Abstract
Massive pulmonary embolism is associated with mortality rates exceeding 50%. Current practice guidelines include the immediate administration of thrombolytic therapy in the absence of contraindications. However, thrombolysis for pulmonary embolism is said to be absolutely contraindicated in the presence of recent hemorrhagic stroke and other conditions. The current contraindications to thrombolytic therapy have been extrapolated from data on acute coronary syndrome and are not specific for venous thromboembolic disease. Some investigators have proposed that the current contraindications be viewed as relative, rather than absolute, in cases of high-risk pulmonary embolism.
We present the case of a 60-year-old woman in whom massive pulmonary embolism led to cardiac arrest with pulseless electrical activity. Eight weeks earlier, she had sustained a hemorrhagic cerebrovascular accident—a classic absolute contraindication to thrombolytic therapy. Despite this practice guideline, we administered tissue plasminogen activator systemically in order to save the patient's life. This therapy did not evoke intracranial bleeding, and the patient was eventually discharged from the hospital. Until guidelines specific to venous thromboembolic disease are developed, we think that the current contraindications to thrombolysis should be considered on an individual basis in patients who are at high risk of death from massive pulmonary embolism.
Keywords: Evidence-based medicine, heart arrest/therapy, practice guidelines as topic, pulmonary embolism/complications/drug therapy, risk assessment, thrombolytic therapy/methods, tissue plasminogen activator/con-traindications/therapeutic use, treatment outcome
When massive pulmonary embolism (PE) results in hemodynamic compromise, the mortality rate is 50% to 100%.1,2 In these emergent cases, the current practice guidelines include immediate thrombolysis, in the absence of contraindications such as hemorrhagic stroke.3,4 However, there are no clear therapeutic guidelines for treating high-risk PE when thrombolytic therapy is said to be contraindicated. In such cases, investigators have proposed that the contraindications be viewed as relative rather than absolute.2,4 We discuss our therapeutic decisions, and their results, in the case of a patient who had massive PE and a recent history of hemorrhagic stroke.
Case Report
In February 2012, a 60-year-old woman who had sustained a hemorrhagic cerebrovascular accident (CVA) 8 weeks earlier presented with acute lethargy, blurred vision, hypotension, and bradycardia. An electrocardiogram revealed a junctional rhythm. A bedside echocardiogram revealed right ventricular (RV) dilation and dysfunction, and pulmonary hypertension. Further evaluation yielded deep vein thrombosis in the right lower extremity, and results of a ventilation/perfusion scan suggested an intermediate probability of PE. Anticoagulation with heparin was initiated for PE with hemodynamic compromise, and dobutamine was started for RV failure. The placement of an inferior vena cava filter was planned.
On the 3rd day of hospitalization, the patient had 2 episodes of cardiac arrest with pulseless electrical activity. After the first resuscitation, an electrocardiogram showed atrial tachycardia, right bundle branch block, a large Q wave in lead III, and mild ST-segment elevation. A chest radiograph revealed left-lower-lobe atelectasis that obscured the left border of the heart, and an area of aerated but hypovolemic lung that was consistent with a Westermark sign. A bedside echocardiogram showed worsening RV dilation and systolic dysfunction, pulmonary hypertension, and a severely under-filled left ventricle (Fig. 1).
Fig. 1.
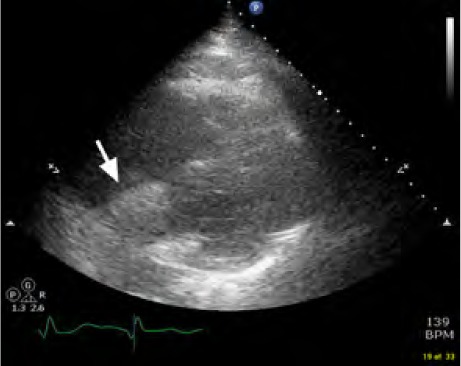
Transthoracic echocardiogram (parasternal short-axis view) at the mid-papillary level shows right ventricular dilation (arrow) with a severely under-filled left ventricle and pulmonary hypertension.
The patient was intubated and supported with mechanical ventilation. Tenuous hemodynamic stability was attained with the addition of multiple vasoactive medications (norepinephrine, epinephrine, and vasopressin). After consultation with the pulmonary critical care specialist, cardiac surgeon, and interventional radiologist, we decided to use systemic tissue plasminogen activator (tPA) infusion, despite the classic consideration of prior hemorrhagic CVA as an absolute contraindication to that therapy. Within one hour after the patient's 2nd cardiac arrest, we administered tPA as a 10-mg bolus and 90-mg infusion. The patient had no subsequent cardiac arrest.
Approximately 3 hours after the tPA infusion, computed tomograms and angiograms of the chest confirmed the diagnosis of massive PE, with the involvement of 5 pulmonary artery segments and signs of right-sided heart strain (Fig. 2). Computed tomograms revealed no signs of new intracranial bleeding. The patient's hemodynamic status gradually improved during the 72 hours after tPA infusion. The vasoactive medications were discontinued, and she was extubated. After tPA infusion, the patient developed rectal, vaginal, and line-insertion-site bleeding with secondary anemia that necessitated multiple red blood cell transfusions. An inferior vena cava filter was placed, and chronic warfarin therapy was initiated. The patient was referred for inpatient physical rehabilitation before her discharge from the hospital. She was lost to follow-up thereafter.
Fig. 2.

Chest computed tomogram shows large filling defects (arrows) in the right and left main pulmonary arteries.
Discussion
High-risk PE is defined as PE with RV failure that causes shock and either a systolic blood pressure of less than 90 mmHg or a pressure drop of at least 40 mmHg that lasts 15 minutes or longer.2 Thrombolysis is beneficial in such cases and is recommended as first-line therapy, in the absence of contraindications.2–4
No specific contraindications to thrombolysis have been determined for patients with venous thromboembolic disease—the existing guidelines were extrapolated from the contraindications to thrombolysis in acute coronary syndrome.2 Two such contraindications are any ischemic CVA in the preceding 3 months and any history of hemorrhagic CVA. Of note, patients who have had a recent CVA are at particular risk of venous thromboembolism; in fact, PE is the primary cause of death 2 to 4 weeks after a CVA.5 Additional contraindications are a history of central nervous system lesions, active bleeding, recent brain or spinal surgery, recent major trauma, and any bleeding disorder.
Local thrombolysis has not proved to be particularly beneficial. The direct infusion of tPA has not increased the rate of thrombolysis and has been associated with bleeding complications at the catheter insertion site.6 In addition, the contraindications are the same for both local and systemic thrombolysis. Endovascular and surgical embolectomy are typically less dangerous than thrombolytic therapy; however, these techniques are not yet widely available.7 Surgical embolectomy is often considered to be too risky for severely decompensated patients, such as ours.
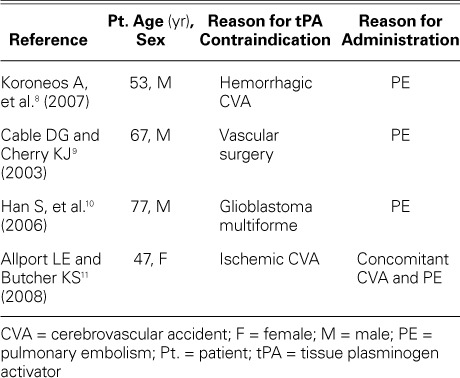
In one report,8 systemic thrombolysis for massive PE was used with success in a patient who had recently had a hemorrhagic stroke, and other reports9–11 have described the successful use of thrombolytic agents in patients with high-risk PE and other seemingly absolute contraindications (Table I). These cases suggest the need for disease-specific guidelines and contraindications to thrombolysis in patients with venous thromboembolism. The mortality rate in high-risk PE exceeds 50%, so the risk of a poor outcome secondary to hemorrhage might outweigh the high risk of death without thrombolytic therapy. Until the results of future investigation elucidate disease-specific guidelines, a case-by-case approach is conceivably best in patients with high-risk PE.
TABLE I.
Case Reports of Successful tPA Use in the Presence of Contraindications
References
- 1.Jerjes-Sanchez C, Ramirez-Rivera A, de Lourdes Garcia M, Arriaga-Nava R, Valencia S, Rosado-Buzzo A et al. Streptokinase and heparin versus heparin alone in massive pulmonary embolism: a randomized controlled trial. J Thromb Thrombolysis. 1995;2(3):227–9. doi: 10.1007/BF01062714. [DOI] [PubMed] [Google Scholar]
- 2.Meneveau N. Therapy for acute high-risk pulmonary embolism: thrombolytic therapy and embolectomy. Curr Opin Cardiol. 2010;25(6):560–7. doi: 10.1097/HCO.0b013e32833f02c5. [DOI] [PubMed] [Google Scholar]
- 3.Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ et al. Antithrombotic therapy for VTE disease: Antithrombotic therapy and prevention of thrombosis, 9th ed.: American College of Chest Physicians evidence-based clinical practice guidelines [published erratum appears in Chest 2012;142(6):1698–704] Chest. 2012;141(2 Suppl):e419S–94S. doi: 10.1378/chest.11-2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Torbicki A, Perrier A, Konstantinides S, Agnelli G, Galie N, Pruszczyk P et al. Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC) Eur Heart J. 2008;29(18):2276–315. doi: 10.1093/eurheartj/ehn310. [DOI] [PubMed] [Google Scholar]
- 5.Harvey RL. Prevention of venous thromboembolism after stroke. Top Stroke Rehabil. 2003;10(3):61–9. doi: 10.1310/54NU-U4CP-5KC8-JM9W. [DOI] [PubMed] [Google Scholar]
- 6.Imberti D, Maraldi C, Gallerani M. Interventional approaches in VTE treatment (vena cava filters, catheter-guided thrombolysis, thrombosuction) Semin Respir Crit Care Med. 2012;33(2):176–85. doi: 10.1055/s-0032-1311796. [DOI] [PubMed] [Google Scholar]
- 7.Lin PH, Chen H, Bechara CF, Kougias P. Endovascular interventions for acute pulmonary embolism. Perspect Vasc Surg Endovasc Ther. 2010;22(3):171–82. doi: 10.1177/1531003510379880. [DOI] [PubMed] [Google Scholar]
- 8.Koroneos A, Koutsoukou A, Zervakis D, Politis P, Sourlas S, Pagoni E, Roussos C. Successful resuscitation with thrombolysis of a patient suffering fulminant pulmonary embolism after recent intracerebral haemorrhage. Resuscitation. 2007;72(1):154–7. doi: 10.1016/j.resuscitation.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 9.Cable DG, Cherry KJ. Systemic thrombolytic therapy after recent abdominal aortic aneurysm repair: an absolute contra-indication? Mayo Clin Proc. 2003;78(1):99–102. doi: 10.4065/78.1.99. [DOI] [PubMed] [Google Scholar]
- 10.Han S, Chaya C, Hoo GW. Thrombolytic therapy for massive pulmonary embolism in a patient with a known intracranial tumor. J Intensive Care Med. 2006;21(4):240–5. doi: 10.1177/0885066606287047. [DOI] [PubMed] [Google Scholar]
- 11.Allport LE, Butcher KS. Thrombolysis for concomitant acute stroke and pulmonary embolism. J Clin Neurosci. 2008;15(8):917–20. doi: 10.1016/j.jocn.2007.03.026. [DOI] [PubMed] [Google Scholar]


