Abstract
Trauma centers are an ideal point of intervention in efforts to prevent posttraumatic stress disorder (PTSD). In order to assist in the development of prevention efforts, this study sought to identify early predictors of PTSD symptoms among adults admitted to a Level I trauma center using a novel analytic strategy (Fournier et al., 2009). Upon admission, participants (N=327) were screened for PTSD symptoms and provided information on potential predictor variables. Their PTSD symptoms were assessed again three months later (N=227). Participants were classified as: symptomatic (positive PTSD screen) or asymptomatic (negative PTSD screen) at the follow-up assessment. Multinomial logistic regression showed that, age, depression, number of premorbid psychiatric disorders, gunshot wound, auto vs. pedestrian accident, and alcohol use predicted who had PTSD symptoms at FU with 76.3% accuracy. However, when controlling for PTSD severity at baseline, only age, number of premorbid psychiatric disorders, and gunshot wounds predicted PTSD symptoms at FU but with 78.5% accuracy. These findings suggest that psychological prevention efforts in trauma centers may be best directed toward adults who are young, have premorbid psychiatric disorders, and those admitted with gunshot wounds.
Keywords: PTSD, Trauma, Predictors, Injury, Logistic Regression
It is estimated that most Americans (81%) will experience a trauma at some point in their lives (Breslau et al., 1998; Kessler et al., 2005; Sledjeski, Speisman, & Dierker, 2008) and a common point of first contact with these individuals is a Level I Trauma Center (Conrad, Hansel, Pejic, & Constans, 2013; Zatzick et al., 2004). Level I Trauma Centers are designated by the American College of Surgeons (American College of Surgeons, 2012) and must meet specific criteria including at least 1,200 trauma patients yearly, 24-hour availability of surgeons in multiple specialties, excellence in education, and an active research program.
Trauma is the leading cause of death for people ages 1-44 in the United States (National Center for Injury Prevention and Control (NCIPC), 2011), and among those who survive, at least 2.8 million are hospitalized each year with varying levels of disability (Hall, DeFrances, Williams, Golosinskiy, & Schwatzman, 2010). Most individuals who experience a trauma (71%-94%) will report Posttraumatic Stress Disorder (PTSD) symptoms immediately following the event (Riggs, Rothbaum, & Foa, 1995; Rothbaum, Foa, Riggs, Murdock, & Walsh, 1992). Although many experience steady emotional recovery, a sizable percentage of these individuals (15-25%) will continue to report symptoms and eventually meet formal diagnostic criteria for PTSD (Riggs et al., 1995; Rothbaum et al., 1992).
Fortunately, treatment for PTSD is highly effective for most (85%) patients (Powers, Halpern, Ferenschak, Gillihan, & Foa, 2010) and there are now pilot data showing that acute intervention may also prevent chronic PTSD (PTSD for ≥3 months) (Rothbaum et al., 2012). However, delivering interventions to all trauma survivors is not cost-effective, considering that many individuals recover without intervention (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Riggs et al., 1995; Rothbaum et al., 1992), and for some, early intervention interferes with natural recovery (van Emmerik, Kamphuis, Hulsbosch, & Emmelkamp, 2002). Accordingly, identifying variables that predict who will develop chronic PTSD symptoms after a trauma may aid the more efficient use of resources for treating, or preventing, possible chronic PTSD, and may aid the development of targeted intervention efforts in Level I Trauma Centers.
To date, studies examining potential PTSD risk factors have yielded inconsistent findings, likely because of various limitations in their methodological approaches (e.g., retrospective vs. prospective designs, adequate vs. inadequate control features in analyses). Despite this, PTSD risk factors have been identified by several meta-analyses (Creamer, Bell, & Failla, 2003; Kessler et al., 1995; Ozer, Best, Lipsey, & Weiss, 2003). Importantly, however, there is a lack of research on PTSD symptom predictors conducted in Level I Trauma Centers (Conrad et al., 2013). Further research is needed to determine which factors are associated with PTSD symptomatology onset, maintenance, or recovery in this setting while using more advanced analyses strategies. As such, we used an empirical four-stage analysis (Fournier et al., 2009) that balances the need to identify as many predictors as possible of PTSD symptomatology while minimizing identifying predictors that only emerge by chance.
To this end, we screened adults for symptoms of PTSD and for a number of potential predictor variables upon hospital admission (baseline) to a Level I Trauma Center, and assessed them for the presence or absence of these symptoms three months later. Recognizing that a formal PTSD diagnosis requires persistence of symptoms for at least one month following a trauma, we categorized patients according to whether or not they screened positive for symptoms of PTSD at a 3-month follow-up. Given the volume of patients admitted to our Trauma Center, these assessments were not intended to be fully diagnostic. However, examining the level of symptoms of PTSD before a formal diagnosis can be made (at baseline) allowed us to control for baseline symptoms levels and examine an understudied time interval which may be very relevant to later development of a PTSD diagnosis. We identified specific predictor variables from the literature (e.g. Brewin, Andrews, & Valentine, 2000; Chiu, deRoon-Cassini, & Brasel, 2011; Ozer, Best, Lipsey, & Weiss, 2003) that may be associated with PTSD development and examined whether any of these variables were related to symptomatology at the 3-month follow-up.
Method
Design and Procedures
The Baylor University Medical Center Dallas Institutional Review Board approved the study protocol. Trained clinical research assistants approached eligible patients once they were medically stable. The participants completed standardized questionnaires while hospitalized (baseline), and completed an assessment of PTSD symptomatology 3 months post injury (follow-up) by phone.
Participants
Participants (N=327) were patients meeting study eligibility criteria, admitted to the Level I trauma center between March 26, 2012 and June 10, 2013, who had sustained a traumatic injury (e.g., fall, motor vehicle collision, violent crime). The sample was primarily male (64%), white (68%), non-Hispanic (81%), with a mean age of 46 (SD=18). Presence of traumatic injury was verified by cross-referencing the trauma and orthopedic trauma admission lists with Trauma Registry database criteria. Inclusion criteria included (1) admission to the trauma service with total hospital admission at least 24 hours, (2) 18 years of age and older, and (3) ability to provide at least one contact phone number for follow-up. Exclusion criteria included (1) traumatic brain injury (TBI) and/or premorbid cognitive deficits (e.g., dementia, Alzheimer’s) that would interfere with the ability to respond to the measures, and (2) inability to understand spoken English or Spanish. All participants provided informed consent.
Measures
PTSD Screening
The Primary Care Post-Traumatic Stress Disorder Screen (PC-PTSD) is a four-item PTSD screen designed for use in medical settings (Reese et al., 2012) and is the current screening instrument used in Veterans Affairs (VA) centers (Prins et al., 2003). The items assess the presence or absence of the three PTSD clusters including re-experiencing, avoidance, and hyperarousal. The PC-PTSD is considered a psychometrically sound screen for determining the presence of PTSD in the VA setting and has also been used in the civilian primary care population. With a cut-off score of 3, the PC-PTSD screener has shown 85% diagnostic efficiency, 78% sensitivity, and 87% specificity (Prins et al., 2003). A score of 3 or higher on the PC-PTSD was considered a positive screen for clinical levels of PTSD symptoms. Individuals were categorized as: symptomatic (positive PTSD screen) or asymptomatic (negative PTSD screen) at the follow-up assessment.
Predictor Variables
Study measures collected at baseline were organized into the following domains: demographic variables, psychological variables, cause of injury, hospitalization characteristics, substance use, and injury related variables.
Demographic variables
Demographic information was taken from the hospital trauma registry including age, gender, ethnicity, marital status, educational level, and income level.
Psychological variables
The Patient Health Questionnaire (PHQ-8) is a psychometrically sound measure of depression for population-based studies and clinical populations (Kroenke, Spitzer, & Williams, 2001).
The Connor-Davidson Resilience Scale 10 Item (CD-RISC 10) is a measure of resilience with sound psychometric properties (Connor & Davidson, 2003) and has been used in populations who have sustained traumatic injuries (White, Driver, & Warren, 2010). The Social Provisions Scale (SPS) assesses social support received within the context of interpersonal relationships and has adequate psychometric properties (Cutrona & Russell, 1987).
The patient’s history of psychiatric illness was assessed by self-report, with patients answering Yes, No, or Unknown to having ever been diagnosed with or treated for psychological conditions including depression, bipolar disorder, PTSD, generalized anxiety disorder, and/or schizophrenia.
Hospitalization characteristics
Hospitalization characteristics were obtained from the hospital Trauma Registry, (TraumaBase – Clinical Data Management, Colorado Springs, CO) and included number of complications, days spent on a ventilator, length of stay in Intensive Care Unit (ICU), total length of hospital stay, and number of comorbidities.
Injury related variables
Injury-related information obtained from the Trauma Registry included mechanism of injury, pain level (Numeric Rating Scale) at baseline, pulse at time of admission, penetrating trauma (or not), the Glasgow Coma Scale (GCS), and the Injury Severity Score (ISS).
The Numeric Rating Scale (NRS) is one of the most commonly used measures in assessing pain and has been validated as a measure of pain intensity (Fraenkel et al., 2012; Lund et al., 2005). For the purposes of the study, participants were asked at baseline to rate pain on average since their injury.
The Glasgow Coma Scale (GCS) was designed to assess the level of consciousness following injury (Rowley & Fielding, 1991; Teasdale & Jennett, 1974, 1976; Teasdale, Kril-Jones, & van der Sande, 1978).
The Injury Severity Score (ISS) is an anatomical scoring system that provides an overall score for patients with multiple injuries (Baker, O’Neill, Haddon, & Long, 1974). Each injury is assigned an Abbreviated Injury Score (AIS) and is allocated to one of six body regions (Head, Face, Chest, Abdomen, Extremities, External). The highest AIS score in each region is used and the three most severely injured regions have their scores squared and added together to produce the ISS score (Baker et al., 1974).
Substance use variables
The Alcohol Use Disorder Identification Test-Consumption (AUDIT-C) has been extensively validated to detect problem drinking and has been a recommended screening tool for alcohol screening (Bush, Kivlahan, & McDonell, 1998). Other substance use variables were obtained from the trauma registry and included blood alcohol level at admission and positive drug screen at admission.
Data Analysis
Logistic regression was used to analyze the data. We identified significant predictors of PTSD level symptoms using an approach developed by Fournier and colleagues (Amir, Taylor, & Donohue, 2011; Fournier et al., 2009). The goal of this stepwise procedure is to extract significant predictors of the PTSD symptoms from each of the domains of predictors that we had identified above (e.g., demographics, substance use, psychological variables, hospitalization variables, injury-related variables, and cause of injury), and then to use these significant predictors in a final model predicting PTSD. The Fournier approach represents a balance between examining multiple predictor variables separately, in which case there might be third-variables that could alternatively explain the relations, and including all variables simultaneously in the prediction equation, which could violate guidelines for the ratio of predictors to subjects, and would likely result in high Type II error (low power). Following the Fournier algorithm, we conducted a step-wise procedure within each domain of predictors. The first phase, Step 1, identifies significant predictors within each domain (group) of predictors (demographics, substance use, psychological variables, hospitalization variables, injury-related variables, and cause of injury). For each domain, Step 1 involved testing a model including all variables in that domain. Step 2 retained the terms from Step 1 that were significant at p<.20. Thus, we performed a second logistic regression for each domain that included those predictors from Step 1 with p<.20. Step 3 (for each domain of predictors) retained the terms from Step 2 that were significant at p<.10. Step 4 retained the terms from Step 3 that were significant at p<.05. Finally, each term that was significant at p<.05 in Step 4 within each domain was included in our final model across domains, allowing the testing of the effects of each variable while controlling for the effects of other important variables.
We performed this Fournier analysis two times, first identifying predictors of PTSD level symptoms at the 3 month follow-up without controlling for PC-PTSD score at baseline and second including baseline scores on the PC-PTSD screen as a covariate in all the analyses. This second analysis yields predictors of a positive PTSD screen (yes/no) at 3 months that are significant predictors over and above PTSD screen scores (0-4) at baseline.
Results
Eligible patients (N = 390) were approached between March 26, 2012 and June 10, 2013. Of these, 327 participants were enrolled into the study, 227 of which completed their 3-month follow up at the time of analysis. No statistically significant differences were found between the group that agreed to participate versus those that declined, nor between those that only completed the baseline assessment and those that also completed the follow-up assessment (including ETOH level, vent days, ISS, GCS, LOS, pulse, gender, race, injury type, ETOH tested or drug tested). Baseline information of these 327 participants is presented in Table 1. The most common cause of injury was a fall (29%), followed by a motor vehicle collision (24%). The mean time from injury to first assessment was 6.42 days.
Table 1.
| Domain/Predictor | Mean ± SD | Count (%) |
|---|---|---|
| Demographic | ||
|
| ||
| Age | 46 ± 18 | |
| Gender (Male) | 145 (64%) | |
| Non-White | 72 (32%) | |
| Non-Hispanic Origin | 183 (81%) | |
| Married | 80 (35%) | |
| Educational Level* | ||
| 1 – 8th grade or less | 7 (3%) | |
| 2 - 9–12th grade | 41 (18%) | |
| 3 - High School diploma | 79 (35%) | |
| 4 - Associate’s degree | 36 (16%) | |
| 5 - Bachelor’s degree | 44 (19%) | |
| 6 - Master’s degree | 13 (6%) | |
| 7 - Doctoral degree | 5 (2%) | |
| 8 – Professional degree | 2 (1%) | |
| Employment | 129 (57%) | |
| Income* | ||
| 1 - <$25k | 58 (33%) | |
| 2 - $25–49k | 28 (16%) | |
| 3 - $50–74k | 41 (24%) | |
| 4 - ≥75k | 47 (27%) | |
|
| ||
| Psychological | ||
|
| ||
| Patient Health Questionnaire - 8 | 7.7 ± 6.2 | |
| Social Provisions Scale | 60.6 ± 3.7 | |
| Connor-Davidson Resilience Scale 10 | 31.4 ± 6.7 | |
| Premorbid Diagnosis | 64 (55%) | |
|
| ||
| Cause of Injury | ||
|
| ||
| Gunshot | 23 (11%) | |
| Motor Vehicle | 52 (24%) | |
| Aggravated Assault | 14 (6%) | |
| Motorcycle | 27 (12%) | |
| Pedestrian/Bike | 21 (10%) | |
| Fall | 63 (29%) | |
| Other | 19 (10%) | |
|
| ||
| Hospitalization & Complications | ||
|
| ||
| Ventilation Days | 0.9 ± 3.2 | |
| Intensive Care Unit Length of Stay | 1.6 ± 4.7 | |
| Total Length of Stay | 8.5 ± 11.6 | |
| Total Complications | 1.0 ± 1.3 | |
| Comorbidities | 191 (85%) | |
|
| ||
| Injury Characteristics | ||
|
| ||
| Injury Severity Score | 11.6 ± 8.2 | |
| Glasgow Coma Scale | 14.4 ± 2.1 | |
| Pulse | 91.2 ± 20.5 | |
| Pain | 6.9 ± 2.4 | |
| Penetrating Trauma | 30 (14%) | |
|
| ||
| Substance Use | ||
|
| ||
| ETOH Tested | 90 (40%) | |
| ETOH Amount | 64.6 ± 104.0 | |
| Drug Tested | 59 (26%) | |
| Drugs Found | 26 (12%) | |
| Positive Audit C | 89 (39%) | |
Although educational level and income are listed as categories, they were treated as continuous variables in the data analysis.
Step-Wise Analyses within each Domain
In the text, we report only the significant results of Step 4 for each domain. Each step of each analysis is fully reported in Table 2.
Table 2.
Odds ratios for being in the PTSD group compared to being in the PTSD absent group.
| Step-Wise Analyses | ||||
|---|---|---|---|---|
| Domain/Predictor | PTSD Symptoms Not Controlling for Baseline PTSD | PTSD Symptoms Controlling for Baseline PTSD | ||
| Odds Ratio (95% C I)a | b | Odds Ratio (95% C I)a | b | |
| DOMAIN: Demographic Variables | ||||
|
| ||||
| Step 1 | ||||
| Age | 0.96(.93–0.99)** | −0.04 | 0.95(.92–.99)** | −0.05 |
| Gender | 0.76(.34–1.66) | −0.28 | 0.73(.31–1.70) | −0.32 |
| Black/African American | 3.39(1.41–8.15)** | −1.22 | 2.30(.91–5.81)† | −0.83 |
| Other Racial Background | 1.59(.48–5.29) | −0.47 | 1.15(.29–4.59) | −0.14 |
| Hispanic Origin | 1.83(.71–4.71) | −0.60 | - | - |
| Married | 1.33(.47–3.82) | −0.29 | 1.13(.35–3.64) | −0.12 |
| Educational Level | 0.98(.72–1.34) | −0.02 | 1.01(.72–1.42) | −0.01 |
| Employment | 0.63(.29–1.34) | −0.47 | 1.03(.44–2.44) | −0.03 |
| Income | 0.89(.61–1.30) | −0.12 | 1.00(.66–1.51) | −0.00 |
| Step 2 (retain effects at p<.20) | ||||
| Age | 0.97(.95–.98)*** | −0.03 | 0.97(.95–.99)** | −0.04 |
| Black/African American | 1.77(.92–3.43)† | 0.57 | 1.53(.73–3.22) | −0.43 |
| Step 3 (retain effects at p<.10) | ||||
| Age | 0.97(.95–.98)*** | −0.03 | 0.96(.95–.98)*** | −0.04 |
| Black/African American | 1.77(.92–3.43)† | 0.57 | - | - |
| Step 4 (retain effects at p<.05) | ||||
| Age | 0.97(.95–.98)*** | −0.04 | 0.96(.95–.98)*** | −0.04 |
|
| ||||
| DOMAIN: Psychological Variables | ||||
|
| ||||
| Step 1 | ||||
| Patient Health Questionnaire (PHQ-8) | 1.14(1.07–1.22)*** | −0.13 | 1.08(1.01–1.16)* | 0.08 |
| Social Provisions Scale (SPS) | 1.04(.94–1.14) | −0.03 | 1.00(.90–1.10) | 0.00 |
| Connor-Davidson Resilience Scale (CD-RISC) | 0.99(.94–1.05) | −0.01 | 1.00(.94–1.06) | 0.00 |
| Pre-Morbid Psych Conditions | 1.26(.99–1.62)† | −0.23 | 1.19(.92–1.54)†† | 0.17 |
| Step 2 (retain effects at p<.20) | ||||
| Patient Health Questionnaire (PHQ-8) | 1.10(1.05–1.16)*** | 0.10 | 1.04(.98–1.11)†† | 0.04 |
| Pre-Morbid Psych Conditions | 1.40(1.12–1.73)*** | 0.11 | 1.29(1.03–1.63)* | 0.26 |
| Step 3 (retain effects at p<.10) | ||||
| Patient Health Questionnaire (PHQ-8) | 1.10(1.05–1.16)*** | 0.10 | - | - |
| Pre-Morbid Psych Conditions | 1.40(1.12–1.73)*** | 0.11 | 1.35(1.09–1.68)** | 0.30 |
| Step 4 (retain effects at p<.05) | ||||
| Patient Health Questionnaire (PHQ-8) | 1.10(1.05–1.16)*** | 0.10 | - | - |
| Pre-Morbid Psych Conditions | 1.40(1.12–1.73)*** | 0.11 | 1.35(1.09–1.68)** | 0.30 |
|
| ||||
| DOMAIN: Cause of Injury | ||||
|
| ||||
| Step 1 | ||||
| Fall | 1.30(.33–5.18) | 0.26 | 0.82(.18–3.64) | −0.20 |
| Motor Vehicle Collision | 3.13(0.80–12.17)†† | 1.14 | 1.51(.35–6.58) | −0.41 |
| Gunshot/Stab Wound | 9.00(2.09–38.79)** | 2.20 | 4.99(1.04–24.02)* | −1.61 |
| Aggravated Assault | 2.78(0.53–14.50) | 1.02 | 1.09(.18–6.59) | −0.08 |
| Motorcycle Collision | 2.50(.57–10.93) | 0.92 | 1.82(.37–9.03) | −0.60 |
| Auto vs Pedestrian | 7.14(1.48–34.38)* | 1.97 | 3.62(.66–19.77)†† | −1.29 |
| Step 2 (retain effects at p<.20) | ||||
| Motor Vehicle Collision | 1.92(0.96–3.84) † | 0.65 | - | - |
| Gunshot/Stab Wound | 5.52(2.30–13.26)*** | 1.71 | 4.19(1.64–10.68)** | 1.43 |
| Auto vs Pedestrian | 4.38(1.53–12.52)** | 1.48 | 3.03(.98–9.41)† | 1.11 |
| Step 3 (retain effects at p<.10) | ||||
| Motor Vehicle Collision | 1.92(0.96–3.84) † | 0.65 | - | - |
| Gunshot/Stab Wound | 5.52(2.30–13.26)*** | 1.71 | 4.19(1.64–10.68)** | 1.43 |
| Auto vs Pedestrian | 4.38(1.53–12.52)** | 1.48 | 3.03(.98–9.41)† | 1.11 |
| Step 4 (retain effects at p<.05) | ||||
| Gunshot/Stab Wound | 4.46(1.93–10.34)*** | 1.50 | 3.72(1.47–9.41)** | 1.32 |
| Auto vs Pedestrian | 3.54(1.28–9.83)* | 1.27 | 1.11 | |
|
| ||||
| DOMAIN: Hospitalization and Complications | ||||
|
| ||||
| Step 1 | ||||
| Days on Ventilator | 1.07(.89–1.29) | −0.07 | 1.09(.87–1.36) | −0.08 |
| Intensive Care Unit Length of Stay | 0.92(.79–1.06) | −0.09 | 0.92(.78–1.07) | −0.09 |
| Total Hospital Length of Stay | 1.00(.96–1.03) | −0.00 | 0.98(.95–1.02) | −0.02 |
| Total Complications | 1.23(.94–1.61) †† | −0.21 | 1.09(.79–1.50) | −0.08 |
| Total Co-morbid Processes | 1.00(.83–1.21) | −0.00 | 0.96(.77–1.20) | −0.04 |
| Step 2 (retain effects at p<.20) | ||||
| Total Complications | 1.10(.90–1.36) | −0.10 | - | - |
|
| ||||
| DOMAIN: Injury –Related Variables | ||||
|
| ||||
| Step 1 | ||||
| Injury Severity Score (ISS) | 1.00(.97–1.04) | 0.00 | 0.98(.94–1.03) | −0.02 |
| Glascow Coma Scale (GCS) | 1.08(.92–1.27) | 0.08 | 1.08(.90–1.31) | −0.08 |
| Pulse | 1.03(1.01–1.04)** | 0.03 | 1.02(1.00–1.04)* | −0.02 |
| Pain at Baseline | 1.16(1.01–1.32)* | 0.15 | 1.09(.94–1.26) | −0.08 |
| Step 2 (retain effects at p<.20) | ||||
| Pulse | 1.02(1.01–1.04)** | 0.02 | 1.02(1.00–1.03)* | −0.02 |
| Pain at Baseline | 1.16(1.02–1.32)* | 0.15 | - | - |
| Step 3 (retain effects at p<.10) | ||||
| Pulse | 1.02(1.01–1.04)** | 0.02 | 1.02(1.00–1.03)* | −0.02 |
| Pain at Baseline | 1.16(1.02–1.32)* | 0.15 | - | - |
| Step 4 (retain effects at p<.05) | ||||
| Pulse | 1.02(1.01–1.04)** | 0.02 | 1.02(1.00–1.03)* | −0.02 |
| Pain at Baseline | 1.16(1.02–1.32)* | 0.15 | - | - |
|
| ||||
| DOMAIN: Substance Use | ||||
|
| ||||
| Step 1 | ||||
| Positive AUDIT-C | 2.03(1.02–4.03)* | 0.71 | 1.65(.77–3.57) | −0.50 |
| Positive Alcohol Screen | 1.11(0.23–5.37) | 0.11 | 0.65(.11–3.97) | −0.43 |
| Alcohol Level | 1.00(.99–1.01) | 0.00 | 1.00(.99–1.01) | −0.00 |
| Step 2 (retain effects at p<.20) | ||||
| Positive AUDIT-C | 2.10(1.07–4.13)* | 0.74 | - | - |
| Step 3 (retain effects at p<.10) | ||||
| Positive AUDIT-C | 2.10(1.07–4.13)* | 0.74 | - | - |
| Step 4 (retain effects at p<.05) | ||||
| Positive AUDIT-C | 2.10(1.07–4.13)* | 0.74 | - | - |
|
| ||||
| DOMAIN: Final Combined Analysis | ||||
|
| ||||
| Step 1 | ||||
| Age at Injury | 0.98(.95–1.00)* | −0.03 | 0.97(.95–.99)** | −0.03 |
| PHQ | 1.12(1.05–1.19)*** | −0.11 | - | - |
| Pre-morbid Psych Conditions | 1.44(1.13–1.84)** | −0.37 | 1.40(1.11–1.76)** | −0.33 |
| Gunshot/Stab Wound | 3.66(1.32–10.19)* | −1.30 | 2.38(0,88–6.41)† | −0.87 |
| Auto vs Pedestrian | 2.90(.90–9.35)† | −1.06 | - | -- |
| Pain Level at Baseline | 1.06(.90–1.24) | −0.05 | - | - |
| Pulse | 1.01(1.00–1.03)†† | −0.01 | 1.01(.99–1.03) | −0.01 |
| Positive AUDIT-C | 2.27(.93–5.51)† | −0.82 | - | - |
| Step 2 (retain effects at p<.20) | ||||
| Age at Injury | 0.98(.95–1.00)* | −0.02 | 0.97(.94–.99)** | −0.03 |
| PHQ | 1.12(1.06–1.19)*** | −0.12 | - | - |
| Pre-morbid Psych Conditions | 1.41(1.11–1.78)** | −0.34 | 1.39(1.10–1.79)** | −0.33 |
| Gunshot/Stab Wound | 3.87(1.41–10.62)** | −1.35 | 2.39(0.89–6.40)* | −0.87 |
| Auto vs Pedestrian | 3.01(.94–9.69)† | −1.10 | - | -- |
| Pulse | 1.01(1.00–1.03)†† | −0.01 | - | - |
| Positive AUDIT-C | 2.20(.92–5.30)† | −0.79 | - | - |
| Step 3 (retain effects at p<.10) | ||||
| Age at Injury | 0.97(.95–.99)* | −0.03 | 0.97(.95–.99)** | −0.03 |
| PHQ | 1.12(1.06–1.19)*** | −0.11 | - | - |
| Pre-morbid Psych Conditions | 1.41(1.12–1.79)** | −0.34 | 1.42(1.13–1.80)** | −0.35 |
| Gunshot/Stab Wound | 4.03(1.48–10.96)** | −1.39 | 2.77(1.02–7.54)* | −1.02 |
| Auto vs Pedestrian | 3.42(1.11–10.59)* | −1.23 | - | - |
| Positive AUDIT-C | 2.38(1.00–5.67)† | −0.87 | - | - |
| Step 4 (retain effects at p<.05) | ||||
| Age at Injury | 0.97(.95–.99)* | −0.03 | 0.96(.94–.9)*** | −0.03 |
| PHQ | 1.12(1.06–1.19)*** | −0.11 | - | - |
| Pre-morbid Psych Conditions | 1.41(1.12–1.79)** | −0.34 | 1.37(1.10–1.72)** | 0.32 |
| Gunshot/Stab Wound | 4.03(1.48–10.96)** | −1.39 | - | - |
| Auto vs Pedestrian | 3.42(1.11–10.59)* | −1.23 | - | - |
| Positive AUDIT-C | 2.38(1.00–5.67)* | −0.87 | - | - |
Odds ratio is for the odds of being in this PTSD group compared to the odds of being in the “No PTSD” group.
All cases in the Recovery group had only “blunt” trauma. Thus, the SD was 0 and the p value was not calculable.
p<.20,
p<.10,
p<.05,
p<.01,
p<.001
Demographic Characteristics
Age was the only demographic variable that was significantly related to PTSD symptom status in Step 4 for demographic characteristics. The odds of being symptomatic were higher for younger, compared to older, patients (OR=.97, p<.001).
Psychological Variables
Step 4 for the psychological variables showed that the odds of being symptomatic were higher for those with higher levels of depressive symptoms (OR=1.12, p<.001) and for those reporting more premorbid psychiatric diagnoses (OR=1.40, p=.003).
Cause of Injury
The analyses of the cause of injury were different from the analyses of the other domains of predictors since, unlike the other domains, these causes were mutually exclusive (if the cause was a gunshot wound, it was not caused by a motor vehicle collision). We dummy coded each cause. Analyses indicated that the odds of being symptomatic were greater for gunshot/stabbing victims than for other victims (OR=4.46, p<.001). Similarly, the odds of being symptomatic were also higher for pedestrian victims hit by a motor vehicle than other victims (OR=3.54, p=.015).
Hospitalization and Complications
Step 4 of the analysis of the hospitalization characteristics showed that the odds of being symptomatic were not significantly related to any of our hospitalization or complications measures.
Injury-related Variables
Higher levels of pain were related to higher odds of being symptomatic at 3 months (OR=1.16, p=.027), and higher pulse rate at admission was similarly related to higher odds of being asymptomatic at the 3 month follow-up (OR=1.02, p=.002).
Substance Use
Step 4 for the substance use variables indicated that the odds of being symptomatic were higher for those who met criteria for alcohol use disorders on the AUDIT-C (OR=2.10, p=.031).
Final Model with All Significant Variables
The final model included the simultaneous entry of all the variables found to be significant in Step 4 of the analyses of each domain. The four Steps for the final model are presented in Table 2.
We discuss only the results for the final step (Step 4) of the final model. In this model, younger patients had greater odds of being symptomatic (OR=0.97, p=.011) than older patients. Also, higher levels of depressive symptoms were related to higher odds of being symptomatic (OR=1.12, p<.001). In addition, a greater number of premorbid psychiatric diagnoses was related to higher odds of being symptomatic (OR=1.41, p=.004), as was meeting criteria for alcohol use disorder on the Audit-C (OR=2.38, p=.050). Finally, type of injury was also related to being symptomatic on the PC-PTSD. Those who were shot/stabbed and those who were pedestrians hit by a motor vehicle had higher odds of being symptomatic at the 3 month follow-up (OR=4.03, p=.006, and OR=3.42, p=.033, respectively).
Predictors of PC-PTSD criterion at 3 months controlling for PC-PTSD symptoms at baseline
Demographic Characteristics
Age was the only demographic variable that was significantly related to PTSD symptom status in Step 4 for demographic characteristics when controlling for baseline PC-PTSD scores. The odds of being symptomatic were higher for younger compared to older patients (OR=.96, p<.001).
Psychological Variables
Step 4 for the psychological variables showed that the odds of being symptomatic were higher for those reporting more premorbid psychiatric diagnoses (OR=1.35, p=.007), after controlling for baseline PC-PTSD scores.
Cause of Injury
After controlling for baseline PC-PTSD score, the odds of being symptomatic were greater for gunshot/stabbing victims than for other victims (OR=3.72, p=.005).
Hospitalization and Complications
Step 4 of the analysis of the hospitalization characteristics showed that the odds of being symptomatic were unrelated to any of our hospitalization or complications measures.
Injury-related Variables
Only a higher pulse was related to higher odds of being symptomatic (OR=1.02, p=.045), while controlling for baseline PC-PTSD scores.
Substance Use
Step 4 for the substance use variables indicated that the odds of being symptomatic were unrelated to any of the substance abuse predictors, after controlling for baseline PC-PTSD scores.
Final Model with All Significant Variables, controlling for baseline PC-PTSD
The final model included the simultaneous entry of all the variables found to be significant in Step 4 of the analyses of each domain. The four Steps for the final model are presented in Table 2.
We discuss only the results for the final step (Step 4) of the final model. After controlling for baseline PC-PTSD (which was significantly related to the odds of being symptomatic at the 3 month follow-up [OR=1.94, p<.001], only two predictors remained significant. Younger patients had greater odds of being symptomatic (OR=0.96, p=.001) than older patients. And a greater number of premorbid psychiatric diagnoses was related to higher odds of being symptomatic (OR=1.37, p=.006.
Accuracy of Predicting PTSD Symptomology 3 Months Later
Our logistic regression models can be used to calculate the probability of being symptomatic at the 3-month follow-up. Table 3 presents the classification tables, which show the model-based predictions of being symptomatic at 3 months (those with a probability of .5 or higher are predicted to be symptomatic) and the actual report of them being symptomatic 3 months later. Both models (the model including baseline PC-PTSD as a covariate and the model not including baseline PC-PTSD) are very similar in their predictions and in the accuracy of their predictions, with the accuracy of predicting being symptomatic or not at follow-up in both models being slightly greater than 76%. As is typical in logistic regression models, the models more accurately predicted the outcome that is more frequent (not being symptomatic), with both models accurately predicting about 85% of those cases. Prediction of the less frequent outcome (being symptomatic) is not quite as good (60%), but still relatively high. One can more accurately predict those who will be symptomatic by using a lower cutoff than .50 probability to predict classification, but the tradeoff is a greater likelihood of false positives (predicting being symptomatic for those who don’t turn out to be symptomatic). Figure 1 shows the ROC curve plotting the tradeoff between correct positives and false positives for these models. This Figure shows that one can identify 90% of those who will be symptomatic at 3 months and perhaps proactively intervene to decrease that likelihood, but at the cost of intervening in 44.5% of the cases would otherwise not become symptomatic.
Table 3.
Predicted and actual PTSD level symptomatology on the PC-PTSD (PC-PTSD≥3)
| Actual PTSD level of Symptoms | Predicted PTSD level of Symptoms
|
|||
|---|---|---|---|---|
| Model not Controlling for Baseline Symptoms | Model Controlling for Baseline Symptoms | |||
|
| ||||
| NO | YES | NO | YES | |
|
|
||||
| NO | 84.9% | 15.1% | 85.1% | 14.9% |
| YES | 40.0% | 60.0% | 39.7% | 60.3% |
|
|
||||
Figure 1.
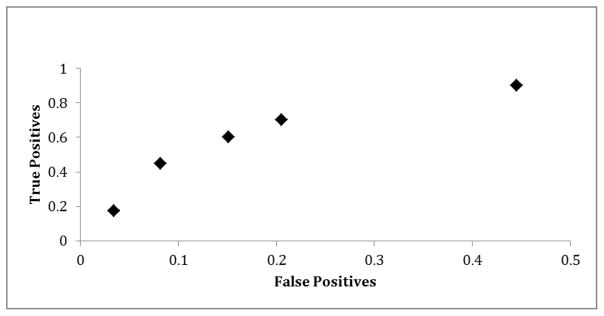
ROC Curve
Discussion
The aim of the present study was to identify predictors of PTSD level symptoms 3 months after admission to a Level I Trauma Center. Multinomial logistic regression showed that, age, depression, number of premorbid psychiatric disorders, gunshot wound, auto vs. pedestrian accident, and alcohol use predicted who had PTSD symptoms at 3-month follow up with 76.3% accuracy. However, when controlling for PTSD severity at baseline, only age, number of premorbid psychiatric disorders, and gunshot wounds predicted PTSD symptoms at 3-month follow up, but with 78.5% accuracy.
Our findings are consistent with the existing literature on PTSD predictors suggesting younger age (Alarcon et al., 2012; Chiu, deRoon-Cassini, & Brasel, 2011), depression (O’Donnell, Creamer, & Pattison, 2004; Shalev et al., 1998), number of premorbid psychiatric disorders (Nickel & Egle, 2006), gunshot wounds/penetrating injuries (Alarcon et al., 2012), auto vs. pedestrian accidents (Alarcon et al., 2012), and alcohol use (McFarlane et al., 2009) are all risk factors for PTSD. However, after controlling for PTSD symptoms at the time of admission, only age, number of premorbid psychiatric disorders, and gunshot wounds remained as significant predictors of later PTSD. Gunshot wounds may be a proxy for trauma severity and type (interpersonal). However, a study with combat traumas suggested that gunshot wounds predicted having some type of mental health diagnosis but not PTSD specifically (MacGregor et al., 2009). Future studies with civilians could include a diagnostic interview to determine if these findings translate from the military population. Consistent with our findings, psychiatric history has also been identified as a potential predisposing factor for development of PTSD (Kessler, Sonnega, Bromet, Hughes, Nelson, & Breslau, 1999). Why this is the case is less clear. For example, it could be that psychiatric severity is associated with several other risk factors such as lower social support, income, and living in environments more prone to trauma. However, our study controlled for many of these alternative explanations and at least one other study showed that it may be more likely that a similar risk factor may predict both PTSD and psychiatric history (McMillen, North, Mosley, & Smith, 2002). Finally, younger age has also been consistently found as a predictor of PTSD (Brewin et al., 2000; Ozer et al., 2003). However, one study suggested younger age may simply be a proxy for assaultive trauma and low SES (Chiu et al., 2011). This is contrary to what we found as trauma type and SES was controlled for and age still came out as a significant independent predictor. It is not clear on the surface what is responsible for the discrepancy. It could be due to differences in data analysic strategy, populations, or assessment instruments. Hopefully replication and extension of the present research will help further determine the reason for the relationship between age and PTSD.
Several variables did not significantly predict PTSD in our study (i.e. gender, ethnicity, education, income, work status, injury severity score, Glasgow coma scale, social support, resilience, marital status, and ICU length of stay). However, these variables were identified as risk factors in previous reports (Alarcon et al., 2012; Chiu et al., 2011; Clapp & Gayle Beck, 2009; Daniels et al., 2012; Harris, Young, Rae, Jalaludin, & Solomon, 2008; O’Donnell, Creamer, Holmes, et al., 2010; O’Donnell, Creamer, McFarlane, Silove, & Bryant, 2010; Peris et al., 2011; Richter, Waydhas, & Pajonk, 2006). Among the possible explanations for the discrepancy in these findings are differences in patient samples, settings, and control features including the novel analysis strategies (i.e. Fournier et al., 2009) in our study. Indeed, one strength of the present study is the simultaneous examination of potential predictors of PTSD symptoms, which allowed us to control for many possible third-variable explanations. Thus, our analyses eliminated many proxy risk factors. Power analyses show that our sample was large enough to detect medium effect sizes with a power of .80 or greater, thereby being able to detect important predictors of PTSD symptoms categories. Accordingly, we did not have sufficient power to detect small (perhaps meaningful) effects. Thus, our analytical approach was conservative: powerful enough to identify substantial predictors, but with strong controls to avoid erroneously identifying proxy risk factors.
Identifying early predictors of PTSD following traumatic injury provides useful information for clinical care. The results of this study suggest that screening for PTSD symptoms in a trauma center for all patients would be a clinically useful endeavor given that a little under half of the sample had substantial PTSD symptoms at either baseline, at three months or at both time points. However, given the limited resources in many trauma centers, our findings provide some direction on intervening to reduce the risk for PTSD. Specifically, if replicated, our findings suggest that effective preventative interventions for PTSD may be best targeted to those who are admitted with gunshot wounds, are younger, and have significant psychiatric history. Our findings also suggest that trauma programs should have some type of routine follow up visit for trauma patients after discharge so they can be assessed for PTSD symptoms given that over one-third of our sample either developed PTSD symptoms at three months or continued to have PTSD symptoms at three months. It is unclear how many trauma programs provide routine follow up visits for their patients, or what percentage of patients attend follow-up visits if they are available. Additionally, by identifying those patients at risk, trauma centers could see a potential cost savings (Greenberg et al., 1999).
Several limitations deserve mention. First, ours was a convenience sample of trauma patients who were prospectively enrolled upon hospital admission. However, the subjects who were approached and agreed to be in the study were similar to the subjects who approached and declined to be in the study. Additionally, the fact that most of our data came from self-report measures, including our measure of PTSD symptoms, is a limiting factor. Although the measure used to determine PTSD is widely-used, valid and reliable screening tool for PTSD in hospital settings, an additional clinical diagnosis confirming potential diagnosis of PTSD or other symptom assessment measures would have made the results more compelling. Further, relying on self-report of comorbid mental disorders may also be problematic, though this methodology is reflective of real-world assessments in a hospital setting. Additionally, the study was also limited in terms of the assessment interval. Specifically, we did not include an assessment of PTSD symptoms at 1-month following injury, which coincides with the required time for a formal diagnosis of acute PTSD. Also, rather than choose only certain predictors based on previous (inconsistent) findings, we opted to conduct the Fournier analysis entering all available predictors. Thus, future studies should shed more light on theoretical underpinnings of the findings that are replicated. Finally, it is unclear if the predictors of later PTSD symptomatology or recovery, respectively, would be different at later follow-ups (i.e., six months, twelve months). Further research should examine the stability of these PTSD symptom predictors. By better identifying which patients are at risk for continued PTSD, as well as individuals who may develop PTSD at a later time period, education and resources can be provided at the time of admission to the trauma center and thus ultimately reduce the rates of PTSD in this potentially vulnerable population.
Highlights.
We examined predictors of PTSD among participants (N = 227) admitted to a Level I Trauma Center
Participants were screened at baseline and 3-months later.
We examined data with a novel multinomial logistic regression analysis strategy (Fournier et al., 2009).
The strongest predictors of PTSD were young age, gunshot wounds, and/or a history of psychiatric disorders
Acknowledgments
Portions of this research were funded by the Stanley Seeger Foundation and a grant from the National Institute on Drug Addiction K01 DA035930.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alarcon LH, Germain A, Clontz AS, Roach E, Nicholas DH, Zenati MS, Sperry JL. Predictors of acute posttraumatic stress disorder symptoms following civilian trauma: highest incidence and severity of symptoms after assault. The Journal of Trauma and Acute Care Surgery. 2012;72(3):629–635. doi: 10.1097/TA.0b013e31824416aa. discussion 635–627. [DOI] [PubMed] [Google Scholar]
- American College of Surgeons. Verified trauma centers. 2012 from http://www.facs.org/trauma/verified.html.
- Amir N, Taylor CT, Donohue MC. Predictors of response to an attention modification program in generalized social phobia. Journal of Consulting and Clinical Psychology. 2011;79(4):533–541. doi: 10.1037/a0023808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker SP, O’Neill B, Haddon WJ, Long WB. The Injury Severity Score: A method for describing patients with multiple injuries and evaluating emergency care. The Journal of Trauma. 1974;14:187–196. [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68:748–766. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB. The AUDIT Alcohol Consumption Questions (AUDIT-C): An effective brief screening test for problem drinking. Archives of Internal Medicine. 1998;3:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Chiu KB, deRoon-Cassini TA, Brasel KJ. Factors identifying risk for psychological distress in the civilian trauma population. Academic Emergency Medicine. 2011;18(11):1156–1160. doi: 10.1111/j.1553-2712.2011.01206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clapp JD, Gayle Beck J. Understanding the relationship between PTSD and social support: the role of negative network orientation. Behaviour Research and Therapy. 2009;47(3):237–244. doi: 10.1016/j.brat.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) Depression and Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Conrad EJ, Hansel TC, Pejic NG, Constans J. Assessment of Psychiatric Symptoms at a Level I Trauma Center Surgery Follow-up Clinic: A Preliminary Report. The American Journal of Surgery. 2013;79(5):492–494. [PubMed] [Google Scholar]
- Creamer M, Bell R, Failla S. Psychometric properties of the impact of event scale - revised. Behaviour Research and Therapy. 2003;41:1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Russell D. The provision of social relationships and adaptation to stress. In: Jones WH, Perlman D, editors. Advances in Personal Relationships. Greenwich, CT: JAI Press; 1987. pp. 37–67. [Google Scholar]
- Daniels JK, Hegadoren KM, Coupland NJ, Rowe BH, Densmore M, Neufeld RW, Lanius RA. Neural correlates and predictive power of trait resilience in an acutely traumatized sample: a pilot investigation. Journal of Clinical Psychiatry. 2012;73(3):327–332. doi: 10.4088/JCP.10m06293. [DOI] [PubMed] [Google Scholar]
- Fournier JC, DeRubeis RJ, Shelton RC, Hollon SD, Amsterdam JD, Gallop R. Prediction of response to medication and cognitive therapy in the treatment of moderate to severe depression. Journal of Consulting and Clinical Psychology. 2009;77(4):775–787. doi: 10.1037/a0015401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraenkel L, Falzer P, Fried T, Kohler M, Peters E, Kerns R, Leventhal H. Measuring pain impact versus pain severity using a numberic rating scale. Journal of General Internal Medecine. 2012;27:555–560. doi: 10.1007/s11606-011-1926-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg PE, Sisitsky T, Kessler RC, Finkelstein SN, Berndt ER, Davidson JRT, Fyer AJ. The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatry. 1999;60(7):427–435. doi: 10.4088/jcp.v60n0702. [DOI] [PubMed] [Google Scholar]
- Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwatzman A. National hospital discharge survey: 2007 summary. National Health Statistics Reports. 2010;29:1–20. [PubMed] [Google Scholar]
- Harris IA, Young JM, Rae H, Jalaludin BB, Solomon MJ. Predictors of post-traumatic stress disorder following major trauma. ANZ Journal of Surgery. 2008;78(7):583–587. doi: 10.1111/j.1445-2197.2008.04578.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, Breslau NN. Epidemiological risk factors for trauma and PTSD. In: Yehuda R, editor. Risk factors for PTSD. Washington DC: American Psychiatric Press; 1999. [Google Scholar]
- Kroenke K, Spitzer R, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medecine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund I, Lundberg T, Sandberg L, Budh CN, Kowalski J, Svensson E. Lack of interchangeability between visual analogue and verbal rating pain scales: A cross sectional description of pain etiology groups. BMC Medical Research Methodology. 2005;5:31. doi: 10.1186/1471-2288-5-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacGregor AJ, Corson KS, Larson GE, Shaffer RA, Dougherty AL, Galarneau MR, Raman R, Baker DG, Lindsay SP, Golomb BA. Injury-specific predictors of posttraumatic stress disorder. Injury. 2009;40:1004–1010. doi: 10.1016/j.injury.2009.04.006. [DOI] [PubMed] [Google Scholar]
- McFarlane AC, Browne D, Bryant RA, O’Donnell M, Silove D, Creamer M, Horsley K. A longitudinal analysis of alcohol consumption and the risk of posttraumatic symptoms. Journal of Affective Disorders. 2009;118:166–172. doi: 10.1016/j.jad.2009.01.017. [DOI] [PubMed] [Google Scholar]
- McMillen C, North C, Mosley M, Smith E. Untangling the psychiatric comorbidity of posttraumatic stress disorder in a sample of flood survivors. Comprehensive Psychiatry. 2002;43:478–485. doi: 10.1053/comp.2002.34632. [DOI] [PubMed] [Google Scholar]
- National Center for Injury Prevention and Control (NCIPC). Web-based injury statistics query and reporting system (WIQARS) 2011 Retrieved November 5 2012, 2012, from http://www.cdc.gov/injury/wisqars.
- Nickel R, Egle UT. Psychological defense styles, childhood adversities and psychopathology in adulthood. Child Abuse Negl. 2006;30(2):157–170. doi: 10.1016/j.chiabu.2005.08.016. [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Creamer M, Holmes AC, Ellen S, McFarlane AC, Judson R, Bryant RA. Posttraumatic stress disorder after injury: does admission to intensive care unit increase risk? The Journal of Trauma. 2010;69(3):627–632. doi: 10.1097/TA.0b013e3181bc0923. [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Creamer M, Pattison P. Posttraumatic stress disorder and depression following trauma: understanding comorbidity. American Journal of Psychiatry. 2004;161(8):1390–1396. doi: 10.1176/appi.ajp.161.8.1390. [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Creamer MC, McFarlane AC, Silove D, Bryant RA. Does access to compensation have an impact on recovery outcomes after injury? Medical Journal of Australia. 2010;192(6):328–333. doi: 10.5694/j.1326-5377.2010.tb03532.x. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychological Bulletin. 2003;129(1):52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Peris A, Bonizzoli M, Iozzelli D, Migliaccio ML, Zagli G, Bacchereti A, Belloni L. Early intra-intensive care unit psychological intervention promotes recovery from post traumatic stress disorders, anxiety and depression symptoms in critically ill patients. Critical Care. 2011;15(1):R41. doi: 10.1186/cc10003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review. 2010;30(6):635–641. doi: 10.1016/J.Cpr.2010.04.007. [DOI] [PubMed] [Google Scholar]
- Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, Sheikh JI. The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry. 2003;9:9–14. [Google Scholar]
- Reese C, Pederson T, Avila S, Koseph K, Nagy K, Dennis A, Wiley D, Starr F, Bokhari F. Screening for traumatic stress among survivors of urban trauma. Journal of Trauma and Acute Care Surgery. 2012;73:462–467. doi: 10.1097/TA.0b013e31825ff713. [DOI] [PubMed] [Google Scholar]
- Richter JC, Waydhas C, Pajonk FG. Incidence of posttraumatic stress disorder after prolonged surgical intensive care unit treatment. Psychosomatics. 2006;47(3):223–230. doi: 10.1176/appi.psy.47.3.223. [DOI] [PubMed] [Google Scholar]
- Riggs DS, Rothbaum BO, Foa EB. A Prospective Examination of Symptoms of Posttraumatic Stress Disorder in Victims of Nonsexual Assault. Journal of Interpersonal Violence. 1995;10(2):201–214. doi: 10.1177/0886260595010002005. [DOI] [Google Scholar]
- Rothbaum BO, Foa EB, Riggs DS, Murdock T, Walsh W. A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress. 1992;5(3):455–475. [Google Scholar]
- Rothbaum BO, Kearns MC, Price M, Malcoun E, Davis M, Ressler KJ, Houry D. Early intervention may prevent the development of posttraumatic stress disorder: a randomized pilot civilian study with modified prolonged exposure. Biological Psychiatry. 2012;72(11):957–963. doi: 10.1016/j.biopsych.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowley G, Fielding K. Reliability and accuracy of the Glasgow Coma Scale with experiences and inexperienced users. Lancet. 1991;337:535–538. doi: 10.1016/0140-6736(91)91309-i. [DOI] [PubMed] [Google Scholar]
- Shalev AY, Freedman S, Peri T, Brandes D, Sahar T, Orr SP, Pitman RK. Prospective study of posttraumatic stress disorder and depression following trauma. American Journal of Psychiatry. 1998;155(5):630–637. doi: 10.1176/ajp.155.5.630. [DOI] [PubMed] [Google Scholar]
- Sledjeski EM, Speisman B, Dierker LC. Does number of lifetime traumas explain the relationship between PTSD and chronic medical conditions? Answers from the National Comorbidity Survey-Replication (NCS-R) Journal of Behavioral Medicine. 2008;31:341–349. doi: 10.1007/s10865-008-9158-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. Lancet. 1974:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Teasdale G, Jennett B. Assessment and prognosis of coma after head injury. Acta Neurochirurgica. 1976;34:45–55. doi: 10.1007/BF01405862. [DOI] [PubMed] [Google Scholar]
- Teasdale G, Kril-Jones R, van der Sande J. Observer variability in assessing impaired consciousness and coma. Journal of Neurology, Neurosurgery & Psychiatry. 1978;41:603–610. doi: 10.1136/jnnp.41.7.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Emmerik AA, Kamphuis JH, Hulsbosch AM, Emmelkamp PMG. Single session debriefing after psychological trauma: A meta-analysis. The Lancet. 2002;360(9335):766–771. doi: 10.1016/S0140-6736(02)09897-5. [DOI] [PubMed] [Google Scholar]
- White B, Driver S, Warren AM. Resilience and indicators of adjustment during rehabilitation from a spinal cord injury. Rehabilitation Psychology. 2010;55(1):23–32. doi: 10.1037/a0018451. [DOI] [PubMed] [Google Scholar]
- Zatzick D, Jurkovich G, Russo J, Roy-Byrne P, Katon W, Wagner A, Rivara F. Posttraumatic distress, alcohol disorders, and recurrent trauma across level 1 trauma centers. The Journal of Trauma. 2004;57(2):360–366. doi: 10.1097/01.ta.0000141332.43183.7f. [DOI] [PubMed] [Google Scholar]


