Abstract
Our ability to adapt to change is fundamental. The cortisol awakening response (CAR) is a sharp rise in cortisol 30-minutes after waking to help prepare an individual for ensuing stress. Children with autism spectrum disorder (ASD) often have difficulty adapting to change. Exploration of the CAR is warranted; yet, the few studies investigating it are inconclusive. The CAR was investigated in 94 pre-pubertal male children 8-to-12 years of age with ASD (46) and typical development (TD, 48). Salivary samples were collected over three diurnal cycles involving two morning samples: M1: Immediately upon Waking and M2: 30-min Post Waking (M2 − M1 = CAR). The magnitude of the CAR was measured by independent two sample t-tests, variability was measured using Levene's Test, the sequence of the CAR was analyzed by a linear mixed-effects model and proportion of children exhibiting a CAR by chi-square test of independence. There were no significant differences on the CAR between the groups based on magnitude (t(92) = −0.14, p = 0.89, d = 0.04), variability (F(45,47) = 1.11, p = 0.72, η2=0.11) or the sequence over three days (F(2,88) = 0.26, p = 0.77, η2=0.01). No significant differences were shown in the proportion of children exhibiting a CAR across the groups based on child (χ2(1) = 0.02, p = 0.89) or adult criterion (χ2(1) = 1.82, p = 0.18). Despite group differences in the regulation and responsivity of cortisol, the CAR is indistinguishable between children with and without ASD. Inconsistencies across studies may be due to age, criterion used, and diagnostic distinctions.
Keywords: autism, ASD, cortisol, CAR, development, children, adolescence, HPA
INTRODUCTION
Our ability to prepare and adapt to the environment is fundamental to human existence. The start of the day is a critical time in which physiological arousal may be necessary to prepare the individual for the day and potential stress. The cortisol awakening response (CAR) is a sharp increase of 38–75% of blood levels of cortisol, which occurs in an estimated 77% of individuals, although there is significant inter- and intra-individual variability (Pruessner et al., 1997; Wust et al., 2000). This rise in circulating cortisol approximately 30-minutes after waking is distinct from the normal circadian rhythm (Pruessner, et al., 1997) and has been hypothesized to be related to the act of waking (Fries, Dettenborn, & Kirschbaum, 2009; Wilhelm, Born, Kudielka, Schlotz, & Wust, 2007).
The CAR is a measure of the “reactive capacity” of the hypothalamic pituitary adrenal (HPA) axis (Schmidt-Reinwald et al., 1999). The presence of the CAR is deemed preparatory allowing the organism to temper the body for upcoming challenges (Fries, et al., 2009). This alerting mechanism appears largely driven by the hippocampus preparing the HPA axis for arousal and stress (Buchanan, Kern, Allen, Tranel, & Kirschbaum, 2004), which may be accompanied by memory representations upon waking that allow orientation to self, place, time and personal demands (Fries, et al., 2009).
The CAR has been positively associated with psychological and physical well-being (Clow, Thorn, Evans, & Hucklebridge, 2004; Fries, et al., 2009; Griefahn & Robens, 2008; Liberzon, Abelson, King, & Liberzon, 2008; Pruessner, et al., 1997). Conversely, the CAR has been implicated in a number of medical and psychiatric disorders including depression (Kuehner, Holzhauer, & Huffziger, 2007) and psychosis (e.g., (Pruessner, Vracotas, Joober, Pruessner, & Malla, 2013).
While previous studies suggest that the CAR is robust and reliable based on age in children and adults (Pruessner, et al., 1997; Wust, Wolf, et al., 2000), developmental changes may influence the presence and magnitude of the CAR especially during adolescence (Gunnar, Wewerka, Frenn, Long, & Griggs, 2009; Kudielka & Kirschbaum, 2003). In adults the CAR has been defined as a significant rise in cortisol of 2.49 nmol or greater (Wust, Wolf, et al., 2000). However, since children seldom reach this level, any rise in cortisol suggests the presence of an awakening response (Rosmalen et al., 2005). Recently in a large population-based study, adolescents were shown to have stable cortisol levels upon waking; however, the mean levels post-waking increased significantly over the adolescent years (Platje et al., 2012). Thus, pubertal development is an important consideration when examining the HPA axis in children and adolescents (Gunnar, et al., 2009).
Morning cortisol concentrations and thus the CAR, are thought to be largely genetically determined based on heritability of daytime cortisol, (Bartels, de Geus, Kirschbaum, Sluyter, & Boomsma, 2003; Bartels, Van den Berg, Sluyter, Boomsma, & de Geus, 2003; Veen et al., 2011). However, a recent review highlights that in addition to the influence of trait variables, a number of state variables can impact the CAR and thereby daily functioning (Law, Hucklebridge, Thorn, Evans, & Clow, 2013). For example, in healthy persons there is a positive correlation between the magnitude of the CAR and increased ambient light in the morning, anticipation of a demanding day, and negative events experienced the day before (see comprehensive review (Law, et al., 2013). Moreover, the CAR can be moderated by different sleep patterns, such as awaking earlier (Federenko et al., 2004), shift work (Griefahn & Robens, 2008; Kudielka, Buchtal, Uhde, & Wust, 2007) and differences in light (Figueiro & Rea, 2012; Thorn, Hucklebridge, Esgate, Evans, & Clow, 2004).
Autism spectrum disorder (ASD) is characterized by impairment in social communication, a pattern of repetitive and restrictive behavior, and is four times more prevalent in boys (APA, 2013). Individuals with autism spectrum disorders (ASD) have long been shown to adapt poorly to novel and rapidly changing situations (Kanner, 1943). As such, investigations have been conducted to determine the stability of the HPA axis revealing heightened reactivity based on different stressors (Corbett, Mendoza, Abdullah, Wegelin, & Levine, 2006; Corbett, Schupp, & Lanni, 2012; Richdale & Prior, 1992; Tordjman et al., 1997). While basal cortisol levels are largely stable, significant variability in characteristics of the diurnal cycle have been reported (Corbett, et al., 2006; Corbett, Mendoza, Wegelin, Carmean, & Levine, 2008; Richdale & Prior, 1992). For example, children with autism exhibited a flattening of the diurnal slope over time evidenced by diminishing morning cortisol and elevated evening cortisol values (Corbett, et al., 2008), which were associated with sensory sensitivity and poor adaptation to changes, respectively (Corbett, Schupp, Levine, & Mendoza, 2009).
To date, only two investigations have been conducted to assess the frequency and magnitude of the CAR in children and adolescents with ASD. One study (Brosnan, Turner-Cobb, Munro-Naan, & Jessop, 2009) examined the frequency of the CAR in a group of 20 adolescent males with Asperger Syndrome (AS) from an institutional setting compared to 18 typically developing (TD) youth from the community. Participants were male, 11 to 16 years and medication free. Samples were collected over two days via passive drool upon being awakened, 30-min after awakening, and one hour before bedtime. The results showed that the CAR was present in 72% of the TD group and 60% of the AS group, which was not statistically significant χ2(1)= 0.63, p > 0.05). However, using the adult criterion, the CAR was evident in 28% of the TD group and essentially absent in the AS group with only 5% showing a response and a reported significant difference between the groups (χ2(1)= 3.70, p = 0.03). The authors speculated that the reported blunted CAR might contribute to the poor response to change. Developmental factors, however, may play a role.
Recently, Zinke and colleagues (Zinke, Fries, Kliegel, Kirschbaum, & Dettenborn, 2010) investigated the CAR in a group of 15 children with high-functioning autism (HFA) compared to 25 TD children, 6 to 12 years of age. Samples were collected from the home over two days and averaged. Parents were instructed to wake their child and obtain a saliva sample and again 30-min later over two consecutive days. Seven HFA children had comorbid conditions and 6 were on medication in contrast to Brosnan (Brosnan, et al., 2009). The results showed a comparable frequency of the CAR between children with and without autism (80% vs. 88%, respectively). There were also no significant differences based on the adult criterion (Wust, Federenko, Hellhammer, & Kirschbaum, 2000) between children with and without autism (73% vs. 84%, respectively). The different findings across the Brosnan (Brosnan, et al., 2009) and Zinke (Zinke, et al., 2010) studies may be attributed to developmental (adolescence vs. childhood), diagnostic (Asperger syndrome vs. HFA), setting (institutional living vs. home) or medication status (off vs. on medication).
The CAR has also been used as a dependent measure to ascertain treatment effects in ASD. Specifically, following the introduction of a service dog, children with ASD showed a significant reduction in the level of the CAR when the dog was with the child followed by a return to higher levels when the dog was removed from the home (Viau et al., 2010). While this study shows the CAR may be responsive to treatment effects, the characterization of the CAR, in terms of magnitude and frequency, was not central to the study.
In summary, despite rather consistent findings in some aspects of the diurnal regulation of cortisol in ASD (Corbett, et al., 2006; Corbett, et al., 2008; Richdale & Prior, 1992), the results of the initial CAR studies appear inconclusive; thereby warranting an expanded study in a large, well-characterized group.
MATERIAL AND METHODS
The goal of the current study was to more thoroughly characterize the CAR in a group of children with ASD by sampling over several (3) days. Based on previous research, we hypothesized that 1) there would not be a significant difference across the groups between children with and without ASD 2) however, we examined whether children with ASD would show greater variability in the CAR as has been reported in other aspects of the circadian pattern of cortisol secretion. To this end, we explored the relationship between the CAR and the child's cognitive and social communication profile.
Participants
The enrollment sample consisted of 97 un-medicated, pre-pubertal, healthy, male children between 8.0 and 12.11 years old, 47 with ASD (classified as 35 with autistic disorder, 5 with Pervasive developmental disorder – not otherwise specified (PDD-NOS), 10 with Asperger syndrome), (mean = 10.3 years) and 50 with typical development (TD) (mean = 9.9 years). ASD diagnosis was based on the Diagnostic and Statistical Manual (DSM-IV) criteria (APA, 2000) and established by all of the following: (1) a previous diagnosis by a psychologist, psychiatrist, or behavioral pediatrician with expertise in ASD; (2) current clinical judgment (BAC) and (3) corroborated by the Autism Diagnostic Observation Scale (ADOS) (Lord et al., 2000). The ADOS consists of a series of structured and semi-structured tasks that involve social interaction between the examiner and the participant. The examiner observes and identifies segments of the participant's behavior and assigns these to predetermined observational categories. Categorized observations are subsequently combined to produce quantitative scores for analysis. The ADOS was administered by research-reliable personnel, with a total score at or above the autism threshold for Module 3. The TD participants were thoroughly evaluated and required to have an absence of ASD symptoms (see SCQ below) and no diagnostic history of a neurodevelopmental disorder. Following initial enrollment and during data analysis, a child with ASD had sampling times that were significantly different than the protocol (i.e., second sample greater than one hour from initial waking sample) and three children (1 ASD, 2 TD) exhibited cortisol values greater than 3 standard deviations away from the mean; thus, these participants were dropped from the final analysis leaving 46 in the ASD group and 48 in the TD group for a total of 94 participants.
The Vanderbilt University Institutional Review Board approved the study conducted in compliance with the Code of the Ethical Principles for Medical Research Involving Human Subjects of the World Medical Association (Declaration of Helsinki) http://www.wma.net/en/30publications/10policies/b3. Informed written consent was obtained from parents and verbal assent was obtained from research participants prior to inclusion in the study.
Diagnostic Variables
Autism Diagnostic Observation Schedule (ADOS)
The ADOS (Lord, et al., 2000) is a semi-structured interview designed to assess behaviors characteristic of ASD. A score of 8 or greater on the social-communication domain of the ADOS Module 3 was required for inclusion in the ASD group.
Wechsler Abbreviated Scale of Intelligence (WASI)
The WASI (Wechsler, 1999) is a measure of cognitive ability used to obtain an estimate of intellectual functioning. Inclusion in the study required an estimated IQ of 70 or higher, which is often considered the cut-off for intellectual disability (APA, 2000).
Pubertal Development Scale (PDS)
The PDS is a parent report measure providing an estimate of the participant's level of pubertal development (Petersen, Crockett, Richards, & Boxer, 1988). Enrollment was limited to those who had not formally entered puberty defined as a score of ”1” (change not yet begun) or “2” (has barely started) in each of three categories: body hair, voice, and facial hair.
Social Communication Questionnaire (SCQ)
The SCQ (Rutter, Bailey, & Lord, 2003) is a 40 item parent-report questionnaire that assesses symptomology (e.g., impairment in social communication) associated with ASD. The primary application of the SCQ results in a single total score to identify individuals who are likely to suffer from ASD. For the current study, the SCQ was used as a screening tool to confirm that children with typical development demonstrated scores, and therefore symptoms, well below the ASD threshold (scores of ≥15 is suggestive of ASD while scores of ≥22 are suggestive of autism). The exclusion criteria for a typically developing child was set at a score ≥10; however, no participants were excluded based on this criteria. The SCQ scores were also used as a measure of social communication ability in correlation analyses.
Cortisol Sampling Protocol
Our established salivary collection protocols were strictly followed, which involved comprehensive baseline home sampling, restricting the intake of beverages and food to one hour before sample collection, no current medication use and employment of standardized procedures. If the parents reported any illness in the child (e.g., cold), then samples were not collected until the child regained healthy status. Samples were collected over three diurnal cycles during regular, consecutive weekdays from the home consisting of four samples per day (M1: Immediate Waking, M2 30-min Post Waking, A: afternoon, and E: evening) (the latter two samples are not part of the current investigation but are collected to establish baseline as part of a stress protocol (Corbett et al., in press). The CAR was calculated using the two morning samples (M2 - M1 = CAR). The collection tubes were stored in a Trackcap™ (Aprex®, Union City, CA), containing a microelectronic cap that provides a precise timestamp when tubes were removed, which ensures adherence to the sampling protocol and confirmed time of sampling (Kudielka, Broderick, & Kirschbaum, 2003).
Salivary samples were collected via passive drool. Trident® Original Sugarless chewing gum was given to the participant to act as a salivary stimulant. After approximately 30 seconds of chewing, the child removed the gum and promptly emitted saliva into a collection tube. Samples were labeled and stored in the home refrigerator for temporary storage.
While there has been recent concern raised regarding the use of gum in regards to the concentration of cortisol and other hormones (Schultheiss, 2013), validation assays conducted in the lab have shown no significant differences in the concentration or cross reactivity of cortisol in previous or current studies (all p >0.05). Explicitly, samples were collected from 8 subjects during the same time of day (afternoon, 3:00 pm) initially collected by passive drool without gum (mean=1.09, SD =0.36) and with gum (mean=1.19, SD =0.29) and compared using a paired samples t-test t(7)) = −.74, p = 0.46, r = 0. 31. Moreover, there were no differences in sample binding t(7) = 1.20, p =0.27, r = 0.09, which fell well within the curve, (37.87 and 34.59) or CV% t(7) = 0.57, p = 0.58 (mean = 3.60 (1.16) and 3.13 (1.56)), r = −0.49. Finally, all of the research participants utilized the gum as a salivary stimulant; thus, any modest influence on cortisol concentration was consistent across the study sample.
Cortisol Storage and Assays
Samples were stored in a −20 C freezer in the lab and then brought to the Laboratory by research personnel. Prior to assay, samples were thawed and centrifuged at 6000 rpm for 10 minutes to separate the aqueous component from mucins and other suspended particles. The salivary cortisol assay was performed using a Coat-A-Count® radioimmunoassay kit (Siemens Medical Solutions Diagnostics, Los Angeles, CA) modified to accommodate lower levels of cortisol in human saliva relative to plasma. Saliva samples, which had been stored at −20°C, were thawed and centrifuged at 3460 rpm for 15 minutes to separate the aqueous component from mucins and other suspended particles. The coated tube from the kit was substituted with a glass tube into which 100 μl of saliva, 100 μl of antibody (courtesy of Wendell Nicholson, Vanderbilt University, Nashville, TN), and 100 μl of 125I-cortisol were mixed. After incubation at 4°C for 24 hours 100 μl of normal rat serum in 0.1% PO4/EDTA buffer (1:50) and precipitating reagent (PR81) were added. The mixture was centrifuged at 3460 rpm for 30 minutes, decanted, and counted. Serial dilution of samples indicated a linearity of 0.99. Interassay coefficient of variation was 10.4%.
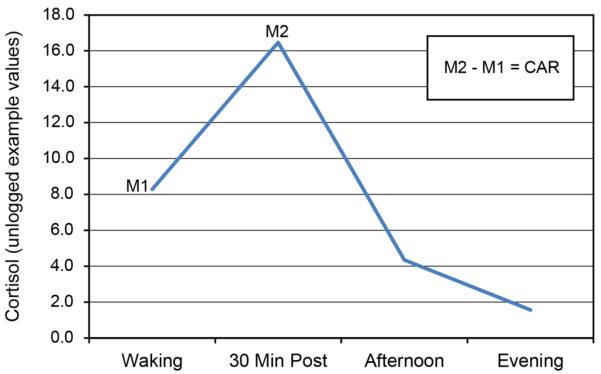
Primary Dependent Variables
For the current study, the primary dependent variable was the Cortisol Awakening Response (CAR), which was calculated by subtracting the Immediate Waking Sample from the 30-min Post Waking Sample and averaging the difference score across the three days of sampling (see Figure 1). Cortisol is highly right skewed, thus, all values were log transformed prior to analysis.
Figure 1.
Example of the Cortisol Awakening Response (CAR) with four salivary samples collected for each participant. Samples include two morning samples: M1: Immediately upon Waking and M2: 30-min Post Waking which are used to calculate the cortisol awakening response (M2 − M1 = CAR). Additionally, afternoon and evening samples are collected and shown here to illustrate the slope; however, they are not part of the current investigation. These samples were used to establish baseline for another study (Corbett, et al., in press).
Statistical Analysis
Between-group analyses were performed across all demographic, diagnostic, inclusion variables, and the primary outcome using two-sample independent t-tests. All analyses were conducted for the entire sample. Variances were compared using Levene's test of homogeneity to determine if the equal variance assumption between the groups was valid and to test the second hypothesis. Additionally, a repeated measures ANOVA model was used to determine the statistical significance of the sequence of the CAR over the three days. The chi-squared test of independence was used to compare the proportions of children between the groups exhibiting a CAR. Finally, the relationship between the CAR and the child's cognitive and social communication profile was compared using Pearson product-moment correlations as well as for measures used in calculation of the CAR. Given our available sample sizes, we have 80% power to detect moderate effects such as a difference in mean CAR levels of 0.28 nmol/L between the groups corresponding to a Cohen's d of 0.58.
RESULTS
As noted, salivary cortisol samples were collected over three diurnal cycles. To validate that sampling time did not confound the study results, repeated measures ANOVA was calculated for Sampling Time over three days as the within-subject factor and diagnosis as the between-subject factor. The results showed that there were no significant differences between the groups across multiple day sampling based on the TrackCap® home sampling times (F(2,84)=1.53, p=0.22, η2=0.04).
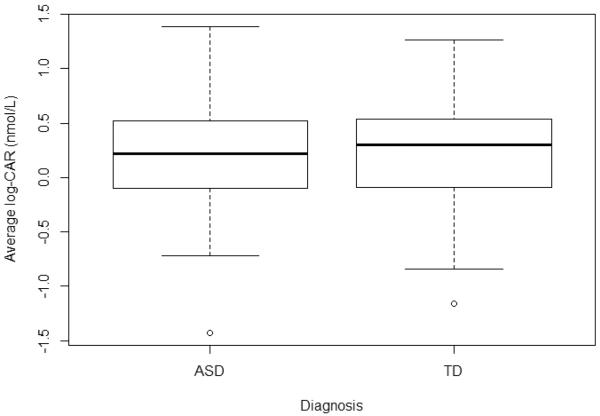
The primary aims of the study were to examine the magnitude (change in levels of morning cortisol as defined above), frequency (percentage of participants exhibiting the CAR) and pattern of CAR values (comparison across multiple day sampling) between male children with and without ASD. We used independent two-sample t-tests to examine the magnitude of the CAR between the groups, which revealed no significant differences (t(92) = −0.14, p = 0.89, d = 0.04; see Table 1 and Figure 2). Furthermore, Levene's Test for Equality of Error Variance was not statistically significant (F(45,47)=1.11, p=0.72, η2=0.11); indicating a similar variance structure in the ASD and TD groups.
Table 1.
Means and Standard Deviations of Demographic, Diagnostic, Inclusion and Average CAR Across Groups
| Variable | ASD (N=46) Mean | SD | TD (N=48) Mean | SD | T | P | 95% Confidence Interval | Cohen's d |
|---|---|---|---|---|---|---|---|---|
| Age | 10.3 | 1.7 | 9.9 | 1.6 | 1.3 | 0.21 | (−1.1, 0.25) | 0.26 |
| IQ | 98.0 | 22.8 | 123.6 | 12.6 | −6.54 | <0.01 | (17.5, 32.8) | 1.37 |
| SCQ | 22.9 | 7.1 | 2.2 | 2.1 | 18.7 | <0.01 | (−22.9, −18.5) | 4.11 |
| CAR Average | 0.21 | 0.50 | 0.23 | 0.48 | −0.14 | 0.89 | (−0.21, 0.19) | 0.03 |
Note: CAR = cortisol awakening response, TD = Typically developing, ASD = autism spectrum disorder, IQ = intelligence quotient, SCQ = social communication questionnaire.
Figure 2.
The figure shows a boxplot of the between Group comparison of the Cortisol Awakening Response (CAR) averaged over 3 days between children with autism spectrum disorder (ASD) and typical development (TD).
In consideration of some investigators analyzing the CAR based simply on the 30-min post-waking cortisol value, we compared these samples across the groups and similarly found no statically significant difference in magnitude of the 30-minute peak (t(92) = 0.35, p = 0.73, d = 0.07).
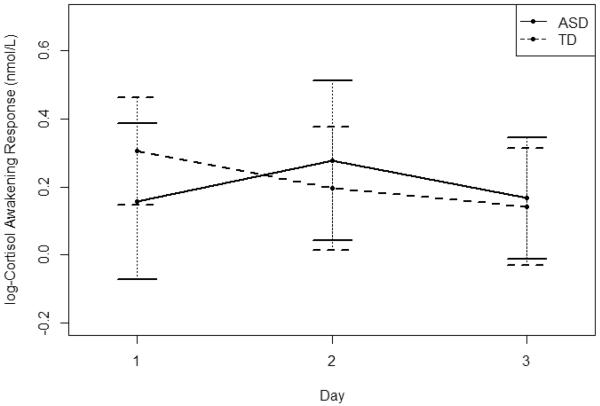
We also computed the sequence of morning CAR responses over the three days using a linear mixed-effects model with the CAR 1 through CAR 3 as the within-subject factor and Diagnosis (ASD vs. TD) as the between-subject factor and individual as the random factor (see Figure 3). The results showed no significant difference in the CAR between the groups (F(2,88)=0.26, p = 0.77, η2=0.01) over time.
Figure 3.
A between groups comparison of the average CAR over three days of home sampling. Cortisol values are log transformed. Children with ASD and TD are represented by the solid and dashed lines, respectively.
Next we assessed the proportion of children within the groups that exhibited a CAR, which is defined in children as a difference score that showed a positive increase above zero (Rosmalen, et al., 2005) between the 30-min Post Waking and Immediate Waking sample. The results showed that the proportion of children between the groups that showed a CAR was not significant (χ2(1) = 0.02, p = 0.89). The percentage of children that showed a CAR on average in the TD group was 68.8% (N=33) and 67.4% (N=31) of the ASD group across the three days of sampling, which was not statistically significant. We also examined the proportion of child participants evidencing a CAR based on adult criterion of greater than 2.49 nmol, which also showed no significant differences between the groups (χ2(1) = 1.82, p = 0.18). Specifically, of the TD 29.2% (N=14) and 17.4% (N=8) of the ASD group met the adult criterion.
The relationship between the CAR and participant's cognitive (IQ) and social communication profile (SCQ) was tested using Pearson product-moment correlations, which showed no association between the CAR and IQ (see Table 2). Additionally, the correlations were calculated between the average morning values and were highly correlated. Comparing the CAR values across the 3 days showed much weaker correlations, especially among children with ASD.
Table 2.
Overall and within group correlations between the cortisol and psychological variables
| Group | Comparison | Correlation | t-score | P-value |
|---|---|---|---|---|
| Overall (n=94) | Morning 1, Morning 2 | 0.825 | 14.0 | <0.001 |
| CAR (Day1, Day2) | 0.383 | 3.82 | <0.001 | |
| CAR (Day1, Day3) | 0.374 | 3.73 | <0.001 | |
| CAR (Day2, Day3) | 0.142 | 1.34 | 0.184 | |
| AVG CAR, IQ | 0.020 | 0.19 | 0.851 | |
| AVG CAR, SCQ | −0.007 | −0.06 | 0.952 | |
| ASD (n=46) | Morning 1, Morning 2 | 0.811 | 9.22 | <0.001 |
| CAR (Day1, Day2) | 0.384 | 2.59 | 0.013 | |
| CAR (Day1, Day3) | 0.287 | 1.89 | 0.065 | |
| CAR (Day2, Day3) | −0.016 | −0.10 | 0.921 | |
| AVG CAR, IQ | 0.099 | 0.66 | 0.514 | |
| AVG CAR, SCQ | 0.001 | 0.01 | 0.995 | |
| TD (n=48) | Morning 1, Morning 2 | 0.837 | 10.4 | <0.001 |
| CAR (Day1, Day2) | 0.410 | 2.98 | 0.005 | |
| CAR (Day1, Day3) | 0.504 | 3.88 | <0.001 | |
| CAR (Day2, Day3) | 0.332 | 2.34 | 0.024 | |
| AVG CAR, IQ | −0.151 | −1.01 | 0.317 | |
| AVG CAR, SCQ | 0.109 | 0.72 | 0.475 |
Note: CAR = cortisol awakening response, TD = Typically developing, ASD = autism spectrum disorder, AVG = average, IQ = intelligence quotient.
DISCUSSION
The current study examined the CAR in a group of high functioning children with ASD compared to age and gender matched typically developing male peers. The results showed that children with ASD show a CAR, which is comparable to typically developing children. Since children do not always exhibit a CAR, we analyzed the data based on both child and adult criteria (Wust, Federenko, et al., 2000); yet, the results remained the same. Specifically, 67.4% of our ASD sample and 68.8% of the TD group showed a significant burst in cortisol 30 minutes after waking. Based on the adult criterion of having at least a 2.98 nmol increase, 17.4% of the ASD group and 29.2% of the TD met the criterion.
The limited research exploring the CAR and ASD has been mixed but may be due, in part, to developmental factors and the criterion used to (child versus adult). Adolescents with Asperger syndrome evidenced a blunted CAR based on adult criteria (Brosnan, et al., 2009). However, when comparison was based on younger participants and the child criteria there were no difference between groups thereby largely consistent with the current findings and Zinke et al., (Zinke, et al., 2010).
Minor distinctions between the previous (Brosnan, et al., 2009; Zinke, et al., 2010) and current studies may be influenced by diagnostic sample categories. While it is currently accepted practice to take a dimensional approach and refer to participants as having ASD (APA, 2013) rather than delineate them based on previously defined categories (i.e., Asperger syndrome and autism), distinctions may exist for some biological phenomenon, such as the HPA axis. The majority of the children in the study were classified based on DSM-IV (APA, 2000) strictly defined criteria of autistic disorder (69%) and a subset had Asperger syndrome or Pervasive Developmental Disorder-Not Otherwise Specified (31%). Since the current study includes diagnostic groups (Asperger and autism) from both studies, and contains a large sample size, it is less likely that such classification would contribute to differences across the studies. Moreover, based on the child criteria for defining the CAR, there does not appear to be differences in the magnitude, frequency or even in the variability of the CAR in children with and without ASD. CAR values based on the adult criterion were also not distinct as shown in Zinke (Zinke, et al., 2010); however, it is in contrast to reported differences in Brosnan (Brosnan, et al., 2009) that did report a lower frequency of CAR in ASD adolescents. It should also be noted that while Zinke (Zinke, et al., 2010) did not report statistically significant differences based on adult criteria, a much larger proportion of children in both the ASD and TD groups exhibited a CAR compared to current findings and Zinke (Zinke, et al., 2010). The findings from these previous studies and the current results are summarized in Table 3.
Table 3.
| ASD Study | Frequency of CAR Child Criterion in study sample | Frequency of CAR Adult Criterion in study sample | Specific Study Characteristics | ||
|---|---|---|---|---|---|
| First Author | TD | ASD | TD | ASD | Age, Diagnosis, Medication, sample size |
| Brosnan | 72% of 18 | 60% of 20 | 28% of 18 | 5% of 20 | 11–16, Asperger, no meds |
| Zinke | 88% of 25 | 80% of 15 | 84% of 25 | 73% of 15 | 6–12 HFA Meds allowed |
| Corbett | 69% of 55 | 61% of 52 | 25% of 55 | 15% of 52 | 8–12 ASD no meds |
Note: CAR = cortisol awakening response, TD = Typically developing, ASD = autism spectrum disorder, HFA = high functioning autism, meds = medication status
Prior research suggests that the CAR is a reliable measure of the reactive capacity of the HPA axis in children and adults (Pruessner, et al., 1997;Schmidt-Reinwald et al., 1999, Wust, Wolf, et al., 2000). It has been implicated in a number of disorders, such as depression (Kuehner, Holzhauer, & Huffziger, 2007). However, in the current study the magnitude, variability and proportion of children exhibiting a CAR did not differentiate the groups despite having adequate power to detect a group difference if one existed.
The normal CAR is in contrast to differences in other diurnal cortisol measures, such as elevated evening values and a decline in the morning diurnal slope over time previously found in ASD (Corbett, et al., 2008). Nevertheless, there was no statistical difference between the first and second morning sample and the CAR was not related to the afternoon or evening values. As such, the CAR as it relates to the absolute regulation of the diurnal cycle does not appear to be distinct in the majority of children with ASD.
The strengths of the study include a careful investigation of the CAR over three days in a large group of well-characterized, unmedicated children with ASD. Samples were collected after natural waking in the child's home over several days, and we employed an electronic device to ensure accurate sampling time and adherence to the protocol. The current study did not include female participants. Due to the 4:1 male-to-female ratio in ASD, we could not collect an ample number of participants to appropriately conduct gender comparisons. Medication use was an exclusion criterion for the investigation, similar to Brosnan et al., (Brosnan, et al., 2009) since a variety of pharmaceutical agents can alter the HPA axis including the CAR. While this is considered an asset in terms of study design, it may limit generalizability to members of the ASD population frequently prescribed medication. It is well-established that sleep (Federenko, et al., 2004), and anxiety (Dahlgren, Kecklund, Theorell, & Akerstedt, 2009) may impact the CAR, and are common comorbid features of ASD (e.g., (Malow et al., 2012)). However, the current study did not include measures (e.g., sleep diary, actigraphy, questionnaires) that may have identified interesting phentotypic distinctions between the CAR and these factors.
In summary, despite children with ASD showing difficulty adapting to change and evidencing increased arousal in response to various stressors (Corbett, et al., 2008; Corbett, et al., 2009), the frequency or magnitude of the CAR does not distinguish children with ASD from typically developing peers. Future studies appear warranted to examine the CAR prospectively as children age across development, and to explore potential diagnostic distinctions within ASD amidst changing diagnostic criteria (APA, 2013).
CONCLUSIONS
The CAR is a measure of the reactive capacity of the HPA axis (Schmidt-Reinwald, et al., 1999), which purportedly helps an individual prepare for upcoming challenges (Fries, et al., 2009). Although children with ASD often exhibit poor adaptation to change which has been associated with elevated evening cortisol levels (Corbett, et al., 2009) and increased stress responsivity (Corbett, et al., 2006; Corbett, et al., 2012; Richdale & Prior, 1992; Tordjman, et al., 1997), the current study showed no differences in the magnitude, variability or presence of the CAR when compared to typically developing peers. Since the CAR is largely genetically determined (Bartels, de Geus, et al., 2003; Veen, et al., 2011), distinctions may be determined by factors beyond the ASD diagnosis. Exploration into secondary factors that may disrupt the CAR that have also been implicated in subgroups of children with ASD, such as sleep disturbance or anxiety, may provide meaningful information and clues for treatment of comorbid conditions.
HIGHLIGHTS
The CAR was investigated in male children with ASD and typical development.
There were no between groups based on the magnitude or variability of the CAR.
The proportion of children exhibiting a CAR was similar across the groups.
Reported differences may be due to age, criterion, and diagnostic distinctions.
Acknowledgements
We are grateful to all the children and families who continue to support our research exploring the biobehavioral profiles of individuals with autism.
Role of the Funding Source: This work was supported in part by the National Institute of Health R01 MH085717 awarded to Blythe Corbett. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institute of Health. The NIHM had no further role in study design, in the collection, analysis and interpretation of the data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- APA . Diagnostic and statistical manual of mental disorders, Fourth Edition, Text Revision (DSM-IV-TR) American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- APA . Diagnostic and statistical manual of mental disorders, Fifth Edition (DSM-5) American Psychiatric Association; Washinton, D.C.: 2013. [Google Scholar]
- Bartels M, de Geus EJ, Kirschbaum C, Sluyter F, Boomsma DI. Heritability of daytime cortisol levels in children. Behav Genet. 2003;33(4):421–433. doi: 10.1023/a:1025321609994. [DOI] [PubMed] [Google Scholar]
- Bartels M, Van den Berg M, Sluyter F, Boomsma DI, de Geus EJ. Heritability of cortisol levels: review and simultaneous analysis of twin studies. Psychoneuroendocrinology. 2003;28(2):121–137. doi: 10.1016/s0306-4530(02)00003-3. [DOI] [PubMed] [Google Scholar]
- Brosnan M, Turner-Cobb J, Munro-Naan Z, Jessop D. Absence of a normal cortisol awakening response (CAR) in adolescent males with Asperger syndrome (AS) Psychoneuroendocrinology. 2009;34(7):1095–1100. doi: 10.1016/j.psyneuen.2009.02.011. [DOI] [PubMed] [Google Scholar]
- Buchanan TW, Kern S, Allen JS, Tranel D, Kirschbaum C. Circadian regulation of cortisol after hippocampal damage in humans. Biol Psychiatry. 2004;56(9):651–656. doi: 10.1016/j.biopsych.2004.08.014. [DOI] [PubMed] [Google Scholar]
- Clow A, Thorn L, Evans P, Hucklebridge F. The awakening cortisol response: methodological issues and significance. Stress. 2004;7(1):29–37. doi: 10.1080/10253890410001667205. [DOI] [PubMed] [Google Scholar]
- Corbett BA, Mendoza S, Abdullah M, Wegelin JA, Levine S. Cortisol circadian rhythms and response to stress in children with autism. Psychoneuroendocrinology. 2006;31(1):59–68. doi: 10.1016/j.psyneuen.2005.05.011. [DOI] [PubMed] [Google Scholar]
- Corbett BA, Mendoza S, Wegelin JA, Carmean V, Levine S. Variable cortisol circadian rhythms in children with autism and anticipatory stress. Journal of Psychiatry and Neuroscience. 2008;33(3):227–234. [PMC free article] [PubMed] [Google Scholar]
- Corbett BA, Schupp CW, Lanni KE. Comparing biobehavioral profiles across two social stress paradigms in children with and without autism spectrum disorders. Mol Autism. 2012;3(1):13. doi: 10.1186/2040-2392-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett BA, Schupp CW, Levine S, Mendoza S. Comparing cortisol, stress and sensory sensitivity in children with autism. Autism Research. 2009;2:32–39. doi: 10.1002/aur.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett BA, Swain DS, Newsom C, Wang L, Song Y, Edgerton D. Biobehavioral profiles of arousal and social motivation in autism spectrum disorders. Journal of Child Psychology and Psychiatry. doi: 10.1111/jcpp.12184. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlgren A, Kecklund G, Theorell T, Akerstedt T. Day-to-day variation in saliva cortisol--relation with sleep, stress and self-rated health. Biol Psychol. 2009;82(2):149–155. doi: 10.1016/j.biopsycho.2009.07.001. [DOI] [PubMed] [Google Scholar]
- Federenko I, Wust S, Hellhammer DH, Dechoux R, Kumsta R, Kirschbaum C. Free cortisol awakening responses are influenced by awakening time. Psychoneuroendocrinology. 2004;29(2):174–184. doi: 10.1016/s0306-4530(03)00021-0. [DOI] [PubMed] [Google Scholar]
- Figueiro MG, Rea MS. Short-wavelength light enhances cortisol awakening response in sleep-restricted adolescents. Int J Endocrinol. 2012;2012:301935. doi: 10.1155/2012/301935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fries E, Dettenborn L, Kirschbaum C. The cortisol awakening response (CAR): facts and future directions. Int J Psychophysiol. 2009;72(1):67–73. doi: 10.1016/j.ijpsycho.2008.03.014. [DOI] [PubMed] [Google Scholar]
- Griefahn B, Robens S. The cortisol awakening response: a pilot study on the effects of shift work, morningness and sleep duration. Psychoneuroendocrinology. 2008;33(7):981–988. doi: 10.1016/j.psyneuen.2008.04.004. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Wewerka S, Frenn K, Long JD, Griggs C. Developmental changes in hypothalamus-pituitary-adrenal activity over the transition to adolescence: normative changes and associations with puberty. Dev Psychopathol. 2009;21(1):69–85. doi: 10.1017/S0954579409000054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanner L. Autistic disturbances of affective contact. Nervous Child. 1943;2:217–250. [PubMed] [Google Scholar]
- Kudielka BM, Broderick JE, Kirschbaum C. Compliance with saliva sampling protocols: electronic monitoring reveals invalid cortisol daytime profiles in noncompliant subjects. Psychosom Med. 2003;65(2):313–319. doi: 10.1097/01.psy.0000058374.50240.bf. [DOI] [PubMed] [Google Scholar]
- Kudielka BM, Buchtal J, Uhde A, Wust S. Circadian cortisol profiles and psychological self-reports in shift workers with and without recent change in the shift rotation system. Biol Psychol. 2007;74(1):92–103. doi: 10.1016/j.biopsycho.2006.08.008. [DOI] [PubMed] [Google Scholar]
- Kudielka BM, Kirschbaum C. Awakening cortisol responses are influenced by health status and awakening time but not by menstrual cycle phase. Psychoneuroendocrinology. 2003;28(1):35–47. doi: 10.1016/s0306-4530(02)00008-2. [DOI] [PubMed] [Google Scholar]
- Kuehner C, Holzhauer S, Huffziger S. Decreased cortisol response to awakening is associated with cognitive vulnerability to depression in a nonclinical sample of young adults. Psychoneuroendocrinology. 2007;32(2):199–209. doi: 10.1016/j.psyneuen.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Law R, Hucklebridge F, Thorn L, Evans P, Clow A. State variation in the cortisol awakening response. Stress. 2013;16(5):483–492. doi: 10.3109/10253890.2013.817552. [DOI] [PubMed] [Google Scholar]
- Liberzon J, Abelson JL, King A, Liberzon I. Naturalistic stress and cortisol response to awakening: adaptation to seafaring. Psychoneuroendocrinology. 2008;33(7):1023–1026. doi: 10.1016/j.psyneuen.2008.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Jr., Leventhal BL, DiLavore PC, et al. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30(3):205–223. [PubMed] [Google Scholar]
- Malow BA, Byars K, Johnson K, Weiss S, Bernal P, Goldman SE, et al. A practice pathway for the identification, evaluation, and management of insomnia in children and adolescents with autism spectrum disorders. Pediatrics. 2012;130(Suppl 2):S106–124. doi: 10.1542/peds.2012-0900I. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: reliability, validity and initial norms. Journal of Youth and Adolescence. 1988;17(2):117–131. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Platje E, Vermeiren RR, Branje SJ, Doreleijers TA, Meeus WH, Koot HM, et al. Long-term stability of the cortisol awakening response over adolescence. Psychoneuroendocrinology. 2012 doi: 10.1016/j.psyneuen.2012.06.007. [DOI] [PubMed] [Google Scholar]
- Pruessner JC, Wolf OT, Hellhammer DH, Buske-Kirschbaum A, von Auer K, Jobst S, et al. Free cortisol levels after awakening: a reliable biological marker for the assessment of adrenocortical activity. Life Sci. 1997;61(26):2539–2549. doi: 10.1016/s0024-3205(97)01008-4. [DOI] [PubMed] [Google Scholar]
- Pruessner M, Vracotas N, Joober R, Pruessner JC, Malla AK. Blunted cortisol awakening response in men with first episode psychosis: Relationship to parental bonding. Psychoneuroendocrinology. 2013;38(2):229–240. doi: 10.1016/j.psyneuen.2012.06.002. [DOI] [PubMed] [Google Scholar]
- Richdale AL, Prior MR. Urinary cortisol circadian rhythm in a group of high-functioning children with autism. J Autism Dev Disord. 1992;22(3):433–447. doi: 10.1007/BF01048245. [DOI] [PubMed] [Google Scholar]
- Rosmalen JG, Oldehinkel AJ, Ormel J, de Winter AF, Buitelaar JK, Verhulst FC. Determinants of salivary cortisol levels in 10–12 year old children; a population-based study of individual differences. Psychoneuroendocrinology. 2005;30(5):483–495. doi: 10.1016/j.psyneuen.2004.12.007. [DOI] [PubMed] [Google Scholar]
- Rutter M, Bailey A, Lord C. The Social Communication Questionnaire. Western Psychological Services; Los Angeles, CA: 2003. [Google Scholar]
- Schmidt-Reinwald A, Pruessner JC, Hellhammer DH, Federenko I, Rohleder N, Schurmeyer TH, et al. The cortisol response to awakening in relation to different challenge tests and a 12-hour cortisol rhythm. Life Sci. 1999;64(18):1653–1660. doi: 10.1016/s0024-3205(99)00103-4. [DOI] [PubMed] [Google Scholar]
- Schultheiss OC. Effects of sugarless chewing gum as a stimulant on progesterone, cortisol, and testosterone concentrations assessed in saliva. Int J Psychophysiol. 2013;87(1):111–114. doi: 10.1016/j.ijpsycho.2012.11.012. [DOI] [PubMed] [Google Scholar]
- Thorn L, Hucklebridge F, Esgate A, Evans P, Clow A. The effect of dawn simulation on the cortisol response to awakening in healthy participants. Psychoneuroendocrinology. 2004;29(7):925–930. doi: 10.1016/j.psyneuen.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Tordjman S, Anderson GM, McBride PA, Hertzig ME, Snow ME, Hall LM, et al. Plasma beta-endorphin, adrenocorticotropin hormone, and cortisol in autism. J Child Psychol Psychiatry. 1997;38(6):705–715. doi: 10.1111/j.1469-7610.1997.tb01697.x. [DOI] [PubMed] [Google Scholar]
- Veen G, Giltay EJ, van Vliet IM, Derijk RH, Klaassens ER, van Pelt J, et al. C-reactive protein polymorphisms are associated with the cortisol awakening response in basal conditions in human subjects. Stress. 2011;14(2):128–135. doi: 10.3109/10253890.2010.515273. [DOI] [PubMed] [Google Scholar]
- Viau R, Arsenault-Lapierre G, Fecteau S, Champagne N, Walker CD, Lupien S. Effect of service dogs on salivary cortisol secretion in autistic children. Psychoneuroendocrinology. 2010;35(8):1187–1193. doi: 10.1016/j.psyneuen.2010.02.004. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. Psychological Corporation; San Antonio, TX: 1999. [Google Scholar]
- Wilhelm I, Born J, Kudielka BM, Schlotz W, Wust S. Is the cortisol awakening rise a response to awakening? Psychoneuroendocrinology. 2007;32(4):358–366. doi: 10.1016/j.psyneuen.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Wust S, Federenko I, Hellhammer DH, Kirschbaum C. Genetic factors, perceived chronic stress, and the free cortisol response to awakening. Psychoneuroendocrinology. 2000;25(7):707–720. doi: 10.1016/s0306-4530(00)00021-4. [DOI] [PubMed] [Google Scholar]
- Wust S, Wolf J, Hellhammer DH, Federenko I, Schommer N, Kirschbaum C. The cortisol awakening response - normal values and confounds. Noise Health. 2000;2(7):79–88. [PubMed] [Google Scholar]
- Zinke K, Fries E, Kliegel M, Kirschbaum C, Dettenborn L. Children with high-functioning autism show a normal cortisol awakening response (CAR) Psychoneuroendocrinology. 2010;35(10):1578–1582. doi: 10.1016/j.psyneuen.2010.03.009. [DOI] [PubMed] [Google Scholar]