Abstract
Patient: Male, 59
Final Diagnosis: Pulmonary embolism
Symptoms: Cardiac arrest • chest pain • dyspnea
Medication: —
Clinical Procedure: Angioplasty
Specialty: Nephrology
Objective:
Rare disease
Background:
Vascular access is the lifeline of hemodialysis patients and access problems are a major source of morbidity and mortality for these patients. Access stenosis and thrombosis are common problems in dialysis patients and require prompt intervention. Every year thousands of these procedures are performed in the United States by radiologists, surgeons, and interventional nephrologists.
Case Report:
A 59-year-old man on chronic hemodialysis with multiple medical problems, including diabetes mellitus, hypertension, chronic obstructive lung disease, hepatitis C infection, and end-stage renal disease, who had clotted his access several times before ,presented with another episode of access clotting. He underwent declotting successfully but upon angioplasty of the access feeding artery, he developed massive pulmonary embolism and died. Postmortem examination showed multiple pulmonary emboli, including cholesterol crystals in his lungs.
Conclusions:
Hemodialysis access declotting and angioplasty are usually benign and do not cause a major problem. However, occasionally they become complicated. In difficult cases and in people with multiple comorbidities, it is preferable to forego the existing dialysis access and either plan for creation of a new vascular access or place a central vein catheter.
MeSH Keywords: Hypercholesterolemia, Blood Coagulation, Renal Dialysis, Pulmonary Embolism
Background
Due to platelet abnormalities resulting from accumulation of uremic toxins [1,2] thromboembolism is rare in dialysis patients and although dialysis treatment decreases platelet abnormality, it does not eliminate it [3]. Due to this, deep vein thrombosis and pulmonary embolism (PE) are rare events in patients with end-stage renal disease [4]. Occasionally, use of recombinant erythropoietin and heparin-induced thrombocytopenia have been reported to be the cause of pulmonary or cerebral embolism [5–7]. When observed, PE could be the result of vascular access infection/thrombosis [6] or a complication of central vein hemodialysis catheters [8]. Vascular access problems, especially access clotting, are common in dialysis patients and every year thousands of these procedures are performed by radiologists, vascular surgeons, and interventional nephrologists in the United States. These interventions are usually successful and free from major complications. However, occasionally, serious complications develop [9,10]. Herein we report such a case.
Case Report
The patient was a 59-year-old Caucasian man with history of diabetes mellitus for many years, arterial hypertension, coronary artery disease, chronic obstructive pulmonary disease, chronic hepatitis C infection, obesity, and end-stage renal disease, on hemodialysis since 2008. His vascular access was a left arm arteriovenous (AV) graft fistula. This access clotted on several occasions and every time it was declotted successfully by the interventional radiologist. He presented on a late Friday afternoon with another episode of access clotting and since he was not fluid overloaded and his serum electrolytes were within the normal range, a decision was made to declot him on Monday of the following week and he was placed on sodium polystyrene sulfonate to prevent him from becoming hyperkalemic. On Monday, he presented to interventional radiology (IR) and he had no complaints. His blood pressure, serum potassium, bicarbonate, prothrombin, and thromboplastin times were within the normal limits. Later on that day, he was taken to IR for access declotting. Initially, the area over-lying the access was anesthetized with several milliliters of lidocaine, French brite tip short sheaths were used to traverse the anastomoses, and then a Kumpe catheter was placed through a glide wire. Once the anastomosis was traversed, contrast was injected and it showed a large clot in the graft outflow vein extending into the left axillary vein. Heparin 5000 units was given, the catheter was advanced into the superior vena cava, and a balloon angioplasty was performed on the left axillary vein. The cleaner thrombectomy device was used to lyse clots in the left axillary vein and throughout the graft. Toward the end of the declotting procedure, the patient became dyspneic but he recovered quickly with supplemental oxygen. During the procedure, the radiologist noted a tight stenosis in the arterial inflow of the access and an angioplasty was performed. Shortly after angioplasty, he developed severe chest pain and dyspnea and he developed cardiopulmonary arrest. Cardiopulmonary resuscitation was unsuccessful and the patient died.
At postmortem examination, the patient was found to have emboli in both pulmonary arteries, pleural effusion, coronary artery disease, and cardiomegaly. Examination of the lungs showed a large embolus closing a major branch point of the right pulmonary artery, a smaller clot in the left pulmonary artery, and multiple clots in smaller pulmonary vessels. In addition, there were multiple cholesterol emboli (Figure 1) and increased number of hemosiderin-laden macrophages, indicating that cholesterol emboli were old rather than due to the recent episode of pulmonary embolism.
Figure 1.
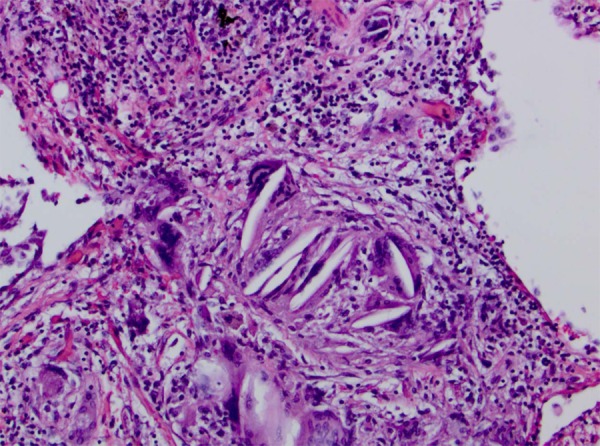
Lung tissue demonstrating cholestrol clefts and infiltration of giant cells indicating that cholestrol embolizations occurred earlier during previous attempts at access declotting, rather than during the final event (×20 magnification).
Discussion
In the United States thousands of people are living on hemodialysis and every year 100 000 or more people are added to this population. Most of these people are on hemodialysis and only a small fraction (about 7%) undergo peritoneal dialysis. In spite of all the efforts by the Fistula First initiative in the last 6 to 6 years, close to 55% of US patients have a fistula and the rest are dialyzed through a graft or a catheter. Grafts, compared to fistulas, are more prone to stenosis and infection but both forms of access are prone to clotting. Access flow, access clotting, and declotting are major problems for dialysis patients and they are a major problem for dialysis units, vascular surgeons, radiologists and interventional nephrologists. Vascular access construction and maintenance are major expenses for both Medicare and private insurers.
Access declotting is done in different ways, and, according to most radiologists, there is no best or worst way to declot an access [11]. It is the experience of the operator that determines the success or failure of any procedure. Access declotting is associated with a high rate of success (90% or better) and is usually free from complications [12,13]. Some radiologists believe percutaneous declotting has better results compared to surgery [14]. Declotting often leads to subclinical and asymptomatic embolization of debris to the lungs, and, not uncommonly, to vessel rupture and bleeding. Embolization is usually to the lungs, but in the presence of a patent foramen ovale (PFO), systemic embolization is possible but it is rare [15].
Our patient was on hemodialysis via a graft AV fistula that had been declotted several times before. Because of the poor condition of his blood vessels, it was difficult to construct a new access or place a central vein catheter. He was declotted several times by the same radiologist, who is very experienced and talented and who has been declotting our dialysis accesses for years. We believe the pulmonary embolism occurred because of angioplasty of the arteriovenous anastomosis of the access, mobilizing a large plaque that embolized to the lungs, causing severe hypoxemia and death. Atherosclerotic plaques are fairly resistant to thrombolysis and are difficult to treat. Back-bleeding technique of the graft and surgical thrombectomy are possible solutions. Unfortunately for our patient, the final event happened so quickly that there was not enough time to rescue him. At postmortem examination, multiple emboli were found in both lungs including cholesterol emboli from previous declottings. In our patient, cholesterol embolization to the lungs, unlike that seen in cholesterol embolization syndrome [16], was not associated with peripheral blood eosinophilia [17]. This raises questions about the pathophysiology of eosinophilia in cholesterol embolization syndrome.
As has been reported, subclinical lung embolization is not uncommon during angioplasty or declotting of dialysis accesses and most patients tolerate it well. Comorbidities in our case may have contributed to the death of our patient. We believe lung embolization with dialysis access declotting is not very common, but it is underreported [18]. Our review of Medline showed very few reports of pulmonary embolism secondary to access declotting. Shah et al. reported the case of a 25-year-old African American man in whom access declotting was complicated by bilateral pulmonary emboli and cardiac arrest, but he survived the event [19]. Toosy et al. and Grebenyuk et al. also reported patients who suffered pulmonary embolism after dialysis access declotting, but in both cases patients survived [20,21].
Conclusions
Access thrombectomy, performed either by vascular surgeons, radiologists, or nephrologists can be complicated by potentially fatal pulmonary embolisms. We believe that in patients with poor vasculature and multiple comorbidities it is better to abandon a clotted access and try to construct a new access or place a central vein catheter. Alternatively, and if feasible, peritoneal dialysis could be a solution.
References:
- 1.Kaw D, Malhotra D. Platelet dysfunction and end stage renal disease. Semin Dial. 2006;19(4):317–22. doi: 10.1111/j.1525-139X.2006.00179.x. [DOI] [PubMed] [Google Scholar]
- 2.Horl WH. Thrombocytopathy and blood complications in uremia. Wien Klin Wochenschr. 2006;18(5–6):134–50. doi: 10.1007/s00508-006-0574-5. [DOI] [PubMed] [Google Scholar]
- 3.Boccardo P, Remuzzi G, Galbusera M. Platelet dysfunction in renal failure. Semin Thromb Hemost. 2004;30(5):579–89. doi: 10.1055/s-2004-835678. [DOI] [PubMed] [Google Scholar]
- 4.Casserly LF, Reddy SM, Dember LM. Venous thromboembolism in end stage renal disease. Am J Kidney Dis. 2000;36(2):405–11. doi: 10.1053/ajkd.2000.8983. [DOI] [PubMed] [Google Scholar]
- 5.Finelli PF, Carley MD. Cerebral venous thrombosis associated with epoetin alfa therapy. Arch Neurol. 2000;57(2):260–62. doi: 10.1001/archneur.57.2.260. [DOI] [PubMed] [Google Scholar]
- 6.Wiesholzer M, Kitzwogerer M, Harm F, et al. Prevalence of preterminal pulmonary thromboembolism among patients on maintenance hemodialysis treatment before and after introduction of recombinant erythropoietin. Am J Kidney Dis. 1999;33(4):702–8. doi: 10.1016/s0272-6386(99)70222-2. [DOI] [PubMed] [Google Scholar]
- 7.Greinacher A, Zinn S, Wizemann, Birk UW. Heparin induced antibodies as a risk factor for thromboembolism and hemorrhage in patients undergoing chronic hemodialysis. Lancet. 1996;348:764. doi: 10.1016/s0140-6736(05)65684-x. [DOI] [PubMed] [Google Scholar]
- 8.Coan KE, O’Donnell ME, Frankhauser GT, et al. Bilateral pulmonary emboli secondary to indwelling hemodialysis reliable outflow catheter. Vasc Endovascular Surg. 2013;47(4):317–19. doi: 10.1177/1538574413484973. [DOI] [PubMed] [Google Scholar]
- 9.Stavroulopoulos A, Aresti V, Zounis C. Right atrial thrombi complicating hemodialysis catheters. A meta-analysis of reported cases and proposal of a management algorithm. Nephrol Dial Transplant. 2012;27(7):2936–44. doi: 10.1093/ndt/gfr739. [DOI] [PubMed] [Google Scholar]
- 10.Ocak G, Van Stralen K, Rosendaal FR, et al. Mortality due to pulmonary embolism, myocardial infarction and stroke among hemodialysis patients. J Thromb Haemost. 2012;10(12):2484–93. doi: 10.1111/j.1538-7836.2012.04921.x. [DOI] [PubMed] [Google Scholar]
- 11.Funski B. Problematic delcots: Complications and irritations. Seminars Intervent Radiol. 2004;21(2):69–75. doi: 10.1055/s-2004-833679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Trerotola SO, Johnson MS, Shah H, et al. Incidence and management of arterial emboli from hemodialysis graft surgical thrombectomy. J Vasc Interv Radiol. 1997;8(4):557–62. doi: 10.1016/s1051-0443(97)70608-0. [DOI] [PubMed] [Google Scholar]
- 13.Peirce RM, Funaki B, Van Ha TG, Lorenz JM. Percutaneous declotting of virgin femoral hemodialysis grafts. Am J Roentgenol. 2005;185:1615–19. doi: 10.2214/AJR.04.0693. [DOI] [PubMed] [Google Scholar]
- 14.Zaleski G. Declotting, maintenance, and avoiding procedural complications of native arteriovenous fistulae. Seminars Intervention Radiol. 2004;21(2):83–93. doi: 10.1055/s-2004-833681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu S, Ahmad I, Qayyum S, et al. Paradoxical embolism after declotting of hemodialysis fistula/grafts in patients with patent foramen ovale. Clin J Am Soc Nephrol. 2011;6(6):1333–36. doi: 10.2215/CJN.09851110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kronzon I, Saric M. Cholestrol embolization syndrome. Circulation. 2010;122:631–41. doi: 10.1161/CIRCULATIONAHA.109.886465. [DOI] [PubMed] [Google Scholar]
- 17.Zumi C, Kondo H, Tamura T, et al. Clinical evaluation of cholestrol embolization syndrome after cardiac catheterization. J Cardiol. 1998;31(4):201–6. [PubMed] [Google Scholar]
- 18.Sabatine MS, Oelberg DA, Kanareck D. Pulmonary cholestrol embolization. Chest. 1997;112(6):1687–92. doi: 10.1378/chest.112.6.1687. [DOI] [PubMed] [Google Scholar]
- 19.Shah A, Ansari N, Hamadeh Z. Cardiac arrest secondary to bilateral pulmonary emboli following arteriovenous fistula thrombectomy: A case report with review of the literature. Case reports in nephrology. 2012 doi: 10.1155/2012/831726. article ID 831726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grebenyuk LA, Marcus RJ, Nahum E, et al. pulmonary embolism following successful thrombectomy of an arteriovenous dialysis fistula. J Vasc Access. 2009;10(1):59–61. doi: 10.1177/112972980901000111. [DOI] [PubMed] [Google Scholar]
- 21.Toosy K, Saito S, Patrascu C, Jean R. Cardiac arrest following massive pulmonary embolism during mechanical declotting of thrombosed hemodialysis fistula: Successful resuscitation with tPA. J Intensive Care Med. 2008;23(2):143–45. doi: 10.1177/0885066607313002. [DOI] [PubMed] [Google Scholar]


