Abstract
Purpose
To determine demographic and refractive risk factors for astigmatism in the Vision in Preschoolers (VIP) Study.
Methods
Three- to 5-year old Head Start preschoolers (N=4,040) from 5 clinical centers underwent comprehensive eye examinations by study-certified optometrists and ophthalmologists, including monocular visual acuity (VA) testing, cover testing, and cycloplegic retinoscopy. Astigmatism was defined as the presence of ≥ +1.5 diopters (D) cylinder in either eye, measured with cycloplegic refraction. The associations of risk factors with astigmatism were evaluated using the odds ratio (OR) and its 95% confidence intervals (95% CI) from logistic regression models.
Results
Among 4,040 VIP Study participants over-representing children with vision disorders, 687 (17%) had astigmatism, and majority of astigmatism was with-the-rule (83.8%). In multivariate analyses, African-American (OR=1.65, 95% CI: 1.22–2.24), Hispanic (OR=2.25, 95% CI: 1.62–3.12) and Asian children (OR=1.76, 95% CI: 1.06–2.93) were more likely to have astigmatism compared with non-Hispanic white children, while American Indian children were less likely to have astigmatism than Hispanic, African American and Asian children (P<0.0001). Refractive error was associated with astigmatism in a non-linear manner, with an OR of 4.50 (95% CI: 3.00 – 6.76) for myopia (≤ −1.0D in spherical equivalent), and 1.55 (95% CI: 1.29 –1.86) for hyperopia (≥ +2.0D) when compared to children without refractive error (> −1.0D, < +2.0D). There was a trend of an increasing percentage of astigmatism among older children (linear trend p=0.06). The analysis for risk factors of with-the-rule astigmatism provided similar results.
Conclusions
Among Head Start preschoolers, Hispanic ethnicity, African-American and Asian race, myopic and hyperopic refractive error were associated with an increased risk of astigmatism, consistent with findings from the population-based Multi-ethnic Pediatric Eye Disease and Baltimore Pediatric Eye Disease studies. American Indian children had lower risk of astigmatism.
Keywords: astigmatism, refractive error, risk factor, preschoolers
Astigmatism is a common vision disorder that leads to blurred vision due to the inability of the ocular system to form a sharply focused image on the retina, and it accounts for approximately 13% of the refractive errors of the human eye. 1 Previous studies have suggested that uncorrected astigmatism is associated with increased risk of myopia or amblyopia.2,3,4,5,6,7 Early detection of astigmatism in pediatric populations is particularly important because of its potential influence on normal visual development.
The exact cause of astigmatism is unknown. However, risk factors for astigmatism have been evaluated, particularly from population-based studies. Recently, pooled data from the Multi-ethnic Pediatric Eye Disease Study (MEPEDS) and the Baltimore Pediatric Eye Disease Study (BPEDS) were analyzed with regard to the demographic, behavioral and clinical risk factors for astigmatism. The pooled data showed that younger age (<12 months), Hispanic ethnicity, African American race, the presence of significant refractive error (myopia or hyperopia) and maternal smoking during pregnancy were each associated with an increased risk of astigmatism.8 However, only children from two areas (Los Angeles, California and Baltimore, Maryland) of the United States were evaluated, and no Asian or American Indian children were included.
The Vision In Preschoolers (VIP) Study was a multicenter study of preschool children in Head Start, representing a large sample of children (N=4,040) from a variety of racial/ethnic groups (African American, American Indian, Asian, Hispanic, and non-Hispanic White) across five VIP clinical centers (Berkeley, California; Boston, Massachusetts; Columbus, Ohio; Philadelphia, Pennsylvania; Tahlequah, Oklahoma). All the children underwent comprehensive eye examinations performed by VIP-certified pediatric optometrists and ophthalmologists. The standardized eye examination data from the VIP Study provided an additional resource for the study of risk factors for astigmatism. Recently, we compared the vision disorders across racial/ethnicity groups and found that prevalence of astigmatism varied across racial/ethnicity groups with the lowest prevalence rate in American Indian (4.3%) and highest in Hispanic children (11.1%). 9 However, this study did not evaluate other risk factors for astigmatism. The purpose of this study was to determine whether the demographic and ocular risk factors for astigmatism identified from the MEPEDS and BPEDS 8 were also associated with astigmatism in the VIP Study participants from disparate racial/ethnic groups.
METHODS
This is a secondary analysis of the VIP Study data. The VIP Study was a multicenter, cross-sectional, two-phased study conducted from 2001 to 2004 and sponsored by the National Eye Institute, to evaluate the effectiveness of vision screening tests for identifying preschool children who would benefit from a comprehensive eye examination. The details of the VIP Study design have been published elsewhere10,11 and only details of the comprehensive eye examination to identify astigmatism are described here.
Subjects
A total of 4,040 VIP participants (36 to 72 months old) were enrolled from Head Start programs near the five VIP clinical centers across the United States. All children who failed their local Head Start screening and a random sample (~20%) of those who did not fail were targeted for enrollment into the VIP Study. This approach provided a study population in which children with vision disorders were over represented. The local institutional review boards associated with each center approved the study protocol. The informed consent documents were obtained from children’s parents or legal guardians.
Comprehensive Eye Examinations
Enrolled children underwent a comprehensive eye examination performed by study-certified optometrists and ophthalmologists who were experienced in providing care to children. The comprehensive eye examination included monocular threshold visual acuity (VA) testing, cover testing, and cycloplegic retinoscopy. Retinoscopy was performed 30 to 40 minutes after instillation of cycloplegic drops. A second set of the cycloplegic agents was instilled at the examiner’s discretion usually in children with darkly pigmented irides. Retinoscopy was performed with the child wearing retinoscopy spectacles corresponding to the examiner’s working distance to control any residual accommodation. The child was instructed to fixate an animated video target presented at 3 m. The examiner used a lens rack or handheld trial lenses to neutralize the refractive error in each eye. Measurements were obtained along the two principal meridians of each eye. Comprehensive eye examinations were conducted in one of five identical mobile vision units specifically designed for the VIP Study and outfitted with the same testing conditions (e.g. seating, lighting and testing equipment) across all five study centers.12
Astigmatism Definition
The refractive error measures from the comprehensive eye examinations were used to define astigmatism. To facilitate the direct comparison with other studies,8 we defined astigmatism as cylindrical refractive error measured after cycloplegia ≥ 1.5 Diopter (D) in either eye expressed in positive correcting cylinder form. Children with astigmatism were further classified into one of three types of astigmatism including: with-the-rule (plus cylinder axis 90° ± 15°), against-the-rule (plus cylinder axis 180° ± 15°), and oblique (plus cylinder axis 15° – 75° or 105° – 165°).
Risk Factors for Astigmatism
Demographic information (birth date, gender, ethnicity and race) of each child was collected at enrollment based on the information provided by the child’s parent or legal guardian. For easier comparison with other studies,8 race/ethnicity was classified as American Indian, Asian, African American, non-Hispanic White, Hispanic, and other/unknown (for those who reported with more than one race category or those without race information). Age was calculated as the difference between the date of the comprehensive eye examination and the child’s birth date, and was grouped as 36–47 months, 48–59 months, and 60–72 months. Ocular risk factors were defined based on findings from the comprehensive eye examinations. To compare our findings of ocular risk factors with those from other studies,8 we determined refractive error based on the spherical equivalent (SE) of the right eye which was calculated as sphere + ½ * cylinder. We classified refractive error as myopia (≤ −1.0 D in SE), hyperopia (≥ +2.0 D in SE), or emmetropia (>−1.0 D and < +2.0 D in SE). Additional analyses were also performed for refractive error using: (1) the spherical equivalent of the eye with significant astigmatism (or the eye with higher amount of astigmatism if both eyes have astigmatism ≥ 1.5 D); (2) the sphere component of the right eye.
Statistical Analysis
The risk factors for astigmatism were first evaluated using univariate analysis through a logistic regression model. Risk factors with P<0.10 from univariate analyses were included in the multivariate logistic regression models. The multivariate logistic regression models were developed using a backward selection method that removed non-significant risk factors one at a time, and the final model kept only statistically significant risk factors (P<0.05). The odds ratio (OR) and its 95% confidence interval (95% CI) for each of the significant risk factors were calculated from the final multivariate logistic regression model.
To examine the possible nonlinear relationship between the spherical equivalent refractive error and astigmatism, we grouped the refractive error into multiple levels, and the adjusted percentage of astigmatism was calculated for each level of spherical equivalent from the multivariate logistic regression model with adjustment of other risk factors. The percentages of astigmatism vs. levels of spherical equivalent were plotted and an iterative, locally weighted, least squares (LOWESS) curve was generated to show the best fit.14 We also assessed whether the risk factors for astigmatism were associated with the severity of astigmatism by comparing the absolute value of cylindrical refractive error across different levels of risk factors among astigmatic children using analysis of variance. All the statistical analyses were performed using SAS v9.3 (SAS Institute Inc., NC, Cary), and two-sided P<0.05 was considered to be statistically significant.
RESULTS
Characteristics of Study Subjects
Among 4,040 VIP participants, 834 (20.6%) were 3-year-olds, 2158 (53.4%) were 4-year-olds, and 1048 (25.9%) were 5-year-olds. Gender was evenly distributed. Approximately half (51%) of the children were African American, the remaining were Hispanic (20%), non-Hispanic White (12%), American Indian (8.5%), Asian (3.7%), and other (4.5%).
Among 4,040 preschoolers that over-represented children with vision disorders, 687 (17%) had astigmatism of ≥1.5 D in either eye. Out of 687 children with astigmatism, 576 (83.8%) had with-the-rule astigmatism, 37 (5.4%) against-the-rule, and 74 (10.8%) had oblique astigmatism; the proportion of each type of astigmatism did not differ across age group (p=0.24) or ethnic group (p=0.45). With respect to the severity of the astigmatism, 266 (38.7%) participants had astigmatism of 1.5 to < 2.0 D, 279 (40.6%) participants had astigmatism of +2.0 to < +3.0 D, and 142 (20.7%) participants had astigmatism of +3.0 D or greater. The median degree of astigmatism was +2.0 D (range: +1.5 D to +8.7 D), and it did not differ across type of astigmatism, with median degree of astigmatism +2.0 D for both with-the-rule and oblique astigmatism, and +1.75 D for against-the-rule astigmatism.
Risk Factors for Astigmatism
The results from univariate analyses for demographic and ocular risk factors for astigmatism are shown in Table 1. Among children aged 36 to 72 months, older age was marginally associated with an increased risk of astigmatism (linear trend P=0.06). Gender was not associated with astigmatism (P=0.24). Race/ethnicity was significantly associated with astigmatism (P<0.0001). In our study population that over-represented children with vision disorders, the highest percentage of astigmatism was in Hispanic children (22%) and the lowest percentage of astigmatism was in American Indian children (8%). Refractive error was significantly associated with astigmatism (P<0.0001), with the highest percentage of astigmatism in myopic (≤ −1.0 D) children (45%) and hyperopic (≥ +2.0 D) children (21%), and the lowest in children without any myopia or hyperopia (15%).
Table 1.
Univariate Analysis for the Risk Factors of Astigmatism (n=4,040).
| Risk Factors | n | Astigmatism‡ (%§) | Odds ratio (95% confidence interval) | P-value |
|---|---|---|---|---|
| Age at examination (months) | 0.06* | |||
| 36–47 | 834 | 124 (14.9%) | 0.79 (0.62, 1.01) | 0.06 |
| 48–59 | 2158 | 373 (17.3%) | 0.94 (0.78, 1.14) | 0.56 |
| 60–72 | 1048 | 190 (18.1%) | 1.00 | |
|
| ||||
| Gender | 0.24 | |||
| Male | 2012 | 328 (16.3%) | 1.00 | |
| Female | 2028 | 359 (17.7%) | 1.10 (0.94, 1.30) | |
|
| ||||
| Race/Ethnicity | <0.0001 | |||
| Non-Hispanic White | 485 | 55 (11.3%) | 1.00 | |
| African American | 2072 | 362 (17.5%) | 1.66 (1.22, 2.24) | 0.001 |
| Hispanic | 811 | 180 (22.2%) | 2.23 (1.61, 3.09) | <0.0001 |
| Asian | 148 | 27 (18.2%) | 1.75 (1.06, 2.88) | 0.03 |
| American Indian | 343 | 27 (7.9%) | 0.67 (0.41, 1.08) | 0.10 |
| Other/Unknown | 181 | 36 (19.9%) | 1.94 (1.23, 3.08) | 0.005 |
|
| ||||
| Spherical equivalent (right eye) | <0.0001 | |||
| ≤ −1.0 D | 102 | 46 (45.1%) | 4.77 (3.19, 7.14) | <0.0001 |
| > −1.0 D, <2.0 D | 2879 | 423 (14.7%) | 1.00 | |
| ≥2.0 D | 1056 | 217 (20.6%) | 1.50 (1.25, 1.80) | <0.0001 |
| Unknown† | 3 | 1 (33.3%) | ||
Defined using the absolute cylinder, from the eye with larger absolute value of cylinder. †Unknown category was not included in the p-value calculation.
Linear trend P-value.
The percentage did not represent the prevalence of astigmatism, because children with vision disorders were over-represented in the study.
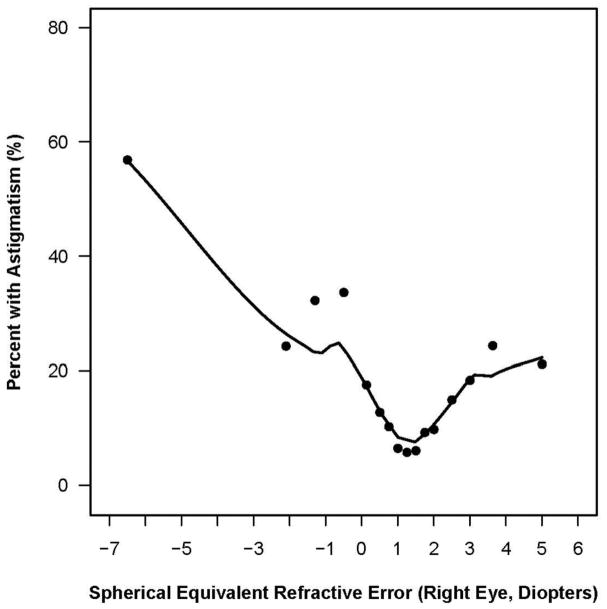
In a multivariate analysis, race/ethnicity and refractive error were independently associated with astigmatism (P<0.0001, Table 2). When compared with non-Hispanic White children, African American, Hispanic and Asian children were significantly associated with an increased risk of astigmatism, with an OR of 1.65 (95% CI: 1.22 – 2.24) for African American, 2.25 (95% CI: 1.62 – 3.12) for Hispanic children, and 1.76 (95% CI: 1.06 – 2.93) for Asian children, respectively. American Indian children were less likely to have astigmatism than Hispanic children (OR=0.31, 95% CI=0.20–0.47), African American (OR=0.42, 95% CI=0.28–0.63), and Asian children (OR=0.39, 95% CI=0.22–0.70). Spherical equivalent refractive error was also significantly associated with astigmatism (P<0.0001). Compared to children without any myopia or hyperopia (>−1.0 D, < +2.0 D in spherical equivalent of right eye), children with either myopia (≤ −1.0 D) or hyperopia (≥ 2.0 D) had an increased risk for astigmatism, with an odds ratio of 4.50 (95% CI: 3.00 – 6.76) for myopia and 1.55 (95% CI: 1.29 – 1.86) for hyperopia. Similar results were found when the myopia and hyperopia were defined using the spherical equivalent of the more astigmatic eye or using sphere component of right eye. When spherical equivalent of the more astigmatic eye was used, the odds ratio was 6.08 (95% CI: 4.09 – 9.03) for myopia (≤ −1.0 D) and 1.55 (95% CI: 1.28 – 1.86) for hyperopia (≥ 2.0 D). When sphere component of right eye was used, the odds ratio was 4.11 (95% CI: 2.56 – 6.63) for myopia (≤ −1.0 D) and 3.21 (95% CI: 2.70 – 3.81) for hyperopia (≥ 2.0 D). The relationship between spherical equivalent refractive error of right eye and astigmatism was nonlinear as shown in Figure 1, which plots the adjusted percentage of astigmatism (from multivariate model) with levels of spherical equivalent for the right eye. The association of race/ethnicity and spherical equivalent with astigmatism was similar when the definition of astigmatism was changed from ≥ 1.5 D to ≥ 2.0 D (data not shown).
Table 2.
Multivariate Analysis for the Risk Factors of Astigmatism (N=4037*)
| Risk Factors | n | Astigmatism (%§) | Odds ratio (95% confidence interval) | P-value |
|---|---|---|---|---|
| Race/Ethnicity | <0.0001 | |||
| Non-Hispanic White | 484 | 55 (11.4%) | 1.00 | |
| African American | 2071 | 361 (17.4%) | 1.65 (1.22, 2.24) | 0.001 |
| Hispanic | 810 | 180 (22.2%) | 2.25 (1.62, 3.12) | <0.0001 |
| Asian | 148 | 27 (18.2%) | 1.76 (1.06, 2.93) | 0.03 |
| American Indian | 343 | 27 (7.9%) | 0.69 (0.43, 1.12) | 0.14 |
| Other/Unknown | 181 | 36 (19.9%) | 2.06 (1.30, 3.27) | 0.002 |
|
| ||||
| Spherical equivalent (right eye) | <0.0001 | |||
| ≤ −1.0 D | 102 | 46 (45.1%) | 4.50 (3.00, 6.76) | <0.0001 |
| > −1.0 D, <2.0 D | 2879 | 423 (14.7%) | 1.00 | |
| ≥ 2.0 D | 1056 | 217 (20.6%) | 1.55 (1.29, 1.86) | <0.0001 |
Three children with missing data in spherical equivalent were excluded.
The percentage did not represent the prevalence of astigmatism, because children with vision disorders were over-represented in the study.
Figure 1.
The non-linear relation of spherical equivalent of right eye with the percentage of astigmatism. The dots represent the percentages with astigmatism at each level of spherical equivalent which were estimated from multivariate logistic regression adjusted by race/ethnicity. The percentages of astigmatism with levels of spherical equivalent were fitted by iterative, locally weighted, least squares (LOWESS) curve.
The multivariate analyses for the risk factors of with-the-rule astigmatism (n=576) showed similar results (Table 3). Compared with the non-Hispanic White children, the OR (95% CI) was 1.58 (1.14 – 2.19) for African American, 2.19 (1.54 – 3.11) for Hispanic children, and 1.67 (0.96 – 2.89) for Asian children, respectively. Both myopia (OR=4.47, 95% CI, 2.91 – 6.88), and hyperopia (OR=1.62, 95% CI, 1.33 – 1.97) were associated with an increased risk of astigmatism. Additionally, 3 years of age was significantly associated with a lower risk for astigmatism (OR = 0.75, 95% CI, 0.57 – 0.99, p=0.04) as compared with 5 years of age. The multivariate analysis for the against-the-rule and oblique-astigmatism could not provide meaningful results due to the small number of astigmatism cases.
Table 3.
Multivariate Analysis for the Risk Factors of With-the-Rule Astigmatism in Preschoolers (N=3927)
| Risk Factors | n | With-the-rule astigmatism† (%§) | Odds ratio (95% Confidence interval) | P-value |
|---|---|---|---|---|
| Race/Ethnicity | <0.0001 | |||
| Non-hispanic White | 477 | 48 (10.0%) | 1.00 | |
| African American | 2010 | 300 (14.9%) | 1.58 (1.14, 2.19) | 0.006 |
| Hispanic | 782 | 152 (19.4%) | 2.19 (1.54, 3.11) | <0.0001 |
| Asian | 143 | 22 (15.4%) | 1.67 (0.96, 2.89) | 0.07 |
| American Indian | 342 | 26 (7.6%) | 0.77 (0.47, 1.27) | 0.31 |
| Other/Unknown | 173 | 28 (16.2%) | 1.86 (1.12, 3.09) | 0.016 |
|
| ||||
| Spherical equivalent (right eye) | <0.0001 | |||
| ≤ −1.0 D | 94 | 38 (40.4%) | 4.47 (2.91, 6.88) | <0.0001 |
| > −1.0 D, <2.0 D | 2805 | 349 (12.4%) | 1.00 | |
| ≥ 2.0 D | 1028 | 189 (18.4%) | 1.62 (1.33, 1.97) | <0.0001 |
|
| ||||
| Age (months) | 0.04 | |||
| 36–47 | 808 | 98 (12.1%) | 0.75 (0.57, 0.99) | 0.04 |
| 48–59 | 2100 | 316 (15.0%) | 0.94 (0.76, 1.16) | 0.57 |
| 60–72 | 1019 | 162 (15.9%) | 1.00 | |
With-the-rule astigmatism was defined as the astigmatism with axis 90° +/− 15°.
The percentage did not represent the prevalence of astigmatism, because children with vision disorders were over-represented in the study.
The Risk Factors for Severity and Degree of Astigmatism
The risk factors for astigmatism were further analyzed for their association with severity of astigmatism and degree of astigmatism among 687children with astigmatism (≥ +1.5 D) (Table 4). Age and race/ethnicity were not associated with either severity or degree of astigmatism (P ≥0.25). Female children were associated with a higher percentage of astigmatism >3.0 D than male children (23.7% vs. 17.4%, P=0.045). More myopic spherical equivalent refractive error was associated with more severe astigmatism (P=0.02, Table 4). Children with myopic astigmatism had the largest mean absolute cylindrical power of +2.74 D, as compared with +2.28 D in emmetropic astigmatism and +2.15 D in hyperopic astigmatism (P<0.0001).
Table 4.
The Comparison of Severity and Degree of Astigmatism among Children with Astigmatism (N=687).
| Astigmatism Severity Level, n (%) | P-value* | Degree of Astigmatism Mean absolute cylindrical power (SE) |
P-value† | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Risk Factors | ≥ 1.5 D, <2 D (n=266) | ≥ 2 D, <3 D (n=279) | ≥ 3 D (n=142) | |||
| Age at examination (months) | ||||||
| 36–47 | 41 (33.1%) | 54 (43.6%) | 29 (23.4%) | 0.61 | 2.35 (0.07) | 0.25 |
| 48–59 | 153 (41.0%) | 147 (39.4%) | 73 (19.6%) | 2.23 (0.04) | ||
| 60–72 | 72 (37.9%) | 78 (41.1%) | 40 (21.1%) | 2.31 (0.07) | ||
|
| ||||||
| Gender | ||||||
| Male | 124 (37.8%) | 147 (44.8%) | 57 (17.4%) | 0.045 | 2.24 (0.05) | 0.28 |
| Female | 142 (39.6%) | 132 (36.8%) | 85 (23.7%) | 2.31 (0.04) | ||
|
| ||||||
| Ethnicity/Race | 0.57 | 0.99 | ||||
| Non-Hispanic White | 19 (34.6%) | 26 (47.3%) | 10 (18.2%) | 2.29 (0.11) | ||
| African American | 152 (42.0%) | 132 (36.5%) | 78 (21.6%) | 2.27 (0.05) | ||
| Hispanic | 68 (37.8%) | 77 (42.8%) | 35 (19.4%) | 2.25 (0.06) | ||
| Asian | 6 (22.2%) | 14 (51.9%) | 7 (25.9%) | 2.36 (0.13) | ||
| American Indian | 9 (33.3%) | 13 (48.2%) | 5 (18.5%) | 2.31 (0.16) | ||
| Other/Unknown | 12 (33.3%) | 17 (47.2%) | 7 (19.4%) | 2.24 (0.10) | ||
|
| ||||||
| Spherical Equivalent (right eye) | 0.02 | <0.0001 | ||||
| ≤ −1.0 D | 13 (28.3%) | 15 (32.6%) | 18 (39.1%) | 2.74 (0.20) | ||
| > −1.0 D, <2.0 D | 158 (37.4%) | 177 (41.8%) | 88 (20.8%) | 2.28 (0.04) | ||
| ≥ 2.0 D | 95 (43.8%) | 86 (39.6%) | 36 (16.6%) | 2.15 (0.05) | ||
SE=Standard error.
From Chi-square test.
From one way analysis of variance.
DISCUSSION
This study evaluated demographic and ocular risk factors for astigmatism among 3- to 5-year old preschoolers in five geographic areas, and quantified the magnitude of association with astigmatism. Our study showed that African American, Hispanic and Asian children had a higher risk for astigmatism than other racial/ethnic groups, and that spherical refractive error (either myopia or hyperopia) was associated with an increased risk of astigmatism. Our results, which over-represented children at risk for vision problems, are consistent with findings from previous population-based studies that established a strong association between race/ethnicity, refractive error and astigmatism based on a pooled analysis of data from the two largest population-based pediatric eye disease studies in the US (MEPEDS and BPEDS).8
Among VIP Study participants from disparate racial/ethnic groups including African American, American Indian, Asian, Hispanic, and non-Hispanic White, we found that African American, Hispanic and Asian children had a higher risk for astigmatism than non-Hispanic White children, while American Indian children had a lower risk for astigmatism than Hispanic, African American and Asian children. We previously reported that American Indian children had the lowest prevalence rate of astigmatism (4.28%), which was statistically significantly lower than that of Hispanic children (11.1%) and African American (8.4%).9 In contrast to the high risk of astigmatism among preschoolers reported in several American Indian tribes in Arizona,13 the risk of astigmatism was lower in our population of American Indians, the majority of whom live in northeastern Oklahoma and represent many tribes. This suggests that risk of astigmatism may vary among tribes of American Indians.
We found that spherical equivalent refractive error was strongly associated with astigmatism. Children with myopia (≤ −1.0 D) were 4.4 times more likely to have astigmatism than children without significant refractive error (>−1.0 D to < +2.0 D), whereas children with hyperopia (≥ +2.0 D) were 1.5 times more likely to have astigmatism. In spite of a higher percentage of astigmatism in our study (17%) as compared to MEPEDS/BPEDS (10%) due to an over-sampling of children with vision disorders, the associations found from the VIP Study were extremely similar to those from MEPEDS/BPEDS (Table 5), which reported odds ratio of 4.6 for myopia (≤ −1.0 D) and 1.6 for hyperopia (≥ +2.0 D). Because both our study and MEPEDS/BPEDS were cross-sectional, we can conclude that children with refractive error were more likely to have astigmatism than children without refractive error, but we cannot further determine a causal relationship.
Table 5.
Comparisons between the VIP Study and the MEPEDS/BPEDS.
| VIP Study | MEPEDS/BPEDS | |
|---|---|---|
| Characteristics of Study | ||
|
| ||
| Population-based | No | Yes |
|
| ||
| Participants (N) | 4,040 | 8,579 |
|
| ||
| With astigmatism (n, %) | 687 (17%) | 859 (10%) |
|
| ||
| Age of participants (months) | 36–72 | 6–72 |
|
| ||
| Race (%) | ||
| Non-Hispanic White | 12% | 22% |
| African American | 51% | 43% |
| Hispanic | 20% | 35% |
| Asian | 4% | 0% |
| American Indian | 9% | 0% |
| Other/Unknown | 4% | 0% |
| Risk factors of Astigmatism | Odds ratios in the VIP Study | Odds ratios in MEPEDS/BPEDS |
|---|---|---|
| Spherical equivalent Refractive Error | ||
| > −1.0 D, <2.0 D | 1.00 | 1.00 |
| ≤ −1.0 D | 4.44 (2.95, 6.67) | 4.61 (3.56, 5.96) |
| ≥ 2.0 D | 1.54 (1.28, 1.85) | 1.64 (1.39, 1.94) |
|
| ||
| Race/ethnicity | ||
| Non-Hispanic White | 1.00 | 1.00 |
| African American | 1.66 (1.22, 2.25) | 1.47 (1.18, 1.85) |
| Hispanic | 2.25 (1.62, 3.12) | 2.38 (1.91, 2.97) |
| Asian | 1.79 (1.08, 2.97) | NA |
| American Indian | 0.70 (0.43, 1.13) | NA |
| Other/Unknown | 2.08 (1.31, 3.30) | NA |
|
| ||
| Age of participants (months) | ||
| 36–47 | 0.81 (0.63, 1.05) | 0.85 (0.66, 1.11) |
| 48–59 | 0.95 (0.78, 1.16) | 0.93 (0.72, 1.20) |
| 60–72 | 1.00 | 1.00 |
|
| ||
| Maternal smoking during pregnancy: Yes vs. No | NA | 1.47 (1.18, 1.85) |
NA = Not Available.
MEPEDS = Multi-ethnic Pediatric Eye Disease Study.
BPEDS = Baltimore Pediatric Eye Disease Study.
In contrast to MEPEDS/BPEDS, this study further evaluated the association of factors with severity and degree of astigmatism. We found that although African American, Hispanic and Asian children had an increased risk of astigmatism compared to non-Hispanic White children, the increased risk was not associated with either severity or degree of astigmatism. Although the risk of astigmatism was lower in American Indian children than Hispanic children, their severity and degree of astigmatism were similar. However, for all racial/ethnic groups, myopic spherical equivalent was associated with both an increased risk and more severe astigmatism.
The strengths of this study include standardized comprehensive eye examinations performed by study-certified optometrists and ophthalmologists. All refractive error measures were performed using cycloplegic retinoscopy in a standardized setting. This study included a large sample of preschool children from a variety of race/ethnicity groups (African American, Asian, Hispanic, non-Hispanic White, and American Indian) and across a wide geographic area within the United States. The enriched sample over-representing preschool children with vision disorders provided a large number of astigmatism cases.
A few limitations in the analyses should be acknowledged. First, all the VIP Study participants were enrolled from Head Start programs, a national, comprehensive child development program that serves low-income preschool children and families, and the children with vision disorders were over-represented. It is uncertain whether these findings can therefore be generalized to a wider population of preschool children. However, the results from this study are consistent with findings from population-based studies. Secondly, because the VIP Study was not originally designed to evaluate the risk factors of astigmatism, the risk factors collected in the VIP Study were not comprehensive. Only a few demographic characteristics and ocular risk factors were included. The MEPEDS/BPEDS Studies performed more comprehensive evaluations of risk factors including demographic, clinical, environmental, behavioral and ocular risk factors. Besides race/ethnicity and refractive error, MEPEDS/BPEDS Studies also found child’s age (particularly in the group of age <12 months) and maternal smoking during pregnancy were risk factors for astigmatism.
In summary, among Head Start preschoolers, Hispanic ethnicity, African American and Asian race, as well as myopic and hyperopic refractive error were each independently associated with an increased risk of astigmatism. American Indian children were associated with a lower risk of astigmatism.
Acknowledgments
Supported by NEI/NIH, DHHS grants: U10EY12644; U10EY12547; U10EY12545; U10EY12550; U10EY12534; U10EY12647; U10EY12648 and R21EY018908. We thank Velma Dobson, PhD, who passed away in 2010, for her invaluable contributions to the VIP Study.
The Vision in Preschoolers (VIP) Study Group
Executive Committee: Paulette Schmidt, OD, MS (Chair); Agnieshka Baumritter, MA; Elise Ciner, OD; Lynn Cyert, PhD, OD; Velma Dobson, PhD; Beth Haas; Marjean Taylor Kulp, OD, MS; Maureen Maguire, PhD; Bruce Moore, OD; Deborah Orel-Bixler, PhD, OD; Ellen Peskin, MA; Graham Quinn, MD, MSCE; Maryann Redford, DDS, MPH; Janet Schultz, RN, MA, CPNP; Gui-shuang Ying, PhD.
Participating Centers
(AA)=Administrative Assistant (BPC)=Back-up Project Coordinator; (GSE)=Gold Standard Examiner for comprehensive vision examinations; (LS)=Lay Screener; (NS)=Nurse Screener; (PI)=Principal Investigator; (PC)=Project Coordinator; (PL)=Parent Liaison; (PR)=Programmer; (VD)=Van Driver; (NHC)=Nurse/Health Coordinator.
Berkeley, CA: University of California Berkeley School of Optometry
Deborah Orel-Bixler, PhD, OD (PI/GSE); Pamela Qualley, MA (PC); Dru Howard (BPC/PL); Lempi Miller Suzuki (BPC); Sarah Fisher, PhD, OD (GSE); Darlene Fong, OD (GSE); Sara Frane, OD (GSE); Cindy Hsiao-Threlkeld, OD (GSE); Selim Koseoglu, MD (GSE); A. Mika Moy, OD (GSE); Sharyn Shapiro, OD (GSE); Lisa Verdon, OD (GSE); Tonya Watson, OD (GSE); Sean McDonnell (LS/VD); Erika Paez (LS); Darlene Sloan (LS); Evelyn Smith (LS); Leticia Soto (LS); Robert Prinz (LS); Joan Edelstein, RN (NS); Beatrice Moe, RN (NS).
Boston, MA: New England College of Optometry
Bruce Moore, OD (PI/GSE); Joanne Bolden (PC); Sandra Umaña (PC/LS/PL); Amy Silbert (BPC); Nicole Quinn, OD (GSE); Heather Bordeau, OD (GSE); Nancy Carlson, OD (GSE); Amy Croteau, OD (GSE); Micki Flynn, OD (GSE); Barry Kran, OD (GSE); Jean Ramsey, MD (GSE); Melissa Suckow, OD (GSE); Erik Weissberg, OD (GSE); Marthedala Chery (LS/PL); Maria Diaz (LS); Leticia Gonzalez (LS/PL); Edward Braverman (LS/VD); Rosalyn Johnson (LS/PL); Charlene Henderson (LS/PL); Maria Bonila (PL); Cathy Doherty, RN (NS); Cynthia Peace-Pierre, RN (NS); Ann Saxbe, RN (NS); Vadra Tabb, RN (NS).
Columbus, OH: The Ohio State University College of Optometry
Paulette Schmidt OD, MS (PI); Marjean Taylor Kulp, OD, MS (Co-Investigator/GSE); Molly Biddle, MA (PC); Jason Hudson (BPC); Melanie Ackerman, OD (GSE); Sandra Anderson, OD (GSE); Michael Earley, OD, PhD (GSE); Kristyne Edwards, OD, MS (GSE); Nancy Evans, OD (GSE); Heather Gebhart, OD (GSE); Jay Henry, OD, MS (GSE); Richard Hertle, MD (GSE); Jeffrey Hutchinson, DO (GSE); LeVelle Jenkins, OD (GSE); Andrew Toole, OD, MS (GSE); Keith Johnson (LS/VD); Richard Shoemaker (VD); Rita Atkinson (LS); Fran Hochstedler (LS); Tonya James (LS); Tasha Jones (LS); June Kellum (LS); Denise Martin (LS); Christina Dunagan, RN (NS); Joy Cline, RN (NS); Sue Rund, RN (NS).
Philadelphia, PA: Pennsylvania College of Optometry at Salus UniversityI
Elise Ciner, OD (PI/GSE); Angela Duson (PC/LS); Lydia Parke (BPC); Mark Boas, OD (GSE); Shannon Burgess, OD (GSE); Penelope Copenhaven, OD (GSE); Ellie Francis, PhD, OD (GSE); Michael Gallaway, OD (GSE); Sheryl Menacker, MD (GSE); Graham Quinn, MD, MSCE (GSE); Janet Schwartz, OD (GSE); Brandy Scombordi-Raghu, OD (GSE); Janet Swiatocha, OD (GSE); Edward Zikoski, OD (GSE); Leslie Kennedy (LS/PL); Rosemary Little (LS/PL); Geneva Moss (LS/PL); Latricia Rorie (LS); Shirley Stokes (LS/PL); Jose Figueroa (LS/VD); Eric Nesmith (LS); Gwen Gold (BPC/NHC/PL); Ashanti Carter (PL); David Harvey (LS/VD); Sandra Hall, RN (NS); Lisa Hildebrand, RN (NS); Margaret Lapsley, RN (NS); Cecilia Quenzer, RN (NS); Lynn Rosenbach, RN (NHC/NS).
Tahlequah, OK: Northeastern State University College of Optometry
Lynn Cyert, PhD, OD (PI/GSE); Linda Cheatham (PC/VD); Anna Chambless (BPC/PL); Colby Beats, OD (GSE); Jerry Carter, OD (GSE); Debbie Coy, OD (GSE); Jeffrey Long, OD (GSE); Shelly Rice, OD (GSE); Shelly Dreadfulwater, (LS/PL); Cindy McCully (LS/PL); Rod Wyers (LS/VD); Ramona Blake (LS/PL); Jamey Boswell (LS/PL); Anna Brown (LS/PL); Jeff Fisher, RN (NS); Jody Larrison, RN (NS).
Study Center
Columbus, OH: The Ohio State University College of Optometry: Paulette Schmidt, OD, MS (PI); Beth Haas (Study Coordinator).
Coordinating Center
Philadelphia, PA: University of Pennsylvania, Department of Ophthalmology: Maureen Maguire, PhD (PI); Agnieshka Baumritter, MA (Project Director); Mary Brightwell-Arnold (Systems Analyst); Christine Holmes (AA); Andrew James (PR); Aleksandr Khvatov (PR); Lori O’Brien (AA); Ellen Peskin, MA (Project Director); Claressa Whearry (AA); Gui-shuang Ying, PhD (Biostatistician).
National Eye Institute
Bethesda, MD: Maryann Redford, DDS, MPH
References
- 1.Read SA, Collins MJ, Carney LG. A review of astigmatism and its possible genesis. Clin Exp Optom. 2007;90:5–19. doi: 10.1111/j.1444-0938.2007.00112.x. [DOI] [PubMed] [Google Scholar]
- 2.Abrahamsson M, Sjostrand J. Astigmatic axis and amblyopia in childhood. Acta Ophthalmol Scand. 2003;81:33–7. doi: 10.1034/j.1600-0420.2003.00022.x. [DOI] [PubMed] [Google Scholar]
- 3.Brown SA, Weih LM, Fu CL, Dimitrov P, Taylor HR, McCarty CA. Prevalence of amblyopia and associated refractive errors in an adult population in Victoria, Australia. Ophthalmic Epidemiol. 2000;7:249–58. [PubMed] [Google Scholar]
- 4.Fulton AB, Hansen RM, Petersen RA. The relation of myopia and astigmatism in developing eyes. Ophthalmology. 1982;89:298–302. doi: 10.1016/s0161-6420(82)34788-0. [DOI] [PubMed] [Google Scholar]
- 5.Gwiazda J, Grice K, Held R, McLellan J, Thorn F. Astigmatism and the development of myopia in children. Vision Res. 2000;40:1019–26. doi: 10.1016/s0042-6989(99)00237-0. [DOI] [PubMed] [Google Scholar]
- 6.Tong L, Saw SM, Carkeet A, Chan WY, Wu HM, Tan D. Prevalence rates and epidemiological risk factors for astigmatism in Singapore school children. Optom Vis Sci. 2002;79:606–13. doi: 10.1097/00006324-200209000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Pascual M, Huang J, Maguire MG, Kulp MT, Quinn GE, Ciner E, Cyert LA, Orel-Bixler D, Moore B, Ying GS. Risk factors for amblyopia in the Vision in Preschoolers Study. Ophthalmology. 2013 Oct 18; doi: 10.1016/j.ophtha.2013.08.040. epub ahead of print. [DOI] [Google Scholar]
- 8.McKean-Cowdin R, Varma R, Cotter SA, Tarczy-Hornoch K, Borchert MS, Lin JH, Wen G, Azen SP, Torres M, Tielsch JM, Friedman DS, Repka MX, Katz J, Ibironke J, Giordano L. Risk factors for astigmatism in preschool children: the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology. 2011;118:1974–81. doi: 10.1016/j.ophtha.2011.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ying GS, Maguire MG, Cyert LA, Ciner E, Quinn GE, Kulp MT, Orel-Bixler D, Moore B. Prevalence of vision disorders by racial and ethnic group among children participating in Head Start. Vision in Preschoolers Study Group. Ophthalmology. 2013 Oct 13; doi: 10.1016/j.ophtha.2013.09.036. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schmidt P, Maguire M, Dobson V, Quinn G, Ciner E, Cyert L, Kulp MT, Moore B, Orel-Bixler D, Redford M, Ying GS. Comparison of preschool vision screening tests as administered by licensed eye care professionals in the Vision in Preschoolers Study. Vision in Preschoolers Study Group. Ophthalmology. 2004;111:637–50. doi: 10.1016/j.ophtha.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 11.Vision in Preschoolers Study Group. Preschool vision screening tests administered by nurse screeners compared with lay screeners in the vision in preschoolers study. Invest Ophthalmol Vis Sci. 2005;46:2639–48. doi: 10.1167/iovs.05-0141. [DOI] [PubMed] [Google Scholar]
- 12.Vision In Preschoolers (VIP) Study Group. Implementation of a preschool vision screening program in a mobile setting. The NHSA Dialog. 2005;8:16–24. [Google Scholar]
- 13.Harvey EM, Dobson V, Clifford-Donaldson CE, Green TK, Messer DH, Miller JM. Prevalence of astigmatism in Native American infants and children. Optom Vis Sci. 2010;87:400–5. doi: 10.1097/OPX.0b013e3181d95b23. [DOI] [PubMed] [Google Scholar]
- 14.Cleveland WS, Grosse E. Computational methods for local regression. Stat Comput. 1991;1:47–62. [Google Scholar]