Abstract
OBJECTIVE:
This prospective study was conducted to evaluate the value of sonographic B-lines (previously called “comet tail artifacts”), which are long, vertical, well-defined, hyperechoic, dynamic lines originating from the pleural line in assessment of interstitial lung diseases (ILD) and compare them with the findings of chest high-resolution computed tomography (HRCT) and pulmonary function tests (PFTs).
MATERIALS AND METHODS:
Sixty-one patients with ILD underwent transthoracic lung ultrasound for assessment of the presence of B-lines and the distance between them. These findings were compared with that of chest HRCT (ground glass, reticular, nodular or honey combing) and PFT as forced vital capacity (FVC), total lung capacity (TLC), diffusion capacity for carbon monoxide (DLCO) and partial arterial oxygen pressure (PaO2).
RESULTS:
All patients had diffuse bilateral B-lines. The distance between each of the two adjacent B lines correlated with the severity of the disease on chest HRCT where B3 (the distance was 3 mm) correlated with ground glass opacity and B7 (the distance was 7 mm) correlated with extensive fibrosis and honey combing. Also, the distance between B-lines inversely correlated with FVC (r = −0.848, P < 0.001), TLC (r = −0.664, P < 0.001), DLCO (r = −0.817, P < 0.001) and PaO2 (r = −0.902, P < 0.001).
CONCLUSION:
B-lines that are lung Ultrasound signs seem to be useful in the assessment of ILD.
Keywords: B-lines, transthoracic ultrasound, interstitial lung disease
Introduction
Interstitial lung diseases (ILDs) represent a heterogeneous group of lung disorders that may be acute or chronic and characterized by diffuse involvement of the interstitium and impairment of the gas exchange capacity through the alveolocapillary membrane, which may lead to respiratory failure. ILDs have different etiologies, clinical presentations, radiological patterns and histological appearance. High-resolution computed tomography (HRCT) is considered the concurrent gold standard for the diagnosis of ILD as it a sensitive method to assess the extent and the pattern of pulmonary fibrosis.[1,2] Reticular pattern involving the subpleural regions, ground glass opacities, nodular and micronodular pattern and honeycombing are the common HRCT signs of pulmonary fibrosis.[3]
Recently, it has been highlighted that lung sonography is highly sensitive to variations of the pulmonary content and balance between air and fluids. In normal lung, ultrasound (US) waves are completely reflected by air; however, in lung diseases that impair alveolar air content and increase interstitial and alveolar fluids, particular artifacts will be created.[4,5] Diffuse parenchymal lung diseases as pulmonary fibrosis, characterized by the presence of multiple diffuse bilateral B-lines that appear as discrete laser-like vertical hyperechoic reverberation artifacts that arise from the pleural line, extend to the bottom of the screen without fading and move synchronously with lung sliding.[6]
The role of transthoracic lung ultrasound, a non-invasive technique in the assessment of a variety of pulmonary conditions, has been reported in several studies.[7,8,9] Only recently has it been considered a valid method for the assessment of interstitial pulmonary fibrosis in patients with connective tissue diseases[10,11] compared with HRCT as the concurrent gold standard. The ultrasound assessment of ILD is determined by the presence and quantification of B-lines, which consist of tails generated by the reflection of the ultrasound beam from thickened sub-pleural interlobar septa at the lung surface interface[7,10]
Some studies found a positive correlation between the number of lung comet and the extent and degree of pulmonary fibrosis in HRCT.[10] The objective of this study was to evaluate the value of B-lines, which are bedside transthoracic chest ultrasound signs, in the assessment of ILD and compare them with the severity of changes in HRCT chest and pulmonary function impairment.
Patients and Methods
Sixty-one patients with ILD (38 men and 23 women with mean age 49.41 ± 11.69 years) were included in this analytic cross-sectional study. Thirty cases had idiopathic pulmonary fibrosis, eight cases had collagen vascular diseases, four cases had sarcoidosis, nine cases had hypersensitivity pneumonitis and 10 cases had other diagnosis (lymphangitis carcinomatosis, silicosis, radiation pneumonitis and viral pneumonias). The diagnosis of these cases was based on clinical presentation, serological tests, pulmonary function tests (PFTs) and HRCT findings. Informed consent was obtained from each patient and the Faculty of Medicine Ethics Committee approved this study.
Study design
Chest HRCT for all patients was carried out at the Radiology Department while PFT and Transthoracic lung ultrasound examinations were carried out at the Department of Chest Diseases in a tertiary hospital.
Chest HRCT assessment
HRCT examination was performed by standard protocol using Aquilion 64, Toshiba, Otawara, Japan helical scanner. Scans were obtained at full inspiration from the apex to the lung base with the patients in the supine position. The acquisition parameters were as follows: Sequential mode, 1-mm collimation and 10-mm interval, 180-260 mA average tube current (depending on body built) and 120-140 kV tube voltage. HRCT assessment does not include the use of contrast media agents.
Pulmonary involvement was evaluated by topographically dividing the lung into segments using the score proposed by Warrick et al. This index includes a “severity score,” ranging from 0 (normal) to 15 (all lesions present), and an “extension score,” ranging from 0 (normal) to 15 (more than nine pulmonary segments involved). A total Warrick score was obtained by summing the severity and the extension scores.[12]
PFTs
Standard spirometry and polythesmography were performed in all patients by means of a fully equipped computerized system (Cosmed SrL, Quark PFTs ergo, P/N Co9035 -12-99, Italy, and D 97723; Zan 300, Oberthulba, Germany, respectively) for measurement of forced expiratory volume (FEV1), forced vital capacity (FVC), FEV1/FVC and total lung capacity (TLC).
Single-breath diffusing capacity for carbon monoxide (DLCO) was also measured using a single breath method (D 97723; Zan 300, Oberthulba, Germany, CO/CH4 analyzer). Actual DLCO values were corrected for hemoglobin and CO levels. The results were expressed as a percentage of the predicted values.[13,14] PaO2 was measured on room air by puncture of radial artery and analyzing the blood sample using blood gases analyzers (Rapid lab 850; CHIRON/Diagnostics Halstead, UK).
Transthoracic Ultrasonography
All the patients underwent transthoracic examination using an ultrasound scanner (Aloka Echo Camera SSD-3500; Aloka Prosound, Yokohama, Japan) equipped with a 3.5-MHz convex probe. The scanning was performed by a pulmonologist trained in chest sonography using the intercostal spaces as acoustic windows with the patient in a sitting or supine position rising his arms above his head to widen the intercostal space and facilitate scanning. In the evaluation of interstitial syndrome, the sonographic technique ideally consists of scanning eight regions. Four chest areas per side considered for complete lung ultrasound examination. Areas 1 and 2 denote the upper anterior and lower anterior chest areas, respectively. Areas 3 and 4 denote the upper lateral and basal lateral chest areas, respectively.[6]
Transthoracic lung ultrasound interpretation
The presence of B lines, which were previously called comet-tail artifacts, generated from the thickened interlobular septa at the lung wall interface was assessed. These were defined as well-defined, vertical, hyperechoic, dynamic lines originating from the pleural line and spreading like a laser ray up to the edge of the screen. These artifacts are best visible under real-time examination, because some of them appear less pronounced on frozen sonograms. A positive region is defined by the presence of three or more B-lines in a longitudinal plane between two ribs and a positive exam is defined by the presence of two or more positive regions bilaterally.[6] The distance between each two adjacent B-lines was measured and expressed in milliliters.
Statistical analysis
Statistical Package for Social Sciences (SPSS-version 20) software was used for analysis of the results. Results in this study are expressed as mean ± standard deviation or number and percentage. The correlation between different parameters was performed using the Pearson test. The difference was considered significant when P < 0.05. Graphics were performed using Microsoft excel.
Results
This study was carried out on 61 patients with ILD, 38 men and 23 women with a mean age of 49.41 ± 11.69 years [Table 1]. Using chest HRCT, ground glass pattern was observed in 14 patients (23%), reticular pattern in 20 patients (32.8%), reticulonodular pattern in 12 patients (19.7%), nodular pattern in two patients (3.3%) and honey combing pattern in 13 patients (21.2%). By transthoracic chest ultrasonography, all patients had diffuse bilateral B-lines on both sides of the lung. There were more than six B-lines per scan. The distance between each of the two adjacent B lines correlated with the severity of the disease on chest HRCT, where in areas of ground glass abnormality, the B-lines seemed to be more numerous and the distances between them were more narrow (3 mm), making the surface of the lung more hyperechoic, giving the description of white lung. However, in patients with reticular and honeycomb abnormalities, the distances between B-lines were wide (7 mm) (P < 0.001) [Figures 1 and 2a-d]. In comparison with the results of PFTs, the distances between each of the two adjacent B-lines inversely correlated with FVC (r = −0.848, P < 0.001), TLC (r = −0.664, P < 0.001), DLCO (r = −0.817, P < 0.001) and PaO2 (r = −0.902, P < 0.001), as shown in Table 2 and Figure 3.
Table 1.
Demographic data of the study group
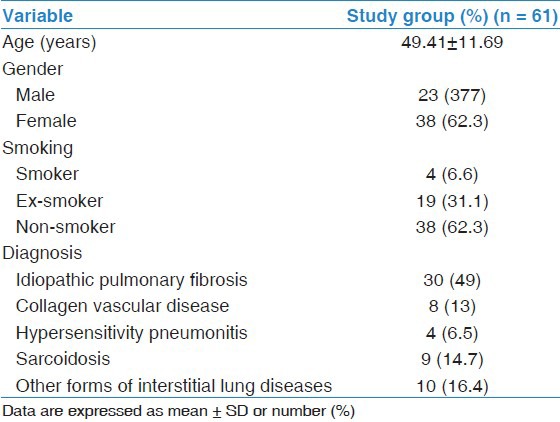
Figure 1.
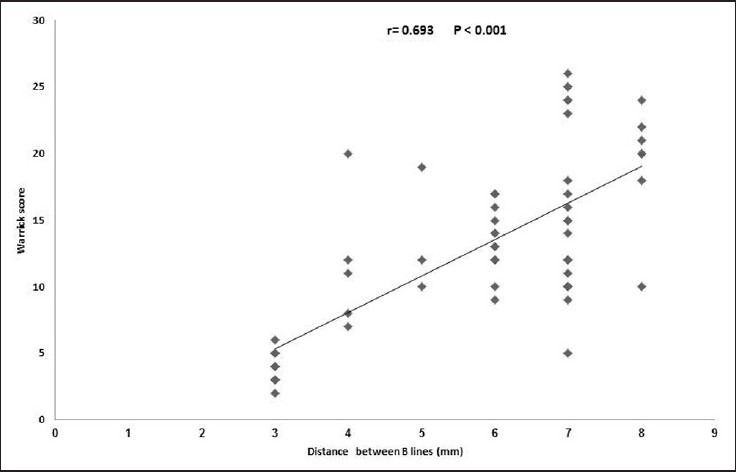
Correlation of distance between B-lines and high-resolution computed tomography findings according to the Warrick score
Figure 2.
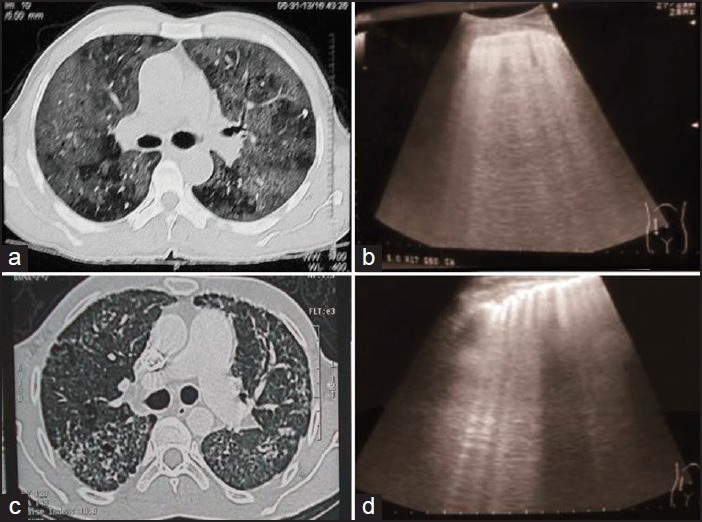
Chest ultrasonography and computed tomography findings. (a) High-resolution computed tomography (HRCT) chest showed ground glass opacity, (b) Ultrasound of the same patient showed diffuse B-lines with a narrow distance between them (about 3 mm), (c) HRCT of the chest showed subpleural reticulation with honey combing and (d) Ultrasound of the same patient showed diffuse B-lines with a wide distance between them (about 7 mm)
Table 2.
Correlations of the distance between B-lines and pulmonary function testing
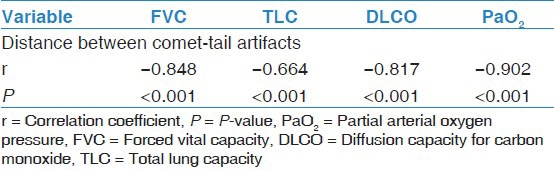
Figure 3.
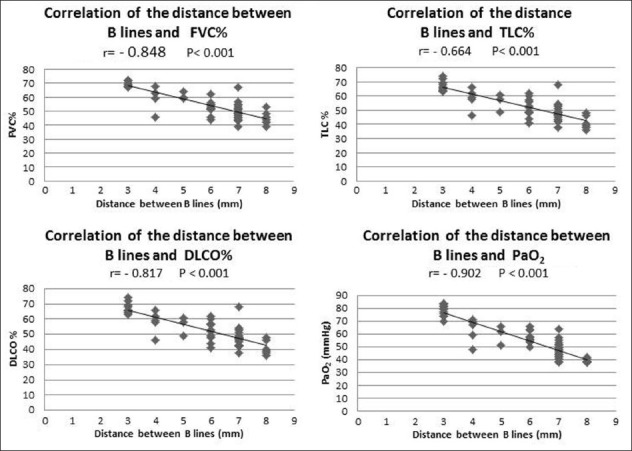
Correlation of the distance between B-lines with pulmonary function testing r = Correlation coefficient, P = P-value, PaO2 = Partial arterial oxygen pressure, FVC = Forced vital capacity, DLCO = Diffusion capacity for carbon monoxide, TLC = Total lung capacity
Discussion
In ultrasonographic examination, the presence of a marked difference in acoustic impedance between an object and its surroundings leads to the appearance of B-line artifacts.[15] Normal lung contains much air and little water, so no reflection of the ultrasonographic beams occurs and normally no B-line artifacts appear. When subpleural septae are thickened by water or fibrosis, a high impedance gradient occurs between these structures and the surrounding air causing reflection of the beams, which create a phenomenon of resonance. The beam seems to be trapped in a closed system, resulting in endless to-and-fro echoing and yielded on the screen as a narrow-based laser-like ray extending from the lung surface to the edge of the screen.[16]
Although chest ultrasound is used to assess different lung conditions, its potential role in the assessment of IPF has been recently proposed in patients with systemic sclerosis.[10,11] In this work, we studied the lungs of patients with ILD with transthoracic ultrasonography and compared the artifacts reflected at the lung surface interface with HRCT as a concurrent “gold standard” for assessment of those patients. In addition, the results of ultrasound examination were compared with respiratory function tests, which measure the degree of pulmonary impairment as a result of fibrosis.
In patients with ILD, the sub-pleural interlobular septa are thickened by deposition of collagen and fibrous tissues. By investigating the lung surface by transthoracic ultrasound, the great impedance gradient between the thickened septa and air in the lung causes reflection of ultrasound beams, creating diffuse B-lines all over the lung surface. However, the correlation of these B-lines with HRCT in those patients was investigated in few studies.[17] In the current study, we found that all patients had diffuse B-lines on both sides of the lung. The distance between each two adjacent B-lines correlated with the degree of interstitial affection on chest HRCT (Warrick score). Well-established fibrosis gives rise to a reticular pattern or honeycombing in HRCT. In ultrasound examination of these patients, the B-lines appear clearly visible and widely separated from each other (7 mm), giving the description of lung rockets. Early stages of ILD even before thickening of the sub-pleural interlobular septa give ground glass areas in HRCT. Ultrasound examination of these areas gives numerous B-lines with a narrow distance between them (3 mm), making the surface of the lung more hyperechoic, giving the description of white lung. This may be due to affection of the alveolar wall by inflammatory cells and edema, making it abut the pleural surface between two septa giving numerous artifacts with a narrow distance between them. These results were compatible with some studies that reported that the average distance between B-lines due to thickened interlobular septa by well-established fibrosis (7 mm) was wider than that due early stage of alveolar–interstitial affection and ground glass attenuation (3 mm).[18] Therefore, ultrasound will be able to detect early stages of pulmonary changes and subclinical lung involvement. Bouhemad et al. found that multiple B-lines 7 mm apart are caused by thickened interlobular septa, characterizing interstitial edema, while B-lines 3 mm or less apart are caused by ground glass areas characterizing alveolar edema.[19]
PFTs are well documented in assessing the disease severity and following-up its progression and response to therapy. In this study, the comparison between transthoracic lung ultrasound and PFTs in patients with ILD revealed that the distance between B-lines inversely correlated with FVC, TLC, DLCO and PaO2 as narrow distances between B-lines represent early alveolar wall affection and little pulmonary function impairment while wide distances between B-lines indicate thickened septa and great impairment in lung function.
Transthoracic lung Ultrasound has many advantages over HRCT and PFT; it is a bedside procedure widely available, easily performed, inexpensive, requires neither ionizing radiation nor a contrast medium and is therefore readily and largely accepted by the patient. In addition, the surface of the lung can be easily studied by US; therefore, the B-lines are quickly detected using either low-frequency (3.5 MHZ) or high-frequency (7.5 MHZ) transducers.[20] In critically ill patients, portable machines even without Doppler power can be sufficient for a complete and detailed lung assessment. Finally, ultrasound is useful in situations where HRCT is not available or undesirable, as in pre-hospital emergencies and in pregnancy and when a patient cannot be transported out of the intensive care unit because of severe disease.[21]
Limitations of the study
The study has some limitations. First, ultrasound had been performed on patients already diagnosed as ILD based on chest HRCT, and this may be considered a bias for the interpretation of the lung ultrasound patterns. However, in this study, we do not evaluate the diagnostic accuracy of lung ultrasound in patients with ILD but study the usefulness of B-lines in evaluation of those patients and if they can play a complementary role in the diagnosis and monitoring of ILD patients, especially when HRCT cannot be done and avoiding unnecessary overload of radiation exposure is needed. Second, pulmonary fibrosis may be not uniformly distributed. This limitation may be ignored as most of the studied patients had diffuse disease and the method used to examine the chest included the upper and lower anterior and lateral parts of the chest so that most of the affected parts were assessed.
Conclusion
B-lines, which are lung ultrasound signs, seem to be useful in the assessment of ILD.
Acknowledgments
The authors thank all the nursing staff in the Chest Ultrasonoghraphy Unit, in their department for their help during the study period.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Launay D, Remy-Jardin M, Michon-Pasturel U, Mastora I, Hachulla E, Lambert M, et al. High resolution computed tomography in fibrosing alveolitis associated with systemic sclerosis. J Rheumatol. 2006;33:1789–801. [PubMed] [Google Scholar]
- 2.Desai SR, Veeraraghavan S, Hansell DM, Nikolakopolou A, Goh NS, Nicholson AG, et al. CT features of lung disease in patients with systemic sclerosis: Comparison with idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia. Radiology. 2004;232:560–7. doi: 10.1148/radiol.2322031223. [DOI] [PubMed] [Google Scholar]
- 3.Strickland B, Strickland NH. The value of high definition, narrow section computed tomography in fibrosing alveolitis. Clin Radiol. 1988;39:589–94. doi: 10.1016/s0009-9260(88)80056-4. [DOI] [PubMed] [Google Scholar]
- 4.Volpicelli G. Lung sonography. J Ultrasound Med. 2013;32:165–71. doi: 10.7863/jum.2013.32.1.165. [DOI] [PubMed] [Google Scholar]
- 5.Piette E, Daoust R, Denault A. Basic concepts in the use of thoracic and lung ultrasound. Curr Opin Anaesthesiol. 2013;26:20–30. doi: 10.1097/ACO.0b013e32835afd40. [DOI] [PubMed] [Google Scholar]
- 6.Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, et al. ; International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS). International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:577–91. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 7.Soldati G, Copetti R, Sher S. Sonographic interstitial syndrome: The sound of lung water. J Ultrasound Med. 2009;28:163–74. doi: 10.7863/jum.2009.28.2.163. [DOI] [PubMed] [Google Scholar]
- 8.Soldati G. Sonographic findings in pulmonary diseases. Radiol Med. 2006;111:507–15. doi: 10.1007/s11547-006-0046-z. [DOI] [PubMed] [Google Scholar]
- 9.Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest. 2008;134:117–25. doi: 10.1378/chest.07-2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gargani L, Doveri M, D’Errico L, Frassi F, Bazzichi ML, Delle Sedie A, et al. Ultrasound lung comets in systemic sclerosis: A chest sonography hallmark of pulmonary interstitial fibrosis. Rheumatology (Oxford) 2009;48:1382–7. doi: 10.1093/rheumatology/kep263. [DOI] [PubMed] [Google Scholar]
- 11.Doveri M, Frassi F, Consensi A, Vesprini E, Gargani L, Tafuri M, et al. Ultrasound lung comets: New echographic sign of lung interstitial fibrosis in systemic sclerosis. Reumatismo. 2008;60:180–4. doi: 10.4081/reumatismo.2008.180. [DOI] [PubMed] [Google Scholar]
- 12.Warrick JH, Bhalla M, Schabel SI, Silver RM. High resolution computed tomography in early scleroderma lung disease. J Rheumatol. 1991;18:1520–8. [PubMed] [Google Scholar]
- 13.Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. Report working party standardization of lung function tests, European Community for Steel and Coal. Official statement of the European Respiratory Society. Eur Respir J Suppl. 1993;16:5–40. [PubMed] [Google Scholar]
- 14.Cotes JE, Chinn DJ, Quanjer PH, Roca J, Yernault JC. Standardization of the measurement of transfer factor (diffusing capacity). Report working party standardization of lung function tests, European Community for Steel and Coal. Official statement of the European Respiratory Society. Eur Respir J Suppl. 1993;16:41–52. [PubMed] [Google Scholar]
- 15.Ziskin MC, Thickman DI, Goldenberg NJ, Lapayowker MS, Becker JM. The comet tail artifact. J Ultrasound Med. 1982;1:1–7. doi: 10.7863/jum.1982.1.1.1. [DOI] [PubMed] [Google Scholar]
- 16.Bourgeois JM, Boynard M, Espinasse P. 1st ed. Paris: Medical Sauramps; 1995. The ultrasound image. [Google Scholar]
- 17.Gutierrez M, Salaffi F, Carotti M, Tardella M, Pineda C, Bertolazzi C, et al. Utility of a simplified ultrasound assessment to assess interstitial pulmonary fibrosis in connective tissue disorders - preliminary results. Arthritis Res Ther. 2011;13:R134. doi: 10.1186/ar3446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lichtenstein D, Mézière G, Biderman P, Gepner A, Barré O. The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med. 1997;156:1640–6. doi: 10.1164/ajrccm.156.5.96-07096. [DOI] [PubMed] [Google Scholar]
- 19.Bouhemad B, Zhang M, Lu Q, Rouby JJ. Clinical review: Bedside lung ultrasound in critical care practice. Crit Care. 2007;11:205.222. doi: 10.1186/cc5668. 2radiating. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Delle Sedie A, Doveri M, Frassi F, Gargani L, D’Errico G, Pepe P, et al. Ultrasound lung comets in systemic sclerosis: A useful tool to detect lung interstitial fibrosis. Clin Exp Rheumatol. 2010;28(5 Suppl 62):S54. [PubMed] [Google Scholar]
- 21.Lichtenstein D. 1st ed. New York: Springer-Verlag; 1992. General Ultrasound in the Critically Ill (L’échographie Générale en Réanimation) pp. 139–41. [Google Scholar]


