Abstract
In keeping with international trends, lung cancer incidence and mortality are increasing among the Irish population with many patients presenting with advanced disease that excludes the potential for curative management. Consequently palliative treatment options for this patient group are being increasingly explored with various degrees of success. Endobronchial stenosis represents a particularly challenging area of management among these patients and a number of techniques have been described without the identification of a single gold standard. We report our experience of the first time use of endobronchial cryotherapy in Ireland with reference to a case series, including an example of its use in the management of benign disease, in order to support patients with borderline lung function and enable definitive palliative treatment.
Keywords: Bronchial stenosis, cryotherapy, lung cancer, lung transplant, palliative management
In keeping with international trends, lung cancer has now become the main cause of cancer-related mortality among both males and females in Ireland, with more than 1, 700 deaths in 2010.[1] The 5-year relative survival rate for lung cancer in Ireland is <10%, with approximately 40% of patients diagnosed with lung cancer receiving no cancer-directed treatment. This high mortality rate is partly due to the late diagnosis of lung cancer cases with symptoms at presentation related to advanced disease including endobronchial obstruction and distant metastasis.[2,3] Consequently palliative treatment options for this patient group are being increasingly explored with endoscopic intervention considered if there is a perceived benefit, i.e., life expectancy >6 weeks, adequate performance status, patient independent of airway limitations and appropriate anatomy (obstructed large airways supplying perfused lung segments). While various treatment modalities exist for patients with early stage disease including curative surgery, the focus of this case series is on patients with inoperable malignancy or end-stage benign disease who would benefit from endobronchial palliation.
A number of potential treatment options exist for the management of patients with obstructive endobronchial disease, including thermal laser treatment, argon plasma coagulation, brachytherapy, photodynamic therapy, stenting and endobronchial cryotherapy.[3,4] However while the traditional use of thermal laser treatment yielded immediate airway expansion, it was associated with complications including bronchial perforation and a periprocedural mortality rate of 2-3%.[3,5] Argon plasma coagulation, a non-contact form of electrocautery, demonstrated an improvement in endobronchial obstruction in up to 66% of patients with a complication rate of 2% (airway perforations, gas embolism); however, this evidence was based on retrospective case series only.[3] Endobronchial brachytherapy provided reasonable symptomatic relief as a palliative strategy with tumor regression generally observed; however, massive hemoptysis has been reported in up to 7% of cases.[3] Photodynamic therapy was successful in approximately 80% of cases, particularly in tumors <1 cm, with the main complication of hemoptysis; however, this evidence only provided for grade D recommendations in endobronchial disease.[3] The evidence surrounding electrocautery use was also based on case series with positive treatment outcomes reported in 69-94% of patients. The main complication was hemorrhage (<2%), however, this level of evidence also only provided grade D recommendations for its use in endobronchial disease.[3] The risks associated with these various treatment modalities have precluded the identification of a single gold standard in the management of endobronchial obstruction, with few thoracic surgical specialist centers having experience with endobronchial cryotherapy.[3,5]
Cryotherapy utilizes rapid freezing of cells to temperatures below −70°C with liquid nitrogen to cause localized tissue necrosis via a freeze-thaw action.[3,5] This results in a delayed observation of clinical effect; if the patient is unable to expectorate debris, there may be a need for a repeat bronchoscopy to extract necrotic tissue.[4,5] However, there is limited evidence behind the use of cryotherapy with most reviews quoting level-3 evidence at best.[3] Consequently we report our experience of the first time use of endobronchial cryotherapy in Ireland among these patient groups to support those with borderline lung function and enable definitive palliative treatment.
Case Report
The first case was a 61-year-old gentleman who previously underwent a left pneumonectomy for squamous cell carcinoma (T2 N1 M0). Approximately 9-months after his initial surgery he developed a right lower lobe recurrence causing obstruction of the right lower lobe bronchus. There was concern at multi-disciplinary review that radiotherapy would compromise the airway lumen due to endobronchial edema with resultant right lower lobe collapse, a potentially fatal complication for a patient with one lung. However, due to the introduction of a cryotherapy service, endobronchial cryotherapy prior to palliative radiotherapy could now be offered.
He underwent a flexible bronchoscopy, which demonstrated an elliptical tumor in the right bronchus intermedius causing narrowing of the lower bronchus to 20% of normal [Figure 1a]. Cryotherapy was performed to the tumor to good effect. Repeat flexible bronchoscopy 2 days later demonstrated an improvement in the endobronchial stenosis and the surrounding mucopurulent necrotic tissue was removed [Figure 1b]. He made a good post-operative recovery and was discharged to home suitable for out-patient palliative radiotherapy.
Figure 1a.
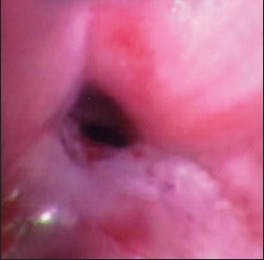
Flexible bronchoscopy, which demonstrated an elliptical tumor in the right bronchus intermedius causing narrowing of the lower bronchus to 20% of normal
Figure 1b.
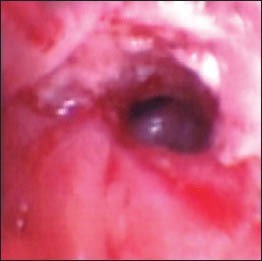
Repeat flexible bronchoscopy 2 days later, which demonstrated an improvement in the endobronchial stenosis
The second case was a 67-year-old female with stage 4 non-small cell lung carcinoma who was managed with palliative chemotherapy. Four weeks after completing her last cycle of chemotherapy, she presented with right-sided lobar collapse and an associated pleural effusion [Figure 2a]. A re-staging computed tomography scan of thorax demonstrated an occluded right upper lobe bronchus with marked narrowing of the right bronchus intermedius [Figure 2b]. She was referred to the thoracic service for potential palliative surgical options.
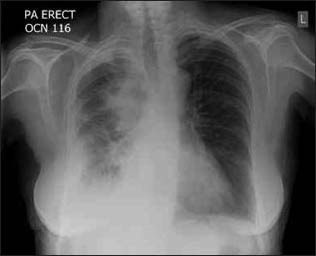
Figure 2a.

A chest radiograph demonstrating right-sided collapse with a pleural effusion
Figure 2b.
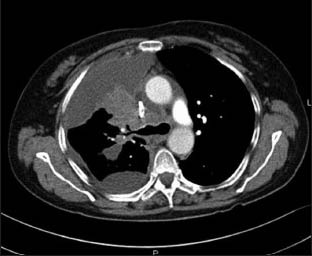
Computed tomography of thorax demonstrating marked narrowing of the right bronchus intermedius
At flexible bronchoscopy, compression of both the anterior and apical posterior segments of the right upper lobe was evident. Cryotherapy application to the right upper lobe tumor was performed to reduce a presumed V-Q (ventilation/perfusion) mismatch and single-port right video-assisted thorascopic surgery facilitated pleural aspiration and pleurodesis. She made a good post-operative recovery and on discharge she had minimal dyspnea and was mobilizing independently. The procedure allowed for the patient to be discharged without the need for home oxygen, as her oxygen saturations at rest were 97% on room air, which compared favorably to her admission saturations of 97% on 3 l of oxygen. Her chest radiograph on the day of discharge, post-operative day-15, was much improved [Figure 2c].
Figure 2c.
The chest radiograph on the day of discharge demonstrating a significant improvement
The third case was a 61-year-old male who had undergone a double-lung transplant 1-year earlier for alpha-1 antitrypsin deficiency emphysema with associated pulmonary hypertension. Due to recurrent symptoms of wheeze and with a flexible bronchoscopy demonstrating stenosis at the anastomotic site of the right bronchus intermedius, he underwent cryotherapy and associated endobronchial stent insertion [Figure 3a and b]. He made an excellent post-operative recovery and was discharged symptom-free.
Figure 3a.

Flexible bronchoscopy, which demonstrated stenosis of the right bronchus intermedius
Figure 3b.

Repeat flexible bronchoscopy 3 days later, which demonstrated a well-positioned stent and a patent bronchus following cryotherapy
Discussion
The increasing incidence of advanced lung cancer rates necessitates the availability of additional treatment options to assist in palliation. As described in this case series, cryotherapy provides a non-operative mechanism of improving airway patency and may be used in combination with other treatment modalities to provide optimal end-of-life care to patients who otherwise may not have been offered any intervention.[3,5] Although cryotherapy is advocated in the current British Thoracic Society and American Thoracic Society guidelines, it is not widely used, which may relate to the limited level three evidence base currently available or the lack of skilled surgical expertise.[3,4] However, symptomatic improvement has been reported with complete or partial restoration of airway patency in over 90% of patients using cryotherapy, a significant goal of therapy in the palliative management of these patients.[3,4,5,6,7] In addition, there is some emerging evidence that cryotherapy may have immunomodulatory effects through induction of an anti-tumor immune response, an additional therapeutic benefit of this treatment modality.[8]
In our case series, we reported the successful use of cryotherapy with flexible bronchoscopy to improve airway patency, ameliorate symptoms and facilitate ongoing palliative management. However, as these were high-risk surgical patients, we would advocate that endobronchial cryotherapy should be performed under general anesthesia with full anesthetic support. We believe that cryotherapy merits consideration as a palliative treatment option among patients with inoperable lung cancer affecting their airway and that this approach can improve quality-of-life through an amelioration of symptoms and more out-of-hospital days while also improving overall survival. There were no post-procedural complications experienced by this patient group indicating the safety profile of the procedure.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.National Cancer Registry 2011. Cancer in Ireland 2011: Annual report of the National Cancer Registry. [Last accessed 2013 Jan 28]. Available from: http://www.ncri.ie/pubs/pubfiles/AnnualReport2011.pdf .
- 2.Herth FJ, Eberhardt R, Vilmann P, Krasnik M, Ernst A. Real-time endobronchial ultrasound guided transbronchial needle aspiration for sampling mediastinal lymph nodes. Thorax. 2006;61:795–8. doi: 10.1136/thx.2005.047829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Du Rand IA, Barber PV, Goldring J, Lewis RA, Mandal S, Munavvar M, et al. British Thoracic Society guideline for advanced diagnostic and therapeutic flexible bronchoscopy in adults. Thorax. 2011;66(Suppl 3):iii1–21. doi: 10.1136/thoraxjnl-2011-200713. [DOI] [PubMed] [Google Scholar]
- 4.Bolliger CT, Mathur PN, Beamis JF, Becker HD, Cavaliere S, Colt H, et al. ERS/ATS statement on interventional pulmonology. European Respiratory Society/American Thoracic Society. Eur Respir J. 2002;19:356–73. doi: 10.1183/09031936.02.00204602. [DOI] [PubMed] [Google Scholar]
- 5.Lee SH, Choi WJ, Sung SW, Kim YK, Kim CH, Zo JI, et al. Endoscopic cryotherapy of lung and bronchial tumors: A systematic review. Korean J Intern Med. 2011;26:137–44. doi: 10.3904/kjim.2011.26.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maiwand MO, Evans JM, Beeson JE. The application of cryosurgery in the treatment of lung cancer. Cryobiology. 2004;48:55–61. doi: 10.1016/j.cryobiol.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Schumann C, Lepper PM, Barth TF, Möller P, Krüger S. Successful immediate cryorecanalization of a simultaneous high-grade tracheal and bronchial stenosis as rare manifestations of bronchial-associated lymphoid tissue lymphoma. J Thorac Cardiovasc Surg. 2009;137:e17–9. doi: 10.1016/j.jtcvs.2008.02.043. [DOI] [PubMed] [Google Scholar]
- 8.Haen SP, Pereira PL, Salih HR, Rammensee HG, Gouttefangeas C. More than just tumor destruction: Immunomodulation by thermal ablation of cancer. Clin Dev Immunol 2011. 2011 doi: 10.1155/2011/160250. 160250. [DOI] [PMC free article] [PubMed] [Google Scholar]


