Abstract
Background
Henoch Schönlein Purpura (HSP) is the most common systemic vasculitis of childhood. There is considerable controversy over whether children with HSP should be treated with corticosteroids. The goal of this study was to investigate whether early corticosteroid administration could reduce the rate of renal or gastrointestinal complications in children with HSP.
Methods
Forty children with HSP, seen in the emergency room of a tertiary-care, paediatric centre, entered a randomized, double-blind, placebo controlled study. The treatment group (n = 21) received oral prednisone, 2 mg/kg/day for one week, with weaning over a second week, while the placebo group (n = 19) received an identical appearing placebo. Co-primary outcomes were the rate of renal involvement at one year and the rate of acute gastrointestinal complications. Co-primary outcomes were analysed using Fisher's Exact test.
Results
At one year, there was no difference in the rate of renal involvement (3/21 prednisone group vs. 2/19 placebo group, P = 1.0). There was also no statistically significant difference in the rate of acute gastrointestinal complications (2/21 prednisone group vs. 3/19 placebo group, P = 0.7). Two children in the placebo group did experience intussusceptions compared with none in the prednisone group (P = 0.2).
Conclusions
Early prednisone therapy in HSP does not appear to reduce the risk of renal involvement at one year, or the risk of acute gastrointestinal complications. There may be a reduced risk of intussusception. The routine, early use of prednisone in uncomplicated HSP cannot be recommended at this time.
Background
Henoch Schönlein purpura (HSP) is a systemic, IgA-mediated, small vessel vasculitis which is common in children [1]. It is characterized by palpable purpuric rash, arthralgias or arthritis with periarticular swelling, bowel involvement and renal involvement. There have also been reports on the involvement of other organs, including lungs [2], brain [3], and testes [4].
In the majority of children, HSP is a self-limited illness with no significant sequelae. However, adverse outcomes are possible. Acutely, bowel involvement may be associated with gastrointestinal haemorrhage in 5%, intussusception in 2% or perforation in less than 1% [5]. Chronically, renal involvement may be associated with some degree of renal insufficiency in 5%, and rarely, chronic renal failure in up to 1.5% [6]. Persistent evidence of renal involvement (microscopic haematuria, proteinuria or hypertension) is reported to be present at greater than one year of follow up in 35–53% of children, although this figure is likely to be an overestimate given the data are from referral-based, tertiary-care populations [6-8].
Predicting which children are at risk of complications in HSP has been difficult. Hypertension, proteinuria >1 g/l, and elevations in serum urea and creatinine have been shown to be risk factors for chronic renal disease [6,8-10]. One group has also identified age greater than seven years, persistence of purpuric rash and low Factor XIII activity as risk factors [11]. In a study of unselected children from Northwest Spain with at least one year follow up, haematuria at the onset of the disease or renal manifestations within the first three months after the onset of the symptoms of the disease were significantly more common in the group of HSP patients with renal sequelae [12]. Also in this study, the presence of nephritic syndrome during the course of the disease was generally associated with permanent renal involvement. Unfortunately, some of these may be late findings, and may not be helpful in the acute management of HSP. More importantly, once established, chronic renal disease due to HSP may not be amenable to therapy. Risk factors for gastrointestinal complications have not been evaluated.
It has been proposed that the early use of corticosteroids in children with HSP could prevent chronic renal disease. There have been eight publications addressing this issue [8,11,13-18], including two by the same author with overlapping patients. Unfortunately, these studies are fraught with methodological flaws, and the only prospective study failed to use appropriate randomization or a placebo [14]. Thus, the overall results are contradictory and confusing, and the question of whether early treatment with corticosteroids reduces the risk of subsequent renal involvement in HSP remains unsettled. To date, no prospective studies have investigated the effect of early treatment with corticosteroids on gastrointestinal complications.
This study is a randomized, placebo-controlled project investigating whether early corticosteroid administration could reduce the rate of renal or gastrointestinal complications in children with HSP. For the purposes of this study, we have defined early administration of corticosteroid as within seven days of disease onset.
Methods
Patients
All children seen with a diagnosis of HSP in the emergency room of the Children's Hospital of Eastern Ontario, Ottawa, Canada between September 1, 1996 and January 31, 2000 were eligible for the study. HSP was defined as palpable purpura and at least one of the following: arthritis, renal involvement (defined as haematuria on urine microscopy greater than or equal to 5 red blood cells per high powered field or red cell casts, proteinuria of urinalysis greater than or equal to 0.3 g/l, hypertension greater than the 90th percentile for age and gender [19]); or gastrointestinal involvement (defined as abdominal pain, gross or occult blood in stool, or a surgical complication, such as intussusception or perforation). Eligible participants also had to be between 2 and 15 years of age and within seven days of disease onset. Children were excluded if there was another reason for purpura (e.g. thrombocytopenia); if they had a known underlying systemic vasculitis; if they had been treated with any corticosteroid in the previous month; if they were known to have an underlying renal, gastrointestinal, or immunodeficiency illness; if they currently had an active infection; or if they were experiencing a life threatening complication of HSP.
Objectives
The co-primary objectives of this study were to determine if the early use of prednisone therapy in children with HSP could prevent the development of renal involvement at one year, or the development of gastrointestinal complications in the acute period. The effects of the intervention on duration of symptoms (abdominal pain, joint pain, rash); need for admission; and risk of recurrence were also investigated.
Intervention
This study was approved by the Research Ethics Board at the Children's Hospital of Eastern Ontario, Canada and informed consent was obtained from the parents/guardians of all participants. Before the start of the study, a computer-generated sequence of random numbers were placed in a series of plain, sealed envelopes with patient numbers on them by the research pharmacist. These envelopes were created and kept in the pharmacy, and only opened at the time of subject randomization, again by the research pharmacist. Individuals directly involved in the study had no access to these envelopes. Subjects were randomized in blocks of eight. Subjects had an equal chance of being assigned to the treatment or placebo groups. The intention was to enrol 20 children into both the treatment and placebo groups. Those assigned to the treatment group were given oral prednisone 2 mg/kg for seven days, followed by a weaning dose of prednisone for the next seven days (75% on days 8 and 9, 50% on days 10 and 11, 25% on days 12, 13, and 14, then discontinue). A starting dose of 2 mg/kg was chosen as it was the maximum dose used in previous studies, and thought to be the most likely to be effective. Those assigned to the placebo group received an identical number of pills, and followed the same schedule. In order to maintain blinding, both prednisone and placebo tablets were placed in opaque, tasteless gelatin capsules. The subjects and all individuals involved in the enrolment and assessment of study participants were blinded to the study group.
Subjects were evaluated at baseline, two weeks, one month and one year, with urine collections at two, three and six months. During the first 14 days of the study, a structured diary was completed by the parent/guardian that documented symptoms, compliance with medication and side effects. The completed diary was collected on 39 subjects. At each visit, a structured history and physical examination was performed. All urine specimens had dipstick testing of protein and blood, as well as microscopy. Blood tests for complete blood count, erythrocyte sedimentation rate, urea, creatinine, coagulation parameters, immunoglobulins, complement components 3 and 4, and albumin were done at baseline, and complete blood count, urea and creatinine at the one year follow up.
Outcomes
Renal involvement at one year was defined as haematuria on microscopy greater than 5 red blood cells per high powered field, red cell casts, proteinuria greater than 0.3 g/l, hypertension greater than 90th percentile for age and gender [19], or renal insufficiency indicated by an elevation in serum creatinine. Acute gastrointestinal complications were defined as gastrointestinal bleeding requiring transfusion or fluid resuscitation, intussusception, perforation or need for operative intervention.
Analysis
The study population was described using nonparametric descriptive statistics. Proportions were compared using χ2 or Fisher's Exact test as appropriate. Medians were compared using the Mann-Whitney U-test. Because symptom durations were censored at 14 days, they were compared using the Kaplan-Meier method and Log-Rank test. The ability of continuous variables to predict either renal involvement at one year or gastrointestinal complications was analysed using logistic regression. Analyses were performed using DataDesk 6.1 for Windows (Data Description Inc., 1996, Ithaca NY, USA) and SAS (SAS 8.0 for Windows, 1999, Cary NC, USA).
All subjects who actually began the study were included in the analysis (intention to treat). For those subjects with incomplete data, the last available assessment was used.
Results
Patients
The flow of patients in the study is summarized in Figure 1. One subject was randomized, but then declined to participate further in the study, and was not included in the analysis. Characteristics of both groups are shown in Table 1. There were no statistically significant differences between the groups (data not shown), although the prednisone group did appear to have a somewhat higher proportion of subjects with gastrointestinal involvement at enrolment.
Figure 1.
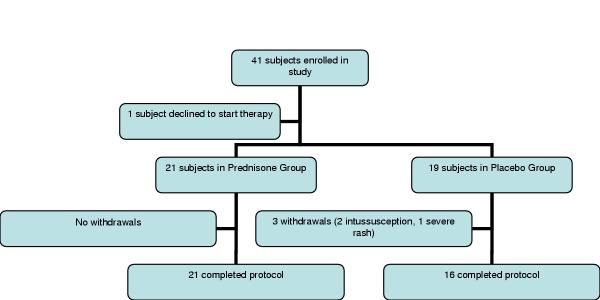
Flow diagram showing the progress of patients through the study
Table 1.
Subject demographics at study enrolment
| Prednisone group (n = 21) | Placebo group (n = 19) | ||
| Age, years – median (range) | 5 (2–11) | 6.1 (3–15) | |
| Gender | Female | 8 | 12 |
| Male | 13 | 7 | |
| Ethnicity | Caucasian | 18 | 18 |
| Other | 3 | 1 | |
| Days since illness onset – median (range) | 4 (1–7) | 3 (1–7) | |
| Symptoms at enrollment- number of subjects (%) | Rash | 21 (100) | 19 (100) |
| Joint | 17 (81) | 18 (95) | |
| Gastrointestinal | 18 (86) | 11 (58) | |
| Renal | 4 (19) | 2 (11) |
Renal involvement
At one year, three children in the prednisone group and two children in the placebo group had evidence of renal involvement, as defined in this study (P = 1.0 by Fisher's Exact test). All of these children had persistent haematuria and/or proteinuria. None had hypertension or renal insufficiency.
A post-hoc power calculation was performed to assess the risk of a Type II error. Assuming that the rate of renal involvement at one year was similar to that seen in the placebo population (2/19 = 10.5%), setting the risk of a Type I error to α = 0.05, this study had a power of 91% to detect a 50% reduction in the rate of renal involvement at one year. An exploratory analysis was also performed to see if differences existed between the two groups at other time points. No differences in renal involvement were seen between the two groups at six months (two in prednisone group, one in placebo group, P = 1.0 by Fisher's Exact test), three months (three in prednisone group, two in placebo group, P = 1.0 by Fisher's Exact test), two months (four in prednisone group, three in placebo group, P = 1.0 by Fisher's Exact test), one month (three in both prednisone and placebo groups, P = 1.0 by Fisher's Exact test) or two weeks (three in prednisone group, one in placebo group, P = 0.6 by Fisher's Exact test). The presence of renal involvement at any time during follow up was not different between the two groups (nine in prednisone group, five in placebo group, P = 0.27 by χ2, df = 1).
Gastrointestinal complications
Acute gastrointestinal complications were seen in two children in the prednisone group (both severe abdominal pain requiring admission but no other intervention), and three children in the placebo group (two intussusceptions, both of which required operative intervention, and one with severe abdominal pain required admission but no other intervention) (P = 0.7 by Fisher's Exact test). When considered separately, the risk of intussusception was not statistically different between the two groups (P = 0.2 by Fisher's Exact test). No children required a blood transfusion or experienced a bowel perforation.
Duration of symptoms
Symptom durations, as recorded in the 14-day diary, are summarised in Table 2. No statistically significant differences were seen between the two groups. There appeared to be a trend for children in the prednisone group to have shorter durations of rash and joint pain. The prednisone group did tend to have a longer duration of abdominal pain, although the two children with intussusception contributed no data to this result.
Table 2.
Summary of symptom durations, based on 14-day diary data (all observations censored at 14 days).
| Prednisone | Placebo | P-value by Log-rank test | |
| Rash duration, days – median (range) (n = 39) | 7 (0–14) | 11 (0–14) | 0.1 |
| Joint pain duration, days – median (range) (n = 38) | 3 (0–12) | 6 (0–14) | 0.1 |
| Abdominal pain duration, days – median (range) (n = 39) | 5.5 (0–14) | 2 (0–14) | 0.8 |
Admission, recurrences and withdrawals
Two children were admitted in the prednisone group (both severe abdominal pain), three in the placebo group (the two with intussusception, the other with severe abdominal pain) (P = 0.7 by Fisher's Exact test). Recurrences (primarily rash) were seen in two children in the prednisone group and four children in the placebo group (P = 0.4 by Fisher's Exact test).
Three children were withdrawn from the study by the investigators, all in the placebo group (both children with intussusception and one child with severe and worsening rash) (P = 0.1 by Fisher's Exact test). Both of the children with intussusception required operative intervention, and were treated with corticosteroids by their attending physicians. The child with the increasing rash was not treated with corticosteroids. All three of these children had uneventful and complete recoveries. No children experienced significant adverse events secondary to prednisone therapy.
Prediction of renal involvement or gastrointestinal complications
Age, time since diagnosis, Factor XIII level, and IgA level were not significant predictors of either renal involvement at one year or gastrointestinal complications, whether using univariate analysis or bivariate analysis to account for treatment group (Table 3).
Table 3.
Potential predictive variables for renal involvement at one year or gastrointestinal complications (using logistic regression)
| Predictor | Renal involvement at one year | Gastrointestinal complication | |||
| β-coefficient | P-value | β-coefficient | P-value | ||
| Univariate (predictor alone) | |||||
| Age | -0.06 | 0.4 | 0 | 1.0 | |
| Time since diagnosis | 0 | 1.0 | -0.02 | 0.6 | |
| Factor XIII level | -0.2 | 0.6 | -0.2 | 0.4 | |
| IgA level | 0.09 | 0.5 | 0.01 | 0.9 | |
| Bivariate (predictor and treatment group) | |||||
| Age | -0.09 | 0.2 | 0.1 | 0.8 | |
| Time since diagnosis | 0.01 | 0.8 | -0.3 | 0.5 | |
| Factor XIII level | -0.3 | 0.4 | -0.1 | 0.6 | |
| IgA level | 0.04 | 0.8 | 0.1 | 0.3 | |
Discussion
This project was a randomized, double-blind, placebo-controlled study investigating the efficacy of early prednisone therapy to prevent complications of HSP. We found no evidence that early prednisone therapy reduced the risk of renal involvement at one year. We also failed to show a statistically significant difference in the risk of gastrointestinal complications, although there did appear to be a trend towards reduced risk in the treatment group. Somewhat surprisingly, we also did not see a statistically significant difference in duration of symptoms, although again there appeared to be a trend towards shorter durations of rash and joint pain in the treatment group. Finally, unlike recent publications [11,15], we were unable to identify any significant predictors of adverse renal or gastrointestinal outcomes.
There remains considerable controversy regarding the use of corticosteroids in uncomplicated HSP. This is understandable, considering the contradictory nature of the literature. However, the lack of consistency between studies is likely to be largely related to the inadequate methods used to date.
Mollica et al have published the only prospective study of the use of corticosteroids to prevent renal injury [14]. Unfortunately, interpretation of these results is hindered by the lack of random group assignment (described as being "alternatively assigned to one of two treatment groups") and the lack of any description of blinding. These deficiencies leave concerns regarding the possibility of bias in this study and, despite the rather strikingly significant results in favour of corticosteroid therapy, prevent it from providing definitive evidence.
The remaining studies concerning renal involvement are retrospective, with corticosteroids given at the discretion of the treating physician for a variety of indications. Some of these studies suggested that corticosteroids were beneficial in preventing renal involvement [11,13], while others showed no benefit [8,15-18]. Unfortunately, interpretation of these studies is hampered by their retrospective design. There is no reasonable expectation that children who were treated were similar to those who were not treated. In particular, it is likely that children with more severe disease would be the most likely to be treated with corticosteroids. This is likely to bias results against showing a benefit for corticosteroid therapy and prevent any of these studies providing useful information about the role of corticosteroids in HSP.
The literature concerning gastrointestinal complications is equally unhelpful. There have been no prospective trials. Three retrospective studies have suggested that corticosteroids are beneficial in the treatment of abdominal pain [17,20,21] and, although this does show consistency, it cannot be considered definitive evidence.
In the current study, bias has been minimized by using a randomized and double-blinded design. Variation in the population has been minimized by ensuring that all participants were early in their illness, with enrolment prior to seven days. Both renal and gastrointestinal complications have been investigated. Thus, this study should provide high quality data concerning the use of corticosteroids in HSP.
This study provides no evidence that corticosteroids reduce the risk of renal involvement at one year. In fact, the treatment group had a slightly higher (not statistically significant) rate of renal involvement compared to the placebo group. Although this was a relatively small study, it had a power of over 90% to show a 50% reduction in renal involvement at one year. Given that our definition of renal involvement is acting as a surrogate marker for the much rarer, and clinically relevant, outcome of chronic renal insufficiency, it was felt that a 50% reduction would be necessary to be considered significant.
Although this study did not show a statistically important difference in the rate of gastrointestinal complications, it is important to note that two children in the placebo group did develop intussusceptions that required operative intervention, a complication that was not seen in the treatment group. It is possible that the study was not large enough to show a statistically significant difference, and that the early use of corticosteroids in HSP may prevent this important complication.
It is interesting that corticosteroid therapy did not seem to reduce symptom duration. There is a trend towards shorter durations of rash and joint pain in the treatment group. A similar trend is not seen for abdominal pain. Unfortunately, both children with intussusceptions were withdrawn early from the study, and so contributed no data about abdominal pain. It is possible that the loss of this data may have compromised this part of the analysis.
Despite the methodological strengths of this study, there are some limitations. The most important is the sample size. However, we have shown that the study does have reasonable power to demonstrate the size of benefit we considered to be clinically relevant. The study might also be criticized for the use of a surrogate outcome for the development of chronic renal insufficiency. This is a rare complication which may develop many years after the acute illness, making a study with it as a primary outcome impossible to perform. Finally, this study involved children seen in the emergency room of a tertiary care paediatric centre. It is possible that this may have skewed the population towards more severe involvement.
Conclusions
In conclusion, this study did not show a difference in the development of renal injury between children treated with corticosteroids or placebo. These results do not support the use of corticosteroids in early HSP to prevent renal injury. It is possible that corticosteroids prevent some acute gastrointestinal complications. Given the small size of this study, these results await confirmation.
Competing interests
None declared.
Authors' contributions
All authors participated in the initial design of the trial. AH collected the data (with the assistance of the research assistants), performed the analysis and drafted the initial manuscript. MP supervised the conduct of the trial, and facilitated data collection. All authors contributed to revisions of the manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
Our most sincere thanks to Terry Sutcliffe and Marni Baird who devoted so much time and effort to this project, and to Dr. Nina Birdi who was instrumental in the concept and design of this project and has been a mentor to Dr. Huber.
Contributor Information
Adam M Huber, Email: adamtheresa@hfx.eastlink.ca.
Jim King, Email: King@exchange.cheo.on.ca.
Peter McLaine, Email: McLaine@cheo.on.ca.
Terry Klassen, Email: terry.klassen@ualberta.ca.
Mary Pothos, Email: pothos@cheo.on.ca.
References
- Saulsbury Frank T. Henoch-Schonlein purpura. Curr Opinion Rheumatol. 2001;13:35–40. doi: 10.1097/00002281-200101000-00006. [DOI] [PubMed] [Google Scholar]
- Chaussain Michelle, de Boissieu Delphine, Kalifa Gabriel, Epelbaum Serge, Niaudet Patrick, Badoual Jean, Gendrel Dominique. Impairment of lung diffusing capacity in Schonlein-Henoch Purpura. J Pediatr. 1992;121:12–16. doi: 10.1016/s0022-3476(05)82533-8. [DOI] [PubMed] [Google Scholar]
- Chen Chein-Liang, Chiou Yee-Hsuan, Wu Chan-Yao, Lai Ping-Hong, Chung Hsiao-Min. Cerebral vasculitis in Henoch-Schonlein purpura:a case report with sequential magnetic resonance imaging changes and treated with plasmapheresis alone. Pediatr Nephrol. 2000;15:276–278. doi: 10.1007/s004670000477. [DOI] [PubMed] [Google Scholar]
- Ben-Sira Liat, Laor Tal. Severe scrotal pain in boys with Henoch Schonlein purpura:incidence and sonography. Pediatr Radiol. 2000;30:125–128. doi: 10.1007/s002470050029. [DOI] [PubMed] [Google Scholar]
- Szer IS. Henoch-Schonlein purpura. Curr Opin Rheumatol. 1994;6:25–31. doi: 10.1097/00002281-199401000-00005. [DOI] [PubMed] [Google Scholar]
- Koskimies O, Mir S, Rapola J, Vilska J. Henoch Schonlein nephritis:long-term prognosis of unselected patients. Arch Dis Child. 1981;56:482–484. doi: 10.1136/adc.56.6.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein AR, White HRW, Akuse R, Chantler C. Long-term follow-up of childhood Henoch-Schonlein nephritis. Lancet. 1992;339:280–282. doi: 10.1016/0140-6736(92)91341-5. [DOI] [PubMed] [Google Scholar]
- Counahan R, Winterborn MH, White RHR, Heaton JM, Meadow SR, Bluett NH, Swetschin H, Cameron JS, Chantler C. Prognosis of Henoch-Schonlein nephritis in children. BMJ. 1977;2:11–14. doi: 10.1136/bmj.2.6078.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coppo R, Mazzucco G, Cagnoli L, Lupo A, Schena FP. Long-term prognosis of Henoch-Schonlein nephritis in adults and children. Nephrol Dial Transplant. 1997;12:2277–2283. doi: 10.1093/ndt/12.11.2277. [DOI] [PubMed] [Google Scholar]
- Niaudet P, Murcia I, Beaufils H, Broyer M, Habib R. Primary IgA nephropathies in children: prognosis and treatment. Adv Nephrol Necker Hosp. 1993;22:121–140. [PubMed] [Google Scholar]
- Kaku Yoshitsugu, Nohara Kaoru, Honda Sunao. Renal involvement in Henoch-Schonlein purpura: A multivariate analysis of prognostic factors. Kidney Int. 1998;53:1755–1759. doi: 10.1046/j.1523-1755.1998.00915.x. [DOI] [PubMed] [Google Scholar]
- Calvino MC, Llorca J, Garcia-Porrua C, Fernandez-Iglesias JL, Rodriguez-Ledo P, Gonzalez-Gay MA. Henoch-Schonlein purpura in children from northwestern Spain: a 20-year epidemiologic and clinical study. Medicine (Baltimore) 2001;80:279–290. doi: 10.1097/00005792-200109000-00001. [DOI] [PubMed] [Google Scholar]
- Buchanec J, Galanda V, Belakova S, Minarik M, Zibolen M. Incidence of renal complications in Schonlein-Henoch purpura syndrome in dependence of an early administration of steroids. Int Urol Nephrol. 1988;20:409–412. doi: 10.1007/BF02549574. [DOI] [PubMed] [Google Scholar]
- Mollica F, Li Volti S, Garozzo R, Russo G. Effectiveness of early prednisone therapy in preventing the development of nephropathy in anaphylactoid purpura. Eur J Pediatr. 1992;151:140–144. doi: 10.1007/BF01958961. [DOI] [PubMed] [Google Scholar]
- Sano Hitomi, Izumida Michiko, Shimizu Hiroshi, Ogawa Yunisuke. Risk factors for renal involvement and significant proteinuria in Henoch-Schonlein purpura. Eur J Pediatr. 2002;161:196–201. doi: 10.1007/s00431-002-0922-z. [DOI] [PubMed] [Google Scholar]
- Saulsbury FT. Corticosteroid therapy does not prevent nephritis in Henoch-Schonlein purpura. Pediatr Nephrol. 1993;7:69–71. doi: 10.1007/BF00861574. [DOI] [PubMed] [Google Scholar]
- Saulsbury FT. Henoch-Schonlein purpura in Children. Report of 100 patients and review of the literature. Medicine. 1999;78:395–409. doi: 10.1097/00005792-199911000-00005. [DOI] [PubMed] [Google Scholar]
- Temmel AFP, Emminger W, Schroth B, Zaunschirm HA, Gadner H. Early prednisone therapy and nephropathy in anaphylactoid purpura. Eur J Pediatr. 1993;152:782–783. doi: 10.1007/BF01954006. [DOI] [PubMed] [Google Scholar]
- Task Force on Blood Pressure Control in Children. National Heart, Lung and Blood Institute, Bethesda, Maryland. Report of the Second Task Force of Blood Pressure Control in Children. Pediatrics. 1987;79:1–25. [PubMed] [Google Scholar]
- Rosenblum Norman D., Winter Harland S. Steroid effects on the course of abdominal pain in children with Henoch-Schonlein purpura. Pediatrics. 1987;79:1018–1021. [PubMed] [Google Scholar]
- Glasier CM, Siegel MJ, McAlister WH, Shackelford GD. Henoch-Schonlein syndrome in children: gastrointestinal manifestations. AJR Am J Roentgenol. 1981;136:1081–1085. doi: 10.2214/ajr.136.6.1081. [DOI] [PubMed] [Google Scholar]


