Abstract
Purpose:
To obtain baseline data and assess the level of awareness and attitudes towards glaucoma among rural communities of Osun State, Nigeria.
Materials and Methods:
This was a community-based study that involved interviews and descriptive cross-sectional analysis. Serial-recruitment was performed of consenting participants who presented at a community-based screening service in March 2011. Socio-demographic data and information about glaucoma were obtained through face-to-face semi-structured questionnaires.
Results:
The study population comprised 259 respondents (mean age 49.73 ± 16.6 years; range 18 to 90 years). There were 159 females (61.4%). Skilled workers were the most common 130/259 (50.3%) participants. Only 41 (15.8%; 95% CI: 11.4-20.2) participants had ever heard of glaucoma. Sources of information were from visits to an eye clinic for 21/41 (51.2%; 95% CI: 35.9-66.5) participants and 15/41 (36.6%) participants who know someone with glaucoma. Reponses to the causes of glaucoma included 20/41 (48.8%; 33.5-64.1) participant who said ‘I don't know’ and 24.4% of participants who responded ‘curse-from-God’. Responses to questions on treatment included 20/41 (48.8%) participants who responded ‘I don't know how it can be treated’ and 10/41 (36.6%) said ‘medically’. Thirty 30/41 (73.2%) participants would refuse surgery, half of them because ‘it cannot cure or reverse the disease’ while (26.7%) would refuse out of ‘fear’. Only 8/41 (19.5%; 95% CI: 7.4-31.6) would accept surgery for maintenance. Statistically significant predictors of glaucoma awareness were older participants, males and skilled workers (teachers) (P = 0.028, P = 0.018, P = 0.0001, respectively).
Conclusions:
The outcomes of study indicate a low level of awareness of glaucoma. Health education at all levels of health and eye care services is required to prevent ocular morbidity and irreversible blindness from glaucoma.
Keywords: Adults, Attitudes, Awareness, Glaucoma, Rural
INTRODUCTION
Glaucoma is a group of diseases characterized by progressive optic neuropathy and characteristic changes and loss in visual field. More recently it has been described as a neurodegenerative disorder of the optic nerve with acquired loss of retinal ganglion cells.1 It is the 2nd most common cause of blindness in Nigeria and worldwide. Glaucoma constituted 0.7% and 0.4% among the blind in Nigeria and the Southwest region, respectively, out of 13,599 individuals aged 40 years or older who were examined.2,3 It is 2nd only to cataract.2,3 Glaucoma is also the most common cause of functional low vision in Nigeria.4 Similar to Nigeria, glaucoma is the 2nd leading treatable cause of irreversible blindness in south India.5
Blindness from glaucoma can however be prevented if detected early and treated effectively. One of the methods for timely detection and treatment is by having regular eye “screening” during adulthood. This endeavor can be successful if there is awareness of glaucoma. The World-Kidney-Week and World-Glaucoma-Day presented an opportunity in 2011 for members of the College of Health Sciences, Osun State University to carry out screening. This disease is particularly important among individuals of African ancestry, with a 3-4 times higher prevalence and risk of developing blindness.6 Glaucoma has no specific symptoms or signs for the actual onset of disease or the period prior to clinical manifestation of the disease. Symptoms and signs at onset are what usually qualifies for complete screen-able disease.7 Hence, it is important that awareness of glaucoma be raised among the public by all eye care as well as health workers. A previous study of hospital workers in western Nigeria showed that few people working in the eye department had awareness of some eye diseases.8 There is no known data on the level of awareness or attitudes of people in these communities and State to glaucoma. This study was performed to collect baseline data, as well as assessing the level of awareness and attitudes towards glaucoma in the rural communities of Osun State, Nigeria. The findings from this study may assist in planning for prevention of glaucoma-related blindness.
MATERIALS AND METHODS
Background
Patient screening was carried out at Alajue, a rural community in Ede South Local Government Area of Osun State and Ibokun, a sub-urban community in Obokun Local Government Area of Osun State. Osun State is located in Southwest Nigeria. It has about 3 million people with rural dwellers as the majority. Farming is the major occupation. It lies in the rainforest belt of the country. Ladoke Akintola University Teaching Hospital (LTH) is located in Osogbo, the State capital. It provides training and specialized eye services to the people in the state and surrounding regions.
Study design
This was a descriptive, cross-sectional study to assess the level of awareness and attitudes to glaucoma among adults in the communities. Adults aged 18 years and above were eligible to be included. Study participants were serially recruited from adults who voluntarily presented for screening at the venue. All consenting adults were recruited into the study.
Pre-screening activities
Ethical clearance was first sought and obtained from the Research and Ethical Committee of the College of Health Sciences, Osun State University, Nigeria. The community leaders were subsequently approached. The purpose was to mark the world glaucoma and world kidney days in 2011. The intention was to raise awareness of these non-communicable diseases i.e., glaucoma and other eye diseases, kidney, and in addition hypertension and diabetes mellitus, so that morbidity from these diseases could be prevented. Secondly, there was a general health screening for these diseases and screening for glaucoma and other eye diseases. The advantages of the free health and eye screenings were discussed with all individuals who presented at the screening venue. The procedure for screening was explained to all individuals and they were assured that no harm would be caused. The community were informed by announcements in the churches, mosques, market days and through the town crier. Permission was sought to enter the community and a date was agreed upon after the community members were duly informed.
Screening/survey activities
This study was performed over 2 days in March 2011. The first day was in Alajue and the second day in Ibokun. The screening was carried out at the community halls. Health talks were given on care of the eyes and common eye problems. There were 4 stations for the screening process. The first station had research assistants registering respondents as well as collecting the demographic data such as gender, occupation, age, and community. The second station was used to test aided and unaided visual acuity one eye at a time. Pinhole testing was performed for visual acuity less than 6/9. An improvement suggested refractive error. Visual acuity was measured by ophthalmic nurses. The third station had two resident ophthalmologists who administered a semi-structured pre-tested questionnaire by face-to-face interview. The questions covered the awareness of glaucoma, sources of information, causes, types of treatment and attitude to surgery. The fourth station had two ophthalmologists who examined the anterior and posterior segments of the eye. The instruments (ophthalmoscopes, tonometer) for examination were well calibrated prior to use to ensure valid results. Suspicious glaucomatous discs were classified as relative afferent pupillary defect (RAPD), cupping of the optic disc >0.6 and cupping in both eyes with asymmetry of >0.1. This group underwent applanation tonometry done using the hand-held Perkins applanation tonometer. Intraocular pressures >21 mmHg was considered a glaucoma suspect. These subjects were sent for perimetry. The other eye diseases such as conjunctivitis were treated while conditions requiring surgery or follow-up were referred to the base hospital.
Data were managed using SPSS software version 15 (IBM Corp., New York, NY, USA). Consistency of data were checked by double entry and checking for outliers. Descriptive analysis was performed with derivation of proportions, 95% confidence interval (CI), mean and standard deviations. Test of significance was performed using bivariate analysis and Chi square test, and P < 0.05 was considered statistically significant.
RESULTS
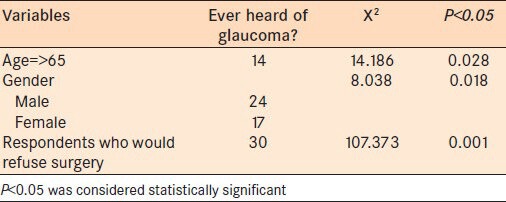
The study sample was comprised of 100 males (38.6%) and 159 females (61.4%). The age of the study sample ranged from 18 to 90 years (mean 49.73 ± 16.6 years). There were statistically significantly more females, especially in the younger age groups, than males.(X2 = 15.685, P = 0.001). Table 1 presents the socio-demographic characteristics with skilled respondents as the most common professionals 100 (38.6%). Fifteen (5.8%) respondents had a family history of blindness, 12 (4.75%) respondents said blindness was not applicable to their family while 232 (89.6%) denied any family history of blindness. Two hundred and eighteen of 259 (84.2%) respondents had never heard of glaucoma and 41/259 (15.8%) respondents had heard of glaucoma. Sources of information were from visits to eye clinic 21/41 (51.2%; 95% CI: 35.9-66.5), relations 15/41 (36.6%; 95% CI: 21.8-51.3), and radio/TV/other sources 5/41 (12.2%; 95% CI: 2.2-22.2). Twenty 20/41 (48.8%; 95% CI: 33.5-64.1) did not know the causative factor while 10 (24.4%; 95% CI: 11.2-37.5) thought it was a ‘curse from God’ [Table 2]. Twenty 20/41 (48.8% CI 33.5-64.1) responded “I don't know how it can be treated” [Table 2]. Other responses are presented in [Table 2]. Thirty 30/41 (73.2%) respondents answered that they would not accept surgery while 8/41 (19.5%; 95% CI: 7.4-31.6) respondents would have accepted surgery for maintenance [Table 2]. Reasons for refusal of surgery included ‘it cannot cure or reverse the disease’ by 15 (50.0%) respondents [Table 2]. Awareness of glaucoma was highest among 65 years and older, while there was a statistically significant reduced level of awareness across all the other age-groups (X2 = 14.186, P = 0.028) [Table 3]. Across gender, males had a statistically significant higher level of awareness than the females (X2 = 8.038, P = 0.018) [Table 3]. The level of awareness was also statistically significantly highest among the skilled professionals who were mainly teachers (X2 = 104,950, P = 0.0001).
Table 1.
Sociodemographic characteristics of 259 respondents surveyed for glaucoma
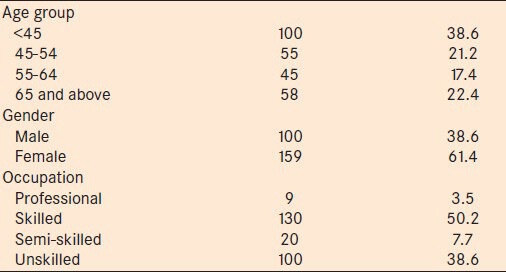
Table 2.
Knowledge and attitude of 41 respondents towards glaucoma
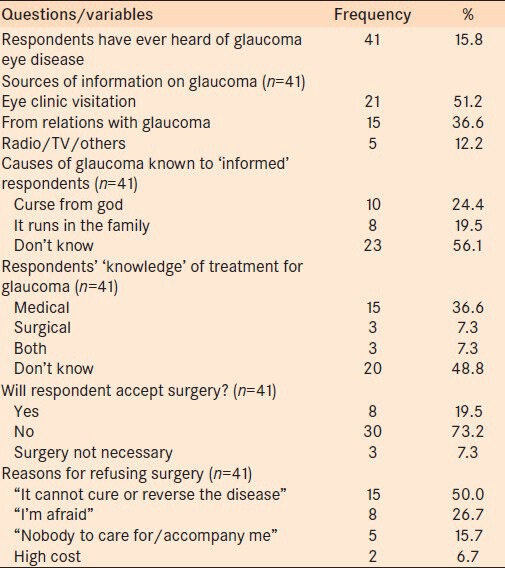
Table 3.
Statistical relationship with age, gender and response to accepting surgery
DISCUSSION
Glaucoma is a non-symptomatic cause of irreversible blindness. Early detection, prompt and effective treatment can be offered to prevent progression of this disease. Awareness of glaucoma can assist in reducing ocular morbidity. In this study, there was a statistically significant greater number females than males (P = 0.001). This could be a reflection of a more caring attitude of women than men towards health care. Similar findings were reported in a Canadian study.10 However this observation is in contrast to findings reported by other authors from Ethiopia11 and Nepal12 where males predominated. The differences between studies may be cultural where women are not allowed to express themselves fully.
Teachers, as one of the skilled professionals topped the list among the professions, closely followed by unskilled groups such as farmers. These could have been due to the education level of teachers compared to most farmers who had little or no education. Additionally the planting season prevented larger numbers of farmers presenting for screening.
There was a large proportion of people (>4/5th), who had never heard of glaucoma, while only 15.8% had heard about it previously. Hence, raising awareness of glaucoma is imperative to eye care workers and other health care workers. This is due to the fact that glaucoma has been found to be the major cause of irreversible blindness and functional low vision in Nigeria. This scenario appears to be applicable to the developing parts of the world such as Asia and Africa where similar reports have been published.5,10 For example, lower values compared to our study have been reported such as 2.4% of 340 people in Ethiopia and, only 0.32% of 5573 respondents in southern Indian rural population study who were aware of glaucoma after being interviewed.5,10 The opposite was the case in countries such as Canada where a study found 73% of 243 respondents had heard of glaucoma and 29% could identify the accurate definition.9 In some Australian studies, 93% and 77% were ‘glaucoma aware’, respectively as far back as 1995-1997.12,13 The outcomes from Canada and Australia are most likely due to the fact that they are a more developed and enlightened community than ours.
The majority of those who had heard of glaucoma did so from visits to, and attendance at the eye clinic. This was closely followed by information from relations (family members) who have glaucoma. These two avenues can be maximally exploited by eye care workers. Health education should usually be given at the waiting area prior to consultation and the Ophthalmologist could always educate the patient on what glaucoma is as well as invite family members for screening. In fact, at the first visit to an eye clinic, a patient should have an opportunistic glaucoma screening. The fact that the radio and TV were the least significant source of information clearly shows a deficiency in educating the public through these media. Notably radio and TV have been proven to be one of the most effective means that could be used to educate the public and raise awareness. This was demonstrated in a study in England where awareness was increased from 22% before and 69% after radio enlightenment among an Indian population.14
Additionally, in southern India, the most common source of awareness of glaucoma was TV/magazines followed by family members with glaucoma.15 In a representative German population survey, the most common source of awareness was through friends 44% of the time, which was greater than from physicians (13% of the time).16 Similar results were presented in a survey of an urban Indian population.17
In the current study, almost half of the respondents did not know the causative factor while about a quarter thought it was ‘a curse from God’. Even though the educational status attained was not recorded in this study, it appeared that greater education was associated with an increase level of awareness as reflected among the teachers. Other authors have also documented that the level of education was strongly associated with an increased level of awareness of glaucoma.9,10 Furthermore, males and those with increased age had greater awareness of glaucoma. Similar findings were reported in another study.11 In contrast to a hospital population study within the same region of this study, those who worked in the ophthalmic unit, and had higher social class had more awareness of eye diseases including glaucoma.8
Approximately 49% (20 of the 41 respondents) had no knowledge of glaucoma treatment while 36% said it could be treated medically. This shows a small proportion of respondents who were aware of treatment. In the study performed in Germany, most of the respondents were aware of certain treatment measures such as surgery (63%) and laser (23%).16 This shows a higher level of knowledge in glaucoma treatment than in our society. It was seen that 73% of the respondents would not accept surgery while 7.3% felt there was no need for surgery.
Fifty percent of those who refused surgery did so because they were told it could not cure or reverse the disease. Cost was seen to be the least of the causes. Similarly, 5/208 (31.2%) patients refused surgery in a survey from Lagos, Nigeria where the major cause of refusing surgery was due to fear among 47.7% of patients, and fear of going blind among 29.2% of those who refused surgery.18 In practice, often times when patients are offered glaucoma surgery, the most common cause of refusal is because they would not be able to recover or regain their vision. This is almost similar to the fear of going blind seen in a previous study from Lagos.18
The outcomes of this study indicate that only a few respondents would usually accept surgery, no matter the explanations and advantages provided to them. An increased level of awareness of glaucoma and possibly knowledge about its irreversible blinding effect is therefore imperative among the population. This would help encourage the public to present for early check-up or uptake of services so that blindness can be prevented. Despite the present low level of glaucoma awareness in our society, it is very possible that this could be changed through public health education as well as having accessible eye care services. An example was seen in Tanzania where many glaucoma patients, who did not have knowledge of the disease and its treatment, still sought eye care. Many had also made numerous visits to the facility and received treatment for glaucoma in the form of eye drops while 16.7% underwent surgery.19
There are some limitations to this study. For example, serial recruitment could confer a certain degree of representation as there could have been selection bias. There was also an inability to obtain the respondents level of education.
In conclusion, there was a low level of awareness of glaucoma and its management in the communities from Osun State, southwest Nigeria surveyed in this study. Attitude to surgical treatment was not encouraging. Health education at all levels of health and eye care services is required to reduce ocular morbidity and irreversible blindness from glaucoma.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Singapore: American Academy of Ophthalmology; 2011. The basic and clinical science course. Section 10, 2011-2012 Glaucoma; p. 3. [Google Scholar]
- 2.Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–51. [PMC free article] [PubMed] [Google Scholar]
- 3.Abdull MM, Sivasubramaniam S, Murthy GV, Gilbert C, Abubakar T, Ezelum C, et al. Causes of blindness and visual impairment in Nigeria: The Nigeria national blindness and visual impairment survey. Invest Ophthalmol Vis Sci. 2009;50:4114–20. doi: 10.1167/iovs.09-3507. [DOI] [PubMed] [Google Scholar]
- 4.Entekume G, Patel J, Sivasubramaniam S, Gilbert CE, Ezelum CC, Murthy GV, et al. Prevalence, causes, and risk factors for functional low vision in Nigeria: Results from the national survey of blindness and visual impairment. Invest Ophthalmol Vis Sci. 2011;52:6714–9. doi: 10.1167/iovs.11-7293. [DOI] [PubMed] [Google Scholar]
- 5.Robin AL, Nirmalan PK, Krishnadas R, Ramakrishnan R, Katz J, Tielsch J, et al. The utilization of eye care services by persons with glaucoma in rural South India. Trans Am Ophthalmol Soc. 2004;102:47–54. [PMC free article] [PubMed] [Google Scholar]
- 6.Friedman DS, Wolfs RC, O’Colmain BJ, Klein BE, Taylor HR, West S, et al. Prevalence of open-angle glaucoma among adults in the United States. Arch Ophthalmol. 2004;122:532–8. doi: 10.1001/archopht.122.4.532. Erratum in: Arch Ophthalmol 2011;129:1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maul EA, Jampel HD. Glaucoma screening in the real world. Ophthalmology. 2010;117:1665–6. doi: 10.1016/j.ophtha.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Adegbehingbe BO, Bisiriyu LA. Knowledge, attitudes, and self care practices associated with glaucoma among hospital workers in Ile-Ife, Osun State, Nigeria. Tanzan J Health Res. 2008;10:240–5. doi: 10.4314/thrb.v10i4.45080. [DOI] [PubMed] [Google Scholar]
- 9.Altangerel U, Nallamshetty HS, Uhler T, Fontanarosa J, Steinmann WC, Almodin JM, et al. Knowledge about glaucoma and barriers to follow-up care in a community glaucoma screening program. Can J Ophthalmol. 2009;44:66–9. doi: 10.3129/i08-175. [DOI] [PubMed] [Google Scholar]
- 10.Tenkir A, Solomon B, Deribew A. Glaucoma awareness among people attending ophthalmic outreach services in Southwestern Ethiopia. BMC Ophthalmol. 2010;10:17. doi: 10.1186/1471-2415-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thapa SS, Berg RV, Khanal S, Paudyal I, Pandey P, Maharjan N, et al. Prevalence of visual impairment, cataract surgery and awareness of cataract and glaucoma in Bhaktapur district of Nepal: The Bhaktapur glaucoma study. BMC Ophthalmol. 2011;11:2. doi: 10.1186/1471-2415-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Attebo K, Mitchell P, Cumming R, Smith W. Knowledge and beliefs about common eye diseases. Aust N Z J Ophthalmol. 1997;25:283–7. doi: 10.1111/j.1442-9071.1997.tb01516.x. [DOI] [PubMed] [Google Scholar]
- 13.Livingston PM, Lee SE, De Paola C, Carson CA, Guest CS, Taylor HR. Knowledge of glaucoma, and its relationship to self-care practices, in a population sample. Aust N Z J Ophthalmol. 1995;23:37–41. doi: 10.1111/j.1442-9071.1995.tb01643.x. [DOI] [PubMed] [Google Scholar]
- 14.Baker H, Murdoch IE. Can a public health intervention improve awareness and health-seeking behaviour for glaucoma? Br J Ophthalmol. 2008;92:1671–5. doi: 10.1136/bjo.2008.143537. [DOI] [PubMed] [Google Scholar]
- 15.Krishnaiah S, Kovai V, Srinivas M, Shamanna BR, Rao GN, Thomas R. Awareness of glaucoma in the rural population of Southern India. Indian J Ophthalmol. 2005;53:205–8. doi: 10.4103/0301-4738.16685. [DOI] [PubMed] [Google Scholar]
- 16.Pfeiffer N, Krieglstein GK, Wellek S. Knowledge about glaucoma in the unselected population: A German survey. J Glaucoma. 2002;11:458–63. doi: 10.1097/00061198-200210000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Dandona R, Dandona L, John RK, McCarty CA, Rao GN. Awareness of eye diseases in an urban population in southern India. Bull World Health Organ. 2001;79:96–102. [PMC free article] [PubMed] [Google Scholar]
- 18.Adekoya BJ, Akinsola FB, Balogun BG, Balogun MM, Ibidapo OO. Patient refusal of glaucoma surgery and associated factors in Lagos, Nigeria. Middle East Afr J Ophthalmol. 2013;20:168–73. doi: 10.4103/0974-9233.110612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewallen S, Hassan HG, Al Attas AH, Courtright P. A population-based study of care-seeking behavior in rural Tanzanians with glaucoma blindness. J Glaucoma. 2011;20:361–5. doi: 10.1097/IJG.0b013e3181eda983. [DOI] [PubMed] [Google Scholar]


