scale. CPR: cardiopulmonary resuscitation.
The durations of CPR corresponding to estimated proportions of patients achieving ROSC are presented in Table 2. We selected data points closest to, but not exceeding, the 50%, 75%, and 90% function of ROSC. Within 9.3 minutes of CPR, 74.1% (95% CI: 62.5%, 84.5%) of patients with good functional outcome had achieved ROSC. Within 16.1 minutes of CPR, 89.7% (95% CI: 80.3%, 95.8%) of patients with good functional outcome had achieved ROSC.
Table 2.
CPR durations that correspond to the estimated 50%, 75%, and 90% proportions of patients achieving ROSC, stratified by outcome. mRS: modified Rankin scale. ROSC: return of spontaneous circulation.
| Patient outcome | Proportion achieving ROSC (95% confidence interval) | CPR duration (minutes) |
|---|---|---|
| mRS 0–3 (n=58) | 50.0% (38.0%, 63.4%) | 6.0 |
| 74.1% (62.5%, 84.5%) | 9.3 | |
| 89.7% (80.3%, 95.8%) | 16.1 | |
| mRS 4–5 (n=55) | 49.1% (36.8%, 62.9%) | 12.3 |
| 74.6%, (62.6%, 85.1%) | 18.1 | |
| 87.3% (77.1%, 94.5%) | 23.4 | |
| mRS 6 (n=361) | 49.9% (44.8%, 55.1%) | 15.9 |
| 74.8% (70.2%, 79.1%) | 21.4 | |
| 89.7% (86.4%, 92.6%) | 29.3 |
The logistic regression models are presented in Table 3. Adjusting for prehospital covariates, CPR duration (minutes) is independently associated with survival to hospital discharge with mRS 0–3 (OR 0.84; 95%CI 0.75, 0.95; p=0.04). Further adjusting for inpatient covariates, therapeutic hypothermia and cardiac catheterization, CPR duration (minutes) is independently associated with survival to hospital discharge with mRS 0–3 (OR 0.84; 95%CI 0.72, 0.98; p=0.02).
Table 3.
Unadjusted and adjusted logistic regression models for mRS 0–3 on hospital discharge. CI: confidence interval. CPR: cardiopulmonary resuscitation. AED: automate external defibrillator. EMS: emergency medical services.
| Odds Ratio | 95% CI | p-value | |
|---|---|---|---|
| Unadjusted Model | |||
| CPR duration (minutes) | 0.87 | 0.83, 0.91 | < 0.001 |
| Prehospital Adjusted Model | |||
| CPR duration (minutes) | 0.84 | 0.75, 0.95 | 0.004 |
| Age (years) | 0.94 | 0.91, 0.99 | 0.007 |
| Male sex | 0.58 | 0.19, 1.78 | 0.34 |
| Witnessed arrest | 4.91 | 1.29, 18.67 | 0.02 |
| AED shock delivered | Absence perfectly predicts failure | ||
| 911 call to EMS arrival (minutes) | 1.00 | 0.85, 1.18 | 0.99 |
| Shockable initial rhythm | 10.31 | 2.79, 38.8 | < 0.001 |
| Chest compression fraction (%) | 0.03 | 0.01, 1.13 | 0.06 |
| Advanced airway attempted | 2.68 | 0.57, 12.57 | 0.21 |
| Epinephrine administered | 0.46 | 0.11, 1.91 | 0.29 |
| Inpatient Adjusted Model | |||
| CPR duration (minutes) | 0.84 | 0.72, 0.98 | 0.02 |
| Age (years) | 0.93 | 0.89, 0.97 | 0.002 |
| Male sex | 0.71 | 0.20, 2.54 | 0.61 |
| Witnessed arrest | 4.38 | 1.07, 18.03 | 0.04 |
| AED shock delivered | Absence perfectly predicts failure | ||
| 911 call to EMS arrival (minutes) | 0.97 | 0.82, 1.16 | 0.76 |
| Shockable initial rhythm | 3.35 | 0.78, 14.34 | 0.10 |
| Chest compression fraction (%) | 0.06 | 0.01, 2.84 | 0.15 |
| Advanced airway attempted | 1.17 | 0.25, 5.43 | 0.84 |
| Epinephrine administered | 0.37 | 0.08, 1.71 | 0.20 |
| Therapeutic hypothermia | 0.40 | 0.12, 1.35 | 0.14 |
| Cardiac catheterization | 5.85 | 1.58, 21.64 | 0.008 |
Discussion
In a single-site OHCA registry, we observed a rapidly diminishing probability of favorable functional status at hospital discharge with increasing durations of CPR (Figure 3). After 16.1 minutes of CPR, 89.7% (95% CI: 80.3%, 95.8%) of patients with eventual mRS 0–3 at hospital discharge had achieved ROSC (Table 2). CPR duration was independently associated with favorable functional status, adjusting for both prehospital and inpatient covariates (Table 3).
Our findings suggest that conventional resuscitation strategies are most effective within the first 10 – 15 minutes, by which time more than 75% of patients with good functional recovery had already achieved ROSC (Figure 2). After 15 minutes, the probability of good functional recovery among all attempted resuscitations falls to ~2% (Figure 3). Repeating the same therapies that did not work during the first 10–15 minutes does not result in incremental favorable survival.
Our findings highlight the need to implement novel resuscitation strategies in appropriate candidates who do not immediately respond to CPR, defibrillation, and the initial dose of epinephrine. An example intervention is extra-corporeal life support (ECLS) for cardiac arrest resuscitation. This resource-intensive therapy has been successfully deployed to boost functionally favorable survival in selected candidates.13–15 However, the potential cost and resource-intensity of ECLS mandate that it be applied in a rational manner with optimal chance to benefit the patient.
For interventions like ECLS to improve outcomes, it is critical that they not be implemented only after prolonged failure of traditional CPR. The traditional resuscitation paradigm emphasizes prompt attention to serial links in the chain of survival: early recognition of cardiac arrest and activation of the emergency response system, early CPR, early defibrillation, early advanced life support, and post-resuscitation care. Our data demonstrate declining proportions of subjects who have favorable functional recovery with each minute that traditional CPR fails to achieve ROSC. Furthermore traditional resuscitation usually fails, making it reasonable to mobilize efforts to apply a novel therapy like ECLS immediately at the recognition of cardiac arrest, concurrently with traditional CPR. In those patients who achieve ROSC rapidly with traditional CPR, the mobilization of novel therapy can be discontinued.
Belohlavek, et al. propose a “hyperinvasive” approach to out-of-hospital cardiac arrest in the methods paper for the “Prague OHCA Study”.26 The authors propose a randomized parallel groups comparative study of mechanical chest compressions, prehospital intra-arrest cooling, ECLS, and immediate coronary angiography compared to standard ACLS-type care. Of note, subjects receive only five minutes of ACLS, before randomization to the “standard” or “hyperinvasive” arm. The “hyperinvasive” approach hinges on rapid deployment of a mechanical chest compression device that facilitates immediate transport to a cardiac arrest center with CPR in progress. Patients that achieve ROSC during transport to the receiving center are still cooled and receive an invasive hemodynamic assessment consisting of coronary angiography, pulmonary angiography, aortography, and transthoracic echocardiography. ECLS is applied at the receiving center in patients without ROSC or patients with ROSC but persistent cardiogenic shock.
Earlier recognition of cardiac arrest coupled with earlier traditional therapies may still improve the proportion of survivors with good functional outcome at hospital discharge. However, current resuscitation strategies have been optimized for the last 58 years, since the inception of manual external chest compressions.27 Observational studies and clinical trials with subsequent guideline updates have refined CPR quality,28–30 defibrillation timing,31 and pharmacological intervention,32–34 but the essence of cardiac arrest resuscitation has not fundamentally changed. A new paradigm may be needed to achieve more than modest improvements in patient outcome.
We advise caution about using these data to guide incorporation of CPR duration into termination of resuscitation guidelines. Our data are derived from a subset of the population at a single site. Subjects were hospitalized at a variety of hospitals with varying sophistication of post-cardiac arrest care. Anecdotally, during this same time period, the authors have treated OHCA patients from other EMS systems who displayed good functional recovery despite total CPR durations longer than 21 minutes. These anecdotal cases may be explained by the 95% confidence intervals for the estimations of CPR duration (Figure 2), probabilities of achieving ROSC (Table 2), and probabilities of mRS 0–3 on hospital discharge (Figure 3). Larger data sets may provide more precise estimates of the longest tolerable CPR duration. Finally, our primary outcome, functional status at hospital discharge is a surrogate for long-term recovery. We have previously demonstrated that a large proportion of patients leaving the hospital have significant functional deficits,35 but that patients continue to improve after hospital discharge.36
Limitations
These are retrospective data are from a single-center registry. As such, there may be unmeasured biases in EMS treatment and local culture that influence resuscitation effort duration. One agency in our system dispatches a physician to each OHCA and termination of resuscitation at the scene is common. Additionally, the post-resuscitative care and prognostic workup may differ between hospitals that care for these patients. A larger cohort is necessary to determine the generalizability of our results. Furthermore, we are subject to an inherent limitation of outcome-driven cardiac arrest research: patients without ROSC do not achieve subsequent outcomes. In this manner, outcomes after cardiac arrest are typically skewed with respect to CPR duration. However, we also note that outcome after ROSC appears to be a function of CPR duration. Patients that achieve ROSC after brief CPR durations are more likely to have improved functional outcome. Likewise, patients that achieve ROSC after longer CPR durations are more likely to have poor functional outcome.
Conclusions
Most CPR efforts fail to produce sustained ROSC after OHCA. Despite some increase in the total number of patients with ROSC when CPR is prolonged, the proportion of OHCA cases that survive to hospital discharge with favorable functional status declines with each minute of CPR. Alternative strategies to traditional resuscitation should be tested immediately after cardiac arrest rather than after failure of traditional CPR.
Clinical Commentary.
Despite advances in systematic post-resuscitation care, only 5–15% of out-of-hospital cardiac arrest (OHCA) victims survive to hospital discharge. Few interventions have proven benefit in cardiac arrest resuscitation, and the typical strategy for patients without rapid return of spontaneous circulation (ROSC) is to repeat failed interventions. No additional resources are brought to bear. Novel approaches to treating OHCA, such as extra-corporeal life support (ECLS) have yielded neurologically favorable survival in select patients who fail traditional resuscitation. We investigated the relationship between duration of CPR and neurologic outcome after cardiac arrest to identify the duration of CPR beyond which repeating traditional resuscitation measures does not result in incremental neurologically favorable survival. Our findings suggest that conventional resuscitation is the most effective within the first 10–15 minutes, by which time 75% of patients with favorable neurologic recovery had achieved ROSC. The probability of favorable neurologic recovery fell to 2% beyond this point. CPR duration was independently associated with favorable neurologic outcome, adjusting for prehospital and inpatient covariates. Alternative strategies to traditional resuscitation should be tested immediately after cardiac arrest, rather than after failure of traditional CPR.
Acknowledgments
The authors thank Joe Condle for his invaluable assistance maintaining the Pittsburgh ROC epistry. The ROC Data Coordinating Center did not partake in the analyses or conclusions. We also acknowledge the assistance of Joyce (Chung-Chou) H. Chang, PhD, Professor Medicine, Biostatistics, and Clinical and Translational Science at the University of Pittsburgh, with statistical methodology.
Funding Sources: The Pittsburgh ROC site is supported by HL077871 from the National Heart, Lung and Blood Institute, National Institutes of Health.
Footnotes
Conflict of Interest Disclosures: Dr. Callaway is funded by NHLBI HL077871-University of Pittsburgh. The rest of the authors have nothing to disclose.
References
- 1.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adielsson A, Hollenberg J, Karlsson T, Lindqvist J, Lundin S, Silfverstolpe J, Svensson L, Herlitz J. Increase in survival and bystander CPR in out-of-hospital shockable arrhythmia: bystander CPR and female gender are predictors of improved outcome. Experiences from Sweden in an 18-year perspective. Heart. 2011;97:1391–6. doi: 10.1136/hrt.2011.222711. [DOI] [PubMed] [Google Scholar]
- 3.Bobrow BJ, Spaite DW, Berg RA, Stolz U, Sanders AB, Kern KB, Vadeboncoeur TF, Clark LL, Gallagher JV, Stapczynski JS, LoVecchio F, Mullins TJ, Humble WO, Ewy GA. Chest compression-only CPR by lay rescuers and survival from out-of-hospital cardiac arrest. JAMA. 2010;304:1447–54. doi: 10.1001/jama.2010.1392. [DOI] [PubMed] [Google Scholar]
- 4.Sunde K, Pytte M, Jacobse D, Mangschau A, Jensen LP, Smedsrud C, Draegni T, Steen PA. Implementation of a standardised treatment protocol for post resuscitation care after out-of-hospital cardiac arrest. Resuscitation. 2007;73:29–39. doi: 10.1016/j.resuscitation.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 5.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS American Heart Association Get with the Guidelines–Resuscitation Investigators. Trends in survival after in-hospital cardiac arrest. New Engl J Med. 2012;367:1912–20. doi: 10.1056/NEJMoa1109148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–63. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 7.Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:1756. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 8.Rittenberger JC, Guyette FX, Tisherman SA, DeVita MA, Alvarez RJ, Callaway CW. Outcomes of a hospital-wide plan to improve care of comatose survivors of cardiac arrest. Resuscitation. 2008;79:198–204. doi: 10.1016/j.resuscitation.2008.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hagihara A, Hasegawa M, Abe T, Nagata T, Wakata Y, Miyazaki S. Prehospital epinephrine use and survival among patients with out-of-hospital cardiac arrest. JAMA. 2012;307:1161–8. doi: 10.1001/jama.2012.294. [DOI] [PubMed] [Google Scholar]
- 10.Bailey ED, Wydro GC, Cone DC. Termination of resuscitation in the prehospital setting for adult patients suffering nontraumatic cardiac arrest. National Association of EMS Physicians Standards and Clinical Practice Committee. Prehospital Emerg Care. 2000;4:190–5. doi: 10.1080/10903120090941498. [DOI] [PubMed] [Google Scholar]
- 11.Ong MEH, Jaffey J, Stiell I, Nesbitt L, Group OS. Comparison of termination-of-resuscitation guidelines for basic life support: defibrillator providers in out-of-hospital cardiac arrest. Ann Emerg Med. 2006;47:337–43. doi: 10.1016/j.annemergmed.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 12.van Walraven C, Forster AJ, Stiell IG. Derivation of a clinical decision rule for the discontinuation of in-hospital cardiac arrest resuscitations. Arch Intern Med. 1999;159:129–34. doi: 10.1001/archinte.159.2.129. [DOI] [PubMed] [Google Scholar]
- 13.Nagao K, Kikushima K, Watanabe K, Tachibana E, Tominaga Y, Tada K, Ishii M, Chiba N, Kasai A, Soga T. Early induction of hypothermia during cardiac arrest improves neurological outcomes in patients with out-of hospital cardiac arrest who undergo emergency cardiopulmonary bypass and percutaneous coronary intervention. Circ J. 2010;74:77–85. doi: 10.1253/circj.cj-09-0502. [DOI] [PubMed] [Google Scholar]
- 14.Tanno K, Itoh Y, Takeyama Y, Nara S, Mori K, Asai Y. Utstein style study of cardiopulmonary bypass after cardiac arrest. Am J Emerg Med. 2008;26:649–54. doi: 10.1016/j.ajem.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 15.Bellezzo JM, Shinar Z, Davis DP, Jaski BE, Chillcott S, Stahovich M, Walker C, Baradarian S, Dembitsky W. Emergency physician-initiated extracorporeal cardiopulmonary resuscitation. Resuscitation. 2012;83:966–70. doi: 10.1016/j.resuscitation.2012.01.027. [DOI] [PubMed] [Google Scholar]
- 16.Le Guen M, Nicolas-Robin A, Carreira S, Raux M, Leprince P, Riou B, Langeron O. Extracorporeal life support following out-of-hospital refractory cardiac arrest. Crit Care. 2011;15:R29. doi: 10.1186/cc9976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldberger ZD, Chan PS, Berg RA, Kronick SL, Cooke CR, Lu M, Banerjee M, Hayward RA, Krumholz HM, Nallamothu BK American Heart Association Get With The Guidelines—Resuscitation (formerly National Registry of Cardiopulmonary Resuscitation) Investigators. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380:1473–81. doi: 10.1016/S0140-6736(12)60862-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morrison LJ, Nichol G, Rea TD, Christenson J, Callaway CW, Stephens S, Pirrallo RG, Atkins DL, Davis DP, Idris AH, Newgard C ROC Investigators. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Resuscitation. 2008;78:161–9. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raina KD, Callaway CW, Rittenberger JC, Holm MB. Neurological and functional status following cardiac arrest: method and tool utility. Resuscitation. 2008;79:249–56. doi: 10.1016/j.resuscitation.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lai SM, Duncan PW. Stroke recovery profile and the Modified Rankin assessment. Neuroepidemiology. 2001;20:26–30. doi: 10.1159/000054754. [DOI] [PubMed] [Google Scholar]
- 21.Stecher FS, Olsen JA, Stickney RE, Wik L. Transthoracic impedance used to evaluate performance of cardiopulmonary resuscitation during out of hospital cardiac arrest. Resuscitation. 2008;79:432–7. doi: 10.1016/j.resuscitation.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Reynolds JC, Callaway CW, El Khoudary SR, Moore CG, Alvarez RJ, Rittenberger JC. Coronary angiography predicts improved outcome following cardiac arrest: propensity-adjusted analysis. J Intens Care Med. 2009;24:179–86A. doi: 10.1177/0885066609332725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang HE, Min A, Hostler D, Chang CC, Callaway CW. Differential effects of out-of hospital interventions on short- and long-term survival after cardiopulmonary arrest. Resuscitation. 2005;67:69–74. doi: 10.1016/j.resuscitation.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 24.Kaji AH, Hanif AM, Thomas JL, Niemann JT. Out-of-hospital cardiac arrest: early in-hospital hypotension versus out-of-hospital factors in predicting in-hospital mortality among those surviving to hospital admission. Resuscitation. 2011;82:1314–7. doi: 10.1016/j.resuscitation.2011.05.030. [DOI] [PubMed] [Google Scholar]
- 25.Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, Callaway CW, Bishop D, Vaillancourt C, Davis D. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120:1241–47. doi: 10.1161/CIRCULATIONAHA.109.852202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Belohlavek J, Kucera K, Jarkovsky J, Franek O, Pokorna M, Danda J, Skripsky R, Kandrnal V, Balik M, Kunstyr J. Hyperinvasive approach to out-of hospital cardiac arrest using mechanical chest compression device, prehospital intraarrest cooling, extracorporeal life support and early invasive assessment compared to standard of care. A randomized parallel groups comparative study proposal. “Prague OHCA study”. J Transl Med. 2012;10:163. doi: 10.1186/1479-5876-10-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elam JO, Brown ES, Elder JD. Artificial respiration by mouth-to-mask method; a study of the respiratory gas exchange of paralyzed patients ventilated by operator’s expired air. N Engl J Med. 1954;250:749–54. doi: 10.1056/NEJM195405062501801. [DOI] [PubMed] [Google Scholar]
- 28.Hostler D, Everson-Stewart S, Rea TD, Stiell IG, Callaway CW, Kudenchuk PJ, Sears GK, Emerson SS, Nichol G Resuscitation Outcomes Consortium Investigators. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. BMJ. 2011;342:d512. doi: 10.1136/bmj.d512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Continuous Chest Compressions (CCC), ClinicalTrials.gov. [Accessed November 30, 2012.];A service of the US National Institutes of Health. http://clinicaltrials.gov/ct2/show/NCT01372748.
- 30.Ong ME, Mackey KE, Zhang ZC, Tanaka H, Ma MH, Swor R, Shin SD. Mechanical CPR devices compared to manual CPR during out-of-hospital cardiac arrest and ambulance transport: a systematic review. Scand J Trauma Resusc Emerg Med. 2012;20:39. doi: 10.1186/1757-7241-20-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stiell IG, Nichol G, Leroux BG, Rea TD, Ornato JP, Powell J, Christenson J, Callaway CW, Kudenchuk PJ, Aufderheide TP, Idris AH, Daya MR, Wang HE, Morrison LJ, Davis D, Andrusiek D, Stephens S, Cheskes S, Schmicker RH, Fowler R, Vaillancourt C, Hostler D, Zive D, Pirrallo RG, Vilke GM, Sopko G, Weisfeldt M ROC Investigators. Early versus later rhythm analysis in patients with out-of-hospital cardiac arrest. N Engl J Med. 2011;365:787–97. doi: 10.1056/NEJMoa1010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Olasveengen TM, Sunde K, Brunborg C, Thowsen J, Steen PA, Wik L. Intravenous drug administration during out-of-hospital cardiac arrest: a randomized trial. JAMA. 2009;302:2222–9. doi: 10.1001/jama.2009.1729. [DOI] [PubMed] [Google Scholar]
- 33.Jacobs IG, Finn JC, Jelinek GA, Oxer HF, Thompson PL. Effect of adrenaline on survival in out-of-hospital cardiac arrest: a randomized double-blind placebo-controlled trial. Resuscitation. 2011;82:1138–43. doi: 10.1016/j.resuscitation.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 34.Ong ME, Pellis T, Link MS. The use of antiarrhythmic drugs for adult cardiac arrest: a systematic review. Resuscitation. 2011;82:665–70. doi: 10.1016/j.resuscitation.2011.02.033. [DOI] [PubMed] [Google Scholar]
- 35.Rittenberger JC, Sangl J, Wheeler M, Guyette FX, Callaway CW. Association between clinical examination and outcome after cardiac arrest. Resuscitation. 2010;81:1128–32. doi: 10.1016/j.resuscitation.2010.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Raina KD, Callaway CW, Rittenberger JC, Holm MB. Neurological and functional status following cardiac arrest: method and tool utility. Resuscitation. 2008;79:249–56. doi: 10.1016/j.resuscitation.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]